Chapter 33 Non-invasive ventilation
Non-invasive ventilation (NIV) is a valuable therapeutic option in the management of acute and chronic respiratory failure – for some diagnoses it is the preferred option. Successful use of NIV in acute respiratory failure (ARF) was first published in 1936,1 and the use of NIV predates the introduction of laryngoscopy (early 1900s) and the widespread use of positive-pressure mechanical ventilation (MV) via an endotracheal tube (1950s).2
NIV is defined as ventilatory support without an (invasive) endotracheal airway. It has an increasingly important role in the short-term management of readily reversible ARF,3,4 and in chronic respiratory failure due to obstructive sleep apnoea (OSA) and neuromuscular disease.
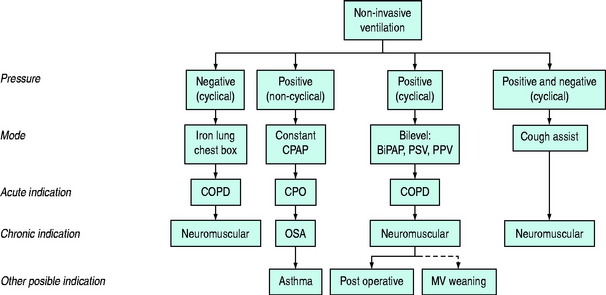
NIV may be achieved either through the delivery of positive airway pressure (Pao) or the application of a negative-pressure generator to the chest (‘chest box’ or cuirass) or body (‘iron lung’). A conceptual framework is shown in Figure 33.1. This chapter deals primarily with the use of positive-pressure NIV to treat ARF.
Negative-pressure generators may be used for the management of acute or chronic respiratory disease.5 Major limitations to the use of negative-pressure generators include the induction of OSA, lack of fractional inspired oxygen (FiO2) control, equipment bulk and size.6 However, external negative-pressure generators suit some patients with chronic respiratory failure, particularly as there is no oral or nasal prosthesis.
The clinical efficacy of NIV depends upon: (1) the mode used; and (2) the nature and severity of the underlying respiratory disorder. Correctly applied, NIV can reduce morbidity and mortality, whereas inappropriate application may delay definitive therapy and adversely affect outcome. An understanding of the physiologic rationale for NIV will assist the clinician in understanding the indications and benefits, and predict the side-effects of the various NIV modes.7,8 Many of the general issues regarding ventilation are discussed in Chapter 27, and this chapter will focus on those issues specific to NIV.
PHYSIOLOGY OF NIV
See Chapter 27 for a more detailed explanation.
This relationship may be rearranged into its individual components, as follows:
where E is the respiratory elastance (inverse of compliance), V is the volume of gas, R is the respiratory and circuit flow-resistance,  is the inspiratory flow rate and PEEPi is the sum of the extrinsic and intrinsic PEEP (≈Pthres).
is the inspiratory flow rate and PEEPi is the sum of the extrinsic and intrinsic PEEP (≈Pthres).
BILEVEL POSITIVE AIRWAY PRESSURE (BPAP)
BPAP allows separate settings for inspiratory (IPAP) and expiratory (EPAP) airway pressure levels, and is conceptually similar to PSV plus CPAP. Respiratory frequency is usually determined by the spontaneous rate but may be time-cycled and independent of patient effort. In some patients BPAP may not be as effective in reducing Pmus as the combination of PSV plus CPAP.2,12
PATIENT–VENTILATOR INTERACTION
This is discussed in Chapter 27, and subdivided into: (1) triggering of inspiration; (2) inspiration; and (3) cessation of inspiration. The only aspect that is specific to NIV arises from mask leaks that may interfere with the ability to sense the end of expiration because there is continued ‘expiratory’ gas flow.
NON-INVASIVE VENTILATION EQUIPMENT
Equipment design varies according to NIV mode and purpose (e.g. critical care or domiciliary setting), and significant variation in performance characteristics have been documented.12,13 The important characteristics of an efficient NIV circuit include:
Many mask designs are also available and the optimal design depends upon the purpose and mode of NIV and patient anatomy and preference. These include intranasal, nasal, oronasal, full-face and helmet (full-head) masks. Desirable features of a mask include light-weight and transparent materials providing a comfortable air-tight seal with minimal dead space and separate inspiratory and expiratory ports to minimise airflow turbulence and rebreathing.13,14 In lung model studies, expiratory ports over the nasal bridge reduce dead space,15 which may prove to be clinically advantageous.
COMPLICATIONS AND ASSESSMENT OF EFFICACY
Contraindications and complications specific to NIV are listed in Table 33.1. Most patients requiring NIV should be managed in a critical care ward with appropriately trained medical and nursing staff. Although the development of sophisticated, portable, non-invasive ventilators makes iteasy to provide NIV in any environment, its benefits may diminish outside the critical care environment.16,17
Table 33.1 Contraindications and complications of non-invasive ventilation
| Contraindications |
NON-INVASIVE VENTILATION AND ACUTE RESPIRATORY FAILURE2,16,18
CARDIOGENIC PULMONARY OEDEMA (CPO)2,8,19
Over 20 prospective randomised controlled trials of NIV in CPO have consistently demonstrated physiologic improvements in hypoxic and hypercapnic respiratory failure, and a significant reduction in the need for intubation, hospital length of stay and improved survival (95% confidence interval (CI) relative risk (RR) = 0.38–0.90).19 Even though the majority of these patients were managed in a critical care setting the average duration of respiratory support was much shorter for NIV (9 ± 11 hours) than those who required MV.20
The optimal mode of NIV in CPO appears to be CPAP alone. The optimal Pao level remains to be resolved, although 10 cmH2O appeared to be safe and effective in the majority of subjects. Whilst the addition of a differential inspiratory pressure (e.g. bilevel21 and PSV22,23) appears to be as effective as CPAP, it does not appear to provide an additional outcome benefit19 and may increase the rate of myocardial infarction24,25 (95% CI RR 0.92–2.42).19 Bilevel NIV and CPAP have equivalent impact on respiratory parameters, but may have different effects on myocardial function.24,25 CPAP reduces preload and afterload9,10 and myocardial catecholamine release26 but the cyclical Pao (of bilevel NIV) may cause preload and afterload to rise and fall during respiration.2,27
Current evidence supports the routine use of mask CPAP in moderate or severe CPO as standard therapy and as the first-line option for respiratory support.16,28
ACUTE RESPIRATORY FAILURE IN CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD)
Both CPAP and PSV reduce Pmus in intubated COPD patients weaning from MV. The importance of NIV in hypercapnic ARF is now supported by at least 14 well-performed prospective randomised controlled studies18,29–31 in over 600 patients. Most investigators have demonstrated a low incidence of side-effects and a significant decrease in intubation rates and in-hospital mortality.31 The meta-analysis of NIV trials reveals significant reductions in mortality (95% CI RR = 0.35–0.76) and the need for intubation (95% CI RR = 0.33–0.53) – the number of patients needed to avoid intubation or death were as few as 4 and 10 respectively.32 Risk reduction appears to be proportional to the severity of respiratory acidosis.33 The incidence of nosocomial pneumonia is lower with NIV34–36 and this may explain some of the mortality reduction associated with NIV.36 Nevertheless, mask intolerance, nursing workload and failure rates are greater than those reported with NIV in CPO.2
Current evidence supports the use of NIV in hypercapnic ARF as a component of standard therapy in COPD subjects. This is supported by many respiratory medicine societies throughout the world,16,28,37 that ‘patients hospitalised for exacerbations of COPD with rapid clinical deterioration should be considered for noninvasive positive pressure [ventilatory support] to prevent further deterioration in gas exchange, respiratory workload and the need for endotracheal intubation’.16
All modes of NIV have been shown to be effective but there are no comparative trials that address the question of optimal mode or pressure level.16 Patients with ARF arising predominantly from airflow obstruction (Pres) and/or threshold load are likely to respond to CPAP. Most patients also have reduced alveolar ventilation, marked hypercapnia or respiratory muscle insufficiency and are therefore likely to benefit from the addition of inspiratory support, i.e. PSV, IPAP or non-invasive positive-pressure ventilation (NIPPV).
NIV is indicated in the presence of respiratory acidosis (pH < 7.37) or persistent breathlessness.32,38 These patients should be managed in a critical care setting where appropriate equipment and skill are available2 and reported outcomes appear better.17,32 The level of inspiratory support (usually 5–15 cmH2O) should be titrated to improve  , as indicated by improvement in tidal volume and pH, and reductions in respiratory rate and PaCO2. Low levels of CPAP (4–8 cmH2O) should be titrated to minimise the patient effort required to trigger inspiratory assistance and the FiO2 titrated to reverse hypoxia.
, as indicated by improvement in tidal volume and pH, and reductions in respiratory rate and PaCO2. Low levels of CPAP (4–8 cmH2O) should be titrated to minimise the patient effort required to trigger inspiratory assistance and the FiO2 titrated to reverse hypoxia.
Early predictors of NIV success in COPD patients include the pH and PaCO2, but not the PaO2, response within the first 2 hours of therapy.32,39 Predictors of NIV failure include mask intolerance, severe acidosis (pH < 7.25), tachypnoea (> 35/min), impaired conscious state and poor clinical response to initial therapy.39 Prior to the commencement of NIV the clinician should develop a clear management strategy for those patients who fail a trial of NIV.
Although reported success rates are high (70–90%), NIV failure (i.e. intubation) appears to increase with the severity of respiratory acidosis.32,38 For the poorly compliant patient, reassurance and explanation together with a trial of different size and/or type of mask, or initiation with lower pressure settings, and brief periods off NIV will sometimes assist. Low-dose anxiolytic drugs may be beneficial where anxiety is a recurrent precipitant of tachypnoea, but should be used with extreme caution because of their respiratory-depressant side-effects.
Late failure (> 48 hours) occurs in 10–20% of patients18,30,39 despite an initial improvement with NIV. This group of patients has a high mortality risk.40 Whether their worse outcome is related to the severity of their underlying disease, or from delayed initiation of MV, remains unclear.
ASTHMA
Asthma is an acute inflammatory lung disease that increases resistive (Pres) and threshold (PEEPi) respiratory work. Physiological and clinical improvement has been demonstrated in acute asthmatics with the application of CPAP41–43 and bilevel NIV.43–45 One randomised controlled trial of bilevel NIV titrated over 30 minutes resulted in significant improvement in forced expiratory volume in 1 second (FEV1) and a lower hospital admission rate.46
The clinical role of NIV in the management of acute asthma and the benefit of differential inspiratory pressure, if any, remains to be clarified. We have found 5 cmH2O CPAP to be effective in moderate to severe asthma not responding to continuous inhaled bronchodilators. Nebulised drugs can be effectively delivered even in the presence of a high-flow NIV circuit.47 Controlled clinical studies with robust end-points are awaited.
ACUTE LUNG INJURY (ALI) AND ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS)
Like CPO, ALI leads to increase in elastic workload (Pel) and, to a lesser extent, resistive workload (Pres) arising from an increase in alveolar–capillary permeability, the release of inflammatory mediators and impaired surfactant function. In contrast to CPO there is little supportive evidence for NIV in ALI and ARDS. Even though the addition of PEEP is important during MV for ALI or ARDS and NIV has a lower prevalence of nosocomial pneumonia,34–36 current data do not support the routine use of NIV in undifferentiated hypoxaemic ARF.48,49
Despite numerous clinical reports of successful use of NIV in the setting of community-acquired pneumonia (without COPD) and other forms of ALI, the failure rate remains high.31,48,50–53 This may reflect the differences in duration, severity and the pathophysiology of pneumonia, ALI and ARDS compared to CPO. Some studies showing apparent benefit have failed to exclude patients with CPO54 or COPD55,56 – specific subgroups known to benefit from NIV.
PNEUMONIA IN THE IMMUNOCOMPROMISED PATIENT
MV is associated with high morbidity and mortality risks in immunocompromised patients.56–58 These patients may benefit from NIV2 through a reduction in intubation and MV,56,57 but it is unclear whether this translates into improved hospital survival56,58 or not.36,57 Whether NIV simply avoids a high-morbidity therapy (i.e. MV)34 or selects those with a more readily reversible form of ARF and those more likely to survive is unclear. Nevertheless it seems reasonable, based on the current data, to offer NIV to these patients.16 Once again, clear guidelines need to be established for the management of those patients who fail a trial of NIV and those in whom MV is deemed inappropriate or futile.
POSTOPERATIVE AND POSTTRAUMATIC ARF
Mask CPAP consistently improves physiological parameters (e.g. oxygenation and respiratory rate) and reduces the risk of intubation in general surgical59 and cardiothoracic patients60 with mild postoperative hypoxic respiratory failure, but evidence for an outcome benefit is lacking. It is possible that the addition of inspiratory support (PSV or BiPAP) may improve survival in certain subgroups, such as postoperative lung resection.61 Many of these patients have underlying COPD, and extrapolation of these results to non-COPD patients awaits further study.
Mask CPAP has been shown to be superior to MV in patients with isolated severe chest trauma,62,63 but the exact role of NIV is unclear. NIV is contraindicated in the presence of other significant injuries such as neurotrauma and intracranial hypertension and in the presence of an untreated pneumothorax.
NIV-ASSISTED WEANING
As a result of the demonstrable benefits of NIV in COPD and the widespread use of invasive PSV to assist weaning from MV, NIV has also been recommended to expedite weaning from MV by allowing early extubation,63 and to treat failed or accidental extubation. The putative advantages relate to reduction in the duration and the risks of MV (e.g. nosocomial pneumonia).
For COPD patients, once again, there appears to be a survival benefit,64 but this is less clear in other groups,65 where controlled studies do not support an overall benefit.16 Although NIV is an option for early weaning it is not a substitute for strategies to improve early access to NIV (to reduce the need for MV) and improve weaning success (to reduce the risk of premature extubation).
NIV AND CHRONIC RESPIRATORY DISEASE
NIV is an important modality for short-term assistance and long-term treatment of severe chronic respiratory failure associated with obstructive and central sleep apnoea syndromes,16,66 and chronic hypoventilation syndromes associated with extrapulmonary disease such as neuromuscular disease,67 and thoracic deformities.68 There appears to be less benefit in chronic parenchymal lung disease, such as (stable) COPD and cystic fibrosis.69
These patients may require short-term MV or NIV in a critical care environment for respiratory support during an acute illness or as an aid to perioperative care. NIV (plus minitracheostomy for secretion removal) may improve outcome compared to intubation and MV70 but failure rates appear to be higher than in acute hypercapnic COPD.71 Alternatively these conditions may be first diagnosed during admission for treatment of severe ARF and, following recovery, will require assessment for long-term NIV.
NIV AND SLEEP APNOEA SYNDROMES72,73
Moderate or severe OSA results in nocturnal hypoventilation and episodic hypoxia that can lead to pulmonary and systemic hypertension, cardiac failure, and daytime hypercapnia and somnolence. Many of these complications can be arrested or reversed through the appropriate use of nocturnal CPAP.16,66,74 Patients with suspected sleep apnoea require accurate assessment by a respiratory physician, including sleep studies, prior to the routine use of domiciliary CPAP. Occasionally bilevel or controlled ventilation will be needed when there is inadequate central respiratory drive. In many patients respiratory drive will improve, and they can then be managed with CPAP after a period of bilevel or controlled ventilation.
NIV AND CHRONIC HYPOVENTILATION SYNDROMES
Domiciliary NIV (predominantly using inspiratory support modes or NIPPV) should be considered in all patients presenting with severe chronic respiratory failure due to neuromuscular disease.67,69,75 Early referral and consideration of domiciliary NIV are recommended because of improved outcomes67,76 and quality of life. In cystic fibrosis patients it may have a role simply as a bridge to organ transplantat.57,68 In direct contrast to the role of NIV in acute exacerbations of COPD, there is little or no benefit of domiciliary NIV in the presence of stable COPD,16,37,71,77 unless one of the former conditions coexists.
Assessment of these patients for domiciliary NIV includes respiratory function tests, blood gas analysis, sleep studies, together with trials of NIV modes and pressure settings. In general, indications for long-term NIV include the demonstration of symptomatic respiratory failure, daytime hypercapnia and a significantly reduced (< 20% predicted) vital capacity. The use of nocturnal or intermittent NIV has been shown to improve daytime respiratory and cardiac function, to improve exercise endurance, to slow the progression of respiratory dysfunction and to reduce the frequency of hospitalisation.67,76
1 Poulton EP. Left-sided heart failure with pulmonary oedema. Its treatment with the ‘pulmonary plus pressure’ machine. Lancet. 1936;231:981-983.
2 Mehta S, Hill NS. Noninvasive ventilation. State of the art. Am J Respir Crit Care Med. 2001;163:540-577.
3 Carlucci A, Richard JC, Wysocki M, et al. Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med. 2001;163:874-880.
4 Demoule A, Girou E, Richard JC, et al. Increased use of noninvasive ventilation in French intensive care units. Intens Care Med. 2006;32:1747-1755.
5 Corrado A, Confalonieri M, Marchese S, et al. Iron lung vs mask ventilation in the treatment of acute on chronic respiratory failure in COPD patients. A multicenter study. Chest. 2002;121:189-195.
6 Brochard L. Negative pressure ventilation. JAMA. 2003;289:983.
7 Duke GJ, Bersten AD. Noninvasive ventilation for acute respiratory failure. Part 1. Crit Care Resusc. 1999;1:187-198.
8 Duke GJ, Bersten AD. Non-invasive ventilation for adult acute respiratory failure. Part 2. Crit Care Resusc. 1999;1:199-210.
9 Buda AJ, Pinsky MR, Ingels NB, et al. The effect of intrathoracic pressure on left ventricular performance. N Engl J Med. 1979;301:453-459.
10 Naughton MT, Rahman A, Hara K, et al. Effect of continuous positive airway pressure on intrathoracic and left ventricular transmural pressures in patients with congestive heart failure. Circulation. 1995;91:1725-1731.
11 Nicholas TE, Power JH, Barr HA. The pulmonary consequences of a deep breath. Respir Physiol. 1982;49:315-324.
12 Calzia E, Lindner KH, Witt S, et al. Pressure–time product and work of breathing during biphasic continuous positive airway pressure and assisted spontaneous breathing. Am J Respir Crit Care Med. 1994;150:904-910.
13 Lofaso F, Brochard L, Hang T, et al. Home versus intensive care pressure support devices. Am J Respir Crit Care Med. 1996;153:1591-1599.
14 Ferguson GF, Gilmartin M. CO2 rebreathing during BiPAP ventilatory assistance. Am J Respir Crit Care Med. 1995;151:1125-1135.
15 Saatci E, Miller DM, Stell IM, et al. Dynamic dead space in face masks used with noninvasive ventilators: a lung model study. Eur Respir J. 2004;23:129-135.
16 American Thoracic Society. International Consensus Conferences in intensive care medicine: noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care. 2001;163:283-291.
17 Plant PK, Owen JL, Parrott S, et al. Cost effectiveness of ward based non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease: economic analysis of randomised controlled trial. Br Med J. 2003;326:956-961.
18 Meduri GU, Turner RE, Abou-Shala N, et al. Noninvasive positive pressure ventilation via face mask. First line intervention in patients with acute hypercapnic and hypoxemic respiratory failure. Chest. 1996;109:179-193.
19 Peter JV, Moran JL, Phillips-Hughes J, et al. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-analysis. Lancet. 2006;367:1155-1163.
20 Bersten AD, Holt AW, Vedig AE, et al. Treatment of severe cardiogenic pulmonary oedema with continuous positive airway pressure delivered by face mask. N Engl J Med. 1991;325:1825-1830.
21 Levitt MA. A prospective, randomized trial of BiPAP in severe acute congestive heart failure. J Emerg Med. 2001;21:363-369.
22 Nava S, Carbone G, DiBattista N, et al. Noninvasive ventilation in cardiogenic pulmonary edema. A multicenter randomized trial. Am J Respir Crit Care Med. 2003;168:1432-1437.
23 Bellone A, Vettorello M, Monari A, et al. Noninvasive pressure support ventilation vs. continuous positive airway pressure in acute hypercapnic pulmonary edema. Intens Care Med. 2005;31:807-811.
24 Mehta S, Jay GD, Woolard RH, et al. Randomized, prospective trial of bilevel versus continuous positive airway pressure in acute pulmonary edema. Crit Care Med. 1997;25:620-628.
25 Sharon A, Shpirer I, Kaluski E, et al. High-dose intravenous isosorbide-dinitrate is safer and better than Bi-PAP ventilation combined with conventional treatment for severe pulmonary edema. J Am Coll Cardiol. 2000;36:832-837.
26 Kaye DM, Mansfield D, Aggarwal A, et al. Acute effects of continuous positive airway pressure on cardiac sympathetic tone in congestive heart failure. Circulation. 2001;103:2336-2338.
27 Duke GJ. Cardiovascular effects of mechanical ventilation. Crit Care Resusc. 1999;1:388-399.
28 British Thoracic Society Standards of Care Committee. Non-invasive ventilation in acute respiratory failure. Thorax. 2002;57:192-211.
29 Bott J, Carroll MP, Keilty SEJ, et al. Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet. 1993;341:1555-1557.
30 Brochard L, Mancebo J, Wysocki M, et al. Non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1995;333:817-822.
31 Keenan SP, Kernerman PD, Cook DJ, et al. Effect of noninvasive positive pressure ventilation on mortality in patients admitted with acute respiratory failure: a meta-analysis. Crit Care Med. 1997;25:1685-1692.
32 Ram FSF, Picot J, Lightowler J, et al. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. 2004.
33 Peter JV, Moran JL. Noninvasive ventilation in exacerbations of chronic obstructive pulmonary disease: implications of different meta-analytic strategies. Ann Intern Med. 2004;141:78-79.
34 Girou E, Brun-Buisson C, Taille S, et al. Secular trends in nosocomial infection and mortality associated with noninvasive ventilation in patients with exacerbation of COPD and pulmonary edema. JAMA. 2003;292:2985-2991.
35 Nourdine K, Combes P, Carton M-J, et al. Does noninvasive ventilation reduce the ICU nosocomial infection risk? A prospective clinical survey. Intens Care Med. 1999;25:567-573.
36 Demoule A, Girou E, Richard JC, et al. Benefits and risks of success or failure of noninvasive ventilation. Intens Care Med. 2006;32:1756-1765.
37 Abramson MJ, Crockett AJ, Frith PA, et al. COPDX: an update of guidelines for the management of chronic obstructive pulmonary disease with a review of recent evidence. Med J Aust. 2006;184:342-345.
38 Lightowler JV, Wedzicha JA, Elliott MW, et al. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. Br Med J. 2003;326:185-190.
39 Confalonieri M, Garuti G, Cattaruzza MS, et al. A chart of failure risk for noninvasive ventilation in patients with COPD exacerbation. Eur Respir J. 2005;25:348-355.
40 Moretti M, Cilione C, Tampieri A, et al. Incidence and causes of non-invasive mechanical ventilation failure after initial success. Thorax. 2000;55:819-825.
41 Martin JG, Shore S, Engel LA, et al. Effect of continuous positive airway pressure on respiratory mechanics and pattern of breathing in induced asthma. Am Rev Respir Dis. 1982;126:812-817.
42 Shivaram U, Miro AM, Cash ME, et al. Cardiopulmonary responses to continuous positive airway pressure in acute asthma. J Crit Care. 1993;8:87-92.
43 Fernandez MM, Villagra A, Blanch L, et al. Noninvasive ventilation in status asthmaticus. Intens Care Med. 2001;27:486-492.
44 Meduri GU, Cook TR, Turner RE, et al. Noninvasive positive pressure ventilation in status asthmaticus. Chest. 1996;110:767-774.
45 Gehlbach B, Kress JP, Kahn J, et al. Correlates of prolonged hospitalization in inner-city ICU patients receiving noninvasive and invasive positive pressure ventilation for status asthmaticus. Chest. 2002;122:1709-1714.
46 Soroksky A, Stav D, Shpirer I. A pilot prospective, randomized, placebo-controlled trial of bilevel positive airway pressure in acute asthmatic attack. Chest. 2003;123:1018-1025.
47 Parkes SN, Bersten AD. Aerosol kinetics and bronchodilator efficacy during continuous positive airway pressure delivered by face mask. Thorax. 1997;52:171-175.
48 Delclaux C, L’Her E, Alberti C, et al. Treatment of acute hypoxemic nonhypercapnic respiratory insufficiency with continuous positive airway pressure delivered by a face mask. A randomized controlled trial. JAMA. 2000;284:2352-2360.
49 Ferrer M, Esquinas A, Leon M, et al. Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. Am J Respir Crit Care Med. 2003;168:1438-1444.
50 Abou-Shala N, Meduri GU. Noninvasive ventilation in patients with acute respiratory failure. Crit Care Med. 1996;24:705-715.
51 Jolliet P, Abajo B, Pasquina P, et al. Non-invasive respiratory support ventilation in severe community-acquired pneumonia. Intens Care Med. 2001;27:812-821.
52 Phua J, Kong K, Lee KH, et al. Noninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive pulmonary disease vs. other conditions: effectiveness and predictors of failure. Intens Care Med. 2005;31:533-539.
53 Antonelli M, Conti G, Moro ML, et al. Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study. Intens Care Med. 2001;27:1718-1728.
54 Kramer N, Meyer TJ, Meharg J, et al. Randomized prospective trial of non-invasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med. 1995;151:1799-1806.
55 Confalonieri M, Potena A, Carbone G, et al. Acute respiratory failure in patients with severe community acquired pneumonia. Am J Respir Crit Care Med. 1999;160:1585-1591.
56 Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever and acute respiratory failure. N Engl J Med. 2001;344:481-487.
57 Antonelli M, Conti G, Bufi M, et al. Noninvasive ventilation for treatment of acute respiratory failure in patients undergoing solid organ transplantation: a randomized trial. JAMA. 2000;283:235-241.
58 Confalonieri M, Calderini E, Terraciano S, et al. Noninvasive ventilation for treating acute respiratory failure in AIDS patients with Pneumocystis carinii pneumonia. Intens Care Med. 2002;28:1233-1238.
59 Squadrone V, Coha M, Cerutti E, et al. Continuous positive air way pressure for treatment of postoperative hypoxemia: a randomized controlled trial. JAMA. 2005;293:589-595.
60 Richter-Larsen K, Ingwersen U, Thode S, et al. Mask physiotherapy in patients after heart surgery: a controlled study. Intens Care Med. 1995;21:469-474.
61 Auriant J, Jallot A, Herve P, et al. Noninvasive ventilation reduces mortality in acute respiratory failure following lung resection. Am J Respir Crit Care Med. 2001;164:1231-1235.
62 Bolliger CT, Van Eeden SF. Treatment of multiple rib fractures. Randomised controlled trial comparing ventilatory with non-ventilatory management. Chest. 1990;97:943-948.
63 Gunduz M, Unlugenc H, Ozalevli M, et al. A comparative study of continuous positive airway pressure (CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest. Emerg Med J. 2005;22:325-329.
64 Nava S, Ambrosino N, Clini E, et al. Noninvasive mechanical ventilation in the weaning of patients with respiratory failure due to chronic obstructive pulmonary disease. A randomized, controlled trial. Ann Intern Med. 1998;128:721-728.
65 Burns KEA, Adhikari NKJ, Meade MO. Noninvasive positive pressure ventilation as a weaning strategy for intubated adults with respiratory failure. Cochrane Database of Systematic Reviews. (issue 4):2003.
66 American Thoracic Society. Indications and standards for use of nasal continuous positive airway pressure (CPAP) in sleep apnoea syndromes. Am J Respir Crit Care Med. 1994;150:1738-1745.
67 Gomez-Merino E, Bach JR. Duchenne muscular dystrophy: prolongation of life by noninvasive ventilation and mechanically assisted coughing. Am J Phys Med Rehabil. 2002;8:411-415.
68 National Association for Medical Direction of Respiratory Care. Clinical indications for non-invasive positive pressure ventilation in chronic respiratory failure due to restrictive lung disease, COPD, and nocturnal hypoventilation – a consensus conference report. Chest. 1999;116:521-534.
69 Madden BP, Kariyawasam H, Siddiqi AJ, et al. Noninvasive ventilation in cystic fibrosis patients with acute or chronic respiratory failure. Eur Respir J. 2002;19:310-313.
70 Vianello A, Bevilacqua M, Arcaro G, et al. Non-invasive ventilatory approach to treatment of acute respiratory failure in neuromuscular disorders. A comparison with endotracheal intubation. Intens Care Med. 2000;26:384-390.
71 Robino C, Faisy C, Diehl J-L, et al. Effectiveness of non-invasive positive pressure ventilation differs between decompensated chronic restrictive and obstructive pulmonary disease patients. Intens Care Med. 2003;29:603-610.
72 Giles Tl, Lasserson TJ, Smith BJ, et al. Continuous positive airway pressure for obstructive sleep apnoea in adults. Cochrane Database of Systemic Reviews. (issue 3):2006.
73 Kaneko Y, Floras JS, Usui K, et al. Cardiovascular effects of continuous positive airway pressure in patients with heart failure and obstructive sleep apnea. N Engl J Med. 2003;348:1233-1241.
74 Granton JT, Naughton MT, Benard DC, et al. CPAP improves respiratory muscle strength in patients with heart failure and central sleep apnoea. Am J Respir Crit Care Med. 1996;153:277-287.
75 Annane D, Chevrolet JC, Chevret S, et al. Nocturnal mechanical ventilation for chronic hypoventilation in patients with neuromuscular and chest wall disorders. Cochrane Database of Systematic Reviews. (issue 1):2000.
76 Aboussouan LS, Khan SU, Meeker DP, et al. Effect of noninvasive positive-pressure ventilation on survival in amyotrophic lateral sclerosis. Ann Intern Med. 1997;127:450-453.
77 Wijkstra PJ, Lacasse Y, Guyatt GH, et al. Nocturnal non-invasive positive pressure ventilation for stable chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. (issue 2):2002.

 ) to reverse respiratory acidosis and hypercarbia
) to reverse respiratory acidosis and hypercarbia ) may be viewed as the summation of the individual forces that must be overcome to generate inspiratory flow, namely: elastic work (or ‘stretch’; Wel), flow-resistive work (airflow obstruction; Wres), and threshold work (Wthres). Since the volume component is constant the equation of motion can be written as:
) may be viewed as the summation of the individual forces that must be overcome to generate inspiratory flow, namely: elastic work (or ‘stretch’; Wel), flow-resistive work (airflow obstruction; Wres), and threshold work (Wthres). Since the volume component is constant the equation of motion can be written as:
 .
.
 . Hypermetabolic states (e.g. trauma, sepsis) increase basal
. Hypermetabolic states (e.g. trauma, sepsis) increase basal  , whereas pulmonary and chest wall diseases increase respiratory workload, and neuromuscular disease impairs respiratory muscle effort. NIV may prevent respiratory failure by counterbalancing the respiratory workload and/or reducing respiratory muscle effort, and thus maintain
, whereas pulmonary and chest wall diseases increase respiratory workload, and neuromuscular disease impairs respiratory muscle effort. NIV may prevent respiratory failure by counterbalancing the respiratory workload and/or reducing respiratory muscle effort, and thus maintain  .
. and elastic work (Pel) as a result of the pre-existing parenchymal damage. Threshold load (PEEPi) is frequently present as a result of airflow obstruction, and is exacerbated during ARF by further increased Wres and respiratory rate. Reversible ARF is a common complication of COPD.
and elastic work (Pel) as a result of the pre-existing parenchymal damage. Threshold load (PEEPi) is frequently present as a result of airflow obstruction, and is exacerbated during ARF by further increased Wres and respiratory rate. Reversible ARF is a common complication of COPD.