7
Other Papulosquamous Disorders
Parapsoriasis
• Two major forms of parapsoriasis are small plaque (lesions usually <5 cm in diameter) and large plaque (usually >5 cm); digitate dermatosis is a form of the former, whereas retiform parapsoriasis is a variant of the latter (Figs. 7.1 and 7.2).


Fig. 7.1 Small plaque parapsoriasis. A Small (<5 cm), pink slight scaly patches. B Digitate dermatosis with elongated finger-like lesions on the flank. Digitate dermatosis is the exception to the 5-cm rule as the lesions may measure 10 cm or more along their long axes. A, Courtesy, Gary Wood, MD, and George Reizner, MD.
Pityriasis Lichenoides et Varioliformis Acuta (PLEVA) and Pityriasis Lichenoides Chronica (PLC)
• In both forms, there are recurrent crops of papules with individual lesions spontaneously resolving over weeks (PLEVA) to months (PLC); only occasionally is there an obvious trigger (e.g. viral infection, medication); the entire course of the disorder can last for years.
• PLEVA occurs more commonly in younger age groups; it is characterized by widespread erythematous papules that are often crusted but may be vesicular or pustular (Fig. 7.3A–C).



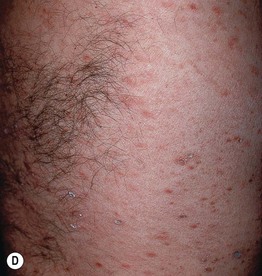

Fig. 7.3 Clinical spectrum of pityriasis lichenoides. In the acute form (PLEVA), widespread erythematous papules and papulovesicles are admixed with crusted lesions (A, B); sometimes there can be an ulcerative component (C). Lesions can heal with varioliform scars. Individuals with the chronic form (PLC) develop multiple red-brown papules, some of which have scale (D); these lesions often heal with hypopigmentation, especially in patients with darkly pigmented skin (E). A, Courtesy, Julie V. Schaffer, MD; B, Courtesy, Thomas Schwarz, MD.
• PLC is characterized by pink to red-brown papules with scale and can resolve with post-inflammatory guttate hypopigmentation (Fig. 7.3D,E).
Pityriasis Rosea
• The etiology is unknown, but viral infections may serve as a trigger.
• Lesions increase in number and extent over a few weeks but then spontaneously resolve; classically, the initial lesion, known as the ‘herald patch,’ is often the largest (Fig. 7.4).

Fig. 7.4 Pityriasis rosea – herald patch. It typically precedes the development of a more widespread eruption. Courtesy, Kalman Watsky, MD.
• The distribution is that of a 1920s bathing suit – proximal extremities and trunk; occasionally, an inverse pattern is seen in which the majority of lesions are in the axillae and/or groin (Fig. 7.5).

Fig. 7.5 Inverse pityriasis rosea. In this variant, the lesions are limited to the groin and/or axillae. The long axes of the lesions follow the lines of cleavage.
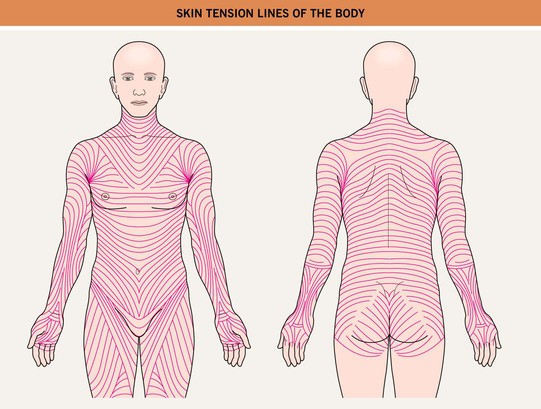
• Pink to salmon-colored papules or plaques are round or oval in shape (Fig. 7.6), with their long axes following Langer’s lines of cleavage (Fig. 7.7), creating a ‘Christmas tree’ pattern on the trunk; scale, both fine white centrally and as a collarette at the edge of the lesion, is the most common secondary change, but occasionally crusting, vesicles, purpura, or even pustules may be seen.



Fig. 7.6 Pityriasis rosea. A, B Both round and oval-shaped plaques can be seen as well as fine white scale and collarettes of scale. C In patients with more darkly pigmented skin, central hyperpigmentation can develop and there may be a more follicular pattern. B, Courtesy, Julie V. Schaffer, MD; C, Courtesy, Aisha Sethi, MD.
• The average duration is 6–8 weeks, with some cases lasting for months.
• DDx: guttate psoriasis, secondary syphilis (preceding chancre, usually genital; accompanied by malaise, lymphadenopathy, other mucocutaneous signs such as condyloma latum, palmoplantar lesions; positive Venereal Disease Research Laboratory [VDRL] or rapid plasma reagin [RPR] test), pityriasis lichenoides chronica (especially if persistent), nummular dermatitis (if vesicular), pityriasis rosea-like drug eruptions (e.g. ACE inhibitors, metronidazole).
Pityriasis Rubra Pilaris
• One of the dermatologic disorders that can lead to an erythroderma (Fig. 7.8), often with an onset in the head and neck region; peaks of incidence – first to second decade of life and sixth decade of life.

Fig. 7.8 Erythroderma due to pityriasis rubra pilaris. Within areas of erythema, follicular hyperkeratosis (knee) may be more difficult to appreciate than in areas of relative sparing (compare to Fig. 7.9A).
• It is characterized by a salmon or orange-red color, islands of sparing, follicular papules (including within the relatively spared areas and on the dorsal fingers), and a waxy keratoderma (Fig. 7.9).



Fig. 7.9 Pityriasis rubra pilaris. A Follicular papules within islands of sparing and confluent orange-red scaly plaques. B The islands of sparing may be sharply demarcated; note the salmon color of the plaques. C Waxy keratoderma, again with an orange hue. C, Courtesy, Irwin Braverman, MD.
• May be exacerbated by exposure to UV light; classic forms spontaneously resolve within 3–5 years (Fig. 7.10).
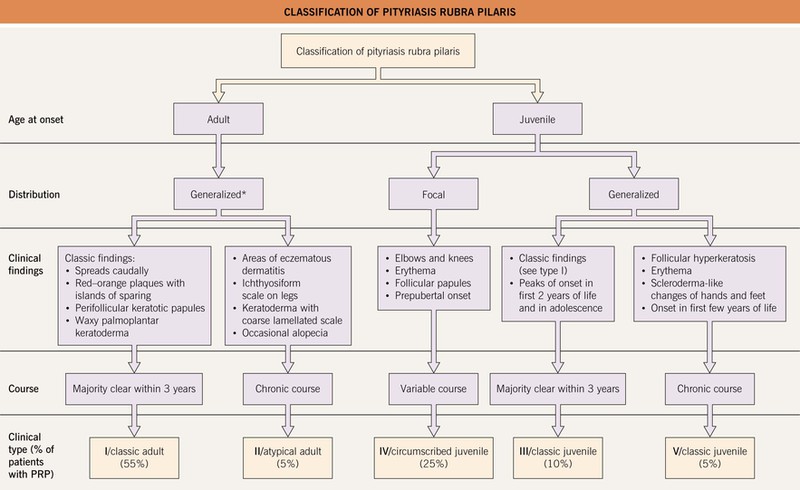
Fig. 7.10 Classification of pityriasis rubra pilaris (PRP). *A generalized distribution of PRP, often with findings similar to type I, may be seen in association with elongated follicular spines, acne conglobata, and hidradenitis suppurativa in HIV-infected individuals; this has been referred to as type VI PRP or the HIV-associated follicular syndrome.
• Five major forms have been described, with distinctions based on age of onset and distribution, with the adult classic form being the most common (Fig. 7.10); occasionally PRP is familial and can be due to CARD14 mutations.
• Rx: oral isotretinion, acetretin, methotrexate, tumor necrosis factor-α inhibitors (mixed results); response should be seen within 6 months.
Pityriasis Rotunda
Granular Parakeratosis
• Red-brown plaques with scale, often thick, that may be related to chronic irritation (Fig. 7.11); there may be secondary maceration and pruritus.
For further information see Ch. 9. From Dermatology, Third Edition.