37
Other Rheumatologic Diseases
Systemic-Onset Juvenile Idiopathic Arthritis (SoJIA; Still’s Disease) and Adult-Onset Still’s Disease (AoSD)
• Among the major types of juvenile idiopathic arthritis (JIA; formerly juvenile rheumatoid arthritis [JRA]), cutaneous manifestations are most common in SoJIA, psoriatic arthritis (see Chapter 6), and rheumatoid factor (RF)-positive polyarthritis (rheumatoid nodules and other findings similar to rheumatoid arthritis [RA]; see below).
• Both SoJIA and AoSD are characterized by daily spiking fevers (especially in the late afternoon/early evening) accompanied by an evanescent eruption of salmon-pink macules and slightly edematous papules and plaques (Fig. 37.1A,B); these lesions are usually asymptomatic and favor sites of pressure or trauma, often occurring in a linear array.



Fig. 37.1 Cutaneous findings in Still’s disease. A Evanescent pink papules and plaques in a child. Note the linear array of some of the lesions. B Multiple pink macules and urticarial papules that developed during a fever spike in a woman. C Flagellate array of pinkish-tan, scaly persistent plaques on the upper back in a teenage girl. A, Courtesy, Carlos Nousari, MD; B, Courtesy, Diane Davidson, MD; C, Courtesy, Julie V. Schaffer, MD.
• Less common skin findings include periorbital edema and persistent pruritic papules and plaques that are scaly, violaceous to reddish brown in color, and linear in configuration (Fig. 37.1C).
• DDx: infections (e.g. parvovirus B19), rheumatic fever, serum sickness-like reactions, urticarial vasculitis, Schnitzler’s syndrome (in adults; see Chapter 14), other autoimmune connective tissue diseases, hereditary periodic fever syndromes (see Table 3.2).
Rheumatoid Arthritis
• Chronic inflammatory disorder characterized primarily by destructive arthritis.
• RF and anti-cyclic citrullinated peptide (CCP) antibodies represent serologic markers of RA.
• Cutaneous manifestations of RA are presented in Table 37.1 and Fig. 37.2; these findings can serve as diagnostic clues or signs of serious systemic disease.
Table 37.1
Cutaneous manifestations of rheumatoid arthritis (RA).
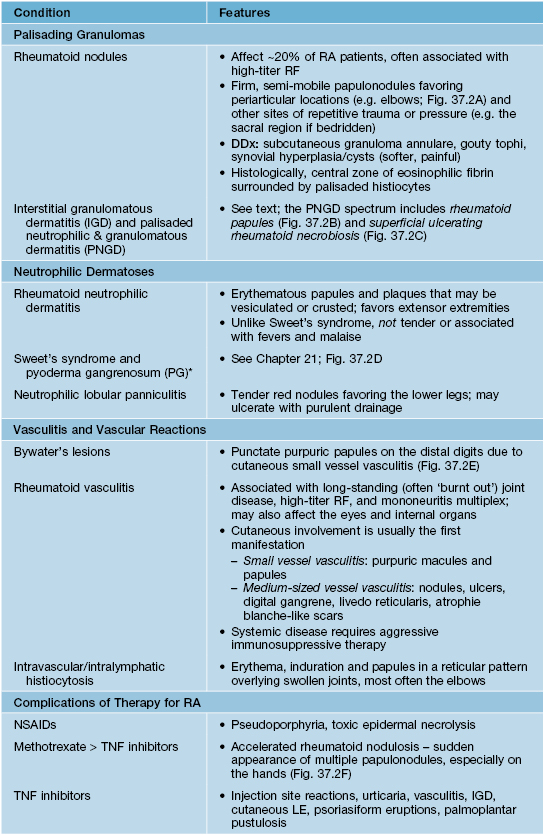
* ‘PG-like’ leg ulcers are a feature of Felty syndrome, which is characterized by the triad of neutropenia, splenomegaly, and RA; Felty syndrome may be associated with T-cell large granular lymphocyte leukemia.






Fig. 37.2 Cutaneous findings in rheumatoid arthritis. A Rheumatoid nodules in a periarticular location on the hands. B Rheumatoid papules presenting as coalescing red-brown lesions, some with scale-crust, on the lower extremity. C Superficial ulcerating rheumatoid necrobiosis manifesting as shiny, yellow-brown plaques with red-brown borders and areas of ulceration; these clinical findings are reminiscent of necrobiosis lipoidica, although both this entity and rheumatoid papules are categorized as forms of palisaded neutrophilic and granulomatous dermatitis. D Pyoderma gangrenosum resulting in recurrent ulcerations on the lower extremities. E Bywater’s lesions. These tender purpuric papules on the distal fingers are characterized histologically by leukocytoclastic vasculitis. F Methotrexate-induced nodulosis. A, Courtesy, Kalman Watsky, MD; B, C, E, Courtesy, Jeffrey Callen, MD; D, Courtesy, Carlos Nousari, MD; F, Courtesy, Jean L. Bolognia, MD.
Interstitial Granulomatous Dermatitis (IGD) and Palisaded Neutrophilic and Granulomatous Dermatitis (PNGD)
• IGD presents as annular erythematous plaques or linear cords (‘rope sign’) that favor the lateral and upper trunk, axillae, medial thighs, and buttocks (Fig. 37.3); patients often have RA or seronegative arthritis.



Fig. 37.3 Interstitial granulomatous dermatitis (IGD). A Large, symmetric pink patches and thin plaques that resemble patch-type granuloma annulare. B Annular lesions on the medial thighs. C Firm linear cord along the axillary line in a patient with rheumatoid arthritis. A, C, Courtesy, Kathryn Schwarzenberger, MD; B, Courtesy, Jeffrey Callen, MD.
• PNGD presents as skin-colored to erythematous, umbilicated papulonodules that are often crusted and favor the elbows (see Fig. 19.11B) and extensor hands/fingers; associated with RA, SLE, and ANCA-positive systemic vasculitides (e.g. Churg–Strauss syndrome).
Sjögren’s Syndrome
• Additional features can include vaginal dryness, arthritis, peripheral neuropathy, internal organ involvement (e.g. kidneys), and development of B-cell lymphoma (often extranodal marginal zone).
• Diagnostic criteria for Sjögren’s syndrome are presented in Table 37.2.
Table 37.2
American College of Rheumatology 2012 classification criteria for Sjögren’s syndrome.
Other possible causes of similar findings include chronic GVHD, primary systemic amyloidosis, sarcoidosis, and radiation therapy of the head and neck.
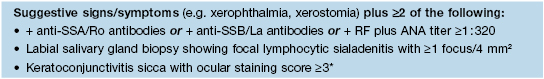
* Using fluorescein and lissamine green to stain the cornea (score of 1–6) and conjunctiva (score of 1–3), respectively; other assessment methods include Schirmer and Rose Bengal tests.
Relapsing Polychondritis
• Most patients develop erythema, swelling and pain of the cartilaginous portion of the auricle, with sparing of the earlobe (Fig. 37.4A).

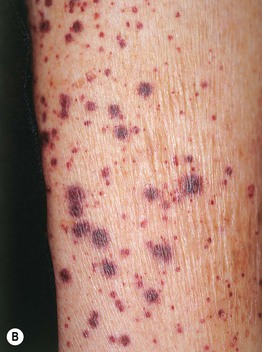
Fig. 37.4 Cutaneous findings in relapsing polychondritis. A Erythema and swelling of the ear with sparing of the earlobe. B Small vessel vasculitis presenting as palpable purpura in a patient who also had myelodysplastic syndrome. A, Courtesy, Kalman Watsky, MD; B, Courtesy, Jean L. Bolognia, MD.
• Other manifestations include cutaneous small vessel vasculitis (Fig. 37.4B), aphthae (oral or genital; may overlap with Behçet’s disease), nasal chondritis (potentially producing a saddle nose deformity), involvement of cartilage of the respiratory tract (e.g. larynx, trachea, bronchi) and costochondral junctions, arthritis, ocular inflammation, audiovestiblar damage, and myelodysplastic syndrome.
• DDx: early phase – erysipelas, cellulitis, infectious chondritis or zoster; nasal destruction – Wegener’s granulomatosis, nasal natural killer/T-cell lymphoma, infections (e.g. mucocutaneous leishmaniasis) (see Table 19.3).
Mixed Connective Tissue Disease (MCTD)
• Favors women (female : male ratio ~9 : 1) in the second and third decades of life.
• Rx: varies depending on the organs involved and disease severity.
For further information see Ch. 45. From Dermatology, Third Edition.







