Chapter 11 Orbital Blood Supply
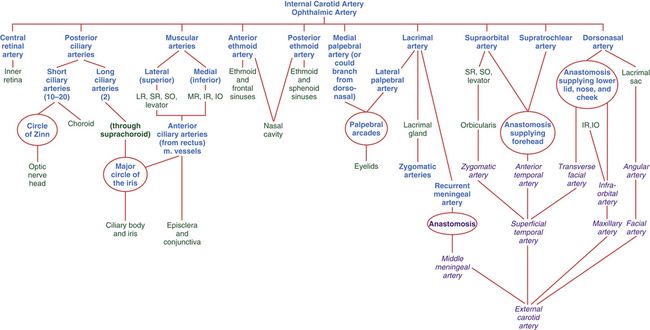
Internal Carotid Artery
The internal carotid artery runs upward through the neck and enters the skull through the carotid canal, located in the petrous portion of the temporal bone just superior to the jugular fossa. Within the anterior portion of the canal, only thin bone separates the artery from the cochlea and the trigeminal ganglion. The internal carotid artery leaves the canal and immediately enters the cavernous sinus, where it runs forward along the medial wall beside the sphenoid bone; it then exits through the roof of the sinus. Within the sinus, the abducens nerve is closely adherent to the lateral border of the internal carotid.1 Throughout its pathway—up the neck, into the skull, and through the cavernous sinus—the internal carotid is surrounded by a plexus of sympathetic nerves from the superior cervical ganglion. The second and third cranial nerves accompany the vessel as it leaves the sinus; the optic nerve lies medial and the oculomotor nerve lies lateral to the internal carotid. The ophthalmic artery branches from the internal carotid artery just as it emerges from the cavernous sinus medial to the anterior clinoid process of the sphenoid bone. It is usually the first major branch from the internal carotid artery.2
Clinical Comment: Sclerosis of the Internal Carotid Artery
Compression of the optic nerve caused by sclerosis of the internal carotid artery was found in some postmortem studies, with pathologic changes such as atrophy, evident in the optic nerve. Visual field defects may be caused by this compression and should be one of the differential diagnoses when optic nerve head atrophy accompanies a field defect.3
Ophthalmic Artery
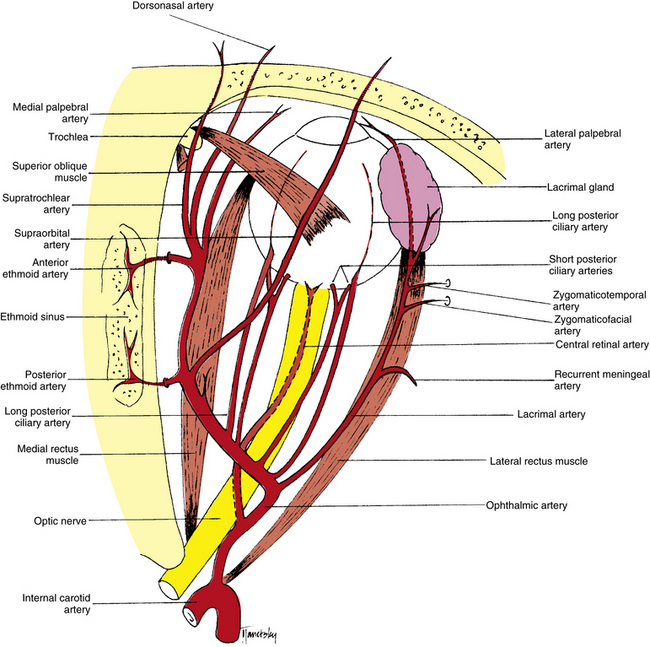
The ophthalmic artery enters the orbit within the dural sheath of the optic nerve and passes through the optic canal, below and lateral to the nerve2 (Figure 11-1). A network of sympathetic nerves surrounds the vessel.4 Once in the orbit the ophthalmic artery emerges from the meningeal sheath, runs inferolateral to the optic nerve for a short distance, and then crosses either above or below the nerve. Together with the nasociliary nerve, the ophthalmic artery runs toward the medial wall of the orbit.5 The artery continues forward between the medial rectus and superior oblique muscles, giving off branches to various areas. Just posterior to the superior medial orbital margin, it divides into its terminal branches, the supratrochlear and dorsonasal arteries. In general, the intraorbital arteries are located in the adipose compartments and perforate the connective tissue septa as they pass between sections.6 The ophthalmic artery is the main blood supply to the globe and adnexa but is supplemented by a few branches from the external carotid supply.
Marked variability is evident in the order of the origin of the branches of the ophthalmic artery, and the sequence appears to correlate with whether the artery crosses above or below the optic nerve. The most common patterns of distribution are shown in Table 11-1.7 Many anatomic variations can occur in the branches and their courses; those most often reported are included here.
| Order of Origin | SEQUENCE OF BRANCHES WHEN OPHTHALMIC ARTERY: | |
|---|---|---|
| Crosses Above Optic Nerve | Crosses Below Optic Nerve | |
| 1 | Central retinal and medial posterior ciliary | Lateral posterior ciliary |
| 2 | Lateral posterior ciliary | Central retinal |
| 3 | Lacrimal | Medial muscular |
| 4 | Muscular to superior rectus and levator | Medial posterior ciliary |
| 5 | Posterior ethmoid and supraorbital, jointly or separately | Lacrimal |
| 6 | Medial posterior ciliary | Muscular to superior rectus and levator |
| 7 | Medial muscular | Posterior ethmoid and supraorbital, jointly or separately |
| 8 | Muscular to superior oblique and medial rectus, jointly or separately | Muscular to superior oblique and medial rectus, jointly or separately |
| 9 | To areolar tissue | Anterior ethmoid |
| 10 | Anterior ethmoid | To areolar tissue |
| 11 | Medial palpebral or inferior medial palpebral | Medial palpebral or inferior medial palpebral |
| 12 | Superior medial palpebral | Superior medial palpebral |
| Terminal | Dorsonasal and supratrochlear | Dorsonasal and supratrochlear |
Modified from Hayreh SS: The ophthalmic artery. III. Branches, Br J Ophthalmol 46:212, 1962.
Central Retinal Artery
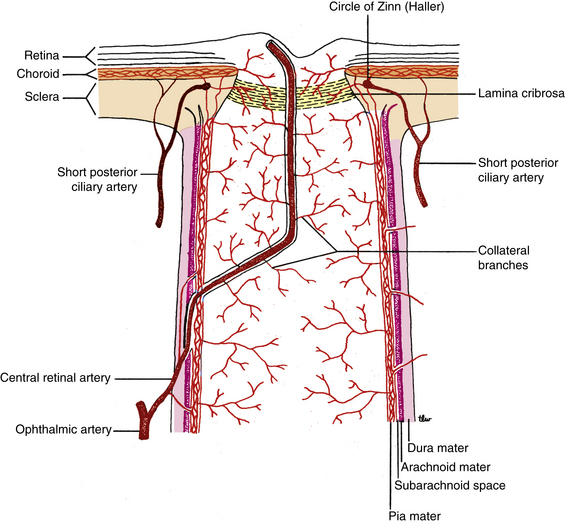
One of the first branches of the ophthalmic artery, the central retinal artery, is among the smallest branches. The central retinal artery leaves the ophthalmic artery as it lies below the optic nerve (see Figure 11-1). The artery runs forward a short distance before entering the meningeal sheath of the nerve about 10 to 12 mm behind the globe (Figure 11-2). While within the optic nerve, the central retinal artery provides branches to the nerve and pia mater.7 (Often, these branches are called collateral branches.) As the central retinal artery runs forward within the optic nerve, a sympathetic nerve plexus (the nerve of Tiedemann) surrounds the artery.8 The central retinal artery passes through the lamina cribrosa and enters the optic disc just nasal to center, branching superiorly and inferiorly. These branches divide into nasal and temporal branches, then continue to branch dichotomously within the retinal nerve fiber layer. The retinal blood vessels are discussed in Chapter 4.
Lacrimal Artery
One of the largest branches, the lacrimal artery, leaves the ophthalmic artery just after it enters the orbit (see Figure 11-1); rarely, it branches before the ophthalmic artery enters the optic canal.9 The lacrimal artery and the lacrimal nerve run forward along the upper border of the lateral rectus muscle. Within the orbit the lacrimal artery may supply branches to the lateral rectus muscle.
A recurrent meningeal artery (see Figure 11-1) might branch from the lacrimal artery and course back, leaving the orbit through the lateral aspect of the superior orbital fissure and then forming an anastomosis with the middle meningeal artery, a branch from the external carotid artery circulation.10 Other branches, the zygomaticotemporal artery and the zygomaticofacial artery, exit the orbit through foramina of the same name within the zygomatic bone (see Figure 11-1) and anastomose with branches from the external carotid in the temporal fossa and on the face.7
Posterior Ciliary Arteries
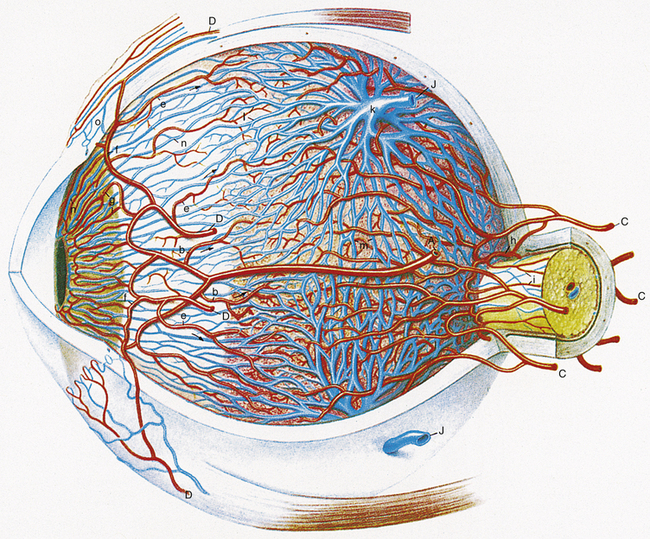
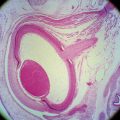
The posterior ciliary arteries are branches of the ophthalmic artery, and much variation can occur in their distribution.11 The short posterior ciliary arteries arise as 1, 2, or 3 branches that then form 10 to 20 branches. They enter the sclera in a ring around the optic nerve and form the arterial network within the choroidal stroma (Figure 11-3). Other branches from the short posterior ciliary arteries anastomose to form the circle of Zinn (Zinn-Haller) (see Figure 11-2), which encircles the optic nerve at the level of the choroid.12,13 The most superficial nerve fibers that occupy the surface of the optic disc are supplied by capillaries from the retinal vasculature with no apparent direct choroidal supply.13–15 The peripapillary network, formed by branches from the short posterior ciliary arteries and from the circle of Zinn, supplies the remaining prelaminar region of the optic nerve.14–17 These vessels do not anastomose with the peripapillary choriocapillaris.14 The laminar region is supplied by the short posterior ciliary arteries either directly or as branches from the circle of Zinn.14–18

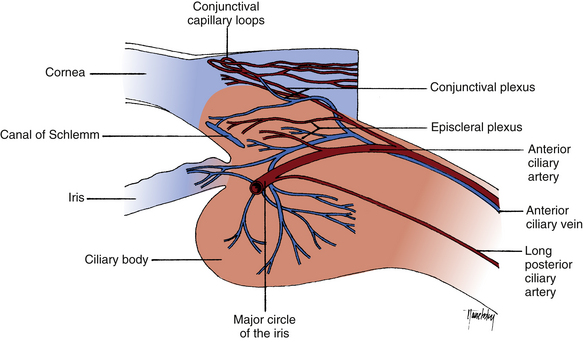
FIGURE 11-3 Uveal blood vessels.
(From Hogan MJ, Alvarado JA, Weddell JE: Histology of the human eye, Philadelphia, 1971, Saunders.)
Clinical Comment: Anterior Ischemic Optic Neuropathy
ANTERIOR ISCHEMIC OPTIC NEUROPATHY (AION) results from nonperfusion or hypoperfusion of the ciliary blood supply to the optic nerve head.14 The oval that forms the circle of Zinn can be divided into superior and inferior portions by the entry points of the medial and lateral short ciliary arteries forming it. This may be the anatomic basis for the altitudinal visual field loss that characterizes nonarteritic AION. The inferior field is more often affected, but there is no adequate explanation for the preferential involvement of the superior part of the ring of vessels.19
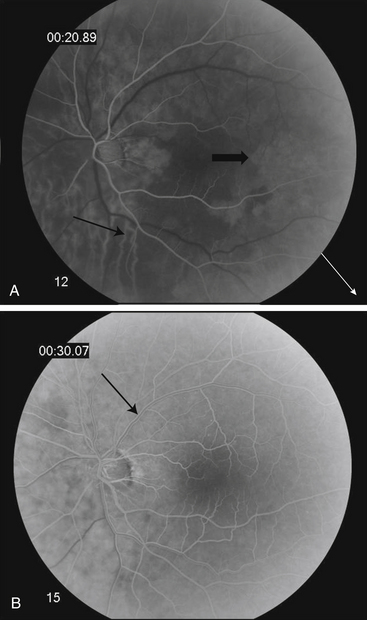
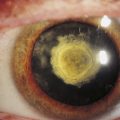
Clinical Comment: Cilioretinal Artery
A CILIORETINAL ARTERY may arise either from the vessels entering the choroid or from the circle of Zinn; thus this vessel, located within the retina, arises from the ciliary circulation and not from the retinal supply. Various studies report a cilioretinal artery occurring in 15% to 50% of the population and usually entering the retina from the temporal side of the optic disc to supply the macular area20,21 (Figure 11-4). If occlusion of the central retinal artery occurs, the direct blood supply to the macular area will be maintained in those individuals with such a cilioretinal artery.
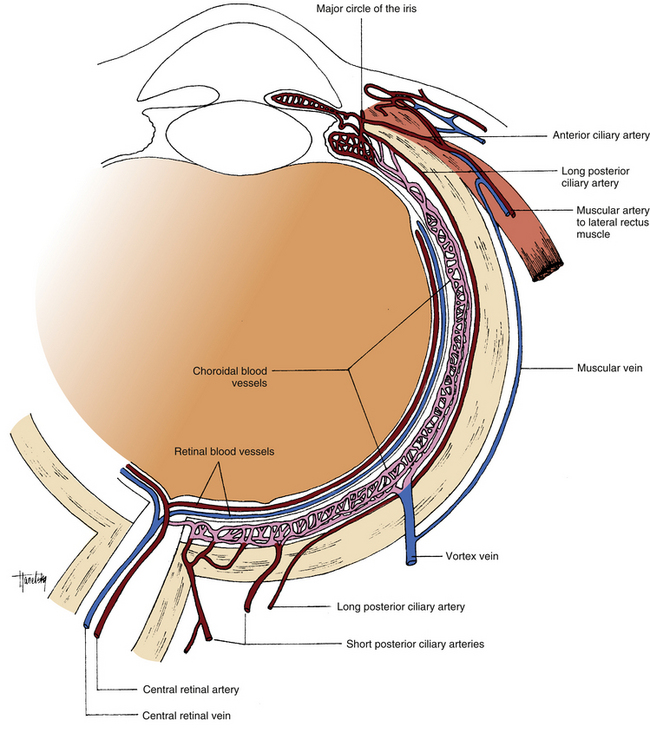
Two long branches of the posterior ciliary arteries enter the sclera: one lateral and one medial to the ring of short ciliary arteries. These are the long posterior ciliary arteries, which run between the sclera and the choroid to the anterior globe (Figure 11-5). Here the arteries enter the ciliary body and branch superiorly and inferiorly.14 These branches anastomose with each other and with the anterior ciliary arteries to form a circular blood vessel, the major arterial circle of the iris (Figure 11-6). This circular artery is located in the ciliary stroma near the iris root and is the source of the radial vessels found in the iris. Before forming the major circle, branches from the long posterior ciliary arteries supply the ciliary body and the anterior choroid, where they form a network that anastomoses with the choroidal vessels from the short posterior ciliary arteries (see Figure 11-3).
Clinical Comment: Fluorescein Angiography
Sodium fluorescein dye can be injected into the systemic circulation to examine the choroidal and retinal circulation for abnormalities (Figure 11-7). Two to five cc of the dye is injected into a vein in the arm. Serial black and white photos are taken of the fundus through filters that enhance the image. This documents the movement of the blood through the choroidal and retinal vasculature. The dye enters the skull through the internal carotid artery, passes into the ophthalmic artery, and then to the posterior ciliary arteries, which fill before the central retinal artery. Within 10 seconds of injection the choroidal flush can be seen; the dye can leak out of the fenestrated choriocapillaris easily but should not seep into the retina because of the blood-retinal barrier of zonula occludens in the RPE. Ten to 12 seconds after injection, the retinal arterioles fill and the capillaries are filled in the next second; another 1 to 2 seconds and the veins fill, and the dye starts to exit the ocular tissue. Defects in the RPE can be seen if the dye leaks into the retina before the retinal vessels fill. Abnormal retinal vasculature such as neovascularization and capillary leakage will be evident.
Ethmoid Arteries
As the ophthalmic artery courses near the medial wall, two branches arise and enter the ethmoid bone (see Figure 11-1). The posterior ethmoid artery passes through the posterior ethmoid canal to supply the posterior ethmoid sinus and the sphenoid sinus; it sends branches into the nasal cavity to supply the upper part of the nasal mucosa. The anterior ethmoid artery generally is larger and passes through the anterior ethmoid canal and supplies the anterior and middle ethmoid sinuses, the sphenoid sinus, the frontal sinus, the nasal cavity, and the skin of the nose.
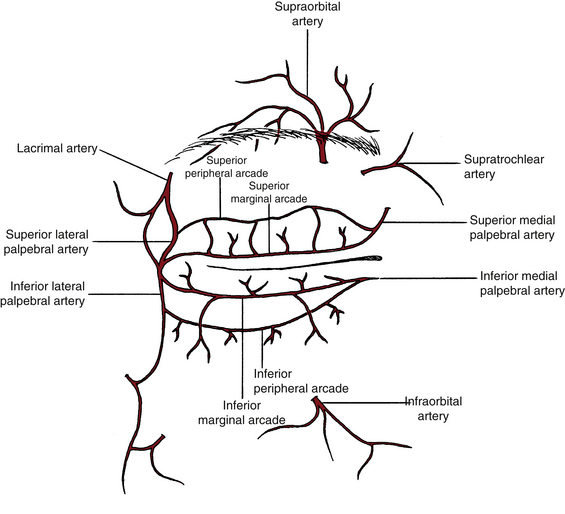
Supraorbital Artery
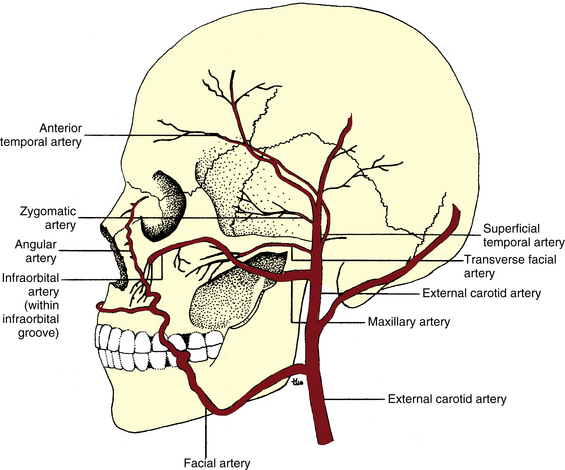
The supraorbital artery arises from the ophthalmic artery as it lies medial to the optic nerve (see Figure 11-1). The supraorbital artery runs upward to a position above the superior extraocular muscles, turns anteriorly, and runs with the supraorbital nerve between the periorbita of the orbital roof and the levator muscle. It passes through the supraorbital notch or foramen, often dividing into two branches to supply the skin and the muscles of the forehead and scalp (see Figure 11-8). Terminal branches anastomose with the artery from the opposite side, with the supratrochlear artery, and with the anterior temporal artery from the external carotid. While the supraorbital artery is in the orbit, it sends branches to the superior rectus, superior oblique, and levator muscles and to the periorbita.
Muscular Arteries
Much variation occurs in the vessels supplying the muscles, and in an individual, any combination of the vessels named here might be present. In one common presentation, the muscular arteries come from the ophthalmic artery as two branches, the lateral (or superior) and the medial (or inferior). The lateral (superior) branch supplies the lateral rectus, superior rectus, superior oblique, and levator muscles.7–9 The medial (inferior) branch supplies the medial rectus, inferior rectus, and inferior oblique muscles.7–9 Additional branches supplying the muscles may come from other sources. The lacrimal artery supplies the lateral and superior rectus muscles. The supraorbital artery supplies the superior rectus, superior oblique, and levator muscles. The infraorbital artery supplies the inferior rectus and inferior oblique muscles (Table 11-2).
| Muscle | Arterial Supply |
|---|---|
| Medial rectus | Medial (inferior) muscular |
| Lateral rectus | Lateral (superior) muscular Lacrimal |
| Superior rectus | Lateral (superior) muscular Lacrimal Supraorbital |
| Inferior rectus | Medial (inferior) muscular Infraorbital |
| Superior oblique | Lateral (superior) muscular Supraorbital |
| Inferior oblique | Medial (inferior) muscular Infraorbital |
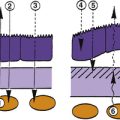
Anterior Ciliary Arteries
The anterior ciliary arteries branch from the vessels supplying the rectus muscles. These arteries exit the muscles near the muscle insertions, run forward along the tendons a short distance, then loop inward to pierce the sclera just outer to the limbus (see Figure 11-3). An accumulation of pigment may be evident at the point at which the artery enters the sclera. Before entering the sclera, the anterior ciliary arteries send branches into the conjunctiva, forming a network of vessels in the limbal conjunctiva (see Figure 11-6). Other branches enter the episclera to form a network of vessels before entering the uvea. The anterior ciliary arteries then enter the ciliary body and anastomose with the branches of the long posterior ciliary arteries, forming the major circle of the iris (see Figure 11-3). Generally, two anterior ciliary arteries emanate from each of the rectus muscles, with the exception of the lateral rectus, which provides only one such artery.
Clinical Comment: “Red Eye”
Inflammations generate an increase of the blood flow to the affected area, causing hyperemia. In cases of a “red eye,” an understanding of the organization of the blood supply in the limbal area can help in differentiating a less serious presentation, such as conjunctivitis, from a more serious situation, such as uveitis. In conjunctivitis and mild corneal involvement, the superficial blood vessels are injected, giving the conjunctiva a bright-red color that often increases toward the fornix. The vessels move with conjunctival movement and can be blanched with a topical vasoconstrictor. In uveitis the deeper scleral and episcleral vessels are injected, giving the circumlimbal area a purplish or rose-pink color.22 These vessels do not move with the conjunctiva and are not blanched with a topical vasoconstrictor.
Medial Palpebral Arteries
Two medial palpebral arteries branch either directly from the ophthalmic artery or from the dorsonasal artery near the trochlea of the superior oblique muscle. The medial palpebral arteries pierce the orbital septum on either side of the medial palpebral ligament and enter the superior and inferior eyelids (see Figure 11-8). These branches run through the eyelid and form arches between the orbicularis muscle and the tarsal plate. They anastomose with branches from the lacrimal artery and form the vessels known as the palpebral arcades. Usually, two arcades occur in each lid: the marginal arcade, which runs near the marginal edge of the tarsal plate, and the peripheral arcade, which runs near the peripheral edge of the tarsal plate. These provide the blood supply for the eyelid structures. Additional branches from the medial palpebral arteries supply the structures in the medial canthus.
Supratrochlear Artery
One of the terminal branches of the ophthalmic artery, the supratrochlear artery, pierces the orbital septum at the superior, medial corner of the orbit5 (see Figure 11-8). It passes with the supratrochlear nerve upward to supply the skin of the forehead and scalp and the muscles of the forehead. The supratrochlear artery forms anastomoses with the supraorbital artery, the opposite supratrochlear artery, and the anterior temporal artery of the external carotid supply.
Dorsonasal Artery
The other terminal branch of the ophthalmic artery, the dorsonasal artery (dorsal nasal artery), also leaves the orbit by piercing the orbital septum below the trochlea above the medial palpebral ligament.5 It sends vessels to supply the lacrimal sac, then runs alongside the nose to anastomose with the angular artery from the external carotid supply.
Physiology of Ocular Circulation
The endothelial cells that line blood vessels secrete substances that modulate vascular tone and vessel caliber. Blood flow is strongly dependent on endothelial-derived vasoactive substances such as nitric oxide, which causes vasodilation and endothelin-1, a vasoconstrictor.23,24 The choroidal blood flow is largely dependent on vasoactive autonomic innervation, and sympathetic stimulation causes vasoconstriction but the effect of parasympathetic stimulation is less clear.23 Retinal vessels lack autonomic innervation and are autoregulated, and blood flow remains stable with transient increases in blood pressure.23 Retinal vessel walls have “pacemaker” mechanisms that regulate vessel wall tension, constriction and dilation, are influenced by changes in the environment in the surrounding tissue, responding to levels of O2 and CO2, as well as pH changes. Some investigators believe that choroidal vessels exhibit some autoregulation.25
Although blood flow through the choroidal vessels is extremely high compared with flow through retinal vessels (2000 ml/min/100 g tissue versus 60 ml/min/100 g tissue), oxygen extraction from the choriocapillaris is low.24 The high choroidal flow rate provides high oxygen tension enhancing oxygen diffusion through Bruch’s membrane and the RPE to mitochondria in the photoreceptor inner segment. The high choroidal blood flow can also act to stabilize temperature, protecting the retina from thermal damage.24,25
External Carotid Artery
Facial Artery
The facial artery arises from the external carotid near the angle of the mandible, runs along the posterior edge of the lower jaw, and curves upward over the outside of the jaw and across the cheek to the angle of the mouth. It ascends along the side of the nose and sends a terminal branch, the angular artery, to the medial canthus (Figure 11-9). The angular artery supplies the lacrimal sac, the medial part of the lower lid, and the skin of the cheek. Some branches pass beneath the medial canthal ligament to anastomose with the infraorbital artery, and some anastomose with the dorsonasal artery.
Superficial Temporal Artery
The superficial temporal artery is a terminal branch of the external carotid artery (see Figure 11-9). Branches of the superficial temporal artery that supply areas near the orbit are the anterior temporal, zygomatic, and transverse facial arteries.26 The anterior temporal artery supplies the skin and muscles of the forehead and anastomoses with the supraorbital and supratrochlear arteries. The zygomatic artery extends above the zygomatic arch and supplies the orbicularis muscle. The transverse facial artery supplies the skin of the cheek and anastomoses with the infraorbital artery.
Clinical Comment: Temporal Arteritis
TEMPORAL ARTERITIS (or giant cell arteritis) is an inflammatory condition that can affect large arteries but is found primarily in the arteries in the temporal or occipital region. The disease often is accompanied by swelling, redness, and tenderness in the temporal area. Ocular symptoms, including vision loss, may occur. Biopsy of the superficial temporal artery often is necessary to confirm the diagnosis before treatment begins.29 The biopsy is taken from the artery as it crosses the zygomatic process and travels superiorly anterior to the ear.28
Maxillary Artery
The other branch of the external carotid that supplies areas in proximity to the orbit is the maxillary artery. It passes through the infratemporal fossa and then upward, medial to the mandibular joint toward the maxillary bone (see Figure 11-9). Within the infratemporal fossa, the maxillary artery shows some variability in both its branching pattern and in its topographic relations with other structures.29–31 It runs along the pterygopalatine fossa and enters the orbit through the inferior orbital fissure as the infraorbital artery. The artery then runs forward along the infraorbital groove in the maxillary bone, passes through the infraorbital canal, and exits through the infraorbital foramen (see Figure 11-8). It supplies the lower eyelid and lacrimal sac, and it anastomoses with the angular artery and the dorsonasal artery.26 While in the infraorbital canal, the infraorbital artery supplies the inferior rectus and inferior oblique muscles and sends some branches to the maxillary sinus and to the teeth of the upper jaw. The branches from the internal and external carotid arteries that supply the ocular structures, as well as their most common anastomoses, are shown in the flow chart in Figure 11-10.
Veins of the Orbit
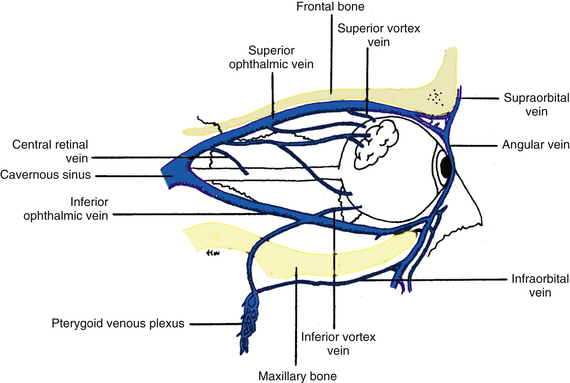
The veins of the orbit have no valves; thus the direction of blood flow may change and is determined by pressure gradients.5 Over a large part of their path, the veins are embedded within the connective tissue septa that compartmentalize the orbit.5 Unlike the parallel routes of veins and arteries in most of the body, many orbital veins follow a course that differs from the corresponding arteries.9,32 The orbit has a single ophthalmic artery but two ophthalmic veins. The superior and inferior ophthalmic veins primarily drain into the cavernous sinus.
Superior Ophthalmic Vein
The superior ophthalmic vein is formed by the joining of the angular and supraorbital veins within the orbit (Figure 11-11). The supraorbital vein enters the orbit through the supraorbital notch, and the angular vein passes through the orbital septum above the medial palpebral ligament.33
The veins that drain into the superior ophthalmic vein are the anterior and posterior ethmoid veins, the muscular veins draining the superior and medial muscles, the lacrimal vein, the central retinal vein, and the superior vortex veins.33
Central Retinal Vein
Clinical Comment: Spontaneous Venous Pulsation
The pressure within the central retinal vein is approximately equal to the intraocular pressure (IOP) and at peak pulse pressure the vessel walls expand slightly. The increase in blood volume can be seen during ophthalmoscopy of the healthy eye as the central retinal vein can be seen to pulsate at its exit through the optic disc. The IOP can vary slightly (1 to 2 mm Hg) with this change in blood volume.24
Clinical Comment: Papilledema
The sheaths that surround the optic nerve are continuous with the meningeal sheaths of the brain. The subarachnoid space, located within these layers, contains cerebrospinal fluid. Thus the fluid that surrounds the optic nerve is continuous with the fluid found throughout the cranial cavity. With increased intracranial pressure, the central retinal vein can be compressed as it crosses the subarachnoid space on its exit from the optic nerve. The central retinal artery is not affected because it has a thicker sheath and is not compressed as easily as is the vein.34 The resultant blockage causes congestion of the retinal veins and edema of the retina. Edema of the optic nerve head (papilledema) will be evident as blurred disc margins, with hemorrhages sometimes evident as well.
Vortex Veins
The vortex veins drain the choroid, and usually one of the four or five vortex veins is located in each quadrant (see Figure 11-3). These veins exit the globe 6 mm posterior to the equator.8 The vortex veins can be seen with an indirect ophthalmoscope and a dilated pupil.
Inferior Ophthalmic Vein
The inferior ophthalmic vein begins as a plexus near the anterior floor of the orbit. It drains blood from the lower and lateral muscles, the inferior conjunctiva, the lacrimal sac, and the inferior vortex veins.33 It may form two branches: one that empties into either the superior ophthalmic vein22,35 or the cavernous sinus and one that empties into the pterygoid venous plexus (see Figure 11-11). The latter branch exits the orbit through the inferior orbital fissure, and the other branch passes through the superior orbital fissure either to join the superior ophthalmic vein or to empty directly into the cavernous sinus.
Infraorbital Vein
The infraorbital vein is formed by several veins that drain the face. It enters the infraorbital foramen and, along with the infraorbital artery and nerve, passes posteriorly through the infraorbital canal and groove. It receives branches from some structures in the inferior part of the orbit and may communicate with the inferior ophthalmic vein. The infraorbital vein drains into the pterygoid venous plexus (see Figure 11-11).
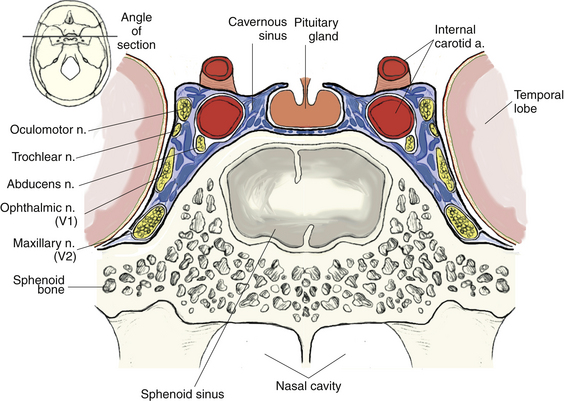
Cavernous Sinus
The cavernous sinus is a relatively large venous channel formed by a splitting of the dura mater on each side of the body of the sphenoid bone. The cavernous sinus extends from the medial end of the superior orbital fissure to the petrous portion of the temporal bone. The internal carotid artery and the abducens nerve are located medially within the sinus, covered by the endothelial lining of the sinus. The oculomotor, ophthalmic, and maxillary nerves are found in the lateral wall of the cavernous sinus (Figure 11-12). The cavernous sinus drains into the superior petrosal sinus, located along the upper crest of the petrous portion of the temporal bone, and into the inferior petrosal sinus, located in the groove between the petrous portion and the occipital bone. Both drain either directly or indirectly into the internal jugular vein (Figure 11-13).
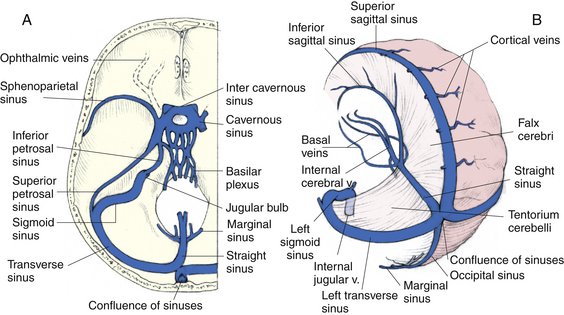
FIGURE 11-13 Superior view of venous sinus drainage of cranium.
(From Mathers LH, Chase RA, Dolph J, et al: Clinical anatomy principles, St Louis, 1996, Mosby.)
Clinical Comment: Carotid-Cavernous Sinus Fistula
A CAROTID-CAVERNOUS SINUS FISTULA is an abnormal communication between the internal carotid artery and the cavernous sinus caused by a tear in the artery wall, either traumatic or spontaneous. The sinus communicates directly with the veins of the orbit, so arterial pressure can be transmitted to the ophthalmic veins, which may become pulsatile. If arterial pressure is reduced because of this leak, a decrease in perfusion to ocular tissue will occur.36,37
Lymphatic Drainage
No lymphatic vessels occur in the globe proper; lymphatics are found in the conjunctiva and the eyelids. The lymphatics that drain the medial aspects of the lids and the medial canthal structures (including the lacrimal sac) empty into the submandibular lymph nodes. Those that drain the lateral eyelids and the lacrimal gland empty into the parotid lymph nodes in the preauricular area9,35 (Figure 11-14).
Effect of Aging on Ocular Circulation
Changes occurring with age differ between individuals. Genetic and environmental factors are contributory, but there are some generalities that can be made. The density of the choroidal and retinal capillary beds and choroidal and retinal vessel diameter all decrease with age.38 Endothelial dysfunction can occur with age and can result in increased vascular tone, a reduction in vessel distensibility, and a decrease in tissue perfusion.38 Because there is a coincident decrease in retinal cells, this decrease in blood flow may be a response to decreased metabolic need.39,40
1. Nuza A.B., Taner D. Anatomical variations of the intracavernous branches of the internal carotid artery with reference to the relationship of the internal carotid artery and sixth cranial nerve. Acta Anat (Basel). 1990;138(3):238.
2. Hayreh S.S., Dass R. The ophthalmic artery. I. Origin and intra-cranial and intra-canalicular course. Br J Ophthalmol. 1962;46:65.
3. Liu X.J. Pathological changes of the optic nerve from compression by the internal carotid artery. Chung Hua Yen Ko Tsa Chih. 1990;26(6):364. (abstract)
4. Erdogmus S., Govsa F. Anatomic characteristics of the ophthalmic and posterior ciliary arteries. J Neuroophthalmol. 2008;28:320-324.
5. Hayreh S.S. The ophthalmic artery. II. Intraorbital course. Br J Ophthalmol. 1962;46:165.
6. Koorneef L. Orbital connective tissue. In: Jakobiec F.A., editor. Ocular anatomy, embryology, and teratology. Philadelphia: Harper & Row; 1982:835.
7. Hayreh S.S. The ophthalmic artery. III. Branches. Br J Ophthalmol. 1962;46:212.
8. Warwick R. Eugene Wolff’s anatomy of the eye and orbit, ed 7. Philadelphia: Saunders; 1976. pp 92, 146, 406
9. Doxanas M.T., Anderson R.L. Clinical orbital anatomy. Baltimore: Williams & Wilkins; 1984. p 153
10. Diamond M.K. Homologies of the meningeal-orbital arteries of humans: a reappraisal. J Anat. 1991;178:223.
11. Yoshii I., Ikeda A. A new look at the blood supply of the retro-ocular space. Anat Rec. 1992;233:321.
12. Olver J.M. Functional anatomy of the choroidal circulation: methyl methacrylate casting of human choroid. Eye. 1990;4:262.
13. Onda E., Cioffi G.A., Bacon D.R., et al. Microvasculature of the human optic nerve. Am J Ophthalmol. 1995;120:92.
14. Hayreh S.S. The blood supply of the optic nerve head and the evaluation of it: myth and reality. Prog Retin Eye Res. 2001;20(5):563.
15. MacKenzie P.J., Cioffi G. Vascular anatomy of the optic nerve head. Can J Ophthalmol. 2008;43:308-312.
16. Hayreh S.S. Blood supply of the optic nerve head and its role in optic atrophy, glaucoma, and oedema of the optic disc. Br J Ophthalmol. 1969;53:721.
17. Hayreh S.S. Pathogenesis of cupping of the optic disc. Br J Ophthalmol. 1974;58:863.
18. Borchert M.S. Vascular anatomy of the visual system. Ophthalmol Clin North Am. 1996;9(3):327.
19. Olver J.M., Spalton D.J., McCartney A.C. Microvascular study of the retrolaminar optic nerve in man: the possible significance in anterior ischaemic optic neuropathy. Eye. 1990;4:7.
20. Hayreh S.S. The central artery of the retina: its role in the blood supply of the optic nerve. Br J Ophthalmol. 1963;47:651.
21. Justice J.Jr., Lehmann R.P. Cilioretinal arteries: a study based on a review of stereo fundus photographs and fluorescein angiographic findings. Arch Ophthalmol. 1976;94:1355.
22. Catania L.J. Primary care of the anterior segment. East Norwalk, Conn: Appleton & Lange; 1988. p 194
23. Brown S.M., Jampol L.M. New concepts of regulation of retinal vessel tone. Arch Ophthalmol. 1996;114:199-204.
24. Cioffi G.A. Granstam E Alm A: Ocular circulation. In Kaufman P.L., Alm A., editors: Adler’s physiology of the eye, ed 10, St Louis: Elsevier, 2003.
25. Kilgaar J.F., dJensen P.K. The choroid and optic nerve head. In: Fischbanrg J., editor. In The Biology of the eye, Amsterdam. Elsevier; 2006:273-290.
26. Tucker S.M., Lindberg J.V. Vascular anatomy of the eyelids. Ophthalmology. 1994;101:1118.
27. Berkow R., editor. The Merck manual, ed 14. Rahway, NJ: Merck; 1982:557.
28. Sires B.S., Gausas R., Cook B.E.Jr., et al. Orbit. In Kaufman P.L., Alm A., editors: Adler’s physiology of the eye, ed 10, St Louis: Elsevier, 2003.
29. Morton A.L., Khan A. Internal maxillary artery variability in the pterygopalatine fossa. Otolaryngol Head Neck Surg. 1991;104(2):204.
30. Ortug G., Moriggl B. The topography of the maxillary artery within the infratemporal fossa. Anat Anz. 1991;172(3):197. (abstract)
31. Pretterklieber M.L., Skopakoff C., Mayr R. The human maxillary artery reinvestigated: topographical relations in the infratemporal fossa. Acta Anat (Basel). 1991;142(4):281.
32. Murakami K., Murakami G., Komatsu A., et al. Gross anatomical study of veins in the orbit. Nippon Ganka Gakkai Zasshi. 1991;95(1):31. (abstract)
33. Cheung N., McNab A.A. Venous anatomy of the orbit. Invest Ophthalmol Vis Sci. 2003;44(3):988.
34. Whiting A.S., Johnson L.N. Papilledema: clinical clues and differential diagnosis. Am Fam Physician. 1992;45(3):125.
35. Wobig J.L. The blood vessels and lymphatics of the orbit and lid. In: Wobig J.L., Reeh M.J., Wirtschafter J.D., editors. Ophthalmic anatomy. San Francisco: American Academy of Ophthalmology; 1981:77.
36. De Keizer R. Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit. 2003;22(2):121.
37. Bhatti M.T., Peters K.R. A red eye and then a really red eye. Surv Ophthalmol. 2003;48(2):224.
38. Ehrlich R., Kheradiya N.S., Winston D.M., et al. Age-related ocular vascular changes. Graefes Arch Clin Exp Ophthalmol. 2009;247:583-591.
39. Grunwald J.E., Hariprasad S.M., DuPont J. Effect of aging on foveolar choroidal circulation. Arch Ophthalmol. 1998;116:150.
40. Lam A.K., Chan S., Chan H., et al. The effect of age on ocular blood supply determined by pulsatile ocular blood flow and color Doppler ultrasonography. Optom Vis Sci. 2003;89(4):305.