Myasthenia gravis and lambert-eaton myasthenic syndrome
Myasthenia gravis
The incidence of myasthenia gravis (MG), an autoimmune disease of the neuromuscular junction, is 1:20,000 in the adult population and higher in patients with other autoimmune diseases, such as thyroiditis and rheumatoid arthritis. Characterized by weakness of voluntary skeletal muscle, MG can be classified by age, etiology (Table 172-1), or the presence or absence of bulbar signs and symptoms because the muscles innervated by the cranial nerves are most frequently involved (Table 172-2).
Table 172-1
Subgroups or Types of Myasthenia Gravis
| Type | Description |
| Nonimmune | |
| Congenital myasthenic syndrome | Defects in proteins at the neuromuscular junction |
| Immune | |
| Neonatal myasthenia gravis | Transplacental passage of AChR antibodies |
| Juvenile myasthenia gravis | Onset before 18 years of age |
| Early-onset myasthenia gravis | Onset at 18 to 50 years of age |
| Late-onset myasthenia gravis | Onset after 50 years of age |
| Seronegative myasthenia gravis | No detectable AChR antibodies |

Table 172-2
Signs and Symptoms Associated with the Classes of Myasthenia Gravis
| Class | Signs and Symptoms |
| I | Any ocular muscle weakness |
| May have weakness of eye closure All other muscle strength is normal |
|
| II | Mild weakness affecting other than ocular muscles May also have ocular muscle weakness of any severity |
| III | Moderate weakness affecting other than ocular muscles May also have ocular muscle weakness of any severity |
| IV | Severe weakness affecting other than ocular muscles May also have ocular muscle weakness of any severity |
| V | Defined by requirement for intubation, with or without mechanical ventilation, except when used during routine postoperative management |
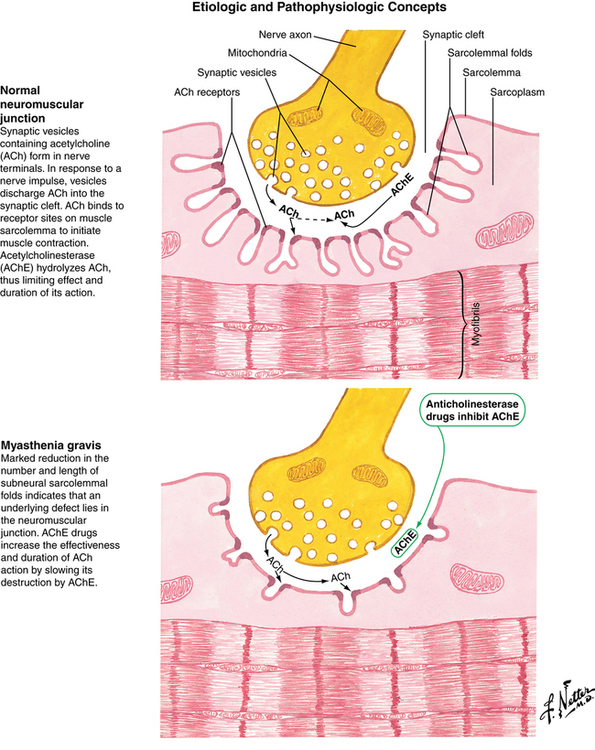
Pathophysiology
Circulating antibodies to acetylcholine (ACh) receptors (AChRs), which are found in 70% to 90% of patients with MG, are thought to reduce the number of functional AChRs via three different mechanisms: competitive blockade of AChRs; complement-mediated lysis of the receptor and muscle end plate, resulting in blocked access to the receptor; and increased destruction and decreased production of AChRs. The net effect of these mechanisms is a motor end plate with decreased surface area and decreased functional AChRs (Figure 172-1).
Lambert-eaton myasthenic syndrome
Lambert-Eaton myasthenic syndrome (LEMS), often confused with MG, is a rare disorder of neuromuscular transmission most often associated with carcinoma of the lung, especially oat cell carcinoma of the bronchus. Antibody-mediated destruction of presynaptic voltage-gated calcium channels leads to deficient release of ACh at the neuromuscular junction, causing muscle weakness. The skeletal muscle weakness associated with LEMS is not reliably reversed with anticholinesterase drugs or corticosteroids. Furthermore, exercise improves, rather than reduces, muscle strength in this condition. Patients with LEMS are very sensitive to the effects of both depolarizing and nondepolarizing NMBAs. The potential for LEMS should be considered in patients with known or probable carcinoma, especially of the lung (Table 172-3).
Table 172-3
Comparison of Lambert-Eaton Myasthenic Syndrome and Myasthenia Gravis
| Characteristic | LEMS | Myasthenia Gravis |
| Manifestations | ||
| Areas of weakness | Proximal limbs (legs more than arms) | Extraocular, bulbar, and facial muscles |
| Response to exercise | Improves strength | Fatigue |
| Muscle pain | Common | Uncommon |
| Reflexes | Absent or decreased | Normal |
| Sex | Male > female | Female > male |
| Coexisting pathology | Small cell carcinoma of the lung | Thymoma |
| Response to drugs | ||
| Succinylcholine | Sensitive | Resistant |
| Nondepolarizing NMBAs | Sensitive | Sensitive |
| Anticholinesterase drugs | Poor | Good |
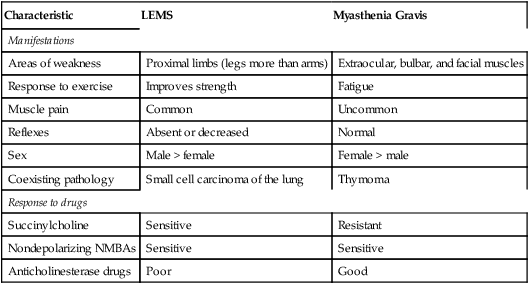
LEMS, Lambert-Eaton Myasthenic syndrome; NMBAs, neuromuscular blocking agents.