CHAPTER 19 Osteochondritis Dissecans
INTRODUCTION
Osteochondral lesions may be the source of chronic elbow pain, swelling, and loss of motion in children or adolescents. The typical presentation is an adolescent gymnast or baseball pitcher.13,34 The dominant arm is usually involved, but may be bilateral in approximately 5% to 20%.34,41
OSTEOCHONDROSIS OF THE CAPITELLUM (PANNER’S DISEASE)
CLINICAL CHARACTERISTICS
Osteochondrosis of the capitellum is characterized by dull, aching pain in the elbow that usually is aggravated by motion or use, particularly by throwing or other violent motions. It usually occurs in boys and always during the period of active ossification of the capitellar epiphysis (ages 7 to 12, peak at 9 years). Panner’s disease is not seen before age 5 years. In addition to pain, loss of 5 to 20 degrees of elbow extension is common. Local swelling and tenderness over the lateral side of the elbow is not unusual.23 Symptoms resolve over time with few sequelae.
RADIOGRAPHIC CHARACTERISTICS
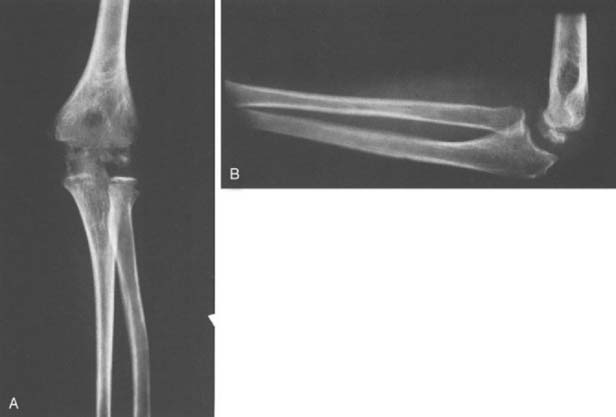
Osteochondrosis of the capitellum is a focal or localized avascular lesion of subchondral bone and its overlying articular cartilage.11 Radiographically, there is fragmentation of the capitellar epiphysis. The fragmentation is due to irregular patches of relative sclerosis alternating with areas of rarefaction (Fig. 19-1A and B). The outline of the epiphysis may be slightly irregular and smaller than that of the opposite normal capitellar epiphysis. Despite the radiographic fragmentation, osteochondral loose bodies do not form. As growth progresses, the capitellar epiphysis eventually assumes a normal appearance in size, contour, and internal architecture as clinical symptoms resolve. Residual deformity of the capitellum is rare.
Magnetic resonance imaging (MRI) findings include decreased signal intensity of the ossified epiphysis on T1-weighted images. Both plain films and MRI images of osteochondrosis of the capitellum are similar to findings in Legg-Calvé-Perthes disease of the hip.25 Deformity and collapse of the articular surface is less common in osteochondrosis of the capitellum than in Perthes’ disease of the hip.
OSTEOCHONDRITIS DISSECANS
INTRODUCTION
Osteochondritis is defined as an inflammation of both bone and cartilage. Osteochondritis dissecans is described as osteochondritis resulting in the splitting of pieces of cartilage into the joint (in Dorland’s Medical Dictionary). The term osteochondritis dissecans was given to this condition by Franz Konig in 1889, who described a knee condition that appeared to suggest a subchondral inflammatory process that dissected a fragment of cartilage from the femoral condyle, leading to formation of a loose body.20
Although no inflammatory process has ever been shown to produce such lesions, the name has remained. Osteochondritis dissecans of the capitellum is similar to osteochondritis dissecans in other joints, such as the knee. It involves localized avascular necrosis of subchondral bone and subsequent loss of structural support for the adjacent articular cartilage. Compared with the knee, however, osteochondritis of the capitellum is much less common. Only 6% of patients with osteochondritis dissecans have elbow involvement.41 Because osteochondritis dissecans occurs after the capitellum has almost completely ossified (early adolescence), it should not be confused with osteochondrosis of the capitellum, nor is it due to an “inflammation,” in spite of the definition of osteochondritis cited earlier.41 Osteochondrosis dissecans and osteonecrosis of the capitellum have been suggested as more appropriate terms, but are rarely used today.
From a practical standpoint, the localized area of osteochondritis, consisting of articular cartilage and underlying bone, either remains in situ and eventually heals or separates from the capitellum and becomes a loose body in the joint. Osteochondritis dissecans is one of several conditions that can cause “Little League elbow” in immature baseball players.38
CLINICAL CHARACTERISTICS
Elbow pain, the most common complaint, is usually dull, poorly localized, and aggravated by use, particularly by athletic endeavors that involve throwing or weight bearing on the upper extremity. Use aggravates the condition and rest relieves it. Lateral elbow pain occurs in approximately 79% to 90% of patients.18,41
A second complaint, limitation of elbow motion, particularly extension, affects about 90% of patients. It is often associated with an effusion, and results in 5 to 20 degrees loss of elbow extension.18,41 Limitation of elbow flexion, pronation, and supination of the forearm also occur, but these problems are less common.
RADIOGRAPHIC CHARACTERISTICS
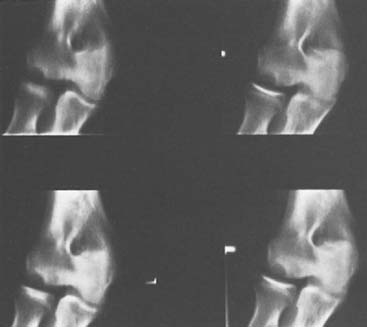
Anteroposterior and lateral radiographs of the elbow are useful and should be obtained in every case. Early in the disease, radiographic changes are most often confined to the capitellum.29 Rarefaction, irregular ossification, and a bony defect adjacent to the articular surface are frequent findings (Fig. 19-2). The crater of rarefaction in the capitellum usually has a sclerotic rim of subchondral bone adjacent to the articular surface.
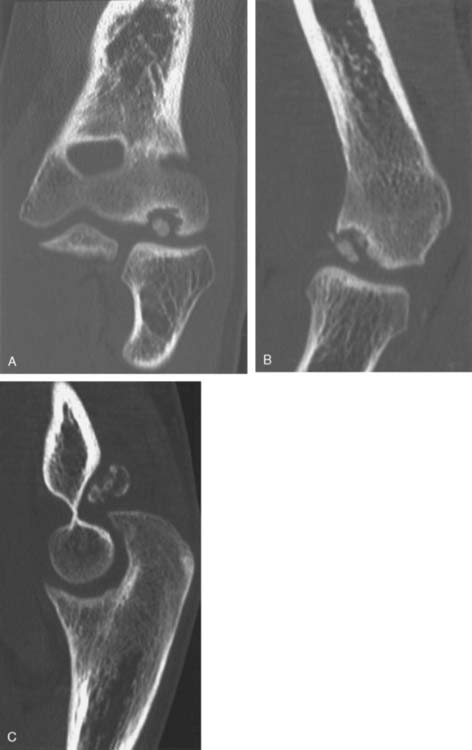
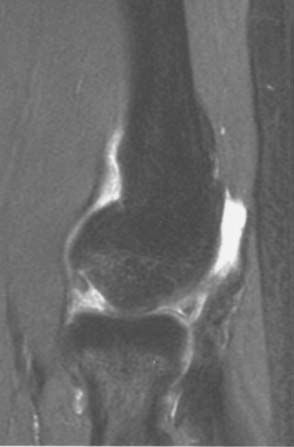
If the central fragment separates, one or more ossific loose bodies may be seen in the joint, and the articular surface of the capitellum may appear to be irregular or flattened, particularly on the lateral view. Only 30% of loose bodies can be seen on plain films.18 Computed tomography (CT) may be necessary to better define the bony anatomy (Fig. 19-3). MRI is the preferred imaging technique for assessing the extent of osteochondritis. MRI is also the best study to assess the integrity of the articular surface and the displacement of osteochondral fragments. Unstable lesions reveal fluid surrounding the osteochondral fragment on T2-weighted images (Fig. 19-4).8
Several other late radiographic changes are worth noting. As degenerative changes occur, the radial head enlarges. Klekamp described seven patients who had developmental dislocations of the radial head as a result of osteochondritis dissecans of the capitellum (Fig. 19-5).15 The cause-and-effect relationship is obscure. In a few instances, premature distal humeral physeal arrest is evident. Late in the course of disease, degenerative changes characterized by irregularity and incongruity of both the capitellar and radial head articular surfaces are evident; these changes are the most important late sequelae of this condition.
If sequestration does not occur, the central sclerotic fragment gradually becomes less distinctive, the surrounding area of rarefaction slowly ossifies, and the lesion heals without significant sequelae. This radiographic evidence of healing may take several years to occur and sometimes is not complete until adult life, long after pain, swelling, and limitation of motion have disappeared (Fig. 19-6A and B).
ETIOLOGY
Ischemia
Because the initial histologic appearance of the involved segment of subchondral bone is that of avascular necrosis, one of the most popular theories holds that some type of ischemic insult affects a localized area of subchondral bone.23 The ischemic theory is based primarily on the histopathologic characteristics of the lesion and the vascular anatomy of the distal humerus.
Haraldsson11 has shown that the vascular supply to the distal humerus is limited in persons aged 5 to 19 years. One or two isolated vessels enter the epiphysis posteriorly, traverse the nonossified cartilaginous epiphysis, and supply the capitellum. No vessels from the metaphysis cross the physis. Because these end arteries supplying the capitellum pass through compressible epiphyseal cartilage, repetitive valgus loading of the elbow may injure the vessels and lead to avascular areas within the epiphysis.34 This theory forms the basis for pitching limitations for young baseball pitchers. The microscopic changes in the involved area of subchondral bone are typical of those seen in bone infarction due to interruption of the subchondral terminal arterial vessels.
If the articular cartilage remains intact and the necrotic segment remains in situ, the avascular segment is eventually absorbed; it is replaced by viable osseous tissue, and the normal architecture of the articular surface is preserved. This healing process may take several years. If, however, the articular cartilage is fractured during the initial stage of the disease, the necrotic segment may become detached and an intra-articular loose body can form.
Trauma
For nearly 100 years, trauma has been suggested as a cause of osteochondritis dissecans. Unfortunately, no experimental data support this or any other theory.17,27
A history of frequent repetitive overuse of the elbow is common in persons who have osteochondritis dissecans. Several authors have noted a relationship between osteochondritis dissecans and baseball pitching.1,4,37,40 The valgus compressive forces generated across the radiocapitellar joint during throwing are believed to induce changes in the distal humerus that lead to osteochondritis dissecans.14 Repetitive trauma also is thought to play a role in the development of the condition in adolescent gymnasts,13,34 who bear their entire body weight on their arms and thus expose their elbows to repetitive compressive forces. Repetitive trauma, particularly forceful extension and pronation of the elbow, creates compression and shearing forces that are transmitted by the radius to the adjacent articular surface of the capitellum. This trauma results in separation and infarction of an area of subchondral bone and the overlying articular cartilage. From a study of cadaver elbows, Schenck suggested that the mechanical disparity between a stiff radial head articulating with a less stiff capitellum produces strain during compressive stresses that can lead to osteochondritis dissecans.33
Genetic Factors
Numerous but sporadic reports describe osteochondritis of the capitellum in one or in several generations of the same family.9,19,25,41 Osteochondritis dissecans has also been reported to occur in more than one joint in a given patient or in more than one family member. Neilson21 reported the incidence of osteochondritis dissecans to be 4.1 per 1000 men. Among male relatives of affected men, he found an incidence of 14.6%. In spite of these reports, there is no convincing evidence that osteochondritis dissecans of the capitellum is a heritable disease.
Multiple epiphyseal dysplasia, which is a rare heritable condition, superficially has many features that are similar to those of this condition.7 Multiple epiphyses are involved. The clinical course and prognosis, however, are in no way similar.
TREATMENT
Treatment of osteochondritis dissecans is dictated by the clinical findings and the radiographic appearance of the lesion. Initial treatment is usually nonoperative: limitation of activities and nonsteroidal anti-inflammatory medications. Rest and protection is continued for several weeks. If these methods fail, good results have been obtained with surgical management. Functional limitations are common.
Intact Lesions
If the lesion is intact with no evidence of displacement from its normal site or of fracture of the articular cartilage, nonoperative treatment is indicated.27 The elbow should be rested and any vigorous use avoided. Application of ice and the use of a nonsteroidal anti-inflammatory medication may relieve symptoms. A hinged elbow brace may be useful to limit activities.28 If pain is a significant complaint, the elbow should be splinted or placed in a cast for 3 to 4 weeks, after which active range-of-motion exercises are prescribed to preserve motion. Activity should be restricted for 6 to 8 weeks after symptoms have resolved. Radiographic changes should be stable or improving before the patient resumes activities. It is unreasonable to restrict all activities until radiographs are normal, because abnormalities can persist for years. When activities are allowed, they should be gradually “advanced” and modified if any symptoms recur. A history of locking or catching should prompt a search for loose or partially attached fragments.34 If symptoms persist but the articular cartilage remains intact, arthroscopic or open antegrade or retrograde subchondral drilling is considered.
Patients with intact lesions treated nonoperatively generally do well.34,41 Most athletes can return to sports, with the exception of baseball pitchers and gymnasts, whose prognosis is more guarded.36,37 With longer follow-up, results are not as good. Takahara, with follow-up of 12 years, found that 50% had clinical and radiographic evidence of osteoarthritis.36
Partially Attached Fragments
If radiographic evaluation or arthroscopic examination finds evidence of fracture or fissure of the articular cartilage or of partial detachment of the fragment, the surgeon has two choices: (1) to reattach the area of avascular bone surgically or (2) to excise the loose fragment.27
In this situation, as in the knee, a partially detached fragment can be pinned in situ with Kirschner wires, Herbert screws, or bioabsorbable implants13,16 under direct vision or arthroscopic control. In situ fixation of large, partially attached or hinged lesions may be useful in preventing complete detachment, loose body formation, and ultimate osteoarthritis.36 The additional value of repeated drilling of the fragment and its bony bed to stimulate revascularization and healing has never been conclusively established. In general, only limited success has been reported from attempts to pin partially attached articular fragments once the underlying bone is exposed.10
Completely Detached Fragments
When the area involved with osteochondritis dissecans has completely detached from the capitellum and is lying free in the joint, the most effective treatment is to remove the fragment surgically, by arthroscopy or arthrotomy.2,13,16,27,34,41 Surgical indications include locking, symptomatic loose bodies, and failure of prolonged nonoperative treatment to relieve symptoms.18,37,41 Arthroscopic techniques using standard 4-mm instruments have been shown to be effective in evaluating and treating elbow disorders such as osteochondritis dissecans.2,10,13 Care must be taken to avoid complications such as nerve palsies.2,26
Most authors agree that the best short-term results are obtained with simple excision of the loose body. Removing the loose body is usually effective in relieving the patient’s pain and mechanical symptoms, although the range of motion may not increase. Late degenerative arthritis may still be the ultimate outcome in as many as 50%.36 Because of evidence that large defects can facilitate degenerative changes, many authors have advocated more complex procedures for such defects. These procedures include drilling, microfracture, fixation, autograft replacement, and autologous cell implantation. Unfortunately, there is little evidence and no long-term follow-up to show that these techniques can prevent the development of osteoarthritis. Procedures other than simple excision are commonly reported but not strongly supported by long follow-up in the literature.2,18,26,34,41 Ruch30 treated 12 elbows with arthroscopic débridement and reported 13 degrees more extension and improved symptoms in 11 elbows (92%) at 3-year follow-up. Curettage and drilling of the defect in the capitellar articular surface is advocated by many.5,12,13,18,31,35,37 The benefit of this approach is difficult to document. In at least two series, the results were no better after drilling, curettage, or trimming of the crater than after removal of the loose body and débridement alone.30,4′ Results are worst with complex procedures involving open excision of the capitellum, bone grafting, and internal fixation of the loose fragment.37,41 Chondral resurfacing and osteochondral grafting procedures have been reported for osteochondritis dissecans of the elbow, but numbers are too small and follow-up is too short to draw conclusions.22,32,39
Short-term postoperative results of arthroscopic loose body removal and débridement vary from series to series. The prognosis for returning to sports varies widely by report but is guarded, especially in throwing sports and gymnastics. McManama and colleagues found that 12 of 14 (86%) patients returned to competitive athletics without restrictions and that elbow range of motion increased 18 degrees after surgeons removed loose bodies, shaved chondral defects, and drilled multiple holes to promote revascularization.18 Tivnon and coworkers37 found a similar 21-degree improvement in range of motion after removal of loose bodies and curettage of the capitellum and improved function in 10 of 12 elbows. After removal of loose bodies, shaving, subchondral drilling, or a combination of these, Janarv and colleagues12 reported that all patients had fewer symptoms or no symptoms and improved elbow motion. Rupp and Tempelhof31 reported mixed results in six patients treated with loose body removal, drilling of the lesion, or débridement of the defect. Results were related to the degree of articular cartilage damage. Singer and Roy34 reported on five female gymnasts with osteochondritis dissecans of the capitellum; two required surgery to excise loose fragments. At 3-year follow-up, all but one had been able to return to competition. In a similar study of gymnasts, Jackson and colleagues found that only one of seven patients was able to continue competitive gymnastics.13 Byrd and Jones treated 10 elbows in adolescent baseball pitchers. All had improved pain but only 4 of 10 (40%) returned to their prior level of activity.6 Tivnon and coworkers37 reported similar (guarded) results among 12 baseball pitchers, only one of whom was able to throw at his prior level.
The long-term prognosis for patients with osteochondritis dissecans of the capitellum depends on the patient’s age and on the size and extent of the lesion. Young patients have more favorable outcomes. Large defects that require surgery in older adolescents often progress to degenerative arthritis. Woodward and Bianco41 (with an average 12-year follow-up, range 2 to 34 years) suggest that most patients believed that they had normal use of their elbow. Bauer and colleagues3 suggest that osteochondritis dissecans of the capitellum leads to osteoarthritis in the majority of patients at long-term follow-up.
SUMMARY
Osteochondritis dissecans of the capitellum is an un-common problem that affects adolescents, especially those engaged in repetitive throwing and gymnastics. Compressive forces at the radiocapitellar joint, along with a tenuous blood supply to the region, may contribute to the development of this condition. Most affected persons are adolescents, who initially note lateral elbow pain, loss of extension, and swelling. These symptoms are aggravated by activity and improve with 6 to 8 weeks of rest. Plain radiographs are usually sufficient to make the diagnosis, although CT, MRI, and arthroscopy may be necessary. It is important to distinguish osteochondritis dissecans from Panner’s disease, a benign, self-limited condition that affects the capitellum in younger children.
1 Albright J.A., Jokl P., Shaw R., Albright J.P. Clinical study of baseball pitchers: correlation of injury to the throwing arm with method of delivery. Am. J. Sports Med. 1978;6:15.
2 Andrews J.R., Carson W.G. Arthroscopy of the elbow. Arthroscopy. 1985;1:97.
3 Bauer M., Jonsson K., Josefsson P.O. Osteochondritis dissecans of the elbow. A long-term follow-up study. Clin. Orthop. 1992;284:156.
4 Brown R., Blazina M.E., Derlan R.K., Carter V.S., Jobe F.W., Carlson G.J. Osteochondritis of the capitellum. J. Sports Med. 1974;2:27.
5 Brownlow H.C., O’Connor-Reid L.M., Perko M. Arthroscopic treatment of osteochondritis dissecans of the capitellum. Knee Surg. Sports Traumatol. Arthrosc. 2006;14:198.
6 Byrd J.W., Elrod B.F., Jones K.S. Elbow arthroscopy for neglected osteochondritis dissecans of the capitellum. J. Southern Orthop. Assoc. 2001;10:12.
7 Clanton T.O., DeLee J.E. Osteochondritis dissecans. Clin. Orthop. 1982;167:50.
8 Fritz R.C., Steinbach L.S., Tirman P.F., Martinez S. MR imaging of the elbow. An update. Radiol. Clin. North Am. 1997;35:117.
9 Gardiner J.B. Osteochondritis dissecans in three members of one family. J. Bone Joint Surg. 1955;37B:139.
10 Guhl J.F. Arthroscopy and arthroscopic surgery of the elbow. Orthopedics. 1985;8:1290.
11 Haraldsson S. On osteochondrosis deformans juvenitis, capituli humeri including investigation of intraosseous vasculature in distal humerus. Acta Orthop. Scand. Suppl. 1959;38:1.
12 Janarv P.M., Hesser U., Hirsch G. Osteochondral lesions in the radiocapitellar joint in the skeletally immature: radiographic, MRI, and arthroscopic findings in 13 consecutive cases. J. Pediatr. Orthop. 1997;17:311.
13 Jackson D.W., Silvino N., Reiman P. Osteochondritis in the female gymnast’s elbow. Arthroscopy. 1989;5:129.
14 King J.W., Brelsford H.S., Tullos H.S. Analysis of the pitching arm of the professional baseball pitcher. Clin. Orthop. 1969;67:116.
15 Klekamp J., Green N.E., Mencio G.A. Osteochondritis dissecans as a cause of developmental dislocation of the radial head. Clin. Orthop. 1997;338:36.
16 Kuwahata Y., Inoue G. Osteochondritis dissecans of the elbow managed by Herbert screw fixation. Orthopedics. 1998;21:449.
17 Lindholm T.S., Osterman K., Vankka E. Osteochondritis dissecans of elbow, ankle, and hip. Clin. Orthop. 1980;148:245.
18 McManama G.B., Michel L.J., Berry M.V., Sohn R.S. The surgical treatment of osteochondritis of the capitellum. Am. J. Sports Med. 1985;13:11.
19 Mitsunaga M.M., Adishian D.O., Bianco A.J.Jr. Osteochondritis dissecans of the capitellum. J. Trauma. 1982;22:53.
20 Naguro S. The so-called osteochondritis dissecans of Konig. Clin. Orthop. 1960;18:100.
21 Neilson N.A. Osteochondritis dissecans capituli humeri. Acta Orthop. Scand. 1933;4:307.
22 Oka Y., Ikeda M. Treatment of severe osteochondritis dissecans of the elbow using osteochondral grafts from a rib. J. Bone Joint Surg. 2001;83B(5):738.
23 Omer G.E.J. Primary articular osteochondroses. Clin. Orthop. 1981;158:33.
24 Paes R.A. Familial osteochondritis dissecans. Clin. Radiol. 1989;40:501.
25 Panner H.J. A peculiar affection of the capitellum humeri, resembling Calve-Perthes disease of the hip. Acta Radiol. 1927;8:617.
26 Papilion J.D., Neff R.S., Shall L.M. Compression neuropathy of the radial nerve as a complication of elbow arthroscopy: a case report and review of the literature. Arthroscopy. 1988;4:284.
27 Pappas A.M. Osteochondritis dissecans. Clin. Orthop. 1981;158:59.
28 Peterson R.K., Savoiem F.H.3rd, Field L.D. Osteochondritis dissecans of the elbow. Instr. Course Lect. 1999;48:393.
29 Roberts N., Hughes R. Osteochondritis dissecans of the elbow joint: a clinical study. J. Bone Joint Surg. 1950;32B:348.
30 Ruch D.S., Cory J.W., Poehling G.G. The arthroscopic management of osteochondritis dissecans of the adolescent elbow. Arthroscopy. 1998;14:797.
31 Rupp S., Tempelhof S. Arthroscopic surgery of the elbow. Therapeutic benefits and hazards. Clin. Orthop. 1995;313:140.
32 Sato M., Ochi O., Uchio Y., Agung M., Baba H. Transplantation of tissue-engineered cartilage for excessive osteochondritis dissecans of the elbow. J. Shoulder Elbow Surg. 2004;13:221.
33 Schenck R.C., Athanasiou K.A., Constantinides G., Gomez E. A biomechanical analysis of articular cartilage of the human elbow and a potential relationship to osteochondritis dissecans. Clin. Orthop. 1994;299:305.
34 Singer K.M., Roy S.P. Osteochondrosis of the humeral capitellum. Am. J. Sports Med. 1984;12:351.
35 Smillie I.S. Osteochondritis Dissecans: Loose Bodies in Joints; Etiology, Pathology, Treatment. Edinburgh: E. & S. Livingstone, 1960.
36 Takahara M., Ogino T., Sasaki I., Kato H., Minami A., Kaneda K. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin. Orthop. 1999;363:108.
37 Tivnon M.C., Anzel S.H., Waugh T.R. Surgical management of osteochondritis dissecans of the capitellum. Am. J. Sports Med. 1976;4:121.
38 Torg J.S. Little League: the theft of a carefree youth. Physician Sports Med. 1973;1:72.
39 Tsuda E., Ishibashi Y., Sato H., Yamamoto Y., Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the capitellum in non-throwing athletes. Arthroscopy. 2005;21:177.e1.
40 Tullos H.S., Erwin W.D., Woods G.W., Wukasch D.C., Cooley D.A., King J.W. Unusual lesions of the pitching arm. Clin. Orthop. 1972;88:169.
41 Woodward A.H., Bianco A.J.Jr. Osteochondritis dissecans of the elbow. Clin. Orthop. 1975;110:35.