Off-pump coronary artery bypass and minimally invasive direct coronary artery bypass
Definitions and indications
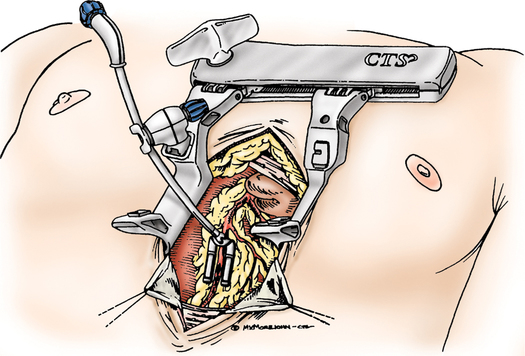
In both techniques, each diseased artery is identified and immobilized, often using a specialized stabilization device. Improved results and more reliable and reproducible coronary anastomoses are achieved when mechanical stabilization devices are used (Figure 145-1). The stenotic segments are bypassed without the use of CPB or the need for cardioplegia or hypothermia.
Anesthetic technique
Preparation and monitoring
Induction and maintenance
Induced bradycardia facilitates surgical success, especially with MIDCAB. Besides optimizing the surgical field, bradycardia reduces myocardial O2 demand until revascularization is complete. Bradycardia may be facilitated by the choice of anesthetic agent (Box 145-1). Induced bradycardia is less critical with OPCAB since the advent of newer stabilization devices, such as the CTS retractor, the Octopus, and the Cohn stabilizer (see Figure 145-1). These devices hold a segment of the diseased coronary artery immobile while the heart is beating so that the anastomoses can be performed.
Surgery on the beating heart readily precipitates arrhythmia—from ischemia, manipulation, and reperfusion—that must be treated aggressively. Lidocaine and magnesium are used routinely; other antiarrhythmic agents must be readily available, and antiarrhythmic strategies may be used (Box 145-2).