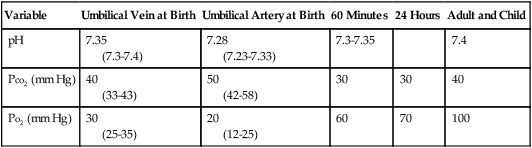
Two maternal uterine arteries supply the placenta—oxygenated blood travels from the mother through the placenta; O2 diffuses across the placenta, binds with neonatal hemoglobin, and is then carried by a single umbilical vein to the body of the fetus. Deoxygenated blood is returned from the fetus to the placenta by two umbilical arteries. As one would expect, at birth, umbilical arterial blood is lower in pH and O2 and higher in CO2 compared with umbilical venous blood (Table 198-1). Umbilical cord blood gas measurements can serve to assess the fetal condition immediately after delivery. Umbilical arterial measurements represent the fetal condition, whereas umbilical vein measurements would represent the maternal condition if the blood were withdrawn prior to cross-clamping the umbilical cord, as well as uterine placental gas exchange.
Table 198-1
Newborn Blood Gas Values
| Variable |
Umbilical Vein at Birth |
Umbilical Artery at Birth |
60 Minutes |
24 Hours |
Adult and Child |
| pH |
7.35
(7.3-7.4) |
7.28
(7.23-7.33) |
7.3-7.35 |
|
7.4 |
| PCO2 (mm Hg) |
40
(33-43) |
50
(42-58) |
30 |
30 |
40 |
| PO2 (mm Hg) |
30
(25-35) |
20
(12-25) |
60 |
70 |
100 |
The majority of births do not require active intervention to establish adequate cardiorespiratory function in the newborn because most newborns undergo a relatively smooth physiologic transition at birth. However, it is of utmost importance to have skilled practitioners available at the time of birth to provide dedicated assessment and resuscitation of the newborn as needed. Such individuals should be capable of managing the airway and have a working knowledge of neonatal physiology and pathology, including vital sign parameters, laboratory values, common congenital anomalies, and their immediate implications. Adequate equipment and resources should be available and checked prior to delivery and should include, at the very minimum, airway supplies (e.g., appropriately sized laryngoscopes, tracheal tubes, and masks), a warming device, suction catheters connected to a suction system, O2, and the ability to provide positive-pressure ventilation, in addition to emergency medications.
When the infant is born, initial maneuvers—such as suctioning of the nose, mouth, and pharynx, as well as stimulation (flicking the feet or rubbing the back)—may be necessary to facilitate regular spontaneous breathing. Infants not responding to such measures may require a range of therapies, including administration of O2, bag-mask ventilation, tracheal intubation and suctioning, chest compressions, and pharmaceutical intervention. Simultaneously, the infant’s color, heart rate, and respiratory effort should be assessed. The goals of such resuscitative efforts are to prevent hypoxic or ischemic injury and to restore adequate spontaneous respiration and cardiac output.
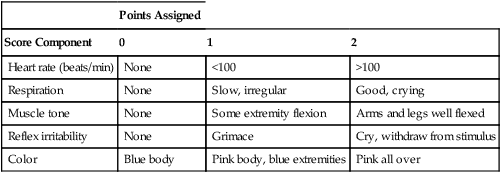
The Apgar scoring system, a rapid assessment tool based on physiologic responses to birth, is used to evaluate the need for resuscitation of a newborn. Created and first utilized in 1953 by an anesthesiologist, Dr. Virginia Apgar, the absolute utility of the system remains in debate today. At intervals of 1 min and 5 min after birth, an experienced and qualified examiner evaluates five physiologic parameters (Table 198-2). Although this assessment may be helpful in evaluating newborns in need of attention, patients may require immediate resuscitation prior to the 1-min scoring.
Table 198-2
Apgar Scoring System
| |
Points Assigned |
| Score Component |
0 |
1 |
2 |
| Heart rate (beats/min) |
None |
<100 |
>100 |
| Respiration |
None |
Slow, irregular |
Good, crying |
| Muscle tone |
None |
Some extremity flexion |
Arms and legs well flexed |
| Reflex irritability |
None |
Grimace |
Cry, withdraw from stimulus |
| Color |
Blue body |
Pink body, blue extremities |
Pink all over |
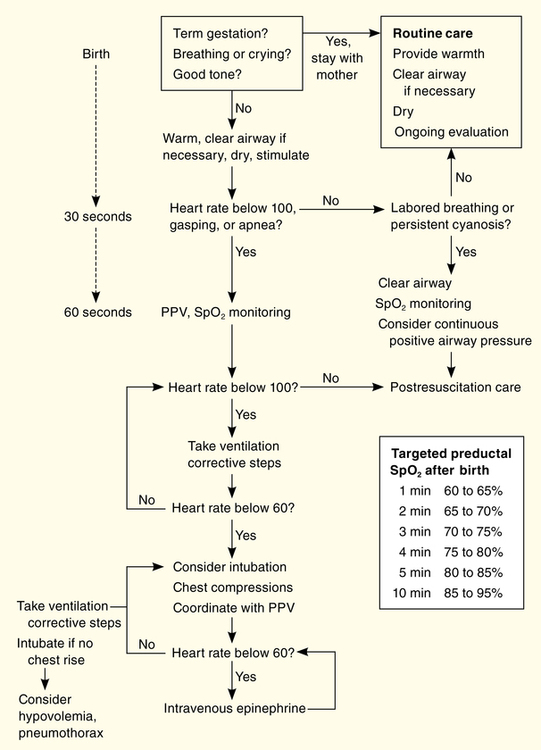
Guidelines for neonatal resuscitation require simultaneous and continuous assessment and treatment (Figure 198-1), which generally consists of a simplified ABCD approach that requires some qualification and clarification. The fundamental principles include evaluating the airway, establishing effective respiration (breathing), determining adequate circulation, and administering medications (drugs).
A review of maternal and prenatal history conducted prior to the neonate’s birth may guide resuscitation efforts. Initially, an infant should be placed in a warmer with his or her head down and the head slightly extended. The neonate’s oropharynx should then be suctioned, while she or he is stimulated and assessed (color, heart rate, respiration).
Meconium staining of amniotic fluid necessitates immediate suctioning of the hypopharynx, nose, and mouth. The decision to perform tracheal suctioning was previously based upon the quality of the meconium present; however, that decision is now based upon the infant’s appearance. If the infant is vigorous, has adequate respiratory effort, and has a heart rate of more than 100 beats/min, tracheal intubation to attempt to aspirate possible meconium should not be attempted. However, if the infant’s respiratory rate and heart rate are depressed and the infant has poor tone, intubation should be undertaken and further tracheal suctioning performed.
The infant’s breathing should be closely monitored and, if necessary, a patent airway should be established by suctioning or intubation. Adequate breathing should be ensured by use of tactile stimulation or positive-pressure ventilation by bag-mask or tracheal tube. Sufficient circulation should be maintained with chest compressions and medications, if required. For further details, refer to the steps outlined in Figure 198-1.
If the infant’s condition deteriorates or does not improve over 30 sec, efforts should be escalated. Currently, room air is recommended for resuscitation and if there is no increase in heart rate or in oxygenation as measured by a pulse oximeter, then supplemental O2 should be considered. Pressures as high as 30 to 40 cm of H2O may be required to ensure adequate ventilation at a rate of 40 to 60 breaths/min. Beware of forcing excessive air into the stomach if performing bag-mask ventilation. Adequate chest rise, symmetrical breath sounds, and presence of end-tidal CO2 should be established.
Chest compression and medications are not needed for most neonates who have mild to moderate cardiac or respiratory depression at birth. Typically, most bradycardia is secondary to hypoxia and responds to effective ventilation. If the heart rate remains lower than 60 beats/min despite adequate ventilation and chest compressions, administration of epinephrine, volume expansion (10 mL/kg of an isotonic crystalloid), or both may be considered. The recommended dose of intravenously administered epinephrine is 0.01 to 0.03 mg/kg per dose. Doses of up to 0.1 mg/kg by tracheal tube may be used if necessary. In rare instances, an opioid antagonist or vasopressors may prove useful. Following resuscitation, the infant may require admission to a neonatal intensive care unit, based on the reasons for and circumstances of the resuscitation.