Chapter 15 Nonintubation Management of the Airway
Airway Maneuvers and Mask Ventilation
I Overview
A Upper Airway Anatomy and Physiology
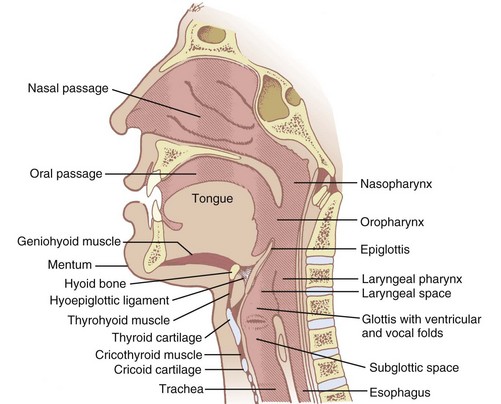
Nonintubation airway management seeks to produce patency to gas flow through the oropharynx, nasopharynx, and larynx without the use of artificial airway devices that extend into the laryngopharynx or trachea. A thorough understanding of upper airway anatomy and physiology is necessary to appreciate the therapeutic maneuvers and devices employed in airway management (Fig. 15-1). More detailed reviews of airway anatomy are found elsewhere in this book and in various atlases and texts.1–3
Gas passes from outside the body to the larynx through the nose or mouth. If through the nose, ambient gas passes through the nares, choanae, and nasopharynx (where it is warmed and humidified). The humidified gas then traverses the oropharynx and hypopharynx (also called laryngopharynx) on its way to the larynx. If through the mouth, the oropharynx and hypopharynx are traversed before entering the glottis. Nasal passages can be obstructed by choanal atresia, septal deviation, mucosal swelling, or foreign material (e.g., mucus, blood). Entry to the oropharynx can be blocked by the soft palate lying against the posterior pharyngeal wall. The pathway of gas by either route can be restricted by the tongue in the oropharynx or the epiglottis in the hypopharynx. These are sites of potential pharyngeal collapse.4–7 Airway manipulation and devices can remedy these causes of obstruction. Laryngeal obstruction related to spasm, however, must be treated by positive airway pressure, deeper anesthesia, muscle relaxants, or endotracheal intubation.
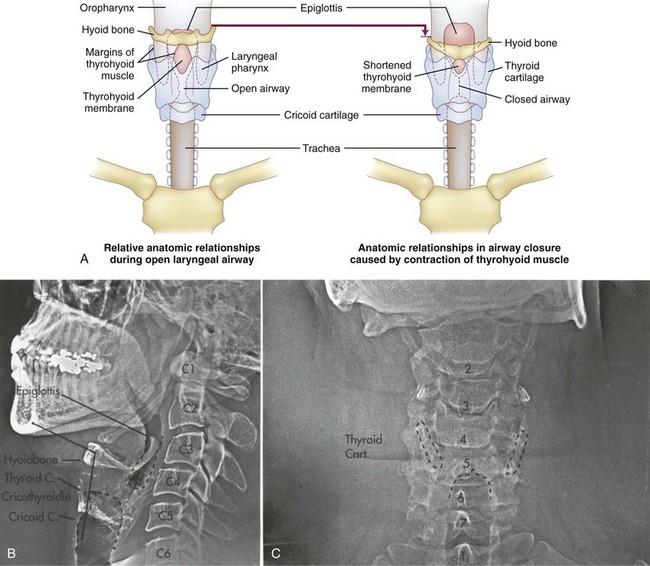
Laryngeal closure is accomplished by the intrinsic or extrinsic muscles of the larynx. Tight closure, as seen in laryngospasm, results from contraction of the external laryngeal muscles, which force the mucosal folds of the quadrangular membrane into apposition (Fig. 15-2). Muscle groups also extend from the thyroid cartilage to the hyoid and cricoid cartilages. When they contract, the interior mucosa and soft tissue (ventricular and vocal folds) are forced into the center of the airway, and the thyroid shield is deformed (compressed inward), providing a spring to reopen the airway rapidly after these muscles relax.8 The larynx closes at the level of the true cords by action of the intrinsic muscles of the larynx during phonation, but this closure is not as tight as the laryngospasm described earlier.
Opening of the pharynx and larynx is achieved by elongating and unfolding the airway from the hyoid to the cricoid cartilage.8 Several muscle groups tether the various airway structures to one another to form a functional airway apparatus. When the head is tilted, the chin and mandible are displaced forward on the temporomandibular joint. This produces maximum stretch at the hyoid-thyroid-cricoid area. The hyoid bone is pulled in an anterior direction along with the epiglottis and base of the tongue, which opens the oropharynx. The ventricular and vocal folds flatten against the sides of the thyroid cartilage, opening the laryngeal airway.8
B Upper Airway Obstruction
1 Pharyngeal Obstruction
In patients susceptible to obstructive sleep apnea, the geometry of the pharynx can be altered during normal sleep.9 Although it is usually oval with the long axis in the transverse plane, the pharynx in patients with obstructive sleep apnea is round or oval with the long axis in the anterior-posterior plane (the lateral walls are thickened).10,11 This obstruction can often be treated effectively with nasal continuous positive airway pressure and with intraoral devices that advance the mandible as much as the jaw thrust maneuver.12–14
2 Hypopharyngeal Obstruction
Hypopharyngeal obstruction has been investigated by placing a nasal fiberscope at the level of the soft palate in anesthetized subjects.15 The epiglottis and the glottic opening can be seen, recorded, and analyzed. The percentage of glottic opening (POGO) seen from this view can be determined. Typically, airflow increases and snoring decreases as POGO increases. However, a POGO of 100% has been documented with airway occlusion, and a POGO of 0% has been documented with no stridor and no obvious impairment to ventilation. Although less than perfect, these evaluations do support the potential for airflow restriction at the hypopharynx and are consistent with the cause being the epiglottis obstructing the airway.
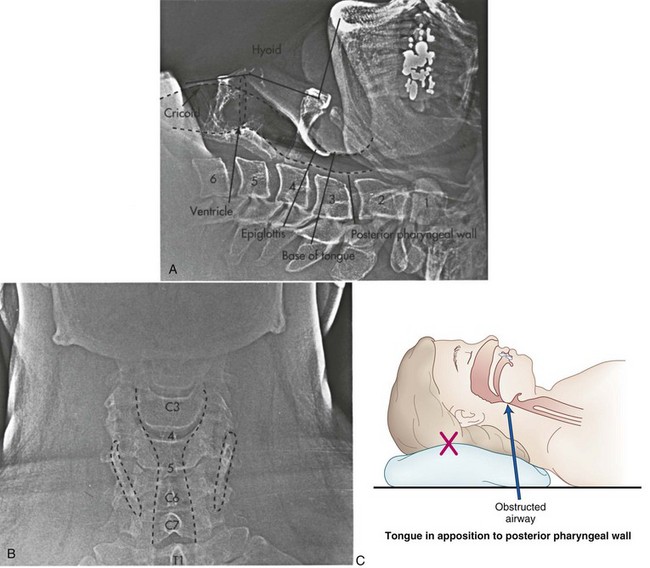
II Nonintubation Approaches to Establish Airway Patency
When the muscles of the floor of the mouth and tongue relax, the tongue may cause soft tissue obstruction by falling back onto the posterior wall of the oropharynx. It is also possible for the epiglottis to overlie and obstruct the glottic opening or to seal against the posterior laryngopharynx. This effect can be exaggerated by flexing the head and neck or opening the mouth, or both (Fig. 15-3), because the distance between the chin and the thyroid notch is relatively short in the flexed position. Any intervention that increases this distance straightens the mentum-geniohyoid-hyoid-thyroid line and therefore elevates the hyoid bone further from the pharynx. The elevated hyoid then secondarily elevates the epiglottis through the hyoepiglottic ligament, potentially alleviating the obstruction.
A Simple Maneuvers for the Native Airway
1 Head Tilt-Chin Lift
The head tilt-chin lift is accomplished by tilting the head back on the atlanto-occipital joint while keeping the mouth closed (teeth approximated) (Fig. 15-4). This technique may be augmented by elevating the occiput 1 to 4 inches above the level of the shoulders (sniffing position) as long as the larynx and posterior pharynx stay in their original position. The head tilt-chin lift is the simplest and first airway maneuver used in resuscitation, but it should be used with extreme caution in patients with suspected neck injuries.
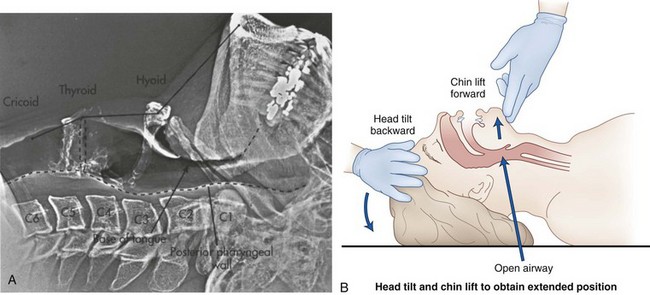
Figure 15-4 A, Lateral xerogram of the head and neck shows the extended position (head tilt) in an awake and supine patient (compare with Fig. 15-3A). The mentum is superior to the hyoid bone, the base of the tongue and the epiglottis are farther from the posterior pharyngeal wall, and the thyroid and cricoid cartilages are at the C4-5 level. The hyoid bone has been raised and elevated from C3-4 to C2-3. B, Diagram of the head tilt-chin lift maneuver.
2 Jaw Thrust
The jaw thrust maneuver more directly lifts the hyoid bone and tongue away from the posterior pharyngeal wall by subluxating the mandible forward onto the sliding part of the temporomandibular joint (mandibular advancement) (Fig. 15-5). The occluded teeth normally prevent forward movement of the mandible, and the thumbs must depress the mentum while the fingers grip the rami of the mandible and lift it upward. This results in the mandibular teeth protruding in front of the maxillary teeth (after the mouth opens slightly). In practice, the insertion of a small airway sometimes makes this procedure easier because it separates the teeth, allowing the mandible to more easily slide forward. In most people, the mandible is readily drawn back into the temporomandibular joint by the elasticity of the joint capsule and masseter muscles. Consequently, this position can be difficult to maintain with one hand.
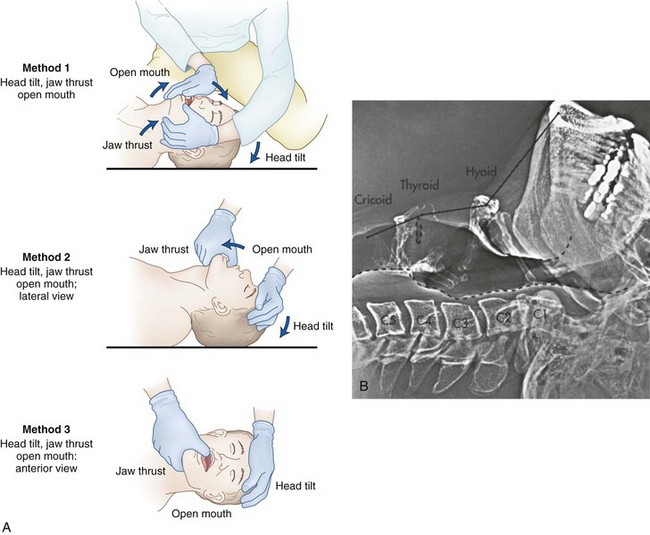
Figure 15-5 The triple airway maneuver includes the head tilt-chin lift, jaw thrust, and open mouth. A, Diagrams show three methods of performing the maneuver: (1) the head extended on the atlanto-occipital joint, (2) the mouth opened to take the teeth out of occlusion, and (3) the mandible lifted upward, forcing the mandibular condyles anteriorly at the temporomandibular joint. B, Lateral xerogram of the head and neck show the extended position with jaw protrusion (compare with Figs. 15-3A and 15-4A). Notice that the mandibular incisors protrude beyond the maxillary incisors and that the mandibular condyles are subluxated anteriorly from the temporomandibular joint.
In up to 20% of patients, the nasopharynx is occluded by the soft palate during exhalation when the airway muscles are relaxed. If the mouth and lips are also closed, exhalation is impeded. In these cases, the mouth must be opened slightly to ensure that the lips are parted. When the head tilt-chin lift, jaw thrust, and open mouth maneuvers are done together, it is known as the triple airway maneuver (see Fig. 15-5). The triple airway maneuver is the most reliable manual method to achieve patency of the native upper airway (Box 15-1).
Box 15-1 Simple Maneuvers for the Native Airway
Head Tilt-Chin Lift
Procedure: With the patient supine, place one hand on the forehead and the first two fingers of the other hand on the underside of the chin. Simultaneously exert upward traction on the chin while tilting the forehead gently backward to extend the head on the atlanto-occipital joint.
Indications: Soft tissue upper airway obstruction
Contraindications: Cervical spine fracture, basilar artery syndrome, infants
Jaw Thrust
Procedure: From above the patient’s head, place the thumbs on the chin and the fingers behind the angle of the jaw bilaterally. Simultaneously open, lift, and displace the jaw forward, subluxating the mandible anteriorly on the temporomandibular joint.
Indications: Soft tissue airway obstruction when a head tilt-chin lift is contraindicated (e.g., fractured neck) or ineffective
Contraindications: Fractured or dislocated jaw, awake patient
Triple Airway Maneuver
Procedure: Perform the head tilt-chin lift followed by a jaw thrust maneuver. Maintain the mouth in an open position after subluxating the mandible during the jaw thrust.
Indications: Expiratory obstruction after a head tilt-chin lift and jaw thrust
Contraindications: Same as for a head tilt-chin lift and jaw thrust
Complications: Same as for a head tilt-chin lift and jaw thrust
3 Heimlich Maneuver
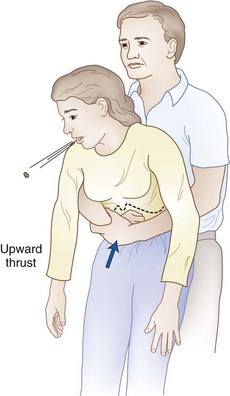
Airway maneuvers can aid in establishing and maintaining airway patency, but they do not relieve an obstruction due to foreign material lodged in the upper airway. Foreign body obstruction should be suspected after a witnessed aspiration when the patient cannot speak, when spontaneous ventilation is absent, or when PPV remains difficult after routine airway maneuvers have been performed. A Heimlich maneuver (subdiaphragmatic abdominal thrusts) is recommended when coughing or traditional means, such as back blows, are unable to relieve complete airway obstruction due to foreign material (Fig. 15-6 and Box 15-2). The goal is to increase intrathoracic pressure sufficiently to simulate a cough. Alternatively, a forceful chest compression in the manner of a rapidly executed bear hug (for upright patients) or a sternal compression (for supine patients) can also be effective. In emergency situations, the failure of one technique to relieve an obstruction should not preclude additional attempts using the various alternatives.
Box 15-2 The Heimlich Maneuver
Procedure: In the upright patient, wrap both arms around the chest with the right hand in a closed fist in the low sternal-xiphoid area and the left hand on top of the fist. With a rapid, forceful thrust, compress upward, increasing subdiaphragmatic pressure and creating an artificial cough.
Indication: Complete upper airway obstruction by a foreign body with impending asphyxia
Contraindications: Partial airway obstruction, fractured ribs (relative), cardiac contusion (relative)
Complications: Fractured ribs or sternum, trauma to liver, spleen, or pancreas
B Artificial Airway Devices
1 Oropharyngeal Airways
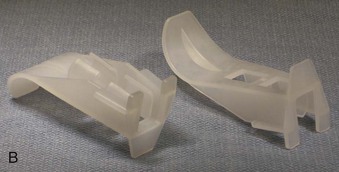
An oropharyngeal airway (OPA) is the most commonly used device to provide a patent upper airway. OPAs are manufactured in a wide variety of sizes from neonatal to large adult, and they are typically made of plastic or rubber (Fig. 15-7). They should be wide enough to make contact with two or three teeth on each of the mandible and maxilla, and they should be slightly compressible so that the pressure exerted by a clenched jaw is distributed over all of the teeth while the lumen remains patent. OPAs are frequently designed with a flange at the buccal (proximal) end to prevent swallowing or over insertion. They also feature a distal semicircular section to follow the curvature of the mouth, tongue, and posterior pharynx so that the tongue is displaced anteriorly (concave side against the tongue). An air channel is often provided to facilitate oropharyngeal suctioning.
The most commonly used OPA in adults is the Guedel Airway (see Fig. 15-7). It has a plastic elliptical tube with a central lumen reinforced by a harder inner plastic tube at the level of the teeth and by plastic ridges along the pharyngeal section. Because the airway is completely enclosed (other than the proximal and distal ends), redundant oral and pharyngeal mucosae cannot occlude or narrow the lumen from the side. Its oval cross section allows the four central incisors to make contact with it during masseter spasm.
The Ovassapian Airway has a large anterior flange to control the tongue and a large opening at the level of the teeth (open posteriorly) to allow a flexible fiberoptic bronchoscope and ETT to be passed through it and later disengaged from the airway (see Fig. 15-7). Consequently, it is often employed during fiberoptic intubations to aid in maintaining upper airway patency.
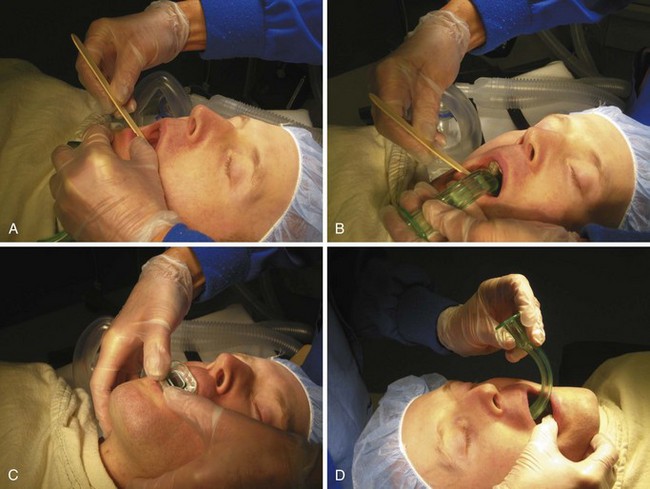
Use of an OPA seems deceptively simple, but the device must be used correctly. The patient’s pharyngeal and laryngeal reflexes should be depressed before insertion to avoid worsening obstruction due to airway reactivity. The mouth is opened, and a tongue blade is placed at the base of the tongue and drawn upward, lifting the tongue off of the posterior pharyngeal wall (Fig. 15-8A). The airway is then placed so that the OPA is just off the posterior wall of the oropharynx, with 1 to 2 cm protruding above the incisors (see Fig. 15-8B). If the flange is at the teeth when the tip is just at the base of the tongue, the airway is too small, and a larger size should be inserted. A jaw thrust is then performed as described previously to lift the tongue off of the pharyngeal wall while the thumbs tap down the airway the last 1 to 2 cm so that the curve of the OPA lies behind the base of the tongue (see Fig. 15-8C). The mandible is then allowed to reduce back into the temporomandibular joint, and the mouth is inspected to ensure that neither the tongue nor the lips are caught between the teeth and the OPA.
An alternative method of placement is to insert the airway backward (convex side toward the tongue) until the tip is close to the pharyngeal wall of the oropharynx. It is then rotated 180 degrees so that the tip rotates and sweeps under the tongue from the side (see Fig. 15-8D). This method is not as reliable as the tongue blade–assisted technique described earlier, and it has the added risk of causing dental trauma in patients with poor dentition.
Two major complications can occur with the use of OPAs: iatrogenic trauma and airway hyperreactivity. Minor trauma, including pinching of the lips and tongue, is common. Ulceration and necrosis of oropharyngeal structures from pressure and long-term contact (days) have been reported.16 These problems necessitate intermittent surveillance during extended use. Dental injury can result from twisting of the airway, involuntary clenching of the jaw, or direct axial pressure. Dental damage is most common in patients with periodontal disease, dental caries, pronounced degrees of dental proclination, and isolated teeth.
2 Nasopharyngeal Airways
The nasopharyngeal airway (NPA) is an alternative airway device for treating soft tissue upper airway obstruction. When in place, an NPA is less stimulating than an OPA and therefore better tolerated in the awake, semicomatose, or lightly anesthetized patient. In cases of oropharyngeal trauma, a nasal airway is often preferable to an oral airway. NPAs are pliable, bent cylinders made of soft plastic or rubber in variable lengths and widths (Fig. 15-9). A flange (or moveable disk) prevents the outside end from passing beyond the nares, thereby controlling the depth of insertion. The concavity is meant to follow the superior side of the hard palate and posterior wall of the nasopharynx. The tip of the airway is beveled to aid in following the airway and minimizing mucosal trauma as it is advanced through the nasopharynx. A narrow NPA is often desirable to minimize nasal trauma but may be too short to reach behind the tongue. As an alternative, an ETT of the same diameter may be cut to the appropriate length to provide a longer airway. A 15-mm adapter should be inserted in the cut end of the ETT to prevent migration of the proximal end beyond the naris (see Fig. 15-9).
Before insertion of an NPA, the nares should be inspected to determine their size and patency and to evaluate for the presence of nasal polyps or marked septal deviation. Vasoconstriction of the mucous membranes can be accomplished with cocaine (which has the added benefit of providing topical anesthesia) or phenylephrine drops or spray. This can also be accomplished by soaking cotton swabs in either of these solutions and then inserting them into the naris (with careful attention to removing the swabs before insertion of the NPA). The NPA is typically lubricated with a water-based lubricant (with or without a water-soluble local anesthetic) and then gently but firmly passed with the concave side parallel to the hard palate through the nasal passage until resistance is felt in the posterior nasopharynx (Fig. 15-10).
III Nonintubation Approaches to Ventilation: Mask Ventilation
A Face Mask Design and Techniques for Use
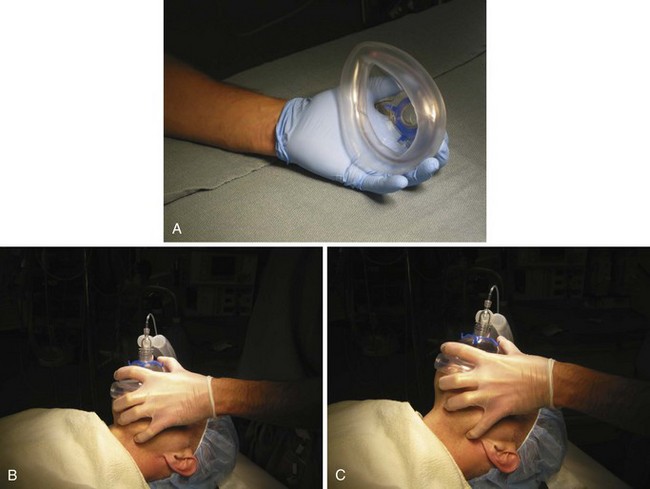
The face mask is typically the starting point for linking a positive-pressure generating device to a patient’s airway. Although face masks have different materials, shapes, types of seal, and degrees of transparency, all are composed of three main parts: a body, a seal (or cushion), and a connector (Fig. 15-11). The body is the main structure of the mask and the primary determinant of the mask’s shape. Because the body rises above the face, all masks increase ventilatory dead space. However, this is rarely clinically significant for spontaneous or controlled ventilation. The seal is the rim of the mask that contacts the patient’s face. The most common type of seal is an air-filled cushion rim. The connector is at the top of the body and provides a 22-mm female adapter for adult and large pediatric masks or a 15-mm male adapter for small pediatric and neonatal masks to connect to a standard breathing circuit. A collar with hooks allows a retaining strap to be attached to hold the mask to the patient’s face (Fig. 15-12). The precise application of the straps (crossed or uncrossed) is a matter of preference and is usually the result of a trial-and-error process to find the best seal for each individual patient.
Several methods are described for holding the mask, but regardless of the precise method chosen, close monitoring for leaks is necessary. Traditionally, the user’s left hand grips the mask with the thumb and index finger around the collar (Fig. 15-13). The left side of the mask fits into the palm, with the hypothenar eminence extending below the left side of the mask. If it does not, the mask may be too large for the user’s hand, and a smaller mask should be tried. The problem with a mask that is too large for the user is that the hypothenar eminence cannot pull the patient’s cheek against the left side of the mask to maintain a seal if pronation is necessary to seal the right side. The patient may require a large mask in which case retaining straps are usually necessary to achieve a satisfactory seal throughout.
The sides of the mask are somewhat malleable to adjust to wide or narrow faces. In edentulous patients, the cheeks are often too hollow to allow for an adequate seal. Edentulous patients also lose vertical dimension to their faces that can be restored with an oral airway. In rare situations, dentures may be left in place to allow a better mask fit (though with the associated risk of dislodgement with consequent airway obstruction by this foreign body). Alternatively, a large mask can be used so that the chin fits entirely within the mask with the seal on the caudal surface of the chin. In this configuration, the cheeks fit within the sides of the mask, and the sides seal along the lateral maxilla and mandible. These maneuvers to make a difficult mask fit possible are often best sidestepped by endotracheal intubation or the use of an LMA, based on clinical judgment (see “Choosing an Airway Technique”). Mask retaining straps can be placed below the occiput and connected to the mask collar to assist the seal, but care should be taken to ensure that the tension on the straps is no more than necessary to achieve a seal.
B Controlled Ventilation by Face Mask
2 Resuscitator Bags
The air-mask-bag unit (AMBU) was described in 1955 by Henning Ruben (Fig. 15-14).17 The AMBU provides an alternative means of controlled ventilation to the standard anesthesia circle system. The bag can be used with a face mask, LMA, or ETT. Its main advantages are that it is self-inflating and readily portable, but it lacks the “feel” (airway compliance and resistance) that the clinician has with a circle system, and it requires a compressed oxygen source to deliver oxygen concentrations above that of room air. Although there are various types of AMBU systems in use, all incorporate one-way valves to allow PPV and to prevent rebreathing. AMBUs are an excellent choice for portable, easy-to-use systems for the delivery of PPV and supplemental oxygen outside of the operating room environment.
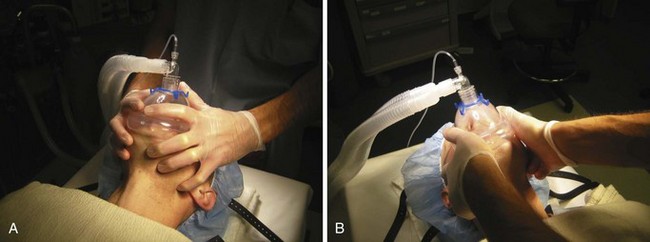
C Determining the Effectiveness of Mask Ventilation
Occasionally, it is sufficiently difficult to maintain an adequate mask seal and patent upper airway with one hand that the patient’s safety is best served with the assistance of a second operator. In this case, the mask and airway are controlled with the first operator’s two hands (one on each side of the face mask) while the second operator ventilates the patient by squeezing the bag (Fig. 15-15). This maneuver can be done from the side of the patient and from above the head. Because this usually is not a stable situation, an alternative airway technique (e.g., placement of an LMA or ETT) usually should be employed.
IV Nonintubation Airway Maintenance in Specific Clinical Scenarios
V Choosing an Airway Technique
Choosing an airway technique for conducting general anesthesia is just as important a medical decision as choosing the drugs and doses to be used. It is based on a risk-benefit analysis of various factors related to the patient, the surgical procedure, the surgeon, and the anesthesiologist involved. The three commonly employed airway techniques that are compatible with a semiclosed or closed breathing system and allow for assisted or controlled ventilation are face mask, LMA, and endotracheal intubation. They vary in their ability to seal the airway, maintain airway patency, and free the hands of the anesthetist. They are associated with different degrees of patient stimulation and potential complications (Box 15-3).
Box 15-3 Airway Management Choices
Face Mask with Oropharyngeal Airway
Indications: Ventilation preceding endotracheal intubation, failed endotracheal intubation, awake or lightly sedated patient requiring a high inspired oxygen concentration
Advantages: Can be done on an awake patient, does not require neuromuscular blocking agents, minimally stimulating to the patient
Disadvantages: Requires constant attention (left hand of anesthesia provider is continuously on the patient’s face or mask), gastric insufflation common if ventilatory pressures frequently exceed 20 cm H2O, minimal protection from aspiration of regurgitated gastric contents
Contraindications: Known increased risk of vomiting or regurgitation, known significant airway obstruction, surgical duration to exceed 60 minutes, adverse patient position (any position other than supine)
Complications: Aspiration risk highest of the three techniques, lip or dental trauma, inadequate airway patency (laryngospasm, upper airway obstruction), facial pressure injury (nerve injury from fingers or retaining straps)
Laryngeal Mask Airway
Indications: Failed endotracheal intubation, difficult mask ventilation
Advantages: Does not require neuromuscular blocking drugs (return to spontaneous ventilation typically faster than with endotracheal intubation), generally smoother emergence than with endotracheal intubation, frees the hands of the anesthesia provider (after placement)
Disadvantages: Cannot reliably generate more than 30 cm H2O of positive pressure, typically requires general anesthetic for placement, does not prevent laryngospasm, risk of atelectasis with extended duration (>2 hours), minimal protection from aspiration of regurgitated gastric contents
Contraindications: Known increased risk of vomiting or regurgitation, known significant airway obstruction, high positive ventilatory pressures required (e.g., laparoscopy)
Complications: Regurgitation and aspiration, laryngospasm, inadequate placement and inadequate ventilation, lingual nerve injury, pharyngeal trauma
Endotracheal Tube Airway
Indications: Increased risk of vomiting or regurgitation, high airway pressures anticipated, inaccessibility of airway during the procedure, need for prolonged controlled ventilation
Advantages: Most secure airway, seals the trachea from the upper airway (lowest risk of aspiration of gastric contents), can remain in place for extended duration (days), can generate the highest inspiratory pressures, laryngospasm not possible after placement
Disadvantages: Most difficult to place of the three techniques, most stimulating to the patient during placement (nociceptive response to tracheal foreign body), coughing during and after extubation and emergence, usually requires neuromuscular blocking drugs to place, can lead to death if esophageal misplacement unrecognized
Contraindications: Unavailability of capnography (relative), significant morbidity from possible minor voice changes (e.g., professional singer) (relative)
Complications: Coughing and straining at emergence and extubation, post-extubation laryngospasm, hypertension/tachycardia, bronchospasm, hoarseness, unrecognized esophageal intubation
VII Clinical Pearls
• An understanding of nonintubation ventilation is critical for the safe management of the airway. It can be applied to many clinical scenarios as a primary management technique or a rescue technique.
• A thorough understanding of upper airway anatomy and physiology is necessary to appreciate the therapeutic maneuvers and devices employed in airway management.
• Airway obstruction can be partial or complete. Partial upper airway obstruction is recognized by noisy inspiratory or expiratory sounds (e.g., snoring). Complete airway obstruction is a medical emergency that requires immediate attention. Signs include inaudible breath sounds; use of accessory neck muscles; sternal, intercostal, and epigastric retraction with inspiratory effort; absence of chest expansion on inspiration; and agitation.
• Two simple maneuvers can relieve upper airway obstruction by lengthening the anterior neck distance from the chin to the thyroid notch: head-tilt-chin lift and jaw thrust.
• When simple airway maneuvers fail to establish upper airway patency, it is often necessary to employ artificial airway devices, such as oropharyngeal airways and nasopharyngeal airways.
• Ventilatory assistance can be achieved through several alternatives other than intubation and typically include bag-mask-valve systems.
• To achieve adequate ventilation using a mask, the user’s left hand grips the mask with the thumb and index finger around the collar. The left side of the mask fits into the palm, with the hypothenar eminence extending below the left side of the mask. To improve airway patency, a chin lift is performed using the middle or ring finger of the left hand. Proper sizing of the mask and continuous observation for leaks are crucial.
• The effectiveness of mask ventilation should be judged by careful attention to and frequent reassessment of many factors: exhaled tidal volume, chest excursion, presence and quality of breath sounds, pulse oximetry, and capnography (when available).
All references can be found online at expertconsult.com.
4 Haponik EF, Smith PL, Bohlman ME, et al. Computerized tomography in obstructive sleep apnea. Correlation of airway size with physiology during sleep and wakefulness. Am Rev Respir Dis. 1983;127:221–226.
5 Issa FG, Sullivan CE. Upper airway closing pressures in obstructive sleep apnea. J Appl Physiol. 1984;57:520–527.
7 Rama AN, Tekwani SH, Kushida CA. Sites of obstruction in obstructive sleep apnea. Chest. 2002;122:1139–1147.
8 Fink BR, Demarest RJ. Laryngeal biomechanics. Cambridge, Mass: Harvard University Press; 1978.
9 Benumof JL. Obesity, sleep apnea, the airway and anesthesia. Curr Opin Anaesthesiol. 2004;17:21–30.
10 Schwab RJ, Gefter WB, Hoffman EA, et al. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis. 1993;148:1385–1400.
11 Schwab RJ, Gupta KB, Gefter WB, et al. Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med. 1995;152:1673–1689.
13 Pitsis AJ, Darendeliler MA, Gotsopoulos H, et al. Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J Respir Crit Care Med. 2002;166:860–864.
15 Meier S, Geiduschek J, Paganoni R, et al. The effect of chin lift, jaw thrust, and continuous positive airway pressure on the size of the glottic opening and on stridor score in anesthetized, spontaneously breathing children. Anesth Analg. 2002;94:494–499.
17 Ruben H. A new nonrebreathing valve. Anesthesiology. 1955;16:643–645.
1 Drake RL, Gray H. Gray’s atlas of anatomy, ed 1. Philadelphia: Churchill Livingstone; 2008.
2 Netter FH. Atlas of human anatomy, ed 5. Philadelphia: Saunders Elsevier; 2010.
3 Fink BR. The human larynx: A functional study. New York: Raven Press; 1975.
4 Haponik EF, Smith PL, Bohlman ME, et al. Computerized tomography in obstructive sleep apnea. Correlation of airway size with physiology during sleep and wakefulness. Am Rev Respir Dis. 1983;127:221–226.
5 Issa FG, Sullivan CE. Upper airway closing pressures in obstructive sleep apnea. J Appl Physiol. 1984;57:520–527.
6 Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002;360:237–245.
7 Rama AN, Tekwani SH, Kushida CA. Sites of obstruction in obstructive sleep apnea. Chest. 2002;122:1139–1147.
8 Fink BR, Demarest RJ. Laryngeal biomechanics. Cambridge, Mass: Harvard University Press; 1978.
9 Benumof JL. Obesity, sleep apnea, the airway and anesthesia. Curr Opin Anaesthesiol. 2004;17:21–30.
10 Schwab RJ, Gefter WB, Hoffman EA, et al. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis. 1993;148:1385–1400.
11 Schwab RJ, Gupta KB, Gefter WB, et al. Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med. 1995;152:1673–1689.
12 Marklund M, Sahlin C, Stenlund H, et al. Mandibular advancement device in patients with obstructive sleep apnea: Long-term effects on apnea and sleep. Chest. 2001;120:162–169.
13 Pitsis AJ, Darendeliler MA, Gotsopoulos H, et al. Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J Respir Crit Care Med. 2002;166:860–864.
14 Randerath WJ, Heise M, Hinz R, Ruehle KH. An individually adjustable oral appliance vs continuous positive airway pressure in mild-to-moderate obstructive sleep apnea syndrome. Chest. 2002;122:569–575.
15 Meier S, Geiduschek J, Paganoni R, et al. The effect of chin lift, jaw thrust, and continuous positive airway pressure on the size of the glottic opening and on stridor score in anesthetized, spontaneously breathing children. Anesth Analg. 2002;94:494–499.
16 Moore MW, Rauscher AL. A complication of oropharyngeal airway placement. Anesthesiology. 1977;47:526.
17 Ruben H. A new nonrebreathing valve. Anesthesiology. 1955;16:643–645.