CHAPTER 117 NEUROLOGY OF DRUG AND ALCOHOL ADDICTIONS
DEFINITIONS
Substance dependence is of two types. Psychic dependence consists of craving and drug-seeking behavior. Physical dependence consists of somatic withdrawal symptoms and signs. Depending on the drug, psychic and physical dependence can occur together or alone. Tolerance is the need for increasing doses of a drug to produce desired effects or to avoid withdrawal symptoms.
ILLICIT DRUG DEPENDENCE
Intoxication and Withdrawal
Psychostimulants
Psychostimulant withdrawal consists of depression, fatigue, and craving but few objective signs.
Medical and Neurological Complications of Illicit Drug Use
Stroke
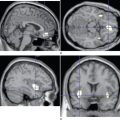
Parenteral drug users are at risk for stroke through systemic complications such as hepatitis, endocarditis, and AIDS. Concomitant tobacco or ethanol abuse also increases stroke risk. In psychostimulant users, ischemic stroke can be cardioembolic as a result of myocardial infarction or arrhythmia. Amphetamine and methamphetamine users are prone to intracerebral hemorrhage in the setting of acute hypertension and high fever. They are also at risk for ischemic stroke secondary to cerebral vasculitis affecting either medium-sized arteries (resembling polyarteritis nodosa) or smaller arteries and veins (resembling hypersensitivity angiitis). In cocaine users, hemorrhagic stroke (including, frequently, rupture of an intracranial saccular aneurysm or a vascular malformation) is also usually secondary to acute surges of blood pressure. Ischemic stroke, however, is seldom secondary to vasculitis and is probably most often the result of acute cerebral vasospasm. Intracerebral and subarachnoid hemorrhage are described in “ecstasy” users in the United States, and both over-the-counter products containing phenylpropanolamine and dietary supplements containing ephedra have been banned by the U.S. Food and Drug Administration because of their association with stroke.
ETHANOL
Ethanol Intoxication
As with other sedative agents, management of severe ethanol overdose requires ventilatory support in an intensive care unit (Table 117-1). Hypovolemia, acid-base or electrolyte imbalance, and abnormal temperature also require attention. Obstreperous or violent patients should not receive sedatives (including neuroleptic agents), which can push them into stupor and respiratory depression. Analeptics are also contraindicated. Hemodialysis or peritoneal dialysis can be considered for BECs above 600 mg/dL; for severe acidosis; for severely intoxicated children; and for concurrent ingestion of methanol, ethylene glycol, or other dialyzable drugs. Ethanol is often taken with other drugs, legal and illicit.
Ethanol Dependence and Withdrawal
Treatment of ethanol withdrawal begins with prevention or reduction of early symptoms (Table 117-2). Benzodiazepines, which have cross-tolerance with ethanol, should be given to recently abstinent alcoholic persons or those with mild early withdrawal symptoms. Neuroleptic agents, which are not cross-tolerant with ethanol and which lower seizure threshold, should be avoided except in patients whose only symptoms are hallucinations or in whom hallucinations have outlasted other withdrawal symptoms. Ethanol should be avoided because it has a low margin of safety and is directly toxic to organs, including the brain.
IM, intramuscularly; IV, intravenously; PO, orally; PRN, as needed.
Delirium tremens is a medical emergency necessitating intensive care (see Table 117-2). In contrast to other withdrawal syndromes, once delirium tremens is present, symptoms are not immediately reversible with any agent. Parenteral benzodiazepines are given in titrated (and sometimes huge) doses. Patients with liver disease are very sensitive to sedative drugs, and in some patients, as delirium tremens clears, hepatic encephalopathy takes its place. General management of delirium tremens includes attention to fluid and electrolyte balance, cardiorespiratory monitoring, and consideration of coexisting illnesses.
Nutritional Disorders Associated with Alcoholism
Many alcoholic patients have deficiencies of thiamine and other vitamins, and a number of neurological disorders have been attributed to these deficiencies. It is increasingly evident, however, that direct ethanol toxicity also plays a role in these disorders. Vitamin deficiency is discussed further in Chapter 109.
Pellagra
Alcoholics with nicotinic acid deficiency develop pellagra, with dermatological, gastrointestinal, and neurological symptoms that include amnesia, delusions, hallucinations, and delirium. Improvement follows treatment with nicotinic acid plus other vitamins, deficiency of which can contribute to symptoms.
Nonnutritional Neurological Complications of Alcoholism
Alcoholic Dementia
On the other hand, several attempts to identify a safe dose threshold for alcoholic dementia, similar to ethanol’s effects on ischemic stroke, found that low-to-moderate amounts reduce the risk of both vascular dementia and Alzheimer’s dementia, whereas higher levels of intake increase the risk. Protection is conferred by spirits, beer, and wine. The protective mechanism is unknown but might be related to the antioxidant properties of alcoholic beverages, especially red wine.
Fetal Alcohol Syndrome
In utero exposure to ethanol causes congenital malformations and delayed psychomotor development. The fetal alcohol syndrome consists of cerebral dysfunction, growth deficiency, and distinctive faces; less often there are abnormalities of the skeleton, heart, urogenital organs, skin, and muscles (Table 117-3). Some children of alcoholic mothers have borderline or retarded intellect without other features of fetal alcohol syndrome (“fetal alcohol effects”), and each anomaly of fetal alcohol syndrome can occur alone or in combination with others.
TABLE 117-3 Major Clinical Features of Fetal Alcohol Syndrome
| Central nervous system | Mental retardation |
| Microcephaly | |
| Hypotonia | |
| Poor coordination | |
| Hyperactivity | |
| Impaired growth | Prenatal for length and weight |
| Postnatal for length and weight | |
| Diminished adipose tissue | |
| Abnormal facies | |
| Eyes | Short palpebral fissures |
| Nose | Short, upturned |
| Hypoplastic philtrum | |
| Mouth | Thin vermilion lip borders |
| Retrognathia in infancy | |
| Micrognathia or prognathia in adolescence | |
| Maxilla | Hypoplastic |
Treatment of Chronic Alcoholism
Brust JCM. Ethanol. In: Spencer PS, Schaumburg HH, editors. Experimental and Clinical Neurotoxicology. 2nd ed. Baltimore: Williams & Wilkins; 1999:541-557.
Brust JCM. Neurological Aspects of Substance Abuse, 2nd ed. Boston: Butterworth-Heinemann, 2004.
Cami J, Farré M. Drug addiction. N Engl J Med. 2003;349:975-986.
Graham AW, Schultz TK, Mayo-Smith MF, et al, editors. Principles of Addiction Medicine, 3rd ed., Chevy Chase, MD: American Society of Addiction Medicine, 2003.
Kosten TR, O’Connor PG. Management of drug and alcohol withdrawal. N Engl J Med. 2003;348:1786-1795.