78
Non-infectious Granulomatous Disorders, Including Foreign Body Reactions
When histiocytes form granulomas within the skin, the cutaneous disorders are referred to as granulomatous. This group of disorders is further divided into infectious (e.g. mycobacterial infections, dimorphic fungal infections) and non-infectious (e.g. sarcoidosis, granuloma annulare). This chapter focuses on the latter category.
Sarcoidosis
• Cutaneous manifestations occur in >30% of patients and may be the first and/or only sign of the disease (Table 78.1).
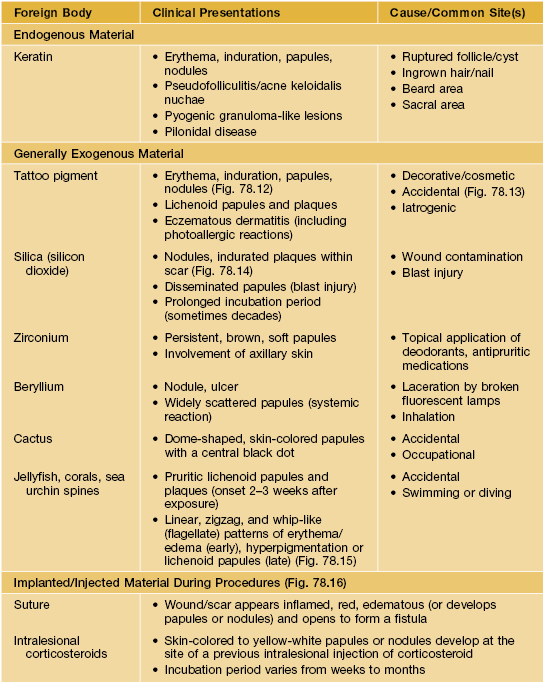
Table 78.1
Clinical features of the major granulomatous dermatitides.
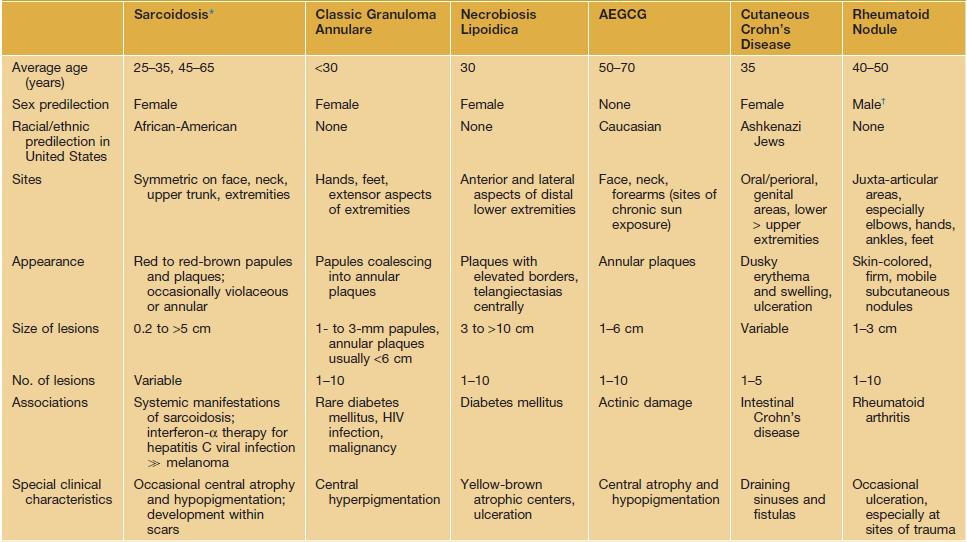
* Clinical variants include lupus pernio and subcutaneous (Darier–Roussy), psoriasiform, ichthyosiform, angiolupoid, and ulcerative sarcoidosis.
† Although rheumatoid arthritis has a female:male ratio of 2–3:1.
AEGCG, annular elastolytic giant cell granuloma.
• The classic lesion is a red-brown papule or plaque with a yellowish color on compression (diascopy), most commonly on the face (Figs. 78.1 and 78.2).





Fig. 78.1 Sarcoidosis. A Cutaneous sarcoidosis usually consists of papules and plaques with a typical reddish-brown color. B, C Lesions often favor the nose, lips, and perioral region. D Hyperpigmented plaques, some of which have scale. E Papules of cutaneous sarcoidosis arising within a tattoo; the differential diagnosis includes foreign body reaction. B, Courtesy, Louis A. Fragola, Jr., MD.

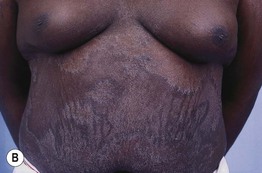

Fig. 78.2 Sarcoidosis – clinical variants. A The hypopigmented variant is more noticeable in individuals with dark skin. B Ichthyosiform presentation with obvious scale. C Coalescing violaceous papules on the nose in lupus pernio; note the notching of the nasal rim. A, Courtesy, Louis A. Fragola, Jr., MD; B, Courtesy, Jean L. Bolognia, MD.
– Lupus pernio – purple to red-brown papules and plaques of the nose, ears, and cheeks; may be beaded along the nasal rim (Fig. 78.2C); associated with chronic pulmonary sarcoidosis (75% of patients) or upper respiratory tract sarcoidosis (50%) and cysts within the distal phalanges.
– Darier–Roussy sarcoidosis (subcutaneous variant) – painless, firm, mobile nodules or plaques.
– Löfgren’s syndrome – hilar adenopathy, fever, migrating polyarthritis, and acute iritis; erythema nodosum is the primary skin finding (see Table 83.2); often spontaneously remits.
– Heerfordt’s syndrome – parotid gland enlargement, uveitis, fever, cranial nerve palsies.
Granuloma Annulare
• Common clinical variants (see Table 78.1) – localized, often acral (Fig. 78.3); subcutaneous on hands, shins, and scalp in children; generalized (Fig. 78.4).


Fig. 78.3 Granuloma annulare. A Annular plaques on the dorsal aspect of the hand, a common location. B Larger lesion on the arm with a figurate border composed of coalescing papules. Note the red-brown color of previously involved skin.
• Less common variants are perforating, often on the hands (Fig. 78.5), patch type on the trunk, and micropapular (Fig. 78.6).

Fig. 78.5 Perforating granuloma annulare. Papules can have a central keratotic plug or umbilication. Courtesy, Ronald P. Rapini, MD.

Fig. 78.6 Papular granuloma annulare of the dorsal hand. Several of the lesions have a central dell. Courtesy, Joyce Rico, MD.
• Generalized granuloma annulare is more likely to be associated with diabetes mellitus or lipid abnormalities (e.g. hypercholesterolemia) compared to other variants; atypical presentations seen in HIV-infected patients (Fig. 78.7).
Necrobiosis Lipoidica
• Typically red-brown plaques on the shins with central clearing that may become yellow and atrophic over time; occasionally, lesions involve the upper extremities, face, and scalp (Fig. 78.8; see Table 78.1).
Annular Elastolytic Giant Cell Granuloma
• Clinically most closely resembles granuloma annulare but lesions have an atrophic, hypopigmented center and sites of predilection are sun-exposed sites including the face, neck, and forearms (Fig. 78.9; see Table 78.1).


Fig. 78.9 Annular elastolytic giant cell granuloma. The border resembles granuloma annulare but the central portion is hypopigmented and/or atrophic (A, B). A biopsy specimen that includes the area outlined in A would contain the three characteristic histologic zones: absence of elastic fibers, granulomatous inflammation, and normal skin. Longitudinal sectioning of the surgical specimen is preferred. B, Courtesy, Kalman Watsky, MD.
• Rx: often ineffective, can try topical and intralesional CS.
Cutaneous Crohn’s Disease
• Specific lesions can be contiguous or noncontiguous (metastatic), and both show granulomas on biopsy.
– Contiguous lesions are seen in the mouth, perioral, anogenital region, and peristomal areas with clinical presentations varying from fissures to cobblestoning to swelling (Figs. 78.10 and 78.11).

Fig. 78.10 Crohn’s disease. Linear ulceration of the mandibular vestibule: the classic oral manifestation of this disease. Courtesy, Charles Camisa, MD.

Fig. 78.11 Cutaneous Crohn’s disease. Note the swelling and violaceous discoloration of the labia majora in this prepubescent girl. Courtesy, Joseph L. Jorizzo, MD.
– Metastatic lesions present as vegetating plaques or nodules, most commonly on the lower extremities (see Table 78.1).
Foreign Body Granulomas
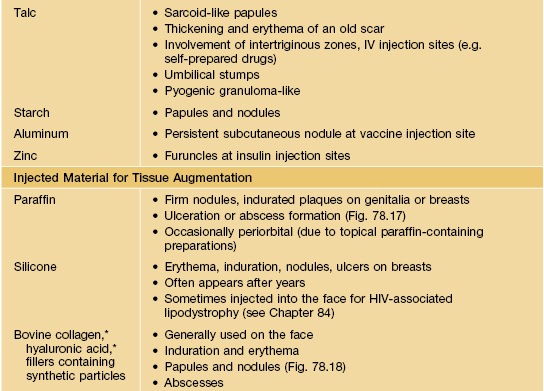
• The most common foreign body is keratin due to ruptured cysts or hair follicles (Table 78.2; Figs. 78.12–78.18).

Fig. 78.12 Granulomatous reaction to the red (cinnabar) portions of a tattoo. During the past several years, cinnabar (mercuric sulfide) has been gradually replaced by cadmium selenide (cadmium red), ferric hydrate (sienna), and organic compounds. Courtesy, Ronald P. Rapini, MD.

Fig. 78.13 Traumatic tattoo of the chin. Bluish discoloration and slight erythema, predominantly due to silica. Courtesy, Ronald P. Rapini, MD.

Fig. 78.15 Coral envenomation. Delayed lichenoid reaction on the calf. The patient accidentally came into contact with a coral reef and developed acute dermatitis that resolved, to be followed 3 weeks later by this severely itchy eruption that responded favorably to intralesional triamcinolone injection. Courtesy, M. A. Abdallah, MD.

Fig. 78.16 Foreign body reactions to polyamide synthetic ‘hair’ implantation. In addition to multiple perifollicular granulomas, there is evidence of chronic folliculitis. Courtesy, Marwa Abdallah, MD.
For further information see Chs. 93 and 94. From Dermatology, Third Edition.