Other neonatal emergencies: Tracheoesophageal fistula and omphalocele
Tracheoesophageal fistula
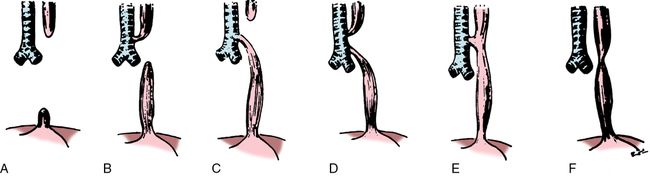
Tracheoesophageal fistula (TEF) occurs as the result of failure of the tracheal bud to develop normally from the primitive foregut. TEF occurs in several forms (Figure 203-1); type C—esophageal atresia (more correctly agenesis because the proximal part of the primitive foregut develops primarily into a trachea rather than an esophagus) with a distal TEF—is the most common form (accounts for 90% of all TEFs). Maternal polyhydramnios may indicate the presence of the lesion before birth. Diagnosis is suspected at birth when the neonate has excessive drooling, cyanotic episodes, or coughing relieved by suctioning or the clinician is unable to pass a soft catheter into the infant’s stomach. TEF can be confirmed by radiography by showing a curled catheter in the upper esophageal pouch with an air bubble in the stomach. Contrast medium is unnecessary and contraindicated because the neonate may aspirate the medium. Associated conditions include prematurity (20%-25%), congenital heart disease (20%-25%), and other midline defects.