Chapter 70 Ocular Histoplasmosis
Historical perspective
In 1942 Reid provided the first description of histoplasmosis-associated ophthalmic abnormalities from a patient with acute disseminated histoplasmosis.1 Following Reid’s description, additional reports surfaced of atrophic chorioretinal lesions associated with positive histoplasmin skin testing.2–4 In 1959 Woods and Wahlen4 published a series of 62 patients with granulomatous uveitis. Nineteen of these patients “showed a peculiar and consistent pattern of ocular lesions” that included both discrete atrophic, sparsely pigmented or unpigmented, peripheral lesions (frequently referred to as “histo spots”) and later cystic lesions in the macula. Skin testing for histoplasmin was positive in all of these 19 patients. Woods and Wahlen concluded that previous benign systemic histoplasmosis was responsible for the ocular findings in these 19 patients.4 A few years later Schlaegel and Kenney5 demonstrated that atrophic lesions around the optic nerve were also part of the clinical spectrum of ocular histoplasmosis syndrome (OHS), often called ocular histoplasmosis or presumed ocular histoplasmosis syndrome (POHS).
Clinical features of ocular histoplasmosis
A clinical diagnosis of ocular histoplasmosis is based on the presence of at least two of the following fundus lesions in one or both eyes in the absence of ocular inflammation:6,7
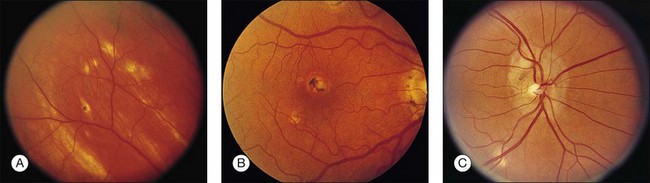
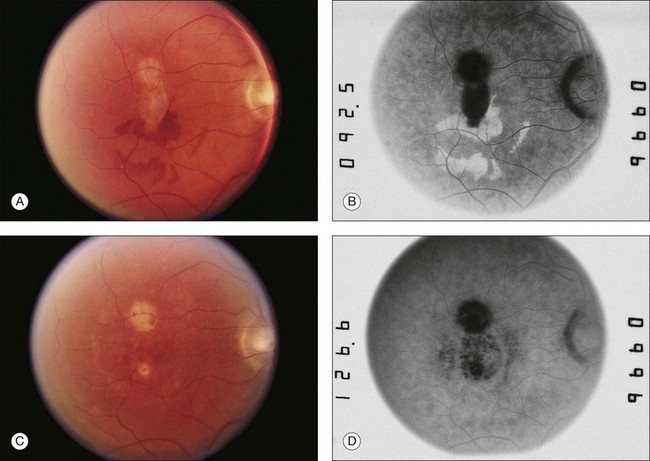
• Discrete, focal, atrophic (i.e., punched-out) choroidal scars in the macula or the periphery, smaller in size than the optic disc (histo spots) (Fig. 70.1).
• Peripapillary chorioretinal scarring (i.e., peripapillary atrophy) (Fig. 70.2).
• CNV or associated sequelae (hemorrhagic retinal detachment, fibrovascular disciform scar) (Figs 70.3–70.5).
Most often both eyes have typical lesions, although the appearance may not be symmetric at initial presentation. The early granulomatous stage of ocular histoplasmosis, as described by Woods and Whalen, is rarely seen clinically.4,6 The initial focal scars are probably too small to be seen with the ophthalmoscope. Gass6 has postulated that lymphocytic infiltration of the surrounding tissue produces enlargement of the lesion over a period of years and thus allows it to become clinically detectable.
Differential diagnosis
The differential diagnosis of ocular histoplasmosis includes a wide spectrum of disorders:
• Multifocal choroiditis with panuveitis. Characterized by multiple chorioretinal scars with similar findings to ocular histoplasmosis. Significant anterior and/or posterior inflammation present in the active phase, and there may have associated CNV. One study examined distinguishing features of multifocal choroiditis compared to ocular histoplasmosis.8 Findings that were more characteristic of multifocal choroiditis included progressive growth of lesions, bridging scars, progressive proliferation of pigment, myopic disc changes, clustering of lesions (e.g., macula, equator), disc swelling, subretinal fibrosis, and narrowed/sheathed vessels.8 These features may be particularly important in distinguishing quiescent multifocal choroiditis from ocular histoplasmosis (see Chapter 76, White spot syndromes and related diseases).
• Myopic degeneration. Peripapillary atrophy and CNV may be seen in patients with myopic degeneration. Small white focal areas of chorioretinal atrophy along with linear atrophic areas (e.g., lacquer cracks) may also be present in the posterior pole (see Chapter 68, Myopic macular degeneration).
• Multiple evanescent white-dot syndrome (MEWDS). White lesions of the retinal pigment epithelium (RPE)/outer retina may be present with associated granularity of the fovea. Often the vision is transiently decreased with an associated enlarged blind spot. Mild inflammation may be present. Scarring and permanent chorioretinal lesions are not usually observed (see Chapter 76, White spot syndromes and related diseases).
• Idiopathic CNV. A diagnosis of exclusion. Particularly in younger individuals, idiopathic CNV is seen in the absence of other signs of ocular histoplasmosis, age-related macular degeneration (AMD), angioid streaks, and other CNV-related conditions.
• Choroidal rupture with CNV. A history of trauma is usually present. A partially circumferential concentric chorioretinal macular scar is typically present and is associated with the CNV. Peripapillary atrophy and associated peripheral chorioretinal atrophy is not present (see Chapter 91, Traumatic chorioretinopathies).
• Punctate inner choroidopathy. Minimal to mild inflammation may be present. Atrophic scars may be associated with CNV. Spots are usually smaller than those seen with ocular histoplasmosis. Predominantly seen in women. Peripapillary atrophy is usually not present. Acute symptoms (e.g., photopsias) are usually associated with the initial diagnosis of the white lesions and may correlate with location of lesions (see Chapter 76, White spot syndromes and related diseases).
• Neovascular AMD. Typically in older patients (i.e., >50 years). Drusen present. Areas of focal atrophy may be present in the macula but the atrophy is not usually seen in the periphery. Peripapillary atrophy is often not present (see Chapter 66, Neovascular (exudative or “wet”) age-related macular degeneration).
• Sarcoidosis. Scattered active inflammatory choroidal lesions may be present. Usually accompanied by anterior/posterior inflammation. CNV and peripapillary atrophy not typically present. Elevated angiotensin-converting enzyme may be seen. Often associated with hilar adenopathy on chest X-ray or CT scan of the chest (see Chapter 78, Sarcoidosis).
Relationship of ocular disease to systemic infection
Systemic infection with Histoplasma capsulatum via the respiratory tract is thought to be the initial event prior to the development of ocular histoplasmosis. Although a definitive causal relationship between H. capsulatum and the ocular disorder has not been demonstrated to satisfy Koch’s postulates completely,9,10 continuing experimental work with primates,11,12 may eventually satisfy this requirement.
• Almost all patients diagnosed as having ocular histoplasmosis in the USA have lived some or all of their lives in an endemic area.13,14
• Positive histoplasmin skin testing occurs more frequently in patients with ocular histoplasmosis compared with controls.14–16
• Activation of lesions of ocular histoplasmosis has been reported following histoplasmin skin testing.2–4,16–18
• DNA from H. capsulatum has been isolated from an enucleated eye previously diagnosed with ocular histoplasmosis.19
Other observations can be used to question the causal relationship between H. capsulatum and the ocular syndrome. In the UK and Europe, a clinical syndrome nearly identical to ocular histoplasmosis may occur.20–24 These patients have never lived in or visited an endemic area, however, and only a small proportion of Europeans are positive reactors to histoplasmin skin testing.20–25 Additionally, H. capsulatum has not been identified in the UK.25 Certainly, the possibility exists that an alternate organism may result in a similar ocular syndrome in these areas.22 Systemic antifungal treatment with amphotericin B has not been shown to be effective for the treatment of the ocular disorder.26.
Clinical features of systemic infection
Goodwin27 classified systemic infection based on the immune status of the host and exposure type. The usual histoplasmosis infection is a relatively mild illness with flu-like respiratory symptoms. Most patients do not seek medical care. Studies in Tennessee have demonstrated that almost 90% of children of 13 years of age had positive reactions to histoplasmin skin tests.28 A great deal of variation has been observed in the distribution of positive reactors by neighborhood of residence.29,30 Rarely, more severe, even fatal cases of disseminated infection may occur, but these are usually associated with immune system deficiencies, such as acquired immunodeficency syndrome (AIDS). Occasionally, epidemics of systemic disease outbreak may occur which are often associated with high levels of environmental exposure (e.g., excavations, construction projects in old buildings, work in chicken or other fowl habitats, or exposure in bat-inhabited caves).31–46
Epidemiology of ocular histoplasmosis
Geographic distribution of H. capsulatum in the USA
The Ohio and Mississippi river valleys make up the largest part of the “histo belt,” where 60% or more of lifelong residents have positive histoplasmin skin testing.47 Comstock described the major endemic histoplasmosis area as a triangle with its apices in Eastern Nebraska, Central Ohio, and Southwestern Mississippi.29
Prevalence and incidence
The prevalence of asymptomatic ocular histoplasmosis in endemic areas (e.g., Ohio, Maryland) within the USA ranges from 1.6 to 5.3%.14,15,48 The disciform lesion prevalence rates in the same areas were 0.0 to 0.1% of the endemic populations.14,15,48 In those eyes that had atrophic spots, the prevalence of disciform lesions was 4.5%.48
The incidence rate of neovascular disciform lesions and atrophic lesions is largely unknown. The development of initial neovascular disciform lesions has been reported at around 2 per 100 000 population per year.49 Studies examining the incidence rate of neovascular lesions in fellow eyes have shown a rate of 0.0 to 12% per year.50–54
Age
The median age of patients with vision-threatening disciform lesions has typically been reported to be in the fourth and fifth decade, with an age range of 10 to 81 years old.13,17,49,55–58 The median age of persons who have atrophic scars has been reported to be in the fourth, fifth, and sixth decades of life by various investigators.15,59 These reports are of the age at detection, however, and not necessarily the age of development of the atrophic lesion. It is likely that these lesions develop earlier in life and are only coincidentally discovered during ophthalmic examinations for causes of visual symptoms that may or may not be related to ocular histoplasmosis.
Gender and race
There is no gender predilection for ocular histoplasmosis. The vast majority of disciform lesions occur in Caucasians with only around a dozen cases reported among African Americans.60 Interestingly, histo spots and positive skin tests have been reported in some studies to have similar prevalence among Caucasians and African Americans.15,61 Other studies have found a much higher prevalence in Caucasians (i.e., nearly 100% of all cases) as compared to Hispanics or African Americans.14,16,48,55
Histocompatibility antigens and genetic predisposition
In disciform lesions, both human leukocyte antigen (HLA)-B7 and HLA-DRw2 have been reported to be two to four times more common among cases than controls.62–64 For histo spots, HLA-DRw2 was twice as common among cases as among controls, but less difference was seen between the groups in regards to HLA-B7.64,65 These findings suggest an underlying genetic susceptibility or predisposition for development of ocular histoplasmosis. It is unclear whether this genetic predisposition specifically reflects the susceptibility to ocular histoplasmosis or to infection by H. capsulatum. Although these associations exist, routine testing for HLA typing in connection with ocular histoplasmosis is not typically performed owing to the lack of significant positive and negative predictive values.
Pathogenesis
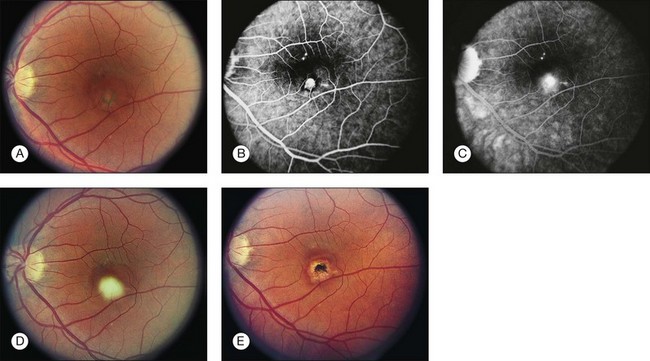
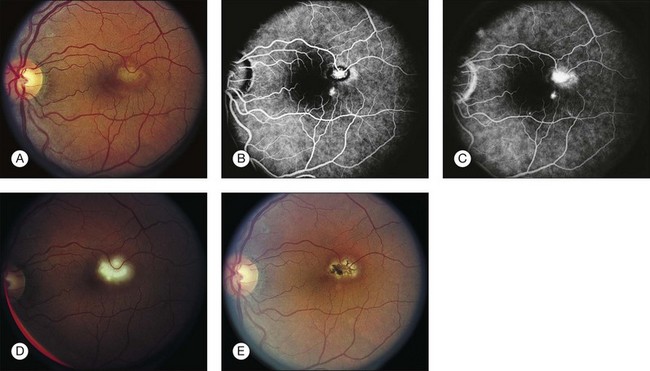
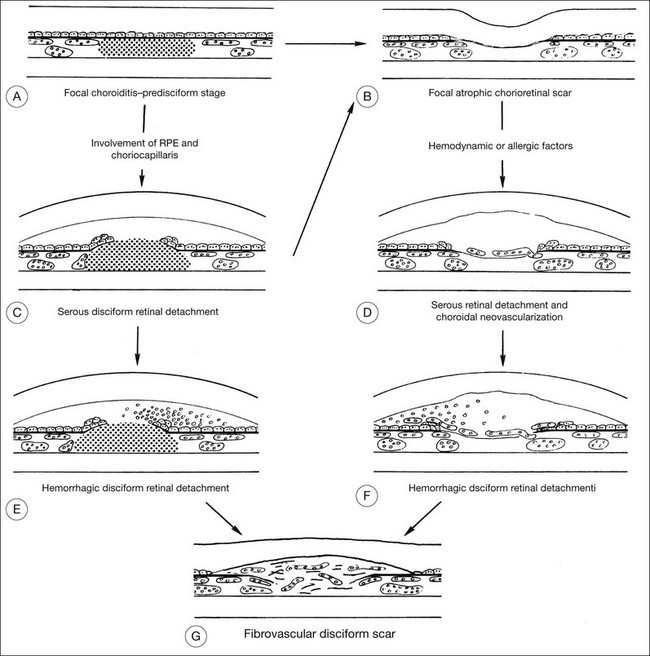
Numerous theories regarding the pathogenesis of ocular histoplasmosis have been proposed. The most widely accepted theory involves focal infection of the choroid at the time of systemic infection. The focal inflammatory/infectious process results in an atrophic scar that disrupts Bruch’s membrane. Alternatively, the infection may involve the retinal pigment epithelium and choriocapillaris and may progress rapidly to subretinal hemorrhage, exudation, and a fibrovascular disciform scar (Fig. 70.6).
CNV formation may be promoted by multiple factors at the site of the atrophic scar. Disruption of Bruch’s membrane provides access to the subretinal space for neovascularization.66 The fragile vessels are prone to hemorrhage and exudation, often ultimately resulting in disorganization of the RPE and neurosensory retina and, ultimately, a fibrovascular scar.
The initiator for CNV development is unknown. The results from HLA typing suggest a possible genetic predisposition for progression from atrophic scars to disciform lesions in ocular histoplasmosis.62–65 Other hypotheses have attributed these phenomena to a larger initial inoculum of the fungus,11,67 reinfection,4,68 hypersensitivity,4,14 and the presence of other factors that compromise the vascular system14,69,70 or the immune system.71 CNV development has also been associated with proangiogenic factors such as vascular endothelial growth factor.72
Studying ocular histoplasmosis with animal models has been difficult. Histoplasmosis is known to occur in many species of animals.73–77 However, efforts to develop an animal model for ocular histoplasmosis have been hampered by two major factors: (1) nonprimates do not have a macula with its special anatomic, physiologic, and neurologic characteristics; and (2) decades are believed to elapse between initial infection with H. capsulatum and the development of characteristic macular lesions. The most promising animal models are primates, in which systemic infection and ocular lesions have been produced.11,12
Natural history of ocular histoplasmosis and public health implications
Histo spots outside the macular area are typically asymptomatic, although visual symptoms occasionally have been reported that correlate with the location of the atrophic scars.78 Active CNV may result in sudden decrease in vision secondary to hemorrhage or exudation. The vision loss in this disease often occurs in middle-aged individuals who are in the most active and productive stage of their life.13,17,49,55–58 Spontaneous recovery of central vision has been reported in the Macular Photocoagulation Study (MPS)51,56 and by other investigators.79–81
Two studies have addressed the public health importance of ocular histoplasmosis as a cause of visual impairment. One study in Tennessee found that ocular histoplasmosis was responsible for 2.8% of visual impairment among applicants for aid for the blind.49 In Maryland a study comparing the 15-year incidence of visual impairment in those persons with histo spots to those persons without histo spots found that there was no difference in the rates of visual impairment.50 The Submacular Surgery Trials Research Group found that individuals with unilateral and bilateral CNV cases had significant deficits in visual function, similar to patients with neovascular age-related macular degeneration (AMD).82 Not surprisingly, the study showed that patients with bilateral CNV had significantly worse functional impairment of all groups, but those with unilateral involvement also had significant functional deficits.82
Treatment
Numerous approaches for ocular histoplasmosis management have been suggested, including avoidance of stress, avoidance of aspirin, avoidance of the Valsalva maneuver, hyposensitization to histoplasmin, use of immunosuppressive agents, and photocoagulation.9 Histoplasmin desensitization,83 amphotericin B,17,26 and other prophylactic interventions84,85 have been tried by many investigators and discarded. No treatment is known to prevent inactive lesions from giving rise to exudative or hemorrhagic neovascular complexes that typically end in disciform macular scars. Systemic corticosteroids also have been suggested, particularly in cases of “active” histo spots and subfoveal CNV.6 in the era of anti-vascular endothelial growth factor (VEGF) and photodynamic therapy (PDT), however, the use of systemic corticosteroids even in subfoveal cases is now mainly of historic interest. Whether there is a role to manage active histo spots is unclear since many or perhaps most spontaneously involute.
Laser photocoagulation
Initiated in 1979, the Macular Photocoagulation Study (MPS) Group demonstrated the effectiveness of laser treatment in comparison to no treatment two randomized clinical trials for patients with well-defined extrafoveal or juxtafoveal CNV.56,57,86,87 The first trial enrolled 262 patients with well-demarcated extrafoveal CNV.57,86 The posterior border of these lesions could not be closer than 200 µm from the center of the foveal avascular zone; initial best-corrected visual acuity of the affected eye was 20/100 or better. Eligible eyes were randomly assigned to argon laser treatment or to no treatment. The eyes were re-examined twice each year, at which time best-corrected VA was measured and color photographs were taken. Fluorescein angiograms were taken at time of study entry, 6 and 12 months after enrollment, and annually thereafter.
In 1983, the MPS Data and Safety Monitoring Committee halted enrollment after concluding that argon laser photocoagulation was beneficial in preventing or delaying large loss of visual acuity compared to observation without treatment. From 18 months through 5 years, a 6 or more line loss of VA was experienced in 10% of treated eyes compared to 40% of untreated controls. Median VA at baseline was 20/25 and after five years dropped to 20/40 in the treated group compared to 20/80 in controls.86 In the laser-treated group, 26% of eyes had persistence of CNV or recurrence of CNV at the scar edge, and 7% developed a new CNV not contiguous with the laser scar.86
In 1981 a second trial was initiated by the MPS Group for patients with juxtafoveal CNV.87 In this trial, best-corrected VA at entry was permitted to be as poor as 20/400 in the study eye. A total of 289 eyes were randomized between krypton laser treatment and no treatment. Five years after the trial began, the MPS Data and Safety Monitoring Committee again halted enrollment after concluding that eyes treated with krypton laser were less likely to lose visual acuity than untreated eyes. A 6- or more line loss was seen in 11% of the treated eyes compared to about 30% of the controls.87 Approximately one-third of treated patients had persistent or recurrent CNV contiguous with the zone of laser treatment; and new, noncontiguous areas of CNV developed in 2% of treated eyes.87 A subgroup analysis by the MPS group of CNV located between the fovea and optic nerve showed that there was no contraindication to treatment of these lesions in the papillomacular bundle with laser.88 A subset of the MPS Group piloted laser photocoagulation for subfoveal CNV secondary to ocular histoplasmosis but observed no short-term benefit compared to observation.89
Photodynamic therapy
The treatment of subfoveal CNV secondary to ocular histoplasmosis with photodynamic therapy (PDT) was first suggested in 2002.90 Since that small study, numerous studies have been published examining the use of PDT for ocular histoplasmosis. In fact, PDT is now approved by the United States Food and Drug Administration (FDA) for the treatment of subfoveal CNV secondary to ocular histoplasmosis.
Most of the studies performed for PDT with ocular histoplasmosis have been retrospective case series. In a 2003 retrospective review of 38 eyes with juxtafoveal CNV treated with PDT, treated eyes were more than twice as likely to have visual improvement or stabilization compared to the natural history group in the corresponding MPS clinical trial. Visual acuity improved or stabilized in 69% of eyes, with 44% of eyes improving at least 2 lines. Nearly 40% of eyes had undergone submacular surgery prior to PDT.91 In 2004 a retrospective review of 11 eyes, of which 5 had juxtafoveal CNV and 6 had subfoveal CNV, documented similar findings. Eighty percent of eyes showed vision stabilization or improvement in the juxtafoveal group. Sixty percent of eyes with juxtafoveal lesions achieved a final visual acuity of 20/40 or better. Eyes with subfoveal lesions had similar results with 83% of eyes having stabilization or improvement in vision. Fifty percent of eyes with subfoveal CNV also had a final visual acuity of 20/40 or better.92 In 2005 a retrospective review of 23 eyes with juxtafoveal CNV associated with ocular histoplasmosis found that approximately 82% of eyes had visual stabilization (less than 2 line loss) or improvement. Thirty percent of eyes gained more than 2 lines of vision. Approximately, 60% of patients required only a single PDT session. Following PDT, submacular surgery was performed in 16% of patients due to CNV progression.93
In 2006 a retrospective review of young patients undergoing PDT for CNV secondary to etiologies other than AMD included 6 patients with ocular histoplasmosis with subfoveal CNV. The mean pretreatment acuity in these eyes was 20/50 and the mean final visual acuity was 20/50. Three of these eyes (50%) required at least one retreatment session with PDT. One of 6 patients improved by more than 1 line of VA. Four eyes (67%) maintained their visual acuity (i.e., less than 2 lines lost or gained), and one eye gained more than 2 lines of VA and one eye lost 2 lines.94
An uncontrolled prospective trial evaluating PDT for subfoveal CNV secondary to POHS included 26 eyes. Examination of 22 eyes 2 years following initial treatment revealed that 45% of eyes had gained 1.5 lines or more. Eighteen percent of eyes lost 1.5 lines or more, including 9% of eyes that lost 3 or more lines of VA. The mean number of treatments was 2.9 during the first year and 1 during the second year. After 2 years, only 15% of eyes had persistent angiographic leakage.95
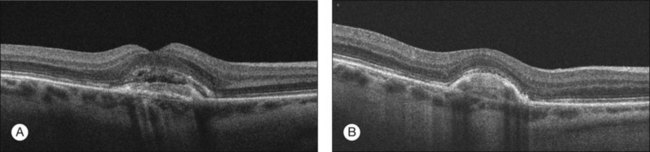
Anti-VEGF therapy
Over the last several years, the use of anti-VEGF agents has transformed the landscape in the treatment of CNV-related disease, particularly neovascular AMD. Case reports and case series suggest that anti-VEGF agents may also be effective in the treatment of CNV secondary to ocular histoplasmosis (Fig. 70.7). In 2007 the first case report was published documenting a 23-year-old female with sudden vision loss to 20/200 with subfoveal CNV. After a single intravitreal injection of bevacizumab, the visual acuity improved to 20/30 by 6 months follow-up.96 Of course, the control arms of the MPS studies discussed above show that spontaneous involution can occur, but following this case report, retrospective consecutive case series were published examining the use of the intravitreal bevacizumab for the treatment of CNV in ocular histoplasmosis. One study examined intravitreal bevacizumab in 24 treatment-naïve eyes. The mean age was 43 years and the average number of injections was 6.8 per year. After 3 months, visual acuity improved from a mean baseline visual acuity of 20/114 to 20/55 (i.e., approximately 3-lines). Fifty-eight percent of eyes had 20/40 or better vision at final follow-up compared to 21% at baseline. Nine patients had 12 month follow-up and improved from a mean baseline visual acuity of 20/150 to 20/45 (i.e., approximately 6 lines). No significant complications were reported.97
A second study examined the use of bevacizumab in 28 eyes with CNV secondary to histoplasmosis. All patients included had active CNV with subfoveal fluid and either juxtafoveal or subfoveal CNV. Previous or concurrent PDT was allowed in this study. Seven patients were treatment naïve, 16 were PDT failures, and 5 patients were treated with combination PDT/bevacizumab therapy. The mean age was 46 years and mean follow-up was 5 months. Overall, the mean initial visual acuity was 20/88 and the mean final visual acuity was 20/54. Stability of visual acuity (<1.5 line loss) was seen in 93% of patients. Additionally, 43% of eyes experienced a 3 or more line gain. Both of the studies examining bevacizumab were retrospective with significant methodologic shortcomings and the results should be interpreted with caution.98
A phase I randomized 12-month clinical trial evaluated ranibizumab for the treatment of CNV secondary to conditions other than AMD has been conducted. This study randomized eyes to monthly ranibizumab or 3-monthly injections followed by an as needed (prn) dosing schedule at monthly visits. Nine eyes (of 30) with ocular histoplasmosis were included in this trial, 4 in the monthly arm and 5 in the prn arm. Prior treatment with other therapeutic modalities was allowed. Subgroup analysis was not performed for each diagnosis included. As a group, mean lines of change from baseline was +7.4 in the monthly injection arm and +5.0 in the prn group. A 3-line or more gain in visual acuity was seen in 66.7% of the monthly arm patients and in 57% in the prn arm. There were no statistically significant differences between the groups at any time point. No serious ocular or systemic adverse events were observed but larger sample sizes are needed to detect infrequent severe adverse events.99
Combination therapy
Similar to AMD, combination therapy is also being considered for the treatment of CNV secondary to ocular histoplasmosis. Combination therapy may reduce the need for ongoing intravitreal injections. PDT or laser photocoagulation may provide a more enduring effect, compared to anti-VEGF therapy alone. Adding anti-VEGF therapy may reduce the required spot size needed for either laser modality. In 2010, a small retrospective case series examining combination anti-VEGF agents with PDT included three eyes with CNV secondary to ocular histoplasmosis. Treatment consisted of PDT and intravitreal bevacizumab initiated concurrently with retreatment with PDT every 10–12 weeks and with bevacizumab every 4–6 weeks. Retreatment was based on persistent edema or subretinal fluid. Three of 3 (100%) eyes improved 2 lines or more at final follow-up.100 As outlined in the previous section, a retrospective case series utilizing bevacizumab for CNV secondary to ocular histoplasmosis included 5 eyes that were treated with concurrent PDT therapy. Subgroup analysis of these five patients revealed that all five eyes experienced stabilization or improvement in visual acuity with a mean gain of 2.4 lines.98
Intravitreal triamcinolone
Given the possible underlying inflammatory pathogenic mechanisms of ocular histoplasmosis, the use of intravitreal steroids may be of use in the treatment of CNV secondary to ocular histoplasmosis. A retrospective case series examined the use of intravitreal triamcinolone in 10 eyes with CNV secondary to ocular histoplasmosis (5 subfoveal and 5 juxtafoveal) was conducted with a median follow-up of 17 months. Visual acuity improved or stabilized in 80% of eyes, including 30% that gained 1 line or more. Twenty percent of eyes lost 1–3 lines of visual acuity, and no eyes lost more than 3 lines of vision. Cataract progression and increased intraocular pressure were concerning ocular side effects.101
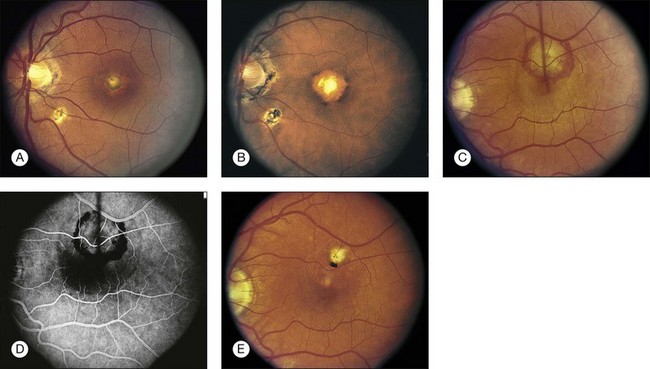
Submacular surgery and macular translocation
Prior to PDT and anti-VEGF therapy, submacular surgery for CNV secondary to ocular histoplasmosis was an important treatment alternative for many patients with significant vision loss.102–104 As with many treatment modalities for CNV, recurrence of CNV is a major issue. In fact, the recurrence rate after submacular surgery is higher than recurrence following laser photocoagulation.105 In 1997 the National Eye Institute and the National Institutes of Health initiated the Submacular Surgery Trials group H trial in order to compare functional outcomes and quality of life between patients assigned to surgery versus those assigned to observation (Fig. 70.8). The trial included 225 patients non-AMD with subfoveal CNV and visual acuity of 20/50 to 20/800. Of the 225 patients, 192 patients had ocular histoplasmosis. At 2 years, vision had improved or remained stable in 20% more patients treated with surgery than with observation.106 This outcome difference was not statistically significant. Subgroup analyses revealed that nearly all of the benefit seen with surgery was in those eyes with 20/100 or worse baseline visual acuity. In this subset of 92 eyes, 76% of surgery eyes remained stable or improved compared to 50% of eyes that were observed. Additionally, quality-of-life scores improved more with surgery.107
Macular translocation has also been utilized for the treatment of patients with bilateral vision loss associated with ocular histoplasmosis.108 One report described three cases of ocular histoplasmosis treated with 360-degree macular translocation. Two of the 3 eyes showed improvement in visual acuity. Two of the 3 cases developed recurrent CNV, and 2 of the 3 cases developed chronic cystoid macular edema.108 Limited macular translocation for ocular histoplasmosis has also been reported, but the specific visual acuity results were not separated from the larger study which included predominantly AMD cases so that conclusions cannot be drawn regarding the effectiveness of limited translocation for ocular histoplasmosis.109 Although surgical intervention remains a viable option in select situations, anti-VEGF therapy and PDT are now the mainstays of treatment for subfoveal and juxtafoveal CNV secondary to ocular histoplasmosis and laser photocoagulation is the typical treatment advised for extrafoveal CNV.
1 Reid JD, Scherer JH, Herbut PA, et al. Systemic histoplasmosis diagnosed before death and produced experimentally in guinea pigs. J Lab Clin Med. 1942;27:419–434.
2 Krause AC, Hopkins WG. Ocular manifestation of histoplasmosis. Am J Ophthalmol. 1951;39:564–566.
3 Schlaegel TF. Granulomatous uveitis: an etiologic survey of 100 cases. Trans Am Acad Ophthalmol Otolaryngol. 1958;62:813–825.
4 Woods AC, Wahlen HE. The probable role of benign histoplasmosis in the etiology of granulomatous uveitis. Trans Am Ophthalmol Soc. 1959;57:318–343.
5 Schlaegel TF, Kenney D. Changes around the optic nerve head in presumed ocular histoplasmosis. Am J Ophthalmol. 1966;62:454–458.
6 Gass JDM. Stereoscopic atlas of macular diseases. Vol. 1, Diagnosis and treatment. St Louis, MO: Mosby; 1987.
7 Patz A, Fine SL. Presumed ocular histoplasmosis. In: Yanuzzi LA, Gitter KA, Schatz H. The macula: a comprehensive text and atlas. Baltimore: Williams & Wilkins, 1979.
8 Parnell JR, Jampol LM, Yannuzzi LA, et al. Differentiation between presumed ocular histoplasmosis syndrome and multifocal choroiditis with panuveitis based on morphology of photographed fundus lesions and fluorescein angiography. Arch Ophthalmol. 2001;119:208–212.
9 Schlaegel TF. Ocular histoplasmosis. New York: Grune & Stratton; 1977.
10 Wong VG, Kwon-Chung KJ, Hill WB. Koch’s postulates and experimental ocular histoplasmosis. Int Ophthalmol Clin. 1975;15:139–145.
11 Smith RE. Natural history and reactivation studies of experimental ocular histoplasmosis in a primate model. Trans Am Ophthalmol Soc. 1982;80:695–757.
12 Jester JV, Smith RE. Subretinal neovascularization after experimental ocular histoplasmosis in a subhuman primate. Am J Ophthalmol. 1985;100:252–258.
13 Van Metre TE, Maumenee AE. Specific ocular uveal lesions in patients with evidence of histoplasmosis. Arch Ophthalmol. 1964;71:314–324.
14 Ganley JP. Epidemiologic characteristics of presumed ocular histoplasmosis. Acta Ophthalmol. 1973;Suppl. 119:1–63.
15 Asbury T. The status of presumed ocular histoplasmosis: including a report of a survey. Trans Am Ophthalmol Soc. 1966;4:371–400.
16 Schlaegel TF, Weber JC, Helveston E, et al. Presumed histoplasmic choroiditis. Am J Ophthalmol. 1967;63:919–925.
17 Makley TA, Long JW, Suie T, et al. Presumed histoplasmic chorioretinitis with special emphasis on the present modes of therapy. Trans Am Acad Ophthalmol Otolaryngol. 1965;69:443–457.
18 McCulloch C. Histoplasmosis. Trans Can Ophthalmol Soc. 1963;26:107–125.
19 Spencer WH, Chan C-C, Shen DF, et al. Detection of Histoplasma capsulatum DNA in lesions of chronic ocular histoplasmosis syndrome. Arch Ophthalmol. 2003;121:1551–1555.
20 Braunstein RA, Rosen DA, Bird AC. Ocular histoplasmosis syndrome in the United Kingdom. Br J Ophthalmol. 1974;58:893–898.
21 Craandijk A. Focal macular choroidopathy. Doc Ophthalmol. 1979;48:1–99.
22 Bottoni FG, Deutman AF, Aandekerk AL. Presumed ocular histoplasmosis syndrome and linear streak lesions. Br J Ophthalmol. 1989;73:528–535.
23 Suttorp-Schulten MSA, Bollemeijer JG, Bos PJM, et al. Presumed ocular histoplasmosis in the Netherlands – an area without histoplasmosis. Br J Ophthalmol. 1997;81:7–11.
24 Ongkosuwito JV, Kortbeek LM, Van der Lelij A, et al. Aetiological study of the presumed ocular histoplasmosis syndrome in the Netherlands. Br J Ophthalmol. 1999;83:535–539.
25 Edwards PQ, Billings EL. Worldwide pattern of skin sensitivity to histoplasmin. Am J Trop Med Hyg. 1971;20:288–319.
26 Giles CL, Falls HF. Further evaluation of amphotericin-B therapy in presumptive histoplasmosis chorioretinitis. Am J Ophthalmol. 1961;51:588–598.
27 Goodwin RA, Shapiro JL, Thurman GH, et al. Disseminated histoplasmosis: clinical and pathologic correlations. Medicine. 1980;95:1–33.
28 Zeidberg LD, Dillon A, Gass RS. Some factors in the epidemiology of histoplasmin sensitivity in Williamson county, Tennessee. Am J Public Health. 1951;41:80–89.
29 Comstock GW, Vicens CN, Goodman NL, et al. Differences in the distribution of sensitivity to histoplasmin and isolations of Histoplasma capsulatum. Am J Epidemiol. 1968;88:195–209.
30 Zeidberg LD. The microdistribution of histoplasmin sensitivity in an endemic area. Public Health Monogr. 1956;39:190–197.
31 Burke DS, Churchill FE, Gaydos JC, et al. Epidemic histoplasmosis in patients with undifferentiated fever. Mil Med. 1982;147:466–467.
32 Ryder KW, Jay SJ, Kiblawi SO, et al. Serum angiotensin converting enzyme activity in patients with histoplasmosis. JAMA. 1983;249:1888–1889.
33 Weber TR, Grosfeld JL, Kleiman MB, et al. Surgical implications of endemic histoplasmosis in children. J Pediatr Surg. 1983;18:486–491.
34 Weinberg GA, Kleiman MB, Grosfeld JL, et al. Unusual manifestations of histoplasmosis in childhood. Pediatrics. 1983;72:99–105.
35 Wheat U, Stein L, Corya BC, et al. Pericarditis as a manifestation of histoplasmosis during two large urban outbreaks. Medicine. 1983;62:110–119.
36 Brodsky AL, Gregg MB, Loewenstein MS, et al. Outbreak of histoplasmosis associated with the 1970 Earth Day activities. Am J Med. 1973;54:333–342.
37 Schwarz J, Salfelder K, Viloria JE. Histoplasma capsulatum in vessels of the choroid. Ann Ophthalmol. 1977;9:633–636.
38 Schlech WF, Wheat U, Ho JL, et al. Recurrent urban histoplasmosis, Indianapolis, Indiana, 1980–1981. Am J Epidemiol. 1983;118:301–312.
39 Waldman RJ, England AC, Tauxe R, et al. A winter outbreak of acute histoplasmosis in northern Michigan. Am J Epidemiol. 1983;117:68–75.
40 Wilcox KR, Waisbren BA, Martin J. The Walworth, Wisconsin, epidemic of histoplasmosis. Ann Intern Med. 1958;49:388–418.
41 Younglove RM, Terry RM, Rose NJ, et al. An outbreak of histoplasmosis in Illinois associated with starlings. Illinois Med J. 1968;134:259–263.
42 Larrabee WF, Ajello L, Kaufman L. An epidemic of histoplasmosis on the isthmus of Panama. Am J Trop Med Hyg. 1978;27:281–285.
43 Loosli CG, Grayston JT, Alexander ER, et al. Epidemiological studies of pulmonary histoplasmosis in a farm family. Am J Hyg. 1952;55:392–401.
44 Bartlett PC, Vonbehren LA, Tewari RP, et al. Bats in the belfry: an outbreak of histoplasmosis. Am J Public Health. 1982;72:1369–1372.
45 Morse DL, Gordon MA, Matte T, et al. An outbreak of histoplasmosis in a prison. Am J Epidemiol. 1985;122:253–261.
46 Sorley DL, Levin ML, Warren JW, et al. Bat-associated histoplasmosis in Maryland bridge workers. Am J Med. 1979;67:623–626.
47 Edwards LB, Acquaviva FA, Livesay VT, et al. An atlas of sensitivity to tuberculin, PPD-B, and histoplasmin in the United States. Am Rev Respir Dis. 1969;99:1–132.
48 Smith RE, Ganley JP. An epidemiologic study of presumed ocular histoplasmosis. Trans Am Acad Ophthalmol Otolaryngol. 1971;75:994–1005.
49 Feman SS, Podgorski SF, Penn MK. Blindness from presumed ocular histoplasmosis in Tennessee. Ophthalmology. 1982;89:1295–1298.
50 Hawkins BS, Ganley JP. Risk of visual impairment attributable to ocular histoplasmosis. Arch Ophthalmol. 1994;112:655–666.
51 Macular Photocoagulation Study Group. Five-year follow-up of fellow eyes of individuals with ocular histoplasmosis and unilateral extrafoveal or juxtafoveal choroidal neovascularization. Arch Ophthalmol. 1996;114:677–688.
52 Lewis ML, Schiffman JC. Long-term follow-up of the second eye in ocular histoplasmosis. Ophthalmol Clin. 1983;23:125–135.
53 Watzke RC, Claussen RW. The long-term course of multifocal choroiditis (presumed ocular histoplasmosis). Am J Ophthalmol. 1981;91:750–760.
54 Sawelson H, Goldberg RE, Annesley WH, et al. Presumed ocular histoplasmosis syndrome: the fellow eye. Arch Ophthalmol. 1976;94:221–224.
55 Gass JDM, Wilkinson CP. Follow-up study of presumed ocular histoplasmosis. Trans Am Acad Ophthalmol Otolaryngol. 1972;76:672–694.
56 Macular Photocoagulation Study Group. Krypton laser photocoagulation for neovascular lesions of ocular histoplasmosis: results of a randomized clinical trial. Arch Ophthalmol. 1987;105:1499–1507.
57 Macular Photocoagulation Study Group. Argon laser photocoagulation for ocular histoplasmosis: results of a randomized clinical trial. Arch Ophthalmol. 1983;101:1347–1357.
58 Schlaegel TF, Weber JC. Follow-up study of presumed ocular histoplasmic choroiditis. Am J Ophthalmol. 1971;71:1192–1195.
59 Smith RE, Ganley JP, Knox DL. Presumed ocular histoplasmosis. II. Patterns of peripheral and peripapillary scarring in persons with nonmacular disease. Arch Ophthalmol. 1972;87:251–257.
60 Baskin MA, Jampol LM, Huamonte FU, et al. Macular lesions in blacks with the presumed ocular histoplasmosis syndrome. Am J Ophthalmol. 1980;89:77–83.
61 Edwards PQ, Palmer CE. Sensitivity to histoplasmin among negro and white residents of different communities in the USA. Bull WHO. 1964;30:575–585.
62 Godfrey WA, Sabates R, Cross DE. Association of presumed ocular histoplasmosis with HLA-B7. Am J Ophthalmol. 1978;85:854–858.
63 Braley RE, Meredith TA, Aaberg TM, et al. The prevalence of HLA-B7 in presumed ocular histoplasmosis. Am J Ophthalmol. 1978;85:859–861.
64 Meredith TA, Smith RE, Duquesnoy RJ. Association of HLA-DRw2 antigen with presumed ocular histoplasmosis. Am J Ophthalmol 1980;89:70–6.
65 Meredith TA, Smith RE, Braley RE, et al. The prevalence of HLA-B7 in presumed ocular histoplasmosis in patients with peripheral atrophic scars. Am J Ophthalmol. 1978;86:325–328.
66 Weingeist TA, Watzke RC. Ocular involvement by Histoplasma capsulatum. Int Ophthalmol Clin. 1983;23:33–47.
67 Smith RE, Macy JI, Parrett C, et al. Variations in acute multifocal histoplasmic choroiditis in the primate. Invest Ophthalmol Vis Sci. 1978;17:1005–1018.
68 Davidorf FH. The role of T-lymphocytes in the reactivation of presumed ocular histoplasmosis scars. Int Ophthalmol Clin. 1975;15:111–124.
69 Gamble CN, Aronson SB, Brescia FB. Experimental uveitis. 1. The production of recurrent immunologic (Auer) uveitis and its relationship to increased uveal vascular permeability. Arch Ophthalmol. 1970;84:321–330.
70 Aronson SB, Fish MB, Pollycove M, et al. Altered vascular permeability in ocular inflammatory disease. Arch Ophthalmol. 1971;85:455–466.
71 Kaplan HJ, Waldrep JC. Immunological basis of presumed ocular histoplasmosis. Int Ophthalmol Clin. 1983;23:19–31.
72 Kwak N, Okamoto N, Wood JM, et al. VEGF is major stimulator in model of choroidal neovascularization. Invest Ophthalmol Vis Sci. 2000;41:3158–3164.
73 De Monbreun WA. The dog as a natural host for Histoplasma capsulatum: report of a case of histoplasmosis in this animal. Am J Trop Med. 1939;19:565–587.
74 Emmons CW, Morlan HB, Hill EL. Histoplasmosis in rats and skunks in Georgia. Public Health Rep. 1949;64:1423–1430.
75 Akun RS. Histoplasmosis in a cat. J Am Vet Med Assoc. 1950;117:43–44.
76 Menges RW. Histoplasmin sensitivity in animals. Public Health Monogr. 1956;39:210–215.
77 Menges RW, Furcolow ML, Hinton A. The role of animals in the epidemiology of histoplasmosis. Public Health Monogr. 1956;39:277–281.
78 Rivers MB, Pulido JS, Folk JC. Ill-defined choroidal neovascularization within ocular histoplasmosis scars. Retina. 1992;12:90–95.
79 Orlando RG, Davidorf FH. Spontaneous recovery phenomenon in the presumed ocular histoplasmosis syndrome. Int Ophthalmol Clin. 1983;23:137–149.
80 Jost BF, Olk RJ, Burgess DR. Factors related to spontaneous visual recovery in the ocular histoplasmosis syndrome. Retina. 1987;7:1–8.
81 Campochiaro PA, Morgan KM, Conway BP, et al. Spontaneous involution of subfoveal neovascularization. Am J Ophthalmol. 1990;109:668–675.
82 Submacular Surgery Trials Research Group. Health- and vision-related quality of life among patients with ocular histoplasmosis or idiopathic choroidal neovascularization at time of enrollment in a randomized trial of submacular surgery. SST report no. 5. Arch Ophthalmol. 2005;123:78–88.
83 Kaiser RJ, Torsch T, O’Connor PR. Prognostic criteria in macular histoplasmic choroiditis. Int Ophthalmol Clin. 1975;15:41–49.
84 Makley TA, Long JW, Suie T. Therapy of chorioretinitis presumed to be caused by histoplasmosis. Int Ophthalmol Clin. 1975;15:181–195.
85 Schlaegel TF. Corticosteroids in the treatment of ocular histoplasmosis. Int Ophthalmol Clin. 1983;23:111–123.
86 Macular Photocoagulation Study Group. Argon laser photocoagulation for neovascular maculopathy: five-year results from randomized clinical trials. Arch Ophthalmol. 1991;109:1109–1114.
87 Macular Photocoagulation Study Group. Laser photocoagulation for juxtafoveal choroidal neovascularization: five-year results from randomized clinical trials. Arch Ophthalmol. 1994;112:500–509.
88 Macular Photocoagulation Study Group. Laser photocoagulation for neovascular lesions nasal to the fovea: results from clinical trials for lesions secondary to ocular histoplasmosis and idiopathic causes. Arch Ophthalmol. 1995;113:56–61.
89 Fine SL, Wood WJ, Isernhagen RD, et al. Laser treatment of subfoveal neovascular membranes of ocular histoplasmosis. Arch Ophthalmol. 1993;111:19–20.
90 Saperstein DA, Rosenfeld PJ, Bressler NM, et al. Photodynamic therapy of subfoveal choroidal neovascularization with verteporfin in the ocular histoplasmosis syndrome. One-year results of an uncontrolled, prospective case series. Ophthalmology. 2002;109:1499–1505.
91 Busquets MA, Shah GK, Wickens J, et al. Ocular photodynamic therapy with verteporfin for choroidal neovascularization secondary to ocular histoplasmosis syndrome. Retina. 2003;23:299–306.
92 Liu JC, Boldt HC, Folk JC, et al. Photodynamic therapy of subfoveal and juxtafoveal choroidal neovascularization in ocular histoplasmosis syndrome: a retrospective case series. Retina. 2004;24:863–870.
93 Shah GK, Blinder KJ, Hariprasad SM, et al. Photodynamic therapy for juxtafoveal choroidal neovascularization due to ocular histoplasmosis syndrome. Retina. 2005;25:26–32.
94 Lam A, Lee HC, Ho AC, et al. Photodynamic therapy in young patients. Ophthalmic Surg Lasers Imaging. 2006;37:182–189.
95 Rosenfeld PJ, Saperstein DA, Bressler NM, et al. Verteporfin in Ocular Histoplasmosis Study Group. Photodynamic therapy with verteporfin in ocular histoplasmosis:uncontrolled, open-label 2-year study. Ophthalmology. 2004;111:1725–1733.
96 Adán A, Navarro M, Casaroli-Marano RP, et al. Intravitreal bevacizumab as initial treatment for choroidal neovascularization associated with presumed ocular histoplasmosis syndrome. Graefes Arch Clin Exp Ophthalmol. 2007;245:1873–1875.
97 Ehrlich R, Ciulla TA, Maturi R, et al. Intravitreal bevacizumab for choroidal neovascularization secondary to presumed ocular histoplasmosis syndrome. Retina. 2009;29:1418–1423.
98 Schadlu R, Blinder KJ, Shah GK, et al. Intravitreal bevacizumab for choroidal neovascularization in ocular histoplasmosis. Am J Ophthalmol. 2008;145:875–878.
99 Heier JS, Brown D, Ciulla T, et al. Ranibizumab for choroidal neovascularization secondary to causes other than age-related macular degeneration: a phase I clinical trial. Ophthalmology. 2011;118:111–118.
100 Han DP, McAllister JT, Weinberg DV, et al. Combined intravitreal anti-VEGF and verteporfin photodynamic therapy for juxtafoveal and extrafoveal choroidal neovascularization as an alternative to laser photocoagulation. Eye (Lond). 2010:713–716.
101 Rechtman E, Allen VD, Danis RP, et al. Intravitreal triamcinolone for choroidal neovascularization in ocular histoplasmosis syndrome. Am J Ophthalmol. 2003;136:739–741.
102 Thomas MA, Kaplan HJ. Surgical removal of subfoveal neovascularization in the presumed ocular histoplasmosis syndrome. Am J Ophthalmol. 1991;111:1–7.
103 Thomas MA, Grand MG, Williams DF, et al. Surgical management of subfoveal choroidal neovascularization. Ophthalmology. 1992;99:952–968.
104 Thomas MA, Dickinson JD, Melberg NS, et al. Visual results after surgical removal of subfoveal choroidal neovascular membranes. Ophthalmology. 1994;101:1384–1396.
105 Melberg NS, Thomas MA, Dickinson JD, et al. Managing recurrent neovascularization after subfoveal surgery in presumed ocular histoplasmosis syndrome. Ophthalmology. 1996;108:1064–1068.
106 Submacular Surgery Trials Research Group. Surgical removal vs observation for subfoveal choroidal neovascularization, either associated with the ocular histoplasmosis syndrome or idiopathic. I. Ophthalmic findings from a randomized clinical trial: Submacular Surgery Trials (SST) group H trial: SST report no. 9. Arch Ophthalmol. 2004;122:1597–1611.
107 Submacular Surgery Trials Research Group. Surgical removal vs observation for subfoveal choroidal neovascularization, either associated with the ocular histoplasmosis syndrome or idiopathic. II. Quality-of-life findings from a randomized clinical trial: SST group H trial: SST report no. 10. Arch Ophthalmol. 2004;122:1616–1628.
108 Ehlers JP, Maldonado R, Sarin N, et al. Treatment of non-age-related macular degeneration submacular diseases with macular translocation surgery. Retina. 2011;31:1337–1346.
109 Ng EW, Fujii GY, Au Eong KG, et al. Macular translocation in patients with recurrent subfoveal choroidal neovascularization after laser photocoagulation for nonsubfoveal choroidal neovascularization. Ophthalmology. 2004;111:1889–1893.