CHAPTER 33 Open Treatment for Hip Cartilage Injuries
Introduction
Cartilage injuries on the acetabulum are more common and typically present as localized cartilage delamination defects in the anterosuperior weight-bearing zone of the acetabular rim. The cause of these defects is most commonly femoroacetabular impingement, which will be discussed in chapter 28.
Surgical technique
Osteochondral Autograft Transfer
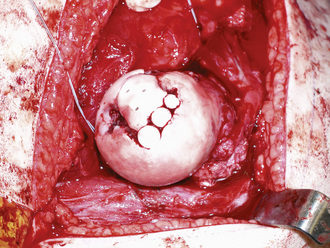
With the use of an osteochondral autograft transfer system (OATS, Arthrex, Inc., Naples, FL), a guidewire is drilled perpendicular to the central portion of the cartilage defect of the femoral head after a surgical hip dislocation has been performed as described by Ganz and colleagues (Figure 33-1). Next, an appropriately sized flat acorn reamer is carried down to the subchondral bone over the guidewire. A recipient punch guide with a diameter that is large enough to encompass the chondral defect in its entirety is selected and tapped down to the subchondral surface of the femoral head. The depth of the osteochondral plug is then measured.
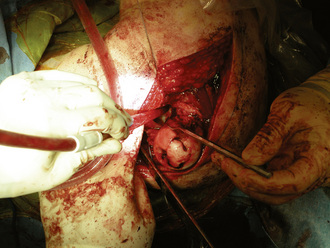
Figure 33–1 A focal chondral defect of the femoral head after a surgical hip dislocation has been performed.
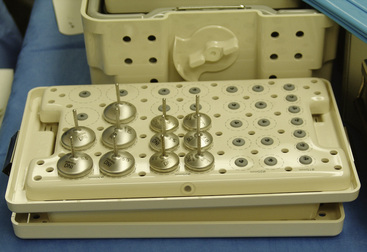
The donor site should be harvested from an area of less contact pressure. At our institution, for the treatment of focal chondral injuries of the femoral head, we have used the ipsilateral knee (i.e., the superolateral aspect of the lateral femoral condyle) as the donor site. With the use of a donor punch guide of the same diameter, the guide is malleted down to the same depth as the recipient plug, and the plug is removed. The donor osteochondral plug can be press fit into the recipient site and lightly impacted with a mallet until it is continuous with the surrounding articular cartilage of the femoral head (Figure 33-2). Multiple plugs may be necessary, depending on the size of the chondral defect (Figure 33-3).
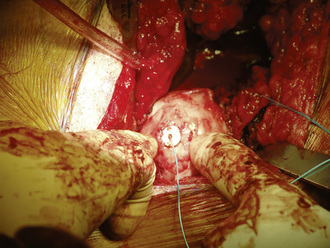
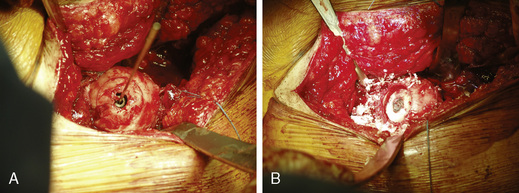
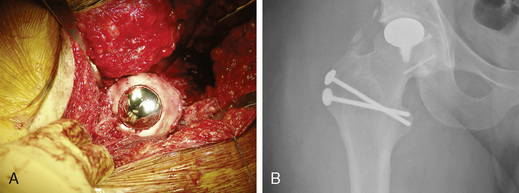
Arthrosurface HemiCAP
The Arthrosurface HemiCAP (Arthrosurface, Inc., Franklin, MA) was designed to treat articular surface defects with an implant that can match the surface and contour of the femoral head (Figure 33-4). The device consists of a titanium fixation screw and a cap-like implant made from a cobalt chrome alloy with a central post on its underside. A surgical hip dislocation is performed as previously described by Ganz and colleagues. The diameter of the defect is measured, and a guidewire is introduced into the middle of the defect (Figure 33-5). The fixation component is used as a central axis, and reamers are then used to map the contours of the patient’s articular cartilage defect (Figure 33-6, A and B). After the surface is prepared, the articular cap implant is seated into position (Figure 33-7, A and B).
Postoperative rehabilitation
Technical Pearls
Byrd J.W. Lateral impact injury. A source of occult hip pathology. Clin Sports Med.. 2001;20:801-815.
Byrd J.W., Jones K.S. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med.. 2004;32:1668-1672.
Ganze R., Gill T.J., Gautier E., et al. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg.. 2001;83B:1119-1124.
Gardner M.J., Suk M., Pearle A., Buly R.L., Helfet D.L., Lorich D.G. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma. 2005;19:334-342.
Lavigne M., Parvizi J., Beck M., Siebenrock K.A., Ganz R., Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res.. 2004;418:61-66.
This article reviews open surgical treatment options for cam and pincer impingement..
Shindle M.K., Foo L.F., Kelly B.T., et al. Magnetic resonance imaging of cartilage in the athlete: current techniques and spectrum of disease. J Bone Joint Surg Am.. 2006;88:27-46.
Shindle M.K., Ranawat A.S., Kelly B.T. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med.. 2006;25:309-326.
Siguier M., Judet T., Siguier T., Charnley G., Brumpt B., Yugue I. Preliminary results of partial surface replacement of the femoral head in osteonecrosis. J Arthroplasty. 1999;14:45-51.
Siguier T., Siguier M., Judet T., Charnley G., Brumpt B. Partial resurfacing arthroplasty of the femoral head in avascular necrosis. Methods, indications, and results. CORR. 2001;386:85-92.