Nerve Block at the Ankle
Technique
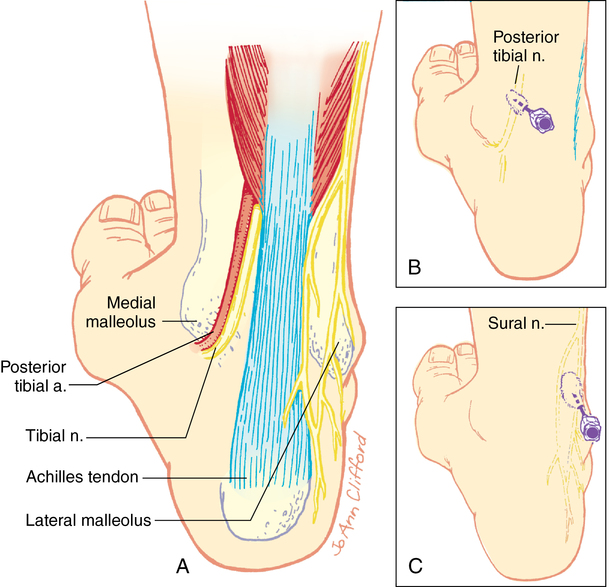
The tibial nerve supplies the sole and plantar portions of the toes up to the nails. It lies behind the posterior tibial artery anteromedial to the Achilles tendon and deep to the flexor retinaculum, which must be penetrated for a successful block (Figure 130-1).
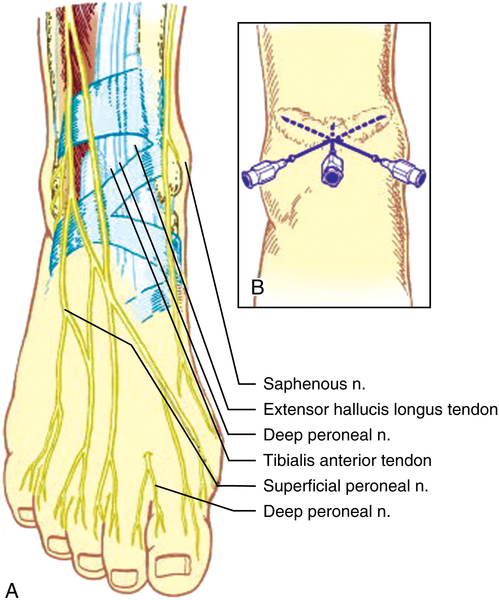
The deep peroneal, superficial peroneal, and saphenous nerves can all be blocked using a single injection site. The deep peroneal nerve courses midway between the malleoli before assuming a position between the anterior tibial tendon and the extensor hallucis longus tendon beneath the extensor retinaculum at the dorsum of the foot. It innervates the short extensors of the toes and provides skin sensation to the interdigital cleft between the great and second toes. With the patient dorsiflexing the foot, the tendons of the anterior tibial and extensor hallucis longus muscles can be readily identified at a level just above a line connecting the malleoli. The pulsation of the anterior tibial (dorsalis pedis) artery will often be felt. The nerve is lateral to the artery and deep to the extensor retinaculum. A 25G, 3-cm to 5-cm needle is inserted perpendicular to skin, as depicted in Figure 130-2. A loss of resistance will often be felt during passage through the extensor retinaculum, at which time between 3 mL and 5 mL of local anesthetic agent is injected.