50
Neonatal care
Introduction
Good-quality neonatal care is extremely important, and may have key implications for the rest of a baby’s life. Those born prematurely need skilled intensive support, and those born with presumed hypoxia need resuscitation, prompt assessment and appropriate subsequent care. The early neonatal period is often the time when congenital abnormalities become apparent and precise diagnosis and management can make a difference to the quality of life, or even influence whether the baby will live or die. The aim of this chapter is not to provide a comprehensive guide to neonatal care, but rather to highlight some of the more common neonatal problems which can occur.
It is essential that the obstetrician, midwife, paediatrician, neonatologist and neonatal nurse collaborate closely as a team. High-quality communication is essential if decision-making is to be optimized.
The transition at birth
The apparent ease with which most babies make the transition from fetal to neonatal life conceals a host of complex physiological changes in virtually every system. Several relatively common neonatal disorders are related to difficulties with this transition.
Respiratory system
The fetal lung at term contains about 100 mL of liquid. This equals the functional residual capacity and in a sense, the fetal lung can be said to form around a liquid cast of the future air spaces. Lung fluid is formed by alveolar cells, and fluid is essential for normal lung growth and development.
The fluid must be cleared at birth to make way for air, and failure to do so leads to breathlessness. This is known as transient tachypnoea of the newborn (TTN). It may last for a day or two, and is commoner after elective caesarean section.
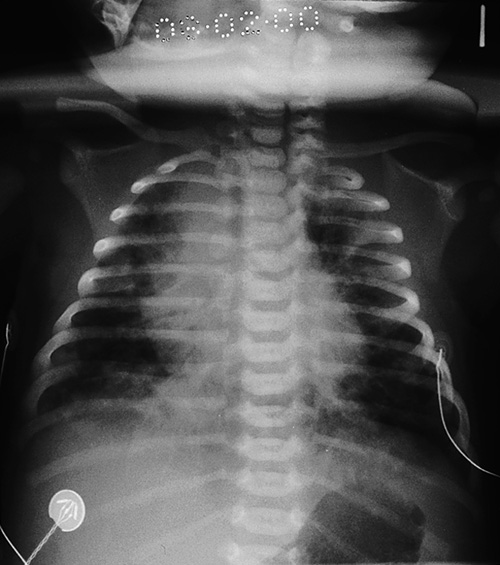
Respiratory distress syndrome (RDS) is caused by a deficiency of surfactant and is commoner in pre-term infants (0.1% at term vs 30% at 28 weeks). Surfactant, a complex lipoprotein consisting largely of phosphatidyl choline, is synthesized by type II pneumocytes within the alveoli and is important in reducing surface tension, allowing the alveolus to expand. Hypoxia, acidosis and hypothermia reduce surfactant production; antenatal steroids increase production and thereby reduce the incidence of RDS. Clinically there is tachypnoea, grunting and intercostal recession commencing within the first 4 h of life, low oxygen saturations requiring oxygen and the chest X-ray demonstrates a generalized reticulogranular appearance referred to as like ‘ground glass’ (Fig. 50.1). Some babies improve with supplemental oxygen or continuous positive airways pressure (CPAP), but increasing respiratory distress and oxygen requirements are indications for intubation and administration of artificial surfactant via an endotracheal tube.
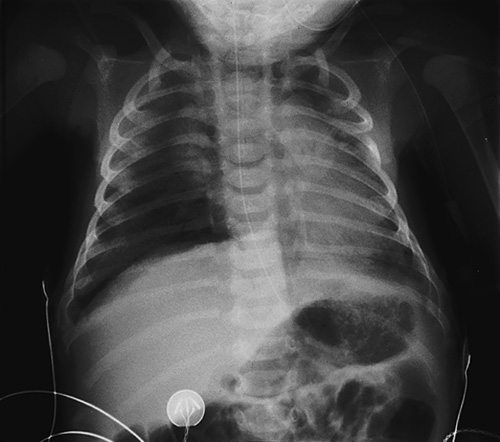
Fig. 50.1Respiratory distress syndrome following emergency caesarean section.
The mother had diabetes, which predisposes to respiratory distress syndrome. Note the ground-glass appearance of the lungs.
Meconium aspiration syndrome is also a potentially serious respiratory complication. In utero, meconium is usually retained within the colon. Although it may be passed through the sphincter under physiological conditions, particularly after 40 weeks, it also has an association with fetal hypoxic stress. Meconium is irritative to the neonatal lungs and may lead to a pneumonitis, the meconium aspiration syndrome (Fig. 50.2). Clinical features range from mild neonatal tachypnoea to severe respiratory compromise. The incidence is probably unrelated to fetal pH (and indeed the majority of babies with meconium aspiration syndrome are not acidotic at delivery) but the syndrome is more likely to be severe if there is associated acidosis. It is also more severe when the meconium is thick. Treatment is with oxygen, mechanical ventilation, surfactant therapy (as meconium can displace or inactivate endogenous surfactant) and, if very severe, extracorporeal membrane oxygenation ± pulmonary lavage.
Cardiovascular system
The switch from fetal to neonatal circulation is normally made rapidly after birth. The key event is relaxation of the smooth muscle in the pulmonary blood vessels, which is triggered by the entry of oxygen into the lung with the first breath (note this paradoxical response to oxygen, which is the opposite to that of all other blood vessels).
In some babies, especially when there has been prolonged fetal hypoxia, this circulatory switch does not occur and may itself lead to further hypoxia. This condition is known as persistent fetal circulation and is difficult to distinguish clinically from congenital cyanotic heart disease.
Genitourinary system
Although the fetal kidney is important in maintaining the amniotic fluid volume, it has a negligible role in the excretion of waste products. After birth, the kidney must excrete all the body’s waste, as well as conserve fluid. In a baby born at term, the kidney is just able to manage this role, although there is always an initial rise in the blood urea and creatinine concentrations. The maximum urine osmolality, which the newborn can attain is about 600 mmol/L (compared with 1800 mmol/L in the adult) and it is therefore not surprising that dehydration and electrolyte disturbances are common complications of neonatal illness.
Gastrointestinal system
The fetus swallows amniotic fluid at about the same rate as it is produced, and deficiencies in fetal swallowing result in polyhydramnios. If there has been polyhydramnios, the baby should be examined for swallowing problems and should have an orogastric tube passed in order to exclude complete oesophageal atresia.
Haematological system
The term fetus has a high haemoglobin concentration, at around 18 g/dL. This is a response to the low arterial oxygen tension (3–4 kPa) which characterizes the latter part of intrauterine life. Once the oxygen tension rises after birth, this high haemoglobin is no longer needed, and falls to around 10 g/dL by about 8 weeks of age.
The white cell count at birth is high (12–20 × 109/L) and polymorphs predominate. By 4 days of age, it is usually in the range 7–12 × 109/L and is mainly lymphocytic.
Routine care at birth
There are several routine observations and procedures to perform on the newborn shortly after birth, but, providing the baby does not need to be resuscitated, none of them should be allowed to prevent the mother from seeing and holding her baby as soon as possible.
Assessment
The baby’s condition at 1 and 5 min of age is assessed by means of the Apgar score (see Table 49.1). The purpose of this is to have a reasonably objective record of how the baby initially responded to the challenge of extrauterine life. It serves as a guide to the need for resuscitation, but, unless the score fails to improve with resuscitation, it has very little predictive value for later disability. A low Apgar score is not synonymous with birth asphyxia. It could, for example, be a reflection of a pre-existing fetal problem or of sedation caused by the maternal drug administration.
Preventing hypothermia
Newborn babies can lose heat faster than they can generate it (Box 50.1). Hypothermia is dangerous and must be prevented. The delivery room must be warm and draughts kept to a minimum. The baby should be immediately dried and wrapped in dry towels or blankets, with a hat put on to prevent heat loss from the head. If resuscitation is required, it should be performed under a radiant heater. Pre-term babies are routinely delivered into polythene bags to minimize evaporative losses and improve temperature control.
Examination
Providing all appears well, all that is needed in the labour ward is a brief examination for any obvious external abnormalities. A full routine examination should be deferred until later.
Weighing and measuring
Weight, length, and head circumference measurements provide an assessment of how well the baby has grown in utero and are a baseline against which to judge subsequent growth. Table 50.1 gives some normative term data and such data are also available for neonates born at earlier gestations.
Table 50.1
Some dimensions of an average male* infant at 40 weeks
| Weight | 3500 g |
| Length | 50 cm |
| Head circumference | 35 cm |
| Brain weight | 400 g (12% of body weight) |
| Blood volume | 280 mL (80 mL/kg) |
* Females are about 10% smaller.
The umbilical cord
The cord should be checked to see whether it contains the usual two arteries and one vein. A single artery has a 20% association with congenital abnormalities, mainly of the genitourinary system. A plastic cord clamp should be fixed so as to leave about 2 cm of cord proximally. Subsequent care of the cord involves ensuring it is kept clean and dry. If the baby is likely to need intensive care, the cord should be left longer as it provides an accessible route for arterial and central venous cannulation.
Preventing haemorrhagic disease of the newborn
Vitamin K does not cross the placenta well and newborn babies have low serum concentrations and poor stores. They do not have gut bacteria to synthesize it for them, and human milk is a relatively poor source of the vitamin. Lack of vitamin K leads to shortage of clotting factors II, VII, IX and X, and about 1 in 1000 breast-fed babies will experience serious bleeding, a condition known as haemorrhagic disease of the newborn. The classical form occurs between days 1–7, although an early form occurs in infants born to mothers taking anticonvulsants and a late (and sometimes more serious form) may also occur, even up to 12 weeks after delivery. Bottle-fed babies are at less risk because formulae are supplemented with vitamins.
Almost complete protection is provided by the administration of vitamin K 1 mg i.m. at the time of birth, and possibly less-complete protection is provided by giving vitamin K 2 mg orally twice in the first week (with a further oral dose at 1 month). Some epidemiological studies have found an association between i.m. vitamin K (as opposed to oral vitamin K) and childhood leukaemias, resulting in a swing away from treatment. Many large subsequent studies have failed to prove the connection.
Perinatal asphyxia
Evolution has equipped the fetus with a remarkable ability to tolerate asphyxia without adverse consequences, to the extent that sometimes 10 or 15 min of absolute anoxia can be compatible with normal survival. In practice, absolute anoxia only occurs with rare events such as massive placental abruption or cord prolapse. Asphyxia may lead to cerebral palsy, essentially a motor disorder affecting posture and movement which is variably accompanied by mental impairment, epilepsy or sensory defects. Despite popular belief, it is likely that less than 10% of cerebral palsy is caused primarily by perinatal asphyxia.
Neonatologists are wary of making a diagnosis of perinatal asphyxia, unless there is a good antenatal history (e.g. abruption) together with neonatal ‘depression’ (e.g. poor Apgar scores) and evidence of subsequent multi-organ failure. Such multi-organ failure may present with seizures, cerebral oedema, oliguria, haematuria, coagulopathy, jaundice or occasionally pulmonary haemorrhage. The question of predicting the likelihood of neurological injury following a specific birth and the question of whether a subsequent developmental abnormality was caused by a specific intrapartum insult is seldom straightforward.
Current evidence suggests that therapeutic induced hypothermia (‘cooling’) to a rectal temperature of 33–34°C for 72 h improves both survival and neurological outcome at 18 months of age in infants with moderate or severe perinatal asphyxial encephalopathy. Therapeutic hypothermia is considered in infants of > 36 weeks completed gestation, admitted to a neonatal unit with one or more of the following:
![]() Apgar ≤ 5 at 10 min of age
Apgar ≤ 5 at 10 min of age
![]() continued need for resuscitation, including endotracheal or mask ventilation, at 10 min after birth
continued need for resuscitation, including endotracheal or mask ventilation, at 10 min after birth
![]() acidosis within 60 min of birth (defined as any occurrence of umbilical cord, arterial or capillary pH < 7.00)
acidosis within 60 min of birth (defined as any occurrence of umbilical cord, arterial or capillary pH < 7.00)
![]() base deficit ≥ 16 mmol/L in umbilical cord or any blood sample (arterial, venous or capillary) within 60 min of birth.
base deficit ≥ 16 mmol/L in umbilical cord or any blood sample (arterial, venous or capillary) within 60 min of birth.
Infants who fulfil one or more of the above criteria then require close observation for signs of seizures or moderate to severe encephalopathy evidenced by an:
![]() altered state of consciousness (reduced or absent response to stimulation) and
altered state of consciousness (reduced or absent response to stimulation) and
![]() abnormal tone (focal or general hypotonia, or flaccid) and
abnormal tone (focal or general hypotonia, or flaccid) and
![]() abnormal primitive reflexes (weak or absent suck or Moro response).
abnormal primitive reflexes (weak or absent suck or Moro response).
Infants who meet both criteria should be considered for cooling. This should be instituted as soon as possible after resuscitation, as evidence suggests that it is unlikely to be beneficial if commenced more than 6–8 h after birth. Techniques include selective head cooling and whole body cooling, and treatment requires specialist cooling equipment. Passive cooling should be considered when indicated in a baby outwith a specialist centre, where transfer is not possible or may be delayed. Most infants require intubation and mechanical ventilation, particularly in the initial stages of treatment and continuous rectal temperature monitoring is essential.
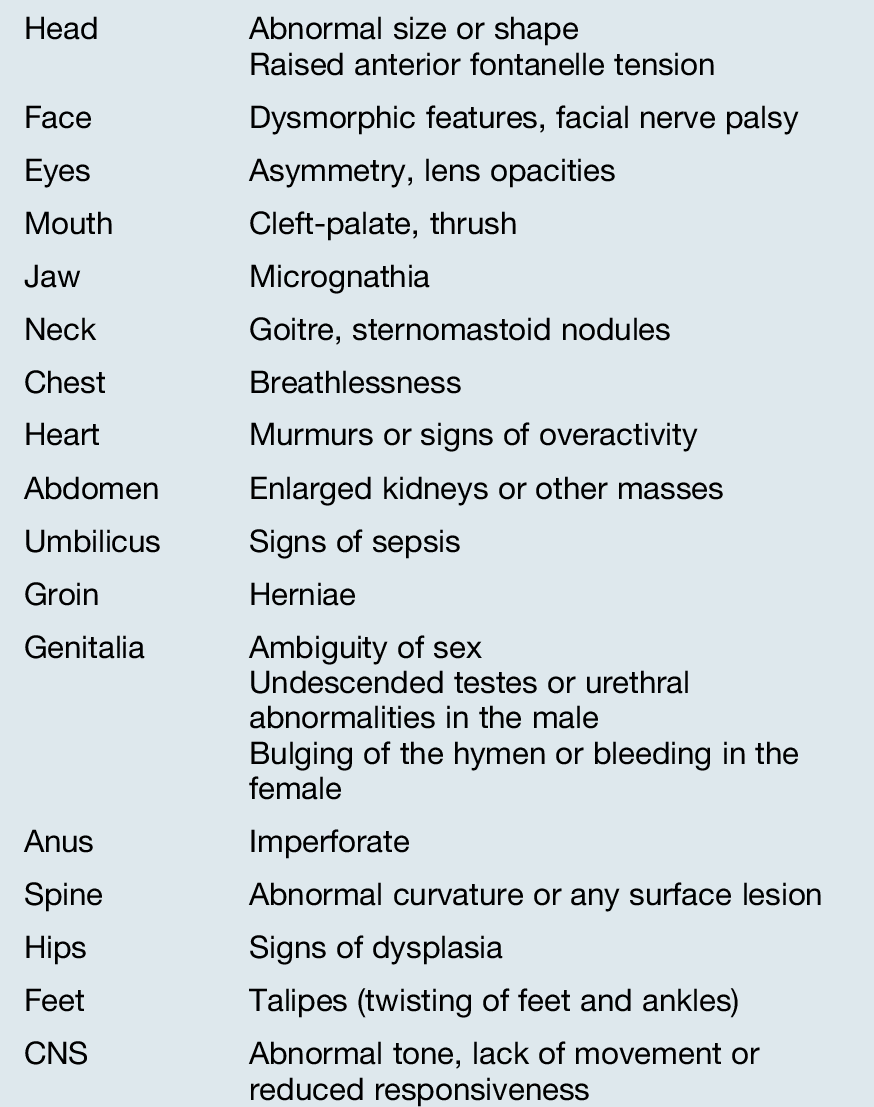
Neonatal examination
Sometime during the first day or two of life, all newborn babies should be carefully and systematically examined, for the reasons outlined in Box 50.2. The technique for this examination must be learned, as must the range of normal findings. It is probably better to follow an anatomical progression from head to toe (Table 50.2), rather than to adopt a system-orientated approach.
Developmental dysplasia of the hip
Developmental dysplasia of the hip (previously referred to as ‘congenital dislocation of the hip’) has an overall incidence of approximately 1%, but is commoner in breech presentation, oligohydramnios, first-born females, large babies and those with a family history. Early neonatal diagnosis carries an excellent prognosis, as most respond to several months in a versatile harness (the Pavlik harness – pronounced ‘Pau-lick’). Those in whom the diagnosis is delayed rarely attain normal hip development. Clinical screening with Ortolani’s test (see History box) may miss a significant proportion of cases. Ultrasound is likely to detect a greater proportion and, although commonly used only in higher-risk neonates, it may become part of the routine screening process.
Biochemical screening
As well as screening by physical examination, babies in the UK are screened biochemically for a number of different disorders by performing a heel-prick blood sample on about the 7th day of life. Disorders tested for include phenylketonuria, congenital hypothyroidism and cystic fibrosis, with medium-chain acyl-coenzyme A dehydrogenase (MCAD) deficiency and sickle cell disease, also included in some regions.
Physical birth injury
Serious physical injury to the baby during birth is rare in Western practice. Injuries are most likely to occur when there is absolute or relative disproportion between the size of the baby and the maternal pelvis, or following malpresentation or instrumental delivery. Pre-term babies are more easily damaged than those at term.
Nerve palsies
These are due either to overstretching of the nerve or to direct external pressure on the nerve. In more than 85% of instances, the nerve fibres remain intact and full recovery occurs. Nerve disruption may result in permanent disability.
Brachial plexus
Erb palsy is caused by injury to roots C5 and C6 and produces a limp arm, held alongside the body with the forearm pronated – ‘waiter’s tip’ posture. Klumpke palsy is rarer, involves C8 and T1, and mainly affects the wrist extensors and the small hand muscles. Injury to the phrenic nerve is rare. It is associated with brachial plexus injury and can cause marked respiratory difficulty (see Fig. 46.7).
Facial nerve
This is a lower motor neuron lesion due to compression of the facial nerve by maternal pelvic bones or forceps. Minor, transient cases (most notable when an infant is crying) are quite common, but permanent weakness is seen in only about 5% of instances.
Skeletal injury
Although the skull often undergoes marked distortion during delivery, fractures are very uncommon and usually cause little trouble. Fractures of the clavicle are not infrequently seen even after normal delivery and usually heal very well, although sometimes with massive callus formation. Fractures of other bones are rare and suggest significant trauma at delivery.
Soft tissue injury
This is rarely of any serious consequence but may be distressing for parents as well as for whoever conducted the birth.
Caput succedaneum
Essentially oedema of the ‘presenting’ scalp, this disappears rapidly after birth and requires no treatment.
Chignon
This is the name given to the swelling produced by a ventouse vacuum extractor. There are usually no complications, but infection and necrosis of the skin can occur.
Cephalhaematoma
Bleeding between a skull bone and its overlying periosteum occurs in about 1% of babies. The lesion is confined to the margins of the bone by attachment of the periosteum, which prevents the amount of blood loss from becoming significant (Fig. 50.3). It is almost always parietal, but can occasionally be occipital. Palpation around the edge of the lesion often gives the impression of an associated depressed fracture, but this is an illusion. In 5% of cases, there is an inconsequential linear fracture of the underlying bone. Spontaneous regression occurs and no treatment is required.
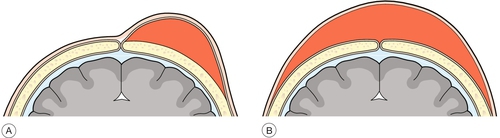
Fig. 50.3Comparison of cephalhaematoma and subaponeurotic haemorrhage.
(A) The space under a cephalhaematoma is relatively small and major blood loss is unlikely. (B) There is a much larger potential space under the aponeurosis, and there may be serious blood loss.
Subaponeurotic haemorrhage
This is much rarer than cephalhaematoma, but may lead to serious blood loss and can be fatal. There is bleeding into the potentially very large space between the skull and the overlying occipitofrontalis aponeurosis (Fig. 50.3).
Sternomastoid tumour
This is a fibrous lump in the sternomastoid muscle, probably secondary to compression of the muscle leading to ischaemia. It settles spontaneously but can cause torticollis.
Congenital abnormalities
Approximately 2% of newborn babies have a serious abnormality detectable at, or soon after, birth. Some of the more serious abnormalities may have been identified antenatally following appropriate screening, particularly neural tube defects, renal agenesis, diaphragmatic hernias and some cardiac problems. In addition to these major abnormalities, 2–3% more babies may have some minor abnormality. Congenital abnormalities are discussed in more detail in Chapter 33.
Feeding
At term, human milk has considerable advantages over a cow’s milk-based formula (see Box 50.3). In addition, breastfeeding is psychologically advantageous to both mother and baby, and also confers physiological and disease-prevention benefits on the mother. Mothers should be encouraged to put the baby to the breast soon after birth, and thereafter the baby should be fed on demand. In many high-income countries, the prevalence of breastfeeding remains low and marketing from artificial-feed companies is intense.
Correct reconstitution of powdered milk formulae is essential for safe artificial feeding, as babies do not tolerate excessive osmolar loads (see Table 50.3). Whichever way the baby is fed, a close watch must be kept on the adequacy of weight gain. Between 170 g and 200 g per week is appropriate for a term neonate during the first few weeks of life.
Table 50.3
Recommended feed volumes for term newborn infants
| Day 1 | 60 mL/kg |
| Day 2 | 75 mL/kg |
| Day 3 | 90 mL/kg |
| Day 4 | 120 mL/kg |
| Day 5 | 150 mL/kg |
Special formulae are available for pre-term babies, and have higher levels of protein, sodium, calcium and phosphate. Pre-term babies should gain weight at about 12 g/kg per day. ‘Special’ milks, such as those based on soya, should only be used when there are clear medical indications.
Signs of illness
Newborn babies have a very limited number of ways to show that they are ill (Box 50.4). These signs may be subtle and most often, are first noticed by the mother or the nursing staff. The signs may occasionally be nonspecific, so that a baby with an infection may initially be clinically indistinguishable from one with a metabolic disorder or even cardiac disease. This, coupled with the speed with which newborn babies deteriorate during serious illness, means that a very high index of suspicion and a low threshold for investigation are appropriate.
When a baby shows some of the features listed in Box 50.4, infection is by far the likeliest cause and the following approach should be pursued:
![]() Take a history, considering particularly:
Take a history, considering particularly:
![]() maternal health during pregnancy
maternal health during pregnancy
![]() risk factors for infection, such as prolonged rupture of the membranes, maternal illness or pyrexia during labour, maternal group B Streptococcus or nursery contact with sick babies
risk factors for infection, such as prolonged rupture of the membranes, maternal illness or pyrexia during labour, maternal group B Streptococcus or nursery contact with sick babies
![]() family history of neonatal illness or neonatal death.
family history of neonatal illness or neonatal death.
![]() Examine the baby. As well as assessing the severity of illness, the examination should seek signs of superficial infection, which might have led to septicaemia, and signs of organ dysfunction.
Examine the baby. As well as assessing the severity of illness, the examination should seek signs of superficial infection, which might have led to septicaemia, and signs of organ dysfunction.
![]() Investigate as follows:
Investigate as follows:
![]() blood culture
blood culture
![]() full blood count and film
full blood count and film
![]() blood glucose
blood glucose
![]() arterial blood gas, if the baby is breathless or seriously ill
arterial blood gas, if the baby is breathless or seriously ill
![]() C-reactive protein
C-reactive protein
![]() urine culture
urine culture
![]() swabs, from any inflamed lesions
swabs, from any inflamed lesions
![]() chest X-ray
chest X-ray
![]() stool culture, if stools abnormal
stool culture, if stools abnormal
![]() lumbar puncture, if sepsis is suspected and the source is unclear.
lumbar puncture, if sepsis is suspected and the source is unclear.
![]() Treat. If infection seems a possibility, broad-spectrum antibiotic therapy should be started, for example a combination of benzylpenicillin or ampicillin and gentamicin or a third-generation cephalosporin. The results of investigations will allow the rationalization of treatment.
Treat. If infection seems a possibility, broad-spectrum antibiotic therapy should be started, for example a combination of benzylpenicillin or ampicillin and gentamicin or a third-generation cephalosporin. The results of investigations will allow the rationalization of treatment.
Jaundice
Clinically apparent jaundice (serum bilirubin greater than about 75 mmol/L) affects more than half of all newborns during the first week of life.
Physiological jaundice
Almost all jaundiced babies will have a harmless physiological jaundice which is part of the normal transition from fetal to postnatal life. The fetal liver does not handle unconjugated bilirubin but rather leaves it to cross the placenta to be conjugated and excreted by the mother. Following birth, the neonatal liver must handle all of the unconjugated bilirubin produced but cannot do so immediately. During the first few days of life, liver function improves rapidly, but, while this is happening, the serum unconjugated bilirubin invariably rises.
Unconjugated bilirubin is lipid soluble and can therefore cross the blood–brain barrier and is toxic to the central nervous system, especially the basal ganglia and the auditory pathways. Bilirubin encephalopathy, or kernicterus, may lead to an athetoid cerebral palsy, deafness, and may even be lethal. The unconjugated serum bilirubin concentration probably needs to exceed 500 mmol/L in order to injure the brain of a healthy term infant and this never occurs with physiological jaundice.
Pathological jaundice
The main problem with physiological jaundice is that it makes it difficult to spot the very few infants with pathological jaundice due to the causes in Box 50.5. Some of these conditions are important in their own right, while others pose a risk of kernicterus. Jaundice which fulfils any of the criteria listed in Box 50.6 should be regarded as potentially pathological.
Most of the pathological causes of jaundice are easy to understand and it is relatively easy to reach a diagnosis if a systematic approach is adopted. Box 50.7 lists the main tests to be performed.
Breast milk jaundice
Breast milk jaundice is still not completely understood but it is thought that compounds in the milk of some women interfere with conjugation of bilirubin in the baby’s liver. It is a harmless condition but problematic because there is no specific test for it. It presents as persistent jaundice which is mainly unconjugated in nature. Other more serious causes of persistent jaundice, such as hypothyroidism or hepatitis, must be excluded before the diagnosis of breast milk jaundice can be safely accepted.
Obstructive jaundice
The diagnosis must be considered in any baby who is still jaundiced at 2 weeks of age and is an important diagnosis to make. The history of pale stools and dark urine should be sought and the urine tested for bilirubin. If obstructive jaundice is suspected, the biliary tree should be investigated using ultrasound, radioisotope scans and possibly liver biopsy. Most cases of biliary atresia can be treated, at least partially, by surgical anastomosis of the liver to the small bowel known as a Kasai portoenterostomy. Success of this procedure decreases markedly after 8 weeks and therefore, prompt diagnosis following a high index of suspicion is essential. Long term, liver transplantation will be required by many survivors of neonatal surgery.
Jaundice due to haemolysis
Some of the pathological causes of neonatal jaundice can raise the serum concentration of unconjugated bilirubin to levels at which encephalopathy might occur. This is most likely with rhesus disease but occasionally happens with ABO incompatibility or other haemolytic disorders. The use of anti-D immunoglobulin to treat rhesus-negative women after childbirth or obstetric procedures has made rhesus disease quite rare. ABO incompatibility usually exists when a group O mother has a group B or A baby (see Chapter 39).
Treatment of pathological jaundice
Above an age-specific bilirubin threshold, phototherapy is indicated. This involves the use of high-intensity light in the 450 nm wavelength to convert stable lipid-soluble unconjugated bilirubin into unstable water-soluble isomers which can be excreted in the bile without the need for conjugation. It takes about 12–24 h to have an effect on the rate of rise of the bilirubin. If the bilirubin rises above a further threshold despite phototherapy, an exchange transfusion is required.
Low birth weight infants
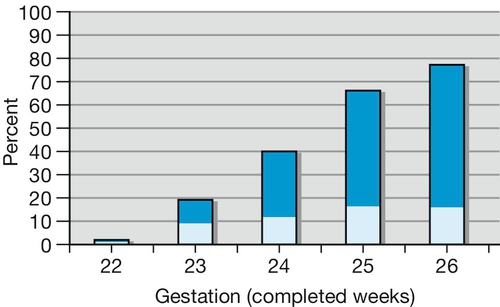
Although low birth weight (LBW) babies account for only 10% of all births in the UK, they account for around 70% of the perinatal mortality. Approximately two-thirds of LBW babies are pre-term (Fig. 50.4) and the rest are term but small-for-gestational age (SGA).
Prematurity-related problems
Survival increases with increasing gestation (Fig. 50.5). Disability is strongly associated with increasing prematurity, and includes cerebral palsy, short stature, respiratory difficulties, visual impairment and poor school performance. It is now well established that corticosteroids given to mothers who subsequently deliver pre-term are effective in reducing the incidence of respiratory distress syndrome by around 50%, as well as the risk of periventricular haemorrhage. Whether or not to start resuscitation with an extremely premature infant (< 24 weeks) can sometimes be a difficult question and, ideally, discussions with the prospective parents should have taken place beforehand in order to gauge their wishes. The problems of prematurity are outlined in Table 50.4.
Table 50.4
The problems of prematurity
| Skin | Extremely pre-term infants have a very high surface area to mass ratio and thin skin, and are extremely liable to hypothermia. This means that it is vitally important to deliver in a warm room with heated towels for drying and some method to keep the baby warm during resuscitation, e.g. an overhead heater. Survival is directly related to the temperature of the infant on admission to the neonatal intensive care unit |
| Lung | At 23–24 weeks, the respiratory epithelial cells start to differentiate into type I (gas exchange) and type II (surfactant production) pneumocytes. Surfactant levels at this gestation are therefore very low but can be increased by antenatal glucocorticoids (see RDS, p. 403). Respiratory support is often by mechanical ventilation, either ‘conventional’ or with ‘high-frequency oscillation’, and exogenous prophylactic surfactant administration. A large proportion of extremely pre-term infants develop chronic lung disease of prematurity (bronchopulmonary dysplasia), with continuing requirements for respiratory support |
| Central nervous system | The subependymal germinal matrix lies close to the ventricular space and contains the developing brain cells of the premature infant. Bleeding from this very vascular area may occur with pre-term birth, giving rise to periventricular haemorrhage. A major intraventricular haemorrhage may lead to hydrocephalus and cortical damage. The extremely pre-term infant is also prone to ischaemic brain injury from low arterial oxygen tension, hypotension, or reduced cerebral blood flow. Subsequent periventricular cysts (periventricular leucomalacia) may form and, if this happens, long-term neurological sequelae are likely. The location of brain injury in the white matter adjacent to the lateral ventricles means that the subsequent disability is mainly motor and often affects the lower limbs. This presents as a spastic diplegia with relative sparing of the intellect and affects about 10% of babies with birth weights below 1500 g |
| GI system | Structurally, the bowel is well developed by the end of the second trimester but there is functional immaturity. Motility and food absorption are both reduced and early enteral feeding may not be tolerated. Parenteral nutrition may be needed during the early days and weeks, but this may lead to numerous problems, both from the need to maintain adequate venous access and the tolerability of the amino acid and lipid solutions. Necrotizing enterocolitis (NEC) is not uncommon in premature infants, and is characterized by ischaemic bowel necrosis. Although the aetiology is unclear, it typically presents after the introduction of enteral feeds and is postulated to be an abnormal reaction to bowel colonization |
| Liver | There may be jaundice, poor clotting, poor glucose control and a limited ability to excrete waste products |
| Blood | There is reduced immunoglobulin and white cell function, so the risk of sepsis is increased. Furthermore, frequent use of multiple, broad-spectrum antibiotics renders the tiny baby more prone to infection with sub-pathogenic bacteria such as Staphylococcus epidermidis, and fungi, especially Candida albicans |
| Eye | Early vasoconstriction damage to the retina occurs as a result of high oxygen pressure and other factors. The incidence of this is reduced by using ventilation at lower PO2 levels. Secondary proliferation of weaker, potentially haemorrhagic, vessels occurs, a condition referred to as retinopathy of prematurity. Regular ophthalmological review is vital as early laser or cryotherapy treatment of these new vessels can preserve vision |
Problems with being small-for-gestational-age
By definition, 10% of babies are small-for-dates, the majority for no pathological reason. Around one-third, however, have fetal growth restriction and is defined as ‘a baby which has failed to reach its genetic growth potential’, and are more at risk of peripartum hypoxia and neonatal hypoglycaemia. The implications of fetal growth restriction are discussed further in Chapter 35.
Infection
Although the fetus is generally isolated from the external bacteriological environment, some pathogens are occasionally able to cross the placenta and infect the baby. This may sometimes lead to permanent damage, and the details of some of these conditions are discussed on page 273.
Newborn babies are immunocompromised relative to older children for the reasons shown in Box 50.8 and are therefore at increased risk of infection. Neonatal infections may be with organisms from the birth canal, such as group B β-haemolytic streptococci, or from the neonatal environment, for example Escherichia coli, Proteus species, Staphylococcus aureus and S. epidermidis. The risks are of pneumonia, meningitis, pyelonephritis and osteomyelitis, and a low index of suspicion is important for these conditions.
Some common minor infections are considered below.
Conjunctivitis
‘Sticky eyes’ are common and most cases respond rapidly to topical antibacterial treatment. Infection with gonorrhoea and chlamydia, however, may be more serious.
![]() Gonococcal ophthalmia usually presents as a fulminant, unilateral or bilateral, purulent infection during the first few days of life. The maternal history may give a clue. Prompt diagnosis and treatment with systemic and local penicillin is needed to prevent corneal damage and permanent visual impairment
Gonococcal ophthalmia usually presents as a fulminant, unilateral or bilateral, purulent infection during the first few days of life. The maternal history may give a clue. Prompt diagnosis and treatment with systemic and local penicillin is needed to prevent corneal damage and permanent visual impairment
![]() Chlamydial eye infections usually present as sticky eyes which do not settle with conventional antibacterial agents. The diagnosis is best made from corneal brushings but can be made from an ordinary eye swab if the laboratory is asked to look specifically for the organism. Treatment is with tetracycline eye drops and systemic erythromycin to clear the organisms from the upper respiratory tract, from where they may go on to cause pneumonia. Systemic tetracycline is never given to babies or young children because it stains dental enamel and interferes with its development.
Chlamydial eye infections usually present as sticky eyes which do not settle with conventional antibacterial agents. The diagnosis is best made from corneal brushings but can be made from an ordinary eye swab if the laboratory is asked to look specifically for the organism. Treatment is with tetracycline eye drops and systemic erythromycin to clear the organisms from the upper respiratory tract, from where they may go on to cause pneumonia. Systemic tetracycline is never given to babies or young children because it stains dental enamel and interferes with its development.
Candida
‘Thrush’ infections are common either in the mouth or in the nappy area and are caused by a yeast, Candida albicans. In the mouth, the appearance is of adherent white patches of exudate. In the nappy area, inflammation may be confused with other causes of nappy rash, although satellite lesions around the main area of erythema are suggestive of candida. Treatment is with topical nystatin or one of the more modern antifungal agents, such as miconazole.
Skin sepsis
Skin sepsis is relatively common and is usually due to staphylococci, although streptococci and other organisms may be involved. Paronychia, pustules and periumbilical infection are the most likely manifestations. Blistering and desquamation are seen with some strains of staphylococci. All suspected staphylococcal or streptococcal infections should be taken very seriously and a low threshold for systemic treatment is appropriate.
Urinary tract infection
Urinary tract infection in babies is more common in boys than in girls and is usually caused by E. coli and other Gram-negative organisms. Screening can be performed using bag specimens but diagnosis is best confirmed by suprapubic aspiration. Because of the association with congenital abnormalities of the urinary tract, an ultrasound scan or other imaging techniques should be considered.
Meningitis
Neonatal meningitis is most commonly caused by group B β-haemolytic streptococci or E. coli and has a high morbidity and mortality. A very low threshold for investigation and treatment is appropriate.