Chapter 20. Musculoskeletal System
Rationale
Movement is so much a part of a child’s activities that it is important to screen for disorders that can affect a child’s socialization, exercise patterns, participation in sports, and ability to engage in self-care. Early diagnosis and intervention in disorders such as developmental dysplasia of the hip can possibly prevent more exhaustive treatment as the child grows.
Anatomy and Physiology
The musculoskeletal system provides support for the body and enables movement. The musculoskeletal system is composed of bones, muscles, tendons, ligaments, cartilage, and joints.
The skeleton arises from mesoderm. At birth the epiphyses of most bones are made of hyaline cartilage. Shortly after birth, secondary ossification centers appear in the epiphyses. The epiphyses ossify, except for the epiphyseal plate, which separates the epiphyses and the diaphyses. The epiphyseal plate is replaced by bone until only the epiphyseal line remains. When the epiphyses are completely ossified, no further bone lengthening occurs.
Muscle fibers are developed by the fourth or fifth month of gestation. The number of muscle fibers remains constant throughout life. Muscle growth is accomplished by increase in the size of the fibers. Muscle mass decreases from one fourth of total body weight at birth to one sixth of total body weight at adolescence. Transient increases in nonlean mass (subcutaneous fat) occur just before the growth spurt, especially in boys, accompanied by decreases 1 to 2 years later. Lean body mass increases, chiefly muscle, occur after the growth spurt, with the increase greater in males than in females.
Preparation
Inquire whether the infant sustained trauma or injury at birth. Inquire whether there is a family history of bone or joint disorders and whether the child has experienced delays in gross or fine motor development, trauma, joint stiffness and swelling, fever, or pain. If the child has or has had pain, it is important to determine the location, type, intensity, and time of occurrence of the pain. Sharp pain that lessens during rest can indicate injury. Constant dull pain that awakens the child might indicate tumor or infection. Inquire about participation in sports activities (type of sport, level of training involved, amount of contact, previous injuries) and diet. Minimal clothing assists with assessment of the spine.
Assessment of Musculoskeletal System
| Assessment | Findings | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| If the child is able to walk, observe the gait. Note the presence of casts and braces. |
Infants and toddlers tend to walk bowlegged. A wide-based gait is normal in the infant and toddler.
Clinical Alert
Limping can indicate developmental dysplasia of one hip (especially in toddlers). If both hips are involved, the child has a waddling gait. (Table 20-1 lists further indications of developmental dysplasia of the hip.)
Limping also indicates scoliosis, Legg-Calvé-Perthes disease, infection of the joints of the lower extremities, a slipped capital femoral epiphysis, or stress fractures of the metatarsals.
Weight bearing on the toes (pes equines) and short heel cords indicate muscular disease or cerebral palsy.
|
| Assessment | Findings | ||
|---|---|---|---|
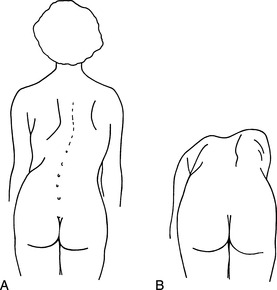
| Observe the curve of the infant’s or child’s spine and note the symmetry of the hips and shoulders while the child is standing erect. Test for scoliosis by having the child bend forward at the waist and observing the child from side; note asymmetry or prominence of rib cage. |
The spine is normally rounded in the infant younger than 3 months. A lumbar curve forms at 12 to 18 months.
Lumbar lordosis is normal in young children.
Clinical Alert
Rigidity of the spine while sitting up can indicate infection of the central nervous system or tension.
Kyphosis (hunchback) can indicate wedge-shaped or collapsed vertebrae secondary to myelomeningocele, spinal tumors, Scheuermann’s disease, tuberculosis of the spine, or sickle cell anemia. Kyphosis can also indicate habitual slouching.
The persistence of lateral curvature of the spine indicates scoliosis. If the child can voluntarily correct the curve or if it disappears when the child is recumbent, the curve might be functional. A persistent curve, accompanied by unequal height of the shoulders and iliac crests when the child is standing erect and asymmetric elevation of the scapula when the child is leaning forward (Figure 20-1), indicates structural scoliosis.
|
||
| Observe the lumbosacral area for abnormalities of the overlying skin (pigmented skin, hairy patches, or dimpling). | Pigmented skin, hairy patches, or dimpling in the lumbosacral area can indicate spina bifida occulta. |
| Assessment | Findings | ||
|---|---|---|---|
| Note the mobility of the spine, especially the cervical spine. |
No resistance or pain should be felt when the child bends or when the neck is flexed or moved from side to side.
Clinical Alert
Pain, crying, or resistance when the neck is flexed indicates meningeal irritation and is known as Brudzinski’s sign. Lateral inclination of the head can indicate congenital torticollis.
Limitations in movement of the cervical spine can indicate cervical fusion, which is found in some children with fetal alcohol syndrome.
Limitations in shoulder movement and pain across the upper back can be related to packing heavy book bags.
|
||
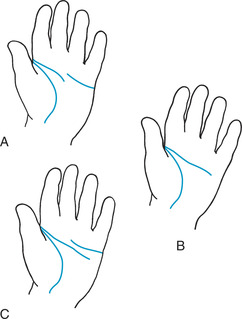
| Inspect and palpate the upper extremities. Note the size, color, temperature, range of motion, and mobility of the joints and abnormalities in the upper extremities. Inspect the palmar creases (Figure 20-2). |
Clinical Alert
Short, broad extremities, hyperextensible joints, and simian creases can indicate the presence of Down syndrome.
The Sydney line is found in children with rubella syndrome.
Abnormal palmar creases can indicate fetal alcohol syndrome.
Abnormally long and tapering fingers, tall and thin build, and hypermobility of joints can indicate Marfan syndrome.
Short, bowed, and fragile bones and hyperextensible joints are found with osteogenesis imperfecta.
Polydactyly (external digits) and syndactyly (webbing) are abnormal findings and may or may not indicate more serious underlying conditions.
Warmth and tenderness of the joints can indicate rheumatoid arthritis. Tenderness also indicates Lyme disease or Henoch-Schönlein purpura (HSP).
Widening of the wrist joints can indicate rickets.
Limitation of elbow extension and pain can indicate subluxation of the head of the radius.
Limitation of movement in elbows, knees, and ankles, as well as complaints of tingling or aching, warmth, redness, and swelling can indicate hemarthrosis, which accompanies hemophilia.
A solid palpable mass along a bone can indicate a tumor.
Pain in the elbow that is aggravated by use can indicate tennis elbow or Little League elbow.
Pain in the shoulder, loss of internal rotation, and increased external rotation can indicate Little League shoulder.
Pain in the shoulder can indicate swimmer’s shoulder.
|
| Assessment | Findings |
|---|---|
| Assess the strength of the upper extremities by asking the child to squeeze your crossed fingers. |
The strength of the upper extremities should be equal.
Clinical Alert
Unilateral weakness can indicate hemiparesis or pain.
The feet of infants and toddlers are flat, and the legs are bowed until walking has been firmly established.
|
|
Inspect and palpate the lower extremities.
Assess for abnormalities of mobility, length, shape, and pulses.
|
Clinical Alert
Fibrosis and contracture of the gluteal and quadriceps muscles occur as complications of intramuscular injections. Observe for limited knee flexion (quadriceps involvement) or hip flexion (gluteal involvement).
|
| Assessment | Findings |
|---|---|
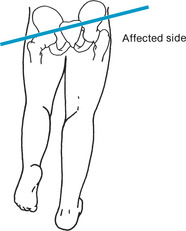
| Assess for genu varum (bowleg or lateral bowing of the tibia) or genu valgum (knock-knee) by instructing the child to stand with ankles together. |
Knock-knee is present until the child is past 7 years of age.
Clinical Alert
A space greater than 5 cm (2 in) between the knees indicates genu varum. Toddlers are generally bowlegged until leg and back muscles develop fully; unilateral bowleggedness after 2 or 3 years of age can be pathologic.
A space greater than 7.5 cm (3 in) between the malleoli in the child older than 7 years indicates genu valgum.
|
| Assess for the presence of clubfoot by lightly scratching the inner and outer soles of the feet. Observe whether the foot assumes a normal angle (i.e., right angle) to the leg when stimulated. |
Clinical Alert
Return of the foot, after stimulation, to a right angle in relation to the leg can indicate metatarsus varus in an infant with adduction and inversion of the forefoot.
Inability of the foot to right itself after stimulation can indicate talipes equinovarus (inversion of the forefoot, plantar flexion, and heel inversion) or talipes calcaneovalgus (eversion of the forefoot and dorsal flexion).
|
|
Assess the child for meningeal irritation by flexing the child’s hips and then straightening each of the knees (Kernig’s sign).
Assess for developmental dysplasia of the hip (see Table 20-1).
|
Clinical Alert
Pain and resistance to straightening of the knees indicate meningeal irritation.
|
| Assessment | Findings |
|---|---|
| Assess for strength in the lower limbs by asking the child to push against your hands with the soles of the forefeet. |
Strength should be symmetric in the lower limbs.
Clinical Alert
Unequal strength can indicate hemiparesis or pain.
Pain with plantar flexion against resistance can indicate Achilles tendonitis.
Pain in the arch or heel is related to repetitive stretching of the plantar fascia.
Pain along the anterior or medial aspect of the midshaft or distal third of the tibia is indicative of shin splints.
|
| Palpate knees for tenderness, warmth, and consistency. |
Clinical Alert
Tenderness, warmth, and boggy consistency can indicate synovitis.
Pain, diffuse swelling, and limitation of movement can indicate sprain.
Bone and joint pain, pallor, fatigue, hemorrhage, and anorexia can indicate leukemia.
|
| If large amounts of fluid are suspected in the knee, instruct the child or adolescent to lie down. Grasp the patella firmly on each side with the left thumb and index finger. With right fingers, push down on the patella. Feel for a click or fluid wave (ballottement test). |
Normal finding is absence of movement of patella.
Clinical Alert
Click or fluid wave indicates large amount of knee joint effusion.
Absence of pain and clicking are normal findings.
|
| If child or adolescent states knee “locks” or “gives way,” perform McMurray’s test. With the child supine, ask the child to flex the affected knee and hip. |
Clinical Alert
Clicking or pain can indicate a torn meniscus of the knee joint.
Overprominence of the tibial tubercle, pain, and tenderness can indicate Osgood-Schlatter disease or Sinding-Larsen syndrome (pain is slightly lower).
|
| Assessment | Findings |
|---|---|
| Place the thumb and index finger of one hand on either side of the knee; with the other hand, rotate the lower leg and foot laterally, holding the heel. Slowly extend the knee, noting pain or clicking. Rotate the lower leg and foot medially, observing for pain and clicking. |
Chronic knee pain, especially after forced extension or overuse of the leg, can indicate patellofemoral syndrome.
Knee joint laxity is the most valid indication of the severity of a sprain; athlete will complain of joint being loose or unstable.
|
Risk for infection: related to invasive procedures, trauma.
Altered tissue perfusion: related to mechanical reduction of arterial flow.
Impaired tissue integrity: related to impaired physical mobility, mechanical factors.
Impaired skin integrity: related to mechanical factors, physical immobilization.
Risk for impaired skin integrity: related to physical immobilization, mechanical factors, skeletal prominence.
Impaired role performance: related to health alterations, pain, fatigue.
Altered parenting: related to lack of knowledge about child health maintenance, physical illness.
Altered family processes: related to shift in health status of a family member, situation crisis.
Impaired physical mobility: related to musculoskeletal impairment; decreased muscle strength, control, or mass; reluctance to initiate movement; loss of integrity of bone structures; joint stiffness; pain.
Impaired walking: related to illness, use of mobility aids.
Dressing/grooming/toileting/hygiene self-care deficit: related to musculoskeletal impairment.
Altered growth and development: related to effects of physical disability.
Knowledge deficit: related to information misinterpretation, unfamiliarity with information resources.
Pain: related to injury agents.
Chronic pain: related to physical disability.