CHAPTER 16 Neuropsychological Testing
Neuropsychological testing as practiced by neuropsychologists is an important, some might say necessary, adjunct to most neurosurgical practices. Neuropsychology has both a clinical and research arm, and over the past century both have been productive in helping humanity achieve a better understanding of the neural basis of cognitive and social functions and the impact of brain disorders on these functions. In this brief chapter I use the term clinical neuropsychologist to refer to a psychologist with specialization in clinical neuropsychology who has a state license to practice and has been “boarded” in clinical neuropsychology. I use the term cognitive neuroscientist to refer to a psychologist or other research scientist who is interested in the brain basis of cognitive, social, personality, or emotional functions but who does not perform clinical evaluations and is not a licensed practitioner. Neuropsychological testing serves a number of functions (e.g., see Table 16-1), including assessment of the cognitive, social-emotional, and sensorimotor abilities of a patient with standardized test instruments; quantification of recovery of function after surgery; prediction of performance in real-life circumstances; hypothesis testing about the major functions of a brain sector; ascertainment of outcome variables in treatment trials; determination of the cognitive or social processes (or both) performed by a brain region that is a candidate for surgical excision or modulation; and prediction of quality of life. Such neuropsychological testing can be relatively abbreviated with the use of screening and similar short-duration tests that take less than an hour to perform or, more typically, be composed of a comprehensive battery of tests to examine most general domains of functioning (e.g., sensorimotor, language, memory, space and visual perception, general intellectual ability, executive functions, and personality), which can take between 3 and 7 hours to complete.
TABLE 16-1 Some Potential Uses of Neuropsychology
| TYPE OF NEUROPSYCHOLOGICAL INPUT | PRACTITIONER | GOAL |
|---|---|---|
| Broad-based or targeted neuropsychological evaluation | Clinical neuropsychologist | Characterization of the patient’s cognition, social skills, personality, and mood. Prediction of outcome |
| Repeated neuropsychological evaluations | Clinical neuropsychologist | Characterize recovery of function over time. Document presurgical and postsurgical (or other intervention) changes in function |
| Neuropsychological rehabilitation | Supervised by a clinical neuropsychologist | Targeted or general improvement in some aspect of neuropsychological function. To facilitate functional outcome |
| Neuropsychological monitoring during surgery | Clinical neuropsychologist or cognitive neuroscientist | Characterize brain areas concerned with specific neuropsychological functions for clinical and/or research purposes |
| Postsurgical neuropsychological testing with implanted electrodes (e.g., on-off stimulation) | Cognitive neuroscientist or clinical neuropsychologist | Characterize brain areas concerned with specific neuropsychological functions for research purposes |
| Postsurgical neuropsychological testing on groups of patients with specific excisions (e.g., anterior temporal lobe) | Cognitive neuroscientist or clinical neuropsychologist | Characterize brain areas concerned with specific neuropsychological functions for research purposes |
Licensed and clinically trained neuropsychologists typically use generally accepted test batteries for their assessment procedures so that interpretation of the test results can be based on a quantitative summary using previously acquired normative data that are typical for a rigidly administered battery, or instead, a neuropsychologist can make a qualitative judgment of the results from a somewhat idiosyncratic test battery (which usually has a core of tests that have normative data). The range of clinically available tests and batteries and an explanation of how to interpret them can be found in many volumes, although a few excellent single-source books are available (e.g., see Lezak and colleagues1). For the vast majority of patients tested by clinical neuropsychologists, a pattern of performance emerges with strengths and weaknesses that enables the clinical neuropsychologist to describe the patient’s current abilities and allows a prediction of future functioning. Cognitive neuroscientists may not be clinically trained and may have somewhat narrow interests (e.g., concerned with identifying the neural substrates of face recognition), but collaboration with these colleagues, in addition to the clinical neuropsychologist, can often lead to much more detailed information about a type of functional representation within a specific brain region, and such information may also have clinical utility if the patient’s lesion falls within that brain region.
Although historically, clinical neuropsychological assessment was also used for diagnostic purposes, with the development of sophisticated imaging, genetic, and related techniques, its contribution to diagnosis is more limited to cases in which imaging may not be helpful, such as in the very early stages of a dementing disease, but some neuropsychological tests may have a degree of sensitivity to change in performance to detect early impairment in these patients (e.g., in incipient idiopathic Alzheimer’s disease or the very early stages of a tumor). Besides evaluation and diagnosis, neuropsychologists also have a prominent role to play in the remediation of functional abilities.2 Such a role includes designing and application of training tasks alone or in combination with other forms of intervention (e.g., drugs, noninvasive brain stimulation techniques, or someday, stem cell therapies) and linking the neuropsychological training techniques to targeted outcomes at work or in the home.
It is also worth mentioning here that at least one myth about the functions of the cerebral cortex needs burial. Conventional wisdom used to proclaim that a neurosurgeon needed to avoid language or eloquent tissue because postsurgical aphasias could significantly affect recovery and outcome. Conversely, removal of relatively large areas of the anterior frontal lobe, particular in the right hemisphere, was relatively acceptable. As the functional role of the right frontal lobe has become more apparent in the past 2 decades, it is clear that certain outcomes (e.g., employment status and interpersonal functioning in the home) may be more impaired by right frontal lesions that compromise the social, cognitive, and emotional abilities supported by that sector of brain than naming deficits.3 Cognitive neuroscientists are playing a major role in revealing the importance of the frontal lobes of the brain, and further findings that will help specify the functions of the human prefrontal cortex to a level equivalent to the functional assignments of the posterior cortex will be forthcoming in the next decade.4 Thus, the clinical neuropsychologist and cognitive neuroscientist can be important team members whose ability to characterize the cognitive, social, and emotional functions of a patient can be invaluable to a neurosurgical practice.
Clinical Assessment
Clinical neuropsychologists use computerized and paper and pencil tests that have undergone varying degrees of standardization so that individual patient results can be compared with a standard normative sample (for the more standardized tests, norms for older adults and adolescents will be included, as well as norms for various patient populations). The assessment can potentially range across a large number of domains of function, from tactile memory to reasoning and problem solving. In general, most domains of ability can be assessed by directly testing the patient. The patient’s social cognition, however, is usually assessed by observation and caregiver or informant reports via scales. Particularly when damage or excisions involve the frontal lobes, the patient’s insight may be compromised, and thus comparison between the patient’s self-report and that of a spouse, parent, or child will be necessary.5
Clinical neuropsychologists may rely on a standard battery of tests that are administered to all patients, such as the Halstead-Reitan Battery, an idiosyncratic, yet standardized (at least on a per test basis) set of tests covering all domains of function, or they may adapt a tailored testing regimen for individual patients, with some tests being applied because of the particular problems of an individual patient.6 Domains of function that can be objectively and quantitatively studied include intelligence, language, perception, visual recognition, attention, sensory and motor skills, spatial ability, emotional processing, and executive functions. Abbreviated tests or batteries such as the Mattis Dementia Rating Scale, Frontal Assessment Battery, or Mini-Mental State Evaluation are also available for use during a simple office visit and rarely take longer than 30 minutes to administer.7 What they lack in sensitivity, breadth, and depth, they make up for by allowing at least a minimal quantification of a patient’s neuropsychological functioning by health practitioners other than neuropsychologists who have some training in or exposure to neuropsychology. In the not too distant future, it should be possible to also objectively assess social skills directly rather than rely only on subjective family reports and patient self-reports. Many standardized batteries will take a morning and afternoon to complete as noted earlier, but this should not be surprising given that our cognitive, social, and sensorimotor abilities are neither simple nor limited in comparison to other species. Alternatively, for both insurance and practical purposes, shorter evaluations can be accomplished, particularly when a question is targeted.
Clinical Interventions
The neuropsychologist may also engage in clinical interventions of various kinds. Such clinical interventions may include cognitive remediation, management of mood states such as anxiety or depression, or vocational-style retraining. As part of rehabilitation, cognitive remediation has taken on significant importance in helping patients recover from brain injuries, such as those suffering from traumatic brain injury or the long-term effects of needed surgical excisions. Although rehabilitation medicine continues to lag behind other specialties in performing efficacy studies for general or specific interventional strategies, even the structuring and attention provided by a clinical neuropsychologist to the patient during the recovery period may help enable that person and family to cope with or compensate for persistent neuropsychological deficits. Neuropsychological interventions are usually time limited, require practice at home, and encourage caregiver involvement. When initially practiced, cognitive remediations required the active involvement of a clinician several times a week for several hours each day. With the advent of the World Wide Web and computer sophistication, many patients are able to import the tasks that they are assigned to their home computer and practice at home, thereby mitigating the need for daily or frequent trips to the clinic. Despite its demonstrated efficacy in individual patients or small groups when the therapy is targeted, replications of efficacy in large samples are often hard to find, there are too many rehabilitation software programs marketed without any proof of effectiveness, and it may be difficult to control for patient and family involvement in the therapy when the majority of practice takes place at home.8 Too often the therapy is administered without a clear vocational or social target, and outcomes can be clouded by this lack of therapeutic mapping to real-life needs.
Prediction of Performance in Real-Life Circumstances
Of course, outcome measures from surgery are not only composed of neuropsychological testing measures but will also include other simple variables ranging from whether the patient survived the surgery to the possibility of return to work and home in an improved or similar capacity as existed before the surgery. Neuropsychological testing is not needed for a judgment of survival, but in conjunction with the use of functional magnetic resonance imaging (fMRI), neuropsychological testing may reveal insights into a patient’s cognitive and behavioral functioning in the transitional states of consciousness (e.g., in locked-in syndrome or the vegetative state) that would otherwise be unobtainable.9 Neuropsychological testing can also predict whether patients will be working or not, their ability to drive (in particular, their judgment in driving situations), their social abilities in certain scenarios, and the likelihood that they can perform specific family tasks. Having been assessed on a standard set of neuropsychological tasks that can offer predictive validity regarding real-life outcome variables that are idiosyncratic across individuals (e.g., type of work) is advantageous for the family.
Advances in Cognitive Neuroscience
Some of the most significant advances in our understanding of the functions of the human brain have been due to the intentional or inadvertent participation of neurosurgeons. For example, studies of patients after excision of brain tissue has led to significant advances in our understanding of the brain circuits critical for reading, object recognition, and memory. Recordings from implanted electrodes have provided important evidence about the neural representation of different forms of knowledge, and even the unintended consequences of surgical procedures have led to such advances as an understanding of the importance of the hippocampus for episodic memory.10 More recently with the advent of the use of implanted brain stimulators for the treatment of Parkinson’s disease and other disorders, it has become possible to investigate the participation of deep structures in several important brain functions by controlling for stimulator settings. Thus, the collaboration of neuropsychologists with neurosurgeons in an effort to disentangle the role of various brain regions and systems in cognition, social behavior, emotion, and more basic sensorimotor processes is crucial for a complete understanding of the functions of the human brain.
Are memory representations stable with a strong relationship between neurons active during encoding and neurons active during representational retrieval? Neurosurgeons have been involved in recording from single neurons in the human hippocampus and adjacent regions. Recently, such recordings have enabled researchers to determine that some of the same neurons that selectively fired during the initial viewing of a video selectively fired again when those specific episodic memories were freely recalled. This finding supported the idea that memories are represented within specific patterns of neural assemblies, with these assemblies consisting of a subset of neurons that represent the memory.11
Study of the cortical representation of language has also been advanced by the investigations of neurosurgeons. For example, Ojemann and colleagues have done substantial mapping of cortical areas in the left hemisphere concerned with specific aspects of language and were able to identify small areas, smaller than those denoted by the traditional Broca-Wernicke area outlines, that were consistently associated with language functions.12 Individual variability in the exact location of these language regions was noted, as was variability in location dependent on sex and intelligence. Thus, anatomic location was insufficient for precise localization; instead, stimulation mapping was recommended.
Although cortical sites have been most amenable to collaborative studies examining cognitive and social functions in the human brain, more recently, deep brain stimulation for Parkinson’s disease and other disorders has allowed study of the role of the basal ganglia and related brain structures in behavior. Thus far the results are mixed, with some studies reporting no cognitive changes and others indicating neuropsychological changes that affect return to work or thinking. The mixed results can be partly blamed on methodologic differences in procedures and study logistics, but this procedure remains a potential tool for teasing out the role of the basal ganglia in behavior rather than sensorimotor skills. For example, Frank and associates noted that deep brain stimulation for Parkinson’s disease relieved the motor symptoms but, at least in some patients, caused an increase in impulsive behavior.13 By detailed studies and computational modeling, they were able to determine that deep brain stimulation interfered only with the normal ability to slow down when faced with decision conflict. Dopaminergic medication did not affect this observation but instead impaired patients’ ability to learn from negative outcomes. Thus, careful cognitive neuroscience investigation of a simple behavior, impulsivity, in collaboration with neurosurgeons resulted in the discovery of two independent mechanisms leading to people becoming impulsive.
Traumatic brain injury, both penetrating and closed, has long been an area of collaboration between neurosurgeons and neuropsychologists that has resulted in scientific advances in our understanding of episodic memory, executive functions such as planning, and social behavior.14 More recently, deep brain stimulation has been attempted in a patient who suffered a traumatic brain injury and was in a minimally conscious state.15,16 Stimulation of the central thalamus in this patient improved limb control, oral feeding, and performance on cognitive measures. Of course, only one case cannot prove efficacy, but it does raise the possibility of deep brain stimulation helping at least a subset of patients in minimally conscious states by increasing their arousal. To objectify more subtle changes, the techniques of cognitive neuroscience would be helpful. This effort may not only be clinically useful in helping the patient communicate better, but as in the other examples presented earlier, it may also lead to a basic scientific advance by improving our understanding of the concepts of arousal and consciousness.
Case Example: Neuropsychology and Cancer
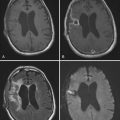
A diagnosis of brain cancer can have significant consequences on brain function. Although surgery and treatment can be effective with some brain cancers, other cancers are extraordinarily difficult to treat and the prognosis is dire. In both cases, the neuropsychologist can play a useful role. In the case of a slow-growing tumor, changes in cognition or social function may be among the first symptoms identified, with formal neuropsychological evaluation being quite sensitive to subtle decrements in performance and behavior.17 Surgical management of a tumor or infiltrative process leads to a surgically defined lesion with its concomitant effects and recovery process that can, as one might anticipate, be precisely quantified by neuropsychological testing. Subsequent postsurgical treatment with radiation, pharmacologic agents, or other methods that may affect brain function, in addition to the effects of the cancer and surgery, can benefit from the quantification of cognitive and social abilities that a neuropsychologist can provide. Although in all these cases careful clinical observation, family reports, and self-reports are essential for gathering information about the effects of interventions, they do not provide objective and sensitive assessments of the cognitive and social functions that may be affected by the cancer and its treatments. A neuropsychologist can be a valuable partner in this regard while also gauging the need for psychological interventions that can be helpful in coping with the mood state changes (e.g., depression or catastrophic reactions) that are a predictable manifestation of life-threatening disease. Finally, neuropsychologists can play an important role in planning rehabilitation and management of treated cancer patients.18
Because therapy for some cancers (e.g., radiation) may produce brain damage,19 structural and functional neuroimaging may aid in identification of the brain sectors sustaining damage, and these imaging results may then be correlated with any measured neuropsychological changes.20 Radiation can also produce cognitive deficits, but some of these deficits may be remediated.21 Memory deficits are a common consequence of radiation therapy, but avoidance of key memory-related regions such as the hippocampus is possible by using image-guided technology.21
As noted earlier, neuropsychologists often play a leading role in the rehabilitation of cognitive and social deficits in patients sustaining brain damage, and there are practical guidelines for developing a pragmatic program of rehabilitation of patients with cancer that takes into account the short and long-term goals of the treatment, prognosis, degree of impairment, competence of patients to monitor their own behavior, and motivation of patients, among other issues.22 In some cases, adjunctive treatment of neuropsychological impairments with pharmacologic agents has also proved beneficial.23
Finally, because neuropsychological evaluation and management of cancer patients can be particularly challenging as a result of a combination of the prognosis, location of brain damage from the cancer, treatments that themselves can cause additional brain damage, and the dynamics of the cancer and treatment effects, special considerations for clinical trials have to be considered and some guidelines have been established.24
Discussion and Future Directions
Much of what I summarized in this chapter can be found in previous editions of this textbook and in much more detail in current neuropsychology or cognitive neuroscience handbooks25,26—that is, a summary of the past and present uses of neuropsychology that are available to neurosurgeons. Where should our collaborations be heading in the future? Two relatively new research areas would seem to be stand out: plasticity and brain-machine interfaces. Plasticity is the study of change in the brain. We already have good knowledge of the variability of our brains in terms of both functional localization and recovery of function.27 However, the exact roles of plasticity are elusive. What is the extent of cognitive maps in the cortex, and what are the principles by which cortical maps expand or contract? How does injury affect maps adjacent to the injured brain sectors or in homologous areas in the uninjured hemisphere? What happens when artificially introduced stem cells integrate within a neural network? Neurosurgeons could play a critically important role in determining the precision of these changes by using cortical mapping and other techniques that have a resolution that is superior to such imaging techniques as fMRI. The second research area of importance is the recently successful introduction of brain-machine interfaces.28 Initially, this effort has gone toward the development of interfaces that can instruct robotic arms to move or facilitate cursor use in patients with paralysis. An electrode array is implanted, and signals are sent to a computer interface, which then interprets the signals and instructs a device. The key to the success of these experiments is reliable interpretation of the neural codes that the computer is receiving and recording of a sufficient number of neurons to permit reliable instructional codes to be transmitted to the computer. This motor control application was obvious as a first attempt at a brain-machine interface, and although much work needs to be done, some promising findings have already emerged, such as those indicating that people can learn to think appropriately so that the computer can encode the output and allow a device to move.29 What about brain-machine interfaces that could aid cognition? Could we develop memory storage devices that could supplement current modes of thinking (some would argue that we can do this now by using handheld computers)? What about interweaving artificial neuronal arrays with real neurons in the cortex or other brain regions to repair them after injury? Ideally, this could all be done with a genetic or epigenetic set of instructions, but this method might be so complicated that it prohibits all but the most general types of instructions, which would be insufficient to promote specific functions or abilities. The neuropsychologist and neurosurgeon have important roles to play in these future efforts.
Birbaumer N, Murguialday AR, Cohen L. Brain-computer interface in paralysis. Curr Opin Neurol. 2008;21:634.
Boller F, Grafman J, editors. Handbook of Neuropsychology, 2nd ed, Amsterdam: Elsevier Science, 2003.
Cicerone K, Levin H, Malec J, et al. Cognitive rehabilitation interventions for executive function: moving from bench to bedside in patients with traumatic brain injury. J Cogn Neurosci. 2006;18:1212.
Dubois B, Slachevsky A, Litvan I, et al. The FAB: a Frontal Assessment Battery at bedside. Neurology. 2000;55:1621.
Farace E. Role of Neuropsychological assessment in cancer patients. In: Meyers A, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:33.
Frank MJ, Samanta J, Moustafa AA, et al. Hold your horses: impulsivity, deep brain stimulation, and medication in parkinsonism. Science. 2007;318:1309.
Gazzaniga MS, editor. The Cognitive Neurosciences III. 3rd ed. Cambridge, MA: MIT Press. 2004:1399.
Gelbard-Sagiv H, Mukamel R, Harel M, et al. Internally generated reactivation of single neurons in human hippocampus during free recall. Science. 2008;322:96.
Grafman J, Christen Y, editors. Neuronal Plasticity: Building a Bridge from the Laboratory to the Clinic. Berlin: Springer. 1999:190.
Jurado MA, Junque C, Vendrell P, et al. Overestimation and unreliability in “feeling of doing” judgments about temporal ordering performance: impaired self-awareness following frontal lobe damage. J Clin Exp Neuropsychol. 1998;20:353.
Kane RL. Standardized and flexible batteries in neuropsychology: an assessment update. Neuropsychol Rev. 1991;2:281.
Khuntia D, Mathew BS, Meyers CA, et al. Brain metastases. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:170.
Levin HS, Grafman J, editors. Cerebral Organization of Function after Brain Damage. New York: Oxford University Press. 2000:392.
Lezak MD, Howieson DB, Loring DW, editors. Neuropsychological Assessment. 4th ed. Oxford, U.K.: Oxford University Press. 2004:1016.
Locke DEC, Cerhan JH, Malec JF. Behavioral strategies and rehabilitation. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:281.
McDonald BC, Saykin AJ, Ahles TA. Brain imaging investigation of chemotherapy-induced neurocognitive changes. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:19.
Meyers CA, Boake C, Levin VA, et al. Symptom management, rehabilitation strategies, and improved quality of life for patients with brain tumors. In: Levin VA, editor. Cancer in the Nervous System. New York: Churchill Livingstone; 1996:4492.
Ojemann G, Ojemann J, Lettich E, et al. Cortical language localization in left, dominant hemisphere. An electrical stimulation mapping investigation in 117 patients. J Neurosurg. 2008;108:411.
Owen AM, Coleman MR. Functional MRI in disorders of consciousness: advantages and limitations. Curr Opin Neurol. 2007;20:632.
Salazar AM, Warden DL, Schwab K, et al. Cognitive rehabilitation for traumatic brain injury: a randomized trial. Defense and Veterans Head Injury Program (DVHIP) Study Group. JAMA. 2000;283:3075.
Schiff ND, Fins JJ. Deep brain stimulation and cognition: moving from animal to patient. Curr Opin Neurol. 2007;20:638.
Schiff ND, Giacino JT, Kalmar K, et al. Behavioural improvements with thalamic stimulation after severe traumatic brain injury. Nature. 2007;448:600.
Schwab K, Grafman J, Salazar AM, et al. Residual impairments and work status 15 years after penetrating head injury: report from the Vietnam Head Injury Study. Neurology. 1993;43:95.
Shaw EG, Butler J, Case LD, et al. Pharmacological interventions for the treatment of radiation-induced brain injury. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:312.
Smith JA, Wefel JS. Neurocognitive testing in clinical trials. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:320.
Squire LR. The legacy of patient H.M. for neuroscience. Neuron. 2009;61:6.
Velliste M, Perel S, Spalding MC, et al. Cortical control of a prosthetic arm for self-feeding. Nature. 2008;453:1098.
Wefel JS, Collins R, Kayl AE. Cognitive dysfunction related to chemotherapy and biological response modifiers. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:97.
Wood JN, Grafman J. Human prefrontal cortex: processing and representational perspectives. Nat Rev Neurosci. 2003;4:139.
1 Lezak MD, Howieson DB, Loring DW, editors. Neuropsychological Assessment. 4th ed. Oxford, U.K.: Oxford University Press. 2004:1016.
2 Cicerone K, Levin H, Malec J, et al. Cognitive rehabilitation interventions for executive function: moving from bench to bedside in patients with traumatic brain injury. J Cogn Neurosci. 2006;18:1212.
3 Schwab K, Grafman J, Salazar AM, et al. Residual impairments and work status 15 years after penetrating head injury: report from the Vietnam Head Injury Study. Neurology. 1993;43:95.
4 Wood JN, Grafman J. Human prefrontal cortex: processing and representational perspectives. Nat Rev Neurosci. 2003;4:139.
5 Jurado MA, Junque C, Vendrell P, et al. Overestimation and unreliability in “feeling of doing” judgments about temporal ordering performance: impaired self-awareness following frontal lobe damage. J Clin Exp Neuropsychol. 1998;20:353.
6 Kane RL. Standardized and flexible batteries in neuropsychology: an assessment update. Neuropsychol Rev. 1991;2:281.
7 Dubois B, Slachevsky A, Litvan I, et al. The FAB: a Frontal Assessment Battery at bedside. Neurology. 2000;55:1621.
8 Salazar AM, Warden DL, Schwab K, et al. Cognitive rehabilitation for traumatic brain injury: a randomized trial. Defense and Veterans Head Injury Program (DVHIP) Study Group. JAMA. 2000;283:3075.
9 Owen AM, Coleman MR. Functional MRI in disorders of consciousness: advantages and limitations. Curr Opin Neurol. 2007;20:632.
10 Squire LR. The legacy of patient H.M. for neuroscience. Neuron. 2009;61:6.
11 Gelbard-Sagiv H, Mukamel R, Harel M, et al. Internally generated reactivation of single neurons in human hippocampus during free recall. Science. 2008;322:96.
12 Ojemann G, Ojemann J, Lettich E, et al. Cortical language localization in left, dominant hemisphere. An electrical stimulation mapping investigation in 117 patients. 1989. J Neurosurg. 2008;108:411.
13 Frank MJ, Samanta J, Moustafa AA, et al. Hold your horses: impulsivity, deep brain stimulation, and medication in parkinsonism. Science. 2007;318:1309.
14 Levin HS, Grafman J, editors. Cerebral Organization of Function after Brain Damage. New York: Oxford University Press. 2000:392.
15 Schiff ND, Fins JJ. Deep brain stimulation and cognition: moving from animal to patient. Curr Opin Neurol. 2007;20:638.
16 Schiff ND, Giacino JT, Kalmar K, et al. Behavioural improvements with thalamic stimulation after severe traumatic brain injury. Nature. 2007;448:600.
17 Farace E. Role of Neuropsychological assessment in cancer patients. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:33.
18 Meyers CA, Boake C, Levin VA, et al. Symptom management, rehabilitation strategies, and improved quality of life for patients with brain tumors. In: Levin VA, editor. Cancer in the Nervous System. New York: Churchill Livingstone; 1996:449.
19 Wefel JS, Collins R, Kayl AE. Cognitive dysfunction related to chemotherapy and biological response modifiers. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:97.
20 McDonald BC, Saykin AJ, Ahles TA. Brain imaging investigation of chemotherapy-induced neurocognitive changes. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:19.
21 Khuntia D, Mathew BS, Meyers CA, et al. Brain metastases. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:170.
22 Locke DEC, Cerhan JH, Malec JF. Behavioral strategies and rehabilitation. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:281.
23 Shaw EG, Butler J, Case LD, et al. Pharmacological interventions for the treatment of radiation-induced brain injury. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:312.
24 Smith JA, Wefel JS. Neurocognitive testing in clinical trials. In: Meyers CA, Perry JR, editors. Cognition and Cancer. New York: Cambridge University Press; 2008:320.
25 Boller F, Grafman J, editors. Handbook of Neuropsychology, 2nd ed, Amsterdam: Elsevier Science, 2003.
26 Gazzaniga MS, editor. The Cognitive Neurosciences III. 3rd ed. Cambridge, MA: MIT Press. 2004:1399.
27 Grafman J, Christen Y, editors. Neuronal Plasticity: Building a Bridge from the Laboratory to the Clinic. Berlin: Springer. 1999:190.
28 Birbaumer N, Murguialday AR, Cohen L. Brain-computer interface in paralysis. Curr Opin Neurol. 2008;21:634.
29 Velliste M, Perel S, Spalding MC, et al. Cortical control of a prosthetic arm for self-feeding. Nature. 2008;453:1098.