Orthopedics
All newborn babies should be examined for evidence of hip dysplasia, spinal dysraphism, and lower and upper extremity deformities. 1
Look at the extremities, and check for asymmetry or an abnormal appearance. Look at the baby when crying to determine if he or she moves all extremities. Gently examine the joints and their range of motion. Finally, stimulating the extremities should result in some kind of response, usually withdrawal. 2
4. A premature newborn infant receiving ventilator support in the NICU has decreased movement in the right lower extremity. What diagnostic tests may be appropriate?
Neonatal osteomyelitis or fracture need to be ruled out. Baseline laboratory testing should be considered (e.g., complete blood count and C-reactive protein) as part of the evaluation for possible joint infections, which are not uncommon in this setting. If an osteomyelitis is suspected, a blood culture should always be obtained. These tests may not be rewarding because infants may develop infection without abnormalities in laboratory values. Plain radiographs of the entire extremity should be obtained to help detect a subtle fracture that may not be apparent on clinical examination. Radiographs are often normal in the early phases of bone and joint infection. In this setting bone and joint infections most often involve more than one site. Therefore careful clinical assessment to detect subtle joint effusions or swelling over long bones is indicated. Often an ultrasound scan is helpful in confirming a joint effusion in the hip because overlying muscle may mask the usual clinical findings. A technetium-99 bone scan is very useful in detecting other sites of multicentric infection. 3
5. The initial evaluation of a first-born infant reveals multiple stiff joints in both the upper and lower extremities and thin, tapered, and “shiny” fingers. What is the main diagnostic consideration?
Arthrogryposis multiplex congenita is a clinical syndrome characterized by poor development of the joints in utero leading to multiple contractures. This does not appear to be a hereditary condition, and there is no increased risk in siblings of the same family. Many mothers report decreased fetal movement in utero. On clinical examination the limbs are usually symmetric. Joints may have either flexion or extension contractures. There is decreased active and passive motion of the affected joints. The normal skin creases are usually absent, and the skin is taut and glossy. Dimpling at the joints may be present. There is atrophy of the limbs. Often the hips are dislocated, and clubfoot (i.e., talipes equinovarus) or congenital vertical talus affects the feet. The upper extremities are usually internally rotated at the shoulder, with elbow flexion or extension contractures. There are often radial head dislocations. The forearms are pronated with adduction deformity of the thumbs. Delivery may be difficult as a consequence of the stiff elbow and knee joints. This may result in birth fractures of the humerus and the femur. General health is not affected by this syndrome, although patients often exhibit minor respiratory difficulties and failure to thrive as newborns. 4
7. A newborn infant is noted to have external rotation of the lower extremities at rest, with little spontaneous movement and bilateral foot deformities. What radiographs should be ordered?
Both spine and pelvis radiographs should be ordered. The abnormalities described can result from anomalies of the spine or the lower extremities. 5
8. A newborn child is suspected of having a genetic skeletal dysplasia. What is the most critical orthopedic radiographic examination?
The most important radiograph is the lateral cervical spine. More than 150 distinct osteochondrodysplasias have been identified. Each has distinctive features, but many also have similar radiographic findings. One of the most common is agenesis or hypoplasia of the upper cervical spine elements. This can lead to instability and places the child at great risk of spinal cord injury during ordinary handling. Detection of cervical instability is mandatory to allow proper stabilization and protection. 6
DDH is a maldevelopment of the hip joint characterized by a spectrum of pathology ranging from instability of the hip to irreducible dislocation. 7
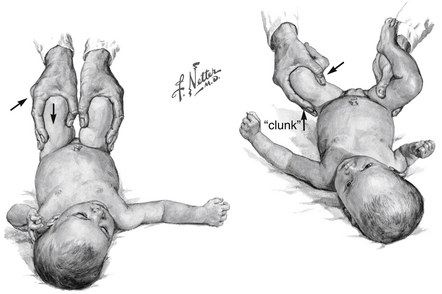
CDH is an outdated term; DDH is preferred because it reflects the evolutionary nature of hip problems in infants in the first months of life. The overt pathologic process may not be present at birth, and periodic examination of the infant’s hip is recommended at each routine well-baby visit until the age of 1 year ( Fig. 16-1). 8
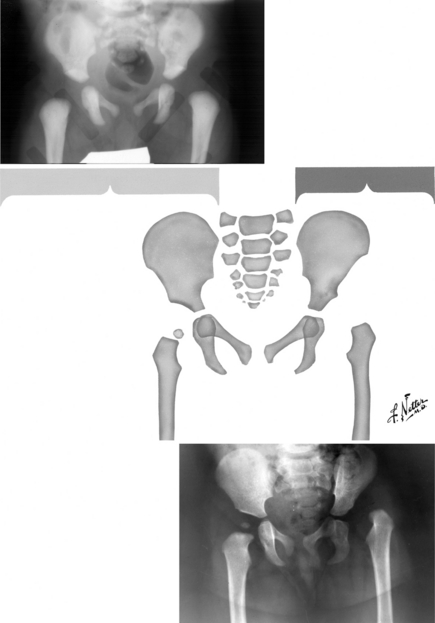
Figure 16-1 Congenital dislocation of the hip. (Netter illustration from www.netterimages.com. © Elsevier Inc. All rights reserved.)
The hip abduction, Ortolani, Barlow, and Galeazzi tests are recommended. 9
Infants should have symmetric hip abduction. Having asymmetry in hip abduction could be a sign of a dislocated hip. 10
13. How do you perform an Ortolani exam?
It is performed with the child in the supine position. Beginning with the hips flexed 90 degrees and adducted to the midline, the examiner places the index finger on the greater trochanter and the thumb on the inside of the thigh, then gently abducts the hip and lifts up on the greater trochanter. If the hip is dislocated and reducible, a palpable sensation will be felt as the hip reduces into the acetabulum (known as an Ortolani-positive hip) ( Fig. 16-2). 11
14. What does it mean to describe a hip as “Ortolani positive”?
The Ortolani examination is a reduction maneuver. Therefore an Ortolani-positive hip is a hip that is dislocated in its resting state and reducible with gentle manipulation. A simple way to remember this: Think of the O in Ortolani meaning that a hip is “out,” or dislocated, when you start the examination. 12
It is performed with the child supine on the examination table. The hip is flexed 90 degrees and adducted just beyond midline. Gentle downward pressure is then applied to the hip through the knee. The sensation of the femoral head sliding out of the acetabulum indicates a Barlow-positive hip. 13
The Barlow examination is a provocative maneuver. A Barlow-positive hip is normally reduced but can be subluxed. A normal hip will not subluxate and is Barlow negative. 14
It is performed with the child supine. The hips and knees are flexed such that the feet are lying flat on the table. The examiner then looks at the heights of the knees. If there is a difference, there may be a dislocated hip. 15
The Galeazzi exam identifies apparent or real shortening of the femur. It could be due to DDH or other congenital anomalies. 16
Ultrasound of the hip is the study of choice for suspected DDH in neonates and infants younger than four months of age. In children of this age the ossific nucleus of the femoral head is completely cartilaginous and therefore will not be seen on x-ray. After the infant is four months of age, radiographs should be obtained. 17
First-born female infants who present in the breech position and have a positive family history of DDH are at a significantly increased risk. A simple mnemonic: First, Female, Family, and Breech 18
Torticollis, congenital hyperextension of the knee, metatarsus adductus, and clubfoot are associated with DDH. 19
In a newborn child DDH can be very effectively treated with dynamic splinting in a brace, such as a Pavlik harness. A child in a Pavlik harness will lie with her hips and knees flexed approximately 90 degrees and her hips abducted to 60 degrees. This position is quite comfortable and natural for the infant. In this position the femoral head is deeply seated within the acetabulum. The soft-tissue structures around the hip will then stabilize with the hip in this reduced position. 20
Clubfoot, (also called talipes equinovarus), is a congenital condition in which the foot points downward and inward. More specifically, the hindfoot is in equinus and varus and the forefoot is in adduction and supination. 21
The incidence of clubfoot is 1.2 per 1000 live births, although this estimate varies with different ethnic subgroups, ranging from as high as 7 per 1000 in Hawaii to 0.87 in India. 22
Boys are affected nearly twice as often as girls, and 50% of the patients have bilateral involvement. 23
The etiology of clubfoot is unknown. It is seen in conjunction with cerebral palsy, myelomeningocele, arthrogryposis, and other neuromuscular conditions. Most often, however, it occurs as an isolated deformity in an otherwise healthy infant (i.e., it is idiopathic). 24
The initial treatment for clubfoot is weekly manipulation and casting according to the Ponseti method. Approximately 6 to 10 casts are required. A brace is worn for 3 to 4 years to maintain the correct position. With this technique, approximately 80% to 90% of idiopathic clubfeet will be successfully treated. Those feet that cannot be corrected with this method will require surgical correction ( Fig. 16-3). 25
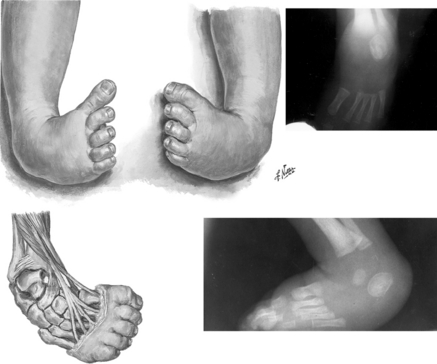
Figure 16-3 Corrective manipulation for clubfoot. (Netter illustration from www.netterimages.com. © Elsevier Inc. All rights reserved.)
As soon as the deformity is recognized, treatment should be started. This can frequently occur in the newborn nursery. 2627
A congenital condition characterized by the triad of a short neck, a low posterior hairline, and fusion of elements of the cervical spine. It results in decreased cervical spine motion. 2829
The cervical spine develops embryologically at the same time as the genitourinary and cardiovascular systems. As a result, patients with cervical spine anomalies may also have genitourinary and cardiovascular anomalies. In addition, other fusions and malformations of the spinal column may occur. There may also be abnormalities within the spinal cord, such as syringomyelia and cord tethering. 3031
These children must undergo an abdominal ultrasound scan to evaluate possible genitourinary anomalies. They should have a careful clinical cardiac examination. If the results of this examination are thought to be abnormal, an echocardiogram should be considered. Complete radiographs of the entire spinal column must be obtained to look for other vertebral anomalies. Finally, a thorough neurologic evaluation, including magnetic resonance imaging from the base of the brain to the cauda equina, should be performed. 32
The inability of the newborn to communicate makes this diagnosis quite difficult; however, there are some hallmark signs to be aware of. Affected children will appear lethargic and irritable. They will have difficulty feeding and will exhibit pseudoparalysis, or decreased movement, of the affected limb. A fever is not obligatory. The diagnosis is made by joint aspiration and microscopic examination of the fluid. 33
Bacteria within the joint will lead to an inflammatory response by the host immune system. The enzymes released (e.g., collagenases, proteases, elastases) by both the leukocytes and bacterial cells cause cartilage damage. Initially, glycosaminoglycans are removed from the cartilage. Over time, there is eventual collagen destruction. This damage is irreversible. In addition, if sufficient pressure develops within the joint, blood flow to the epiphysis will be compromised and may lead to avascular necrosis. 34
Neonatal fractures generally heal more quickly than their counterparts in children or adults. Because of this, and because of the difficulty in casting neonates, some fractures that would be severely problematic in an adult are barely treated in a neonate. A clavicular fracture will heal within 3 weeks in a newborn infant, as opposed to 6 to 8 weeks in an adult, and does not need to be immobilized in most cases. Femoral fractures, common in premature infants with rickets, are usually well healed within 3 weeks, compared with the 6 to 10 weeks required in an older child or adult with this fracture. Femoral fractures usually are splinted or placed in a Pavlik harness to help healing, but not always if there is minimal displacement.
38. The foot of a newborn appears to be dorsiflexed such that the top of the foot lies directly against the anterior portion of the lower leg. What are the two diagnostic considerations, and how would you differentiate between the two?
40. A newborn exhibits swelling over the midshaft of the right clavicle. What are the two most common diagnostic considerations?
Birth fractures of the clavicle are extremely common but most often are accompanied by pseudoparalysis of the extremity (caused by “splinting” from pain) for at least 3 to 5 days. There is pain with passive movement. Radiographs show the fracture, which usually heals with a massive callus. In the absence of pain, the clinician must consider congenital pseudarthrosis of the clavicle. The pseudarthrosis is fully present at birth. There is no history of birth injury or other trauma. The right clavicle is almost always affected. At the pseudarthrosis, the clavicular ends are enlarged, and there is painless motion between the two fragments. The etiology remains unknown, but several theories have been proposed, including exaggerated arterial pulsations and pressure on the clavicle by the subclavian artery that is normally more cranial on the right side. In bilateral cases it is thought that an abnormally high subclavian artery is present on both sides. With growth the deformity increases, and the overlying skin becomes thin and atrophic. The affected shoulder often droops, and there is asymmetry between the two shoulders. No functional impairment is noted. Treatment involves resection of the nonunion and internal fixation with bone grafting.
1Blasco PA. Pathology of cerebral palsy. In: Sussman MD, editor. The diplegic child. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1992. p. 3–20.
2Blasco PA. Pathology of cerebral palsy. In: Sussman MD, editor. The diplegic child. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1992. p. 3–20.
3Shaw BA, Kasser JR. Acute septic arthritis in infancy and childhood. Clin Orthop Relat Res 1990;257:212–25.
4Einhorn T. Orthopaedic Basic Science, Rosemont, IL: American Academy of Orthopaedic Surgery, 2006.
Morrissy R, Weinstein S, editors. Lovell and Winter’s Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 293–296.
5Einhorn T. Orthopaedic Basic Science, Rosemont, IL: American Academy of Orthopaedic Surgery, 2006.
Morrissy R, Weinstein S, editors. Lovell and Winter’s Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 293–296.
6Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
7Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
8Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
9Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
10Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
11Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
12Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
13Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
14Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–242.
15Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
16Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
17Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
18Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
19Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg 2000;8:232–42.
20Roye BD, Hyman JE, Roye DP Jr. Congenital idiopathic talipes equinovarus. Pediatr Rev 2004;25:124–30.
21Roye BD, Hyman JE, Roye DP Jr. Congenital idiopathic talipes equinovarus. Pediatr Rev 2004;25:124–30.
22Roye BD, Hyman JE, Roye DP Jr. Congenital idiopathic talipes equinovarus. Pediatr Rev 2004;25:124–130.
23Roye BD, Hyman JE, Roye DP Jr. Congenital idiopathic talipes equinovarus. Pediatr Rev 2004;25:124–30.
24Roye BD, Hyman JE, Roye DP Jr. Congenital idiopathic talipes equinovarus. Pediatr Rev 2004;25:124–30.
25Roye BD, Hyman JE, Roye DP Jr. Congenital idiopathic talipes equinovarus. Pediatr Rev 2004;25:124–130.
26Hyman JE, Roye DP Jr. Torticollis. In: Burg FD, Ingelfinger JR, Polin RA, Gershon AA, editors. Gellis and Kagan’s current pediatric therapy. Philadelphia: Saunders; 2002. p. 849–50.
27Einhorn T. Orthopaedic Basic Science, Rosemont, IL: American Academy of Orthopaedic Surgery, 2006.
Morrissy R, Weinstein S, editors. Lovell and Winter’s Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 332.
28Hyman JE, Roye DP Jr. Torticollis. In: Burg FD, Ingelfinger JR, Polin RA, Gershon AA, editors. Gellis and Kagan’s current pediatric therapy. Philadelphia: Saunders; 2002. p. 849–50.
29Einhorn T. Orthopaedic Basic Science, Rosemont, IL: American Academy of Orthopaedic Surgery, 2006.
Morrissy R, Weinstein S, editors. Lovell and Winter’s Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 889–891.
30Hyman JE, Roye DP Jr. Torticollis. In: Burg FD, Ingelfinger JR, Polin RA, Gershon AA, editors. Gellis and Kagan’s current pediatric therapy. Philadelphia: Saunders; 2002. p. 849–50.
31Einhorn T. Orthopaedic Basic Science, Rosemont, IL: American Academy of Orthopaedic Surgery, 2006.
Morrissy R, Weinstein S, editors. Lovell and Winter’s Pediatric Orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 889–891.
32Shaw BA, Kasser JR. Acute septic arthritis in infancy and childhood. Clin Orthop Relat Res 1990;257:212–225.
33Shaw BA, Kasser JR. Acute septic arthritis in infancy and childhood. Clin Orthop Relat Res 1990;257:212–25.
34Shaw BA, Kasser JR. Acute septic arthritis in infancy and childhood. Clin Orthop Relat Res 1990;257:212–25.