Chapter 81C Noncolorectal nonneuroendocrine metastases
Overview
Hepatic resection is a well-established therapy for patients with liver metastases from colorectal or neuroendocrine carcinoma. Resection of liver metastases from colorectal cancer (CRC) results in a 3-year survival rate of 30% to 61% and a 5-year survival rate of 16% to 51%, depending on patient selection (Choti et al, 2002; Fong et al, 1997, 1999; Scheele et al, 1995; Schlag et al, 1990; Tomlinson et al, 2007; see Chapter 81A). In patients with hepatic neuroendocrine metastases, 5-year survival rates of 76% have been achieved with surgical resection, and some surgeons occasionally employ liver transplantation (Chamberlain et al, 2000; Lehnert, 1998; see Chapter 81B). In contrast, the role of hepatectomy in patients with liver metastases from noncolorectal, nonneuroendocrine (NCNN) tumors is not well defined, but the number of reports on this topic is increasing.
Series Summarizing Multiple Primary Tumor Types
Most current reports regarding hepatectomy for metastases of NCNN tumors combine multiple primary tumor types in order to have a sufficient number of patients to analyze. Despite this approach, most series are still limited by small numbers or inclusion of patients with neuroendocrine metastases (Benevento et al, 2000; Buell et al, 2000; Elias et al, 1998; Goering et al, 2002; Hamy et al, 2000; Hemming et al, 2000; Karavias et al, 2002; Laurent et al, 2001; Schwartz, 1995; Takada et al, 2001; van Ruth et al, 2001; Yamada et al, 2001).
Goering and colleagues (2002) reported the outcome of 48 patients who had undergone liver resection or ablation for liver metastases from noncolorectal tumors. With a median follow-up of 48 months, the 5-year survival rate was 39%, and the median overall survival was 45 months. No difference was found in survival between patients treated with liver resection versus those treated with cryotherapy. The 3-year survival for patients with primary neuroendocrine (n = 13), genitourinary (n = 16), and soft tissue tumors (n = 15) was 91%, 52%, and 34%, respectively (P = .26).
Elias and colleagues (1998) performed hepatectomy in 147 patients with liver metastases from a noncolorectal primary. Operative mortality was 2%. The overall 5-year survival rate was 36% with the following results for various primary tumors: breast cancer 20% (n = 35), neuroendocrine tumor 74% (n = 27), testicular cancer 46% (n = 20), sarcoma 18% (n = 13), and gastric cancer 20% (n = 11). The authors pointed out that the overall survival was similar to results they obtained in 270 patients who underwent liver resection for metastases of CRC.
Hemming and associates (2000) performed liver resections in 37 patients with NCNN primaries. After a median follow-up of 22 months, the overall 5-year survival rate was 45%. Curative resection and primary tumor type were independent prognostic markers of overall survival in this series. In the subgroup with nongastrointestinal primary tumors (n = 30), the overall 5-year survival rate was 60% compared with 0% for patients with gastrointestinal primary tumors (n = 7; P = .01).
Laurent and coworkers (2001) analyzed the outcome of 39 patients who underwent potentially curative resection of NCNN liver metastases. Patients had primary gastrointestinal (n = 15), genitourinary (n = 12), or miscellaneous (n = 12) tumors. The 5-year survival for the entire group was 35%. Notably, 5-year survival was 100% for patients with a disease-free interval that exceeded 24 months from removal of the primary versus 10% otherwise (P = .01). No other prognostic parameters were identified.
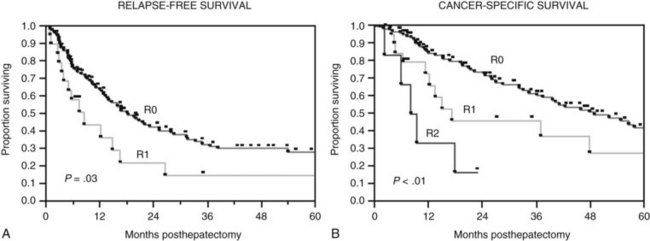
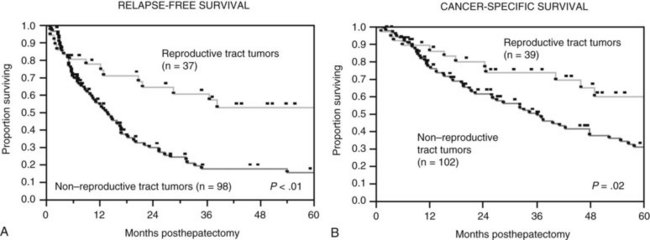
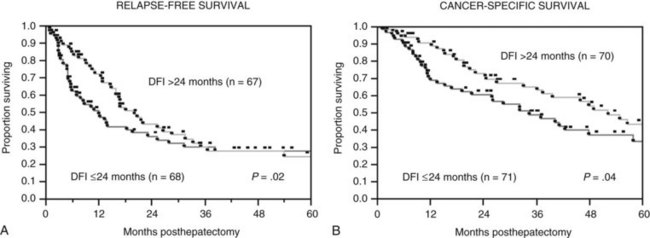
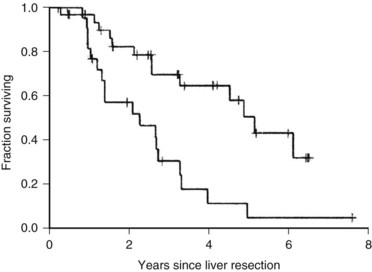
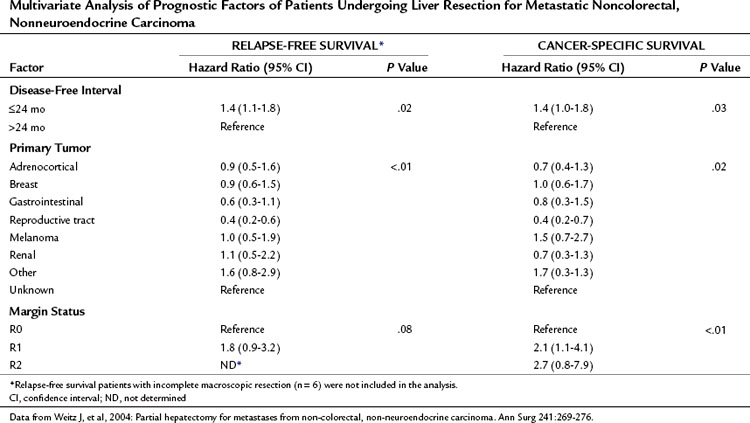
The Memorial Sloan-Kettering Cancer Center (MSKCC) experience of hepatic resection for metastases from NCNN carcinoma was analyzed by Weitz and associates (2004). The objectives of this study were to define perioperative and long-term outcome and to define prognostic factors for survival in 141 patients who underwent resection for liver metastases from NCNN carcinoma during the period from April 1981 through April 2002. Table 81C.1 depicts the primary tumor types. The median operative time was 238 minutes (interquartile range, 180 to 321 minutes), and the median blood loss was 600 mL (interquartile range, 250 to 1420 mL). The median length of hospital stay was 9 days (interquartile range, 7 to 12 days). Of 141 patients, 46 (33%) developed postoperative complications, but the 30-day mortality rate was 0%. The median follow-up was 26 months, with a median follow-up of 35 months. The 3-year relapse-free survival rate was 30% (median, 17 months), and the 3-year cancer-specific survival rate was 57% (median, 42 months). Primary tumor type and length of disease-free interval from the primary tumor were significant independent prognostic factors for relapse-free and cancer-specific survival (Figs. 81C.1 to 81C.3; Table 81C.2).
Table 81C.1 Primary Tumor Type of Patients Undergoing Liver Resection for Metastatic Noncolorectal, Nonneuroendocrine Tumors
| Primary Tumor | No. (%) |
|---|---|
| Breast | 29 (20) |
| Melanoma | 17 (12) |
| Reproductive tract | 39 (28) |
| Testicular | 20 (14) |
| Gynecologic | 19 (14) |
| Ovarian | 12 |
| Endometrial | 4 |
| Cervical | 2 |
| Fallopian tube | 1 |
| Adrenocortical | 15 (11) |
| Renal | 11 (8) |
| Gastrointestinal | 12 (9) |
| Stomach | 3 |
| Duodenal | 1 |
| Pancreatic | 5 |
| Ampullary | 2 |
| Anal | 1 |
| Other | 13 (9) |
| Lung | 4 |
| Salivary gland | 3 |
| Nasopharyngeal | 2 |
| Glottal | 1 |
| Tonsil | 1 |
| Thyroid | 1 |
| Sweat gland | 1 |
| Unknown | 5 (3) |
Data from Weitz J, et al, 2004: Partial hepatectomy for metastases from non-colorectal, nonneuroendocrine carcinoma. Ann Surg 241:269-276.
Table 81C.2 Multivariate Analysis of Prognostic Factors of Patients Undergoing Liver Resection for Metastatic Noncolorectal, Nonneuroendocrine Carcinoma
Laparoscopy might be a reasonable staging tool for patients with NCNN liver metastases. D’Angelica and coworkers (2002) examined 30 patients with potentially resectable NCNN tumors based on preoperative imaging. Nine of these patients had unresectable disease, six of whom were identified by laparoscopy.
Adam and colleagues (2006) reported the results of 1452 patients undergoing hepatic resection for NCNN liver metastases. The primary tumors were most commonly located in the breast (32%) and the gastrointestinal (GI) tract (16%) or were urologic tumors (14%). Operative mortality rate was 2.3%, with a surgical morbidity of 21.5%. Overall 5- and 10-year survival rates were 36% and 23%, respectively. On multivariate analysis, patient age (>60 years), type of primary tumor (non-breast, melanoma, or squamous cell histology), extrahepatic disease, R2 resection, and major hepatectomy were independent adverse prognostic factors. Using these factors, patients could be classified into low risk (0 to 3 risk factors, 5-year survival: 46%), medium risk (4 to 6 risk factors, 5-year survival: 33%), and high risk (>6 risk factors, 5-year survival: <10%; P = .0001).
Series Focused on One Primary Tumor Type
Sarcoma
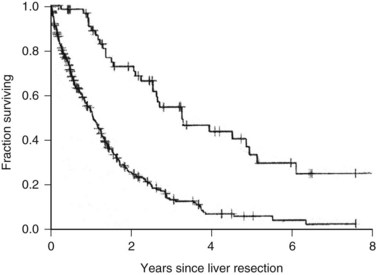
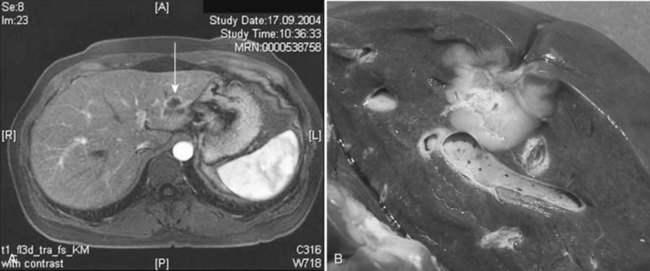
One of the largest surgical series of patients with sarcoma metastatic to the liver was composed of 56 patients who underwent liver resection (DeMatteo et al, 2001). These patients were selected from 331 patients with liver metastases from sarcomas who had been admitted to MSKCC during the years 1982 through 2000. Gastrointestinal stromal tumors (GISTs; Fig. 81C.4) and leiomyosarcomas were the most common histology; no perioperative deaths were reported in patients undergoing complete resection of the tumor, and the 5-year overall survival rate was 30% with a median of 39 months in completely resected patients. Patients who did not undergo complete resection had a 5-year survival of only 4% (Fig. 81C.5). A disease-free interval of less than 24 months was a significant adverse prognostic parameter for survival on univariate and multivariate analysis (Fig. 81C.6).
In a report from Pawlik and colleagues (2006b), 66 patients undergoing liver resection and/or ablation were included; the 5-year disease-free and overall survival rates were 16.4% and 27.1%, respectively. Patients in whom RFA was part of the treatment and patients who did not receive chemotherapy, mostly imatinib mesylate for metastatic GISTs, showed a significantly reduced survival.
The treatment strategy for patients with liver metastases from GISTs has changed since the development of the targeted agent imatinib mesylate, which achieves dramatic tumor response rates (Corless et al, 2004; DeMatteo, 2002) such that imatinib is now the first-line treatment. Resection is considered for patients when they reach the maximal response to imatinib, if all gross tumor can be removed and for those who have immediate or limited acquired resistance to the drug (Antonescu et al, 2005). Patients with mulitfocal resistance to imatinib seem not to beneftit from surgical intervention (DeMatteo et al, 2007).
Breast Cancer
In a small proportion (4% to 5%) of patients with breast cancer, liver metastases are the only sign of disseminated disease (Fig. 81C.7; Elias et al, 2003). Although it has not been formally proven that liver resection prolongs survival for selected patients with liver metastases of breast cancer, 5-year survival was 33% to 61% in more recently published series (Caralt et al, 2008; Elias et al, 2003; Vlastos et al, 2004). Patients with liver metastases from breast cancer receiving chemotherapy only rarely, if ever, survive 5 years (Wyld et al, 2003). Even with aggressive systemic chemotherapy, the median survival for patients with isolated liver metastases of breast cancer was only 23 to 27 months, with time to progression of 8 to 10 months in two more recent trials (Atalay et al, 2003). Resection for liver metastases in this setting may prolong survival for a subset of highly selected patients (Singletary et al, 2003).