Chapter 22 Musculoskeletal Injections
Iliopsoas, Quadratus Lumborum, Piriformis, and Trigger Point Injections
 Trigger points in the quadratus lumborum and iliopsoas muscles are a common source of low back pain.
Trigger points in the quadratus lumborum and iliopsoas muscles are a common source of low back pain. Quadratus lumborum and iliopsoas muscle injections are more accurately performed under fluoroscopic guidance because of their depth and location in the back.
Quadratus lumborum and iliopsoas muscle injections are more accurately performed under fluoroscopic guidance because of their depth and location in the back. When performing these injections, the practitioner should bear in mind that the quadratus lumborum and psoas muscles form the posterior abdominal wall and that there are associated organs and vascular structures anterior to these muscles.
When performing these injections, the practitioner should bear in mind that the quadratus lumborum and psoas muscles form the posterior abdominal wall and that there are associated organs and vascular structures anterior to these muscles. Good results can be achieved with a thorough history and physical examination and careful patient selection often after other more common diagnoses are eliminated.
Good results can be achieved with a thorough history and physical examination and careful patient selection often after other more common diagnoses are eliminated. Using dual guidance with fluoroscopy and nerve stimulation allows the practitioner to safely and quickly predictably deposit medications into the belly of the piriformis muscle.
Using dual guidance with fluoroscopy and nerve stimulation allows the practitioner to safely and quickly predictably deposit medications into the belly of the piriformis muscle. Practitioners should avoid injecting with any paresthesias or with a dye study that suggests intraneural, intravascular injection or injection into another structure.
Practitioners should avoid injecting with any paresthesias or with a dye study that suggests intraneural, intravascular injection or injection into another structure. Patients with quadratus lumborum pain have more pain arising from a supine to a sitting position than going from sitting to standing.
Patients with quadratus lumborum pain have more pain arising from a supine to a sitting position than going from sitting to standing. During the injection, the practitioner should look at the direction of the fibers when injecting the contrast to determine whether the injection has been in the quadratus muscle.
During the injection, the practitioner should look at the direction of the fibers when injecting the contrast to determine whether the injection has been in the quadratus muscle. If the practitioner is unsure whether the injection is deep enough, he or she should stop and inject some contrast before advancing the needle.
If the practitioner is unsure whether the injection is deep enough, he or she should stop and inject some contrast before advancing the needle. It is very important not to advance the needle too anteriorly with this injection because intraorgan injection is possible.
It is very important not to advance the needle too anteriorly with this injection because intraorgan injection is possible.Myofascial Pain and Trigger Point Injections
Myofascial pain is a common source of discomfort in the lower back. It is a painful condition that results in localized trigger points in the affected muscle. Myofascial pain syndrome was first clearly defined by Simons et al1 in the 1980s. It is characterized by trigger points in a specific muscle that may or may not respond to snapping palpation with a local twitch response and secondary decreased range of motion caused by the pain.1 A trigger point is a localized taut band of muscle that is tender to palpation and produces pain that radiates when palpated. Tactile pressure to trigger points result in known, reproducible but nondermatomal referral patterns, also known as zones of reference.1,2 There is significant variability among practitioners in the identification of trigger points for the diagnosis of myofascial pain syndrome, although there is some evidence that the interrater reliability can be significantly improved with training.3 There is currently no gold standard test for trigger point identification, leaving a fair amount of subjectivity in the diagnosis. The twitch response is the most specific clinical test of a trigger point.1 Trigger points are either active or latent.1 Both active and latent trigger points have tender taut bands within the muscle, but latent trigger points are not associated with spontaneous pain. Latent trigger points may be the result of prior injury that then becomes painful with reinjury. Trigger points may be further subdivided into primary, secondary, and satellite trigger points.1,2 Primary trigger points become active as a result of trauma, overload or overuse injury, or after leaving a muscle in a prolonged contracted or shortened position.1 Primary trigger points are in a discrete and separate location, with adjacent secondary trigger points that are often the result of spasm. Satellite trigger points are felt in the area of the referred pain remote from the primary trigger point location. The more irritable the trigger point, the more painful and extensive the referred pain; muscle size does not affect the amount or extent of the referred pain. Producing referred pain requires less pressure applied to an active than to a latent trigger point.1 Latent trigger points, by definition, are inactivated when key trigger points are inactivated. 1,2 Although in the past their mere existence was questioned, we now know that trigger points can be documented by electromyography (EMG). Hubbard and Berkoff4 in their 1993 article were the first to report spontaneous needle EMG activity at the trigger point site now described as spontaneous electrical activity (SEA).4 Endplate noise that has been recorded from specific myofascial trigger points are thought to be attributable to excessive acetylcholine release in the neuromuscular junction.1 Sympathetic activity appears to play a role in the activity of trigger points, with increased EMG amplitude seen under conditions of psychological stress and reduced firmness after a stellate ganglion block.5,6
Myofascial pain is not the same as the pain endured by those with fibromyalgia, which is a more diffuse, centralized musculoskeletal condition with many associated symptoms (e.g., irritable bowel). Predisposing factors are anything that increases or changes the demands on the muscle. These may include repetitive use, deconditioning, poor posture, and occupational or recreational injury related to muscle imbalances.6 If treated early, the prognosis for myofascial pain is good. Treatment includes physical therapy, including stretching and strengthening or conditioning; trigger point injections; acupuncture; biofeedback; transcutaneous electrical nerve stimulation (TENS); and some medications. It is not entirely clear why trigger points are painful because there is no direct evidence of inflammation or enhanced nociceptors within the trigger point sites. However, after the pain is initiated, sensitization at the level of the dorsal horn may occur, which then progresses to the development of central sensitization and the subsequent development of chronic myofascial pain.6
Although local anesthetic is the substance most often used by pain physicians in trigger point injections, there is not much evidence for its superiority over normal saline or dry needling. It does appear that the best response to trigger point injections occurs if a local twitch response is elicited.7 Part of the problem is that placebo-controlled studies of local anesthetic injections are extremely difficult to accomplish. Many of the studies do not have consistent criteria for trigger points, and some do not distinguish between the tender points of fibromyalgia and the trigger points of myofascial pain. The relief from the local anesthetic consistently outlasts the half-life of the local anesthetic, giving some credence to central sensitization in myofascial pain syndrome. All local anesthetics are somewhat myotoxic, with bupivacaine being the most myotoxic by far, but the muscle quickly regenerates with little long-term ill effect.8 The mechanism of bupivacaine’s effect appears to be on the calcium release related to the channel-ryanodine receptor of skeletal muscle.8–10 Injected steroid can also be myotoxic and should be used in low doses. Dry needling has been used with varied success but has the disadvantage of postneedling soreness, depending on the sensitivity of the patient before and during the procedure and whether or not acupuncture needles, associated with less soreness, were used.6 Although not all acupuncture points (e.g., in the ear) are the same as trigger points, there is a striking similarity between acupuncture points and those used for dry needling and for trigger point injections.
The muscles involved in myofascial pain of the lower back can be divided into the posterior (superficial to the transverse process) and anterior (deep to the transverse process) muscles. The posterior muscles include the multifidus (located closest to the spinous process) and the adjacent erector spinae muscles. The latissimus dorsi are attached to the spine by the thoracolumbar fascia, which envelops the multifidus and erector spinae muscles posterior to the quadratus lumborum. The thoracolumbar fascia extends distally and is in contact with the contralateral gluteus maximus and is thus thought an important factor in the transfer of load from the spine to the lower extremities. The quadratus lumborum is replaced distally by the iliolumbar ligament, one of the strongest ligaments in the body and the one responsible for much of the stability of the lumbosacral segment. More anteriorly and inferiorly to the quadratus are the iliopsoas muscles. These descend into the pelvic brim and attach to the lesser trochanter of the femur.11
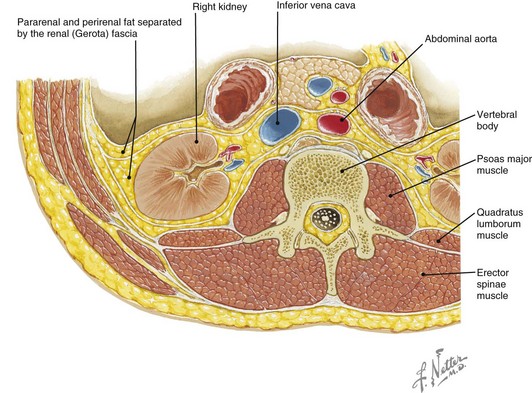
Pain involving the quadratus lumborum and iliopsoas muscles can be either primary myofascial or secondary in nature, reflecting pathology in the spine or other nearby organs. The quadratus lumborum, psoas major, and iliacus (which comes together to form the iliopsoas) muscles make up the major muscles of the posterior abdominal wall (Fig. 22-1).
Quadratus Lumborum Injections
Establishing a Diagnosis
The diagnosis of myofascial pain is a clinical one, largely dependent on the findings of the history and physical examination. The quadratus lumborum muscle allows lateral movement and extension of the mid and lower back. This muscle is a common source of myofascial pain because of its frequent use in normal daily activities such as walking and sitting; it is made worse by poor posture.2 Pain is felt in the flank, lower back, hip, and sometimes the buttocks but is mostly above the iliac crest and exacerbated by movement of the spine. It may mimic radicular or even sacroiliac joint pain because of its attachment to the iliac crest. Acute myofascial pain of the quadratus lumborum may be precipitated by sudden movements (e.g., lifting in a way that twists the lower back), and even the most mundane of movements such as coughing or deep breathing become painful. Even sleep can be problematic because patients are unable to find a comfortable position in which to sleep because of pain with any lateral movement of the spine. Patients describe pain with arising from the supine position. Because of its proximity to the abdominal organs, disease of these organs, particularly kidney disease, may present as low back pain and must be excluded. Pronounced asymmetry of the dominant quadratus lumborum in elite cricket players (fast bowlers) and resultant pars fractures involving the nondominant side have been reported in the literature in several case reports.12 Pain from the quadratus lumborum may be confused with pain that comes from injury to the iliolumbar ligament.13 The iliolumbar ligament connects the transverse process of L5 to the iliac crest. This very strong, thick ligament stabilizes the L5 body to the ilium and prevents axial rotation and translational movement on the sacrum. Pain from the quadratus lumborum may be distinguished from pain caused by iliolumbar ligament injury because of the absence of pain around the area of the flank with iliolumbar pain. The quadratus lumborum lies deep to the erector spinae muscles and the thoracolumbar fascia, so it may be difficult to distinguish these muscles from the erector spinae just on the basis of palpation.14
Physical examination involves observation and palpation for trigger points. When the patient is standing, the practitioner should look from behind for obvious signs of spasm causing a functional scoliosis or tilt and should look for elevation of the posterior superior iliac spine. The practitioner should observe for an antalgic gait and palpate for tender trigger points just below the twelfth rib and around the area of the iliac crest; this may be increased with back rotation. Part of the physical examination includes looking for a functional leg length discrepancy caused by spasm of the quadratus lumborum. The shortened leg is associated with the side of quadratus spasm and subsequent contraction resulting in upward motion of the pelvis.15 Provocative maneuvers include palpation of trigger points while twisting the back.
Anatomy
The quadratus lumborum is shaped like a quadrangle and has as its origin the aponeurosis of the iliolumbar ligament and part of the iliac crest. It is posterior to the psoas muscle and lateral to the thoracolumbar fascia. It inserts at the twelfth rib and the transverse processes of L1 to L4. It serves as an anchor between the twelfth rib and the pelvis, and the majority of the fibers attach to the twelfth rib.16 This creates a stable base for the diaphragm, allowing for its function as a basic muscle of respiration.13 The quadratus lumborum pulls down on the diaphragm and laterally flexes the lumbar spine (unilateral) and aids in back extension (bilateral). Its innervation is from the ventral rami of T12 to L4.
Phillips et al13 in their cadaver study of the anatomy of the quadratus lumborum showed that although there is considerable variation in the presence and location of the muscle fascicles, the muscle exists in three broad layers, and about half of the quadratus lumborum fascicles acts on the twelfth rib and the rest exert their actions on the lumbar vertebra. The compressive forces exerted by the quadratus lumborum is insignificant compared with that exerted by the erector spinae and multifidus, and thus there is little evidence for a major stabilizing role of the quadratus lumborum on the lumbar spine.13
Technique
Quadratus Lumborum Trigger Point Injections Under Fluoroscopic Guidance
The authors have not performed these injections under ultrasound guidance; however, an anatomical study17 has been done involving the use of ultrasound guidance to identify the psoas and quadratus lumborum and erector spinae muscles. The study showed that these muscles are readily identified under ultrasonography, but this technique is not easily translated to overweight (body mass index, 25 to 29.9 kg/m2) or more obese patients. These authors identified the lumbar spinal levels by counting the images of the transverse processes starting at the level of the sacrum and proceeding in a cephalad direction. When using ultrasonography, the landmarks are first identified using the longitudinal view, where the probe is placed approximately 3 cm parallel to the spinous processes, then when at the desired level, rotating the probe to the short-axis or transverse view.17
Iliopsoas Muscle Injections
Establishing the Diagnosis
The major role of the iliopsoas, supported by EMG evidence, is the main hip flexor of the body.18 Pain coming from the iliopsoas, when ipsilateral, is close to the midline but described as being vertical along the spinal column, sometimes radiating to the groin. Occupations that require patients to sit for many hours (e.g., driving for long hours daily), particularly with their knees above their hips, leave the iliopsoas in prolonged contraction and subsequent possibility of pain.1 The psoas muscle is continuously active with prolonged sitting or standing, but the iliacus muscle is relatively inactive during standing.1 Patients often describe pain in the lower back when changing positions from sitting to standing, particularly arising from a deep seated chair. Coughing and deep breathing do not cause pain as they do with myofascial pain of the quadratus lumborum. Patients often elect to sleep in the fetal position at night, but they awaken from the fetal position and extend the back to get out of bed, thereby stretching the iliopsoas muscle. Iliopsoas pain may radiate to the hip and anterior thigh. Pain involving the iliopsoas bursa can be an important source of unilateral hip and groin pain. Iliopsoas muscle tendinitis is seen with activities that require repetitive hip flexion and may result in a snapping hip. Iliopsoas bursitis is seen with overuse injuries in gymnasts and uphill runners and cyclists, presenting with anterior hip and groin pain.19 Lumbar spinal stenosis most often affects L4-L5 then L3-L4 levels. Iliopsoas weakness, which may present as difficulty climbing stairs, has been described as an early sign of lumbar spinal stenosis because of its innervations by the muscles of the lumbar plexus.20
As with quadratus lumborum, myofascial pain involving the psoas muscle is a clinical diagnosis based on history and physical examination. Pathological processes involving the psoas muscle can be ruled out radiographically (e.g., hematoma and abscess). The physical examination starts with observation of the patient, including observation of the gait to look for an antalgic gait. It is difficult to palpate the iliopsoas muscle from the back, so provocative maneuvers will help with the diagnosis. The Thomas test, or inability to straighten the knee with the contralateral leg flexed while the patient is supine, has a positive result with a tight, contracted iliopsoas muscle. Pain is more often felt when rising from a seated position. Active straight-leg raise or resisted knee flexion causes pain. Prone hip extension that results in psoas stretch may also be painful. With iliopsoas bursitis, pain is felt with palpation at the insertion site in the femoral triangle at the lesser trochanter with the knee bent in the position used for the FABER (flexion abduction external rotation) test. Iliopsoas function is tested by passive testing of hip flexion strength; pain elicited by this maneuver may emanate from the iliopsoas.21
Anatomy
The iliopsoas is a combination of the psoas major, psoas minor, and iliacus muscles. The psoas major has its origin along the anterolateral vertebral column at the levels of T12-L4 and passes under the inguinal ligament to attach, along with the iliacus, as the iliopsoas muscle on the lesser trochanter of the femur. There is a large iliac bursa, which sometimes communicates with the hip joint.14 The psoas minor is only variably present in a segment of the population and has its origin along the transverse processes of L1-L5; it is anterior to the psoas major. The iliacus muscle originates in the iliac fossa of the pelvis and occupies the anterior portion of the pelvic brim. The psoas major combines with the iliacus muscle at approximately the level of the inguinal ligament and inserts on the lesser trochanter of the femur to become the functional unit called the iliopsoas muscle. The iliopsoas muscle is the most powerful thigh flexor in the body, which is its main function. It lies deep or anterior and medial to the quadratus lumborum. The iliopsoas muscle is covered by the iliacus fascia. It is only directly palpable at the level of the femoral triangle.
The psoas muscles are arranged in a very homogenous fashion such that the bundles from each of the individual segments are of the same length. Compared with its function as the major hip flexor, its significance with respect to the lumbar spine is limited except to use the lumbar spine as a base for its action on the hip.16,22 It is unique as a primary muscle of the leg in that its origins are from the lumbar spine.22 It has very little influence in lumbar flexion or extension; however, the psoas muscle does exert significant stress on the lumbar spine in the form of tremendous axial compressive and shear forces on the lower lumbar spine, particularly at the L5-S1 disc space. It also serves to increase the lumbar lordosis of the spine. This is maximized in activities that contract the psoas (e.g., sit-ups).22 EMG activity is controversial as to whether the iliopsoas plays some role in lateral rotation of the femur.14,19 The psoas major is innervated by the anterior (ventral) rami of L1-L3. The nerves of the lumbar plexus pass through the psoas major on route to the lower extremity.
Basic Science
Technique
Fluoroscopic Guidance
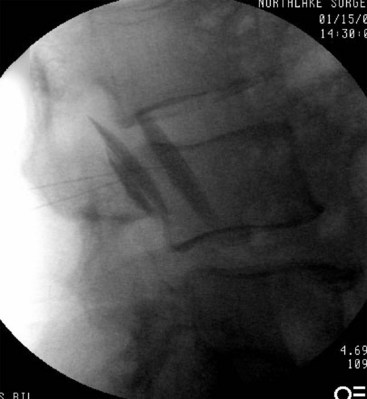
Sterile prep and drape are done. The L4 transverse process is visualized under fluoroscopy. Needle entrance is at the inferior edge of the transverse process, approximately 1 to 1.5 cm medial to the insertion site for the quadratus injection. The needed is advanced approximately 1 to 1.5 cm. One mL of nonionic contrast solution is injected to get good muscle spread along the psoas muscle (distinct pattern) without vascular spread. A lateral confirmatory view is obtained. Local anesthetic with or without steroid is injected. There should be no paresthesias, blood, or CSF with needle insertion. It is important to be mindful of the vascular structures (aorta and inferior vena cava) anterior and medial to the psoas muscle (Figs. 22-2 and 22-3).
Evaluation and Treatment of Pain from the Piriformis Muscle
Establishing a Diagnosis
The most common complaint with piriformis syndrome is gluteal (buttock) pain. Nearly the entire buttock (spanning from the sacral margin to the greater trochanter) can be painful and tender. This pain is usually made worse with prolonged sitting (classic complaint of pain during a long car ride) and with sit-to-stand transfers.23 It is rare to have associated axial back pain, although occasionally there can be associated paraspinal lumbar pain.23 Furthermore, the gluteal pain may radiate into the entire posterior thigh proximal to the knee as a function of posterior cutaneous nerve of the thigh irritation.24 If there is associated irritation of the entire sciatic nerve, symptoms can even extend all the way into the toes, although it is not common to develop true focal neurological deficits. Interestingly, because of the anatomical closeness of the piriformis muscle with the pelvic and abdominal walls, symptoms can occur with bowel movements and sexual activity.23
Historically, in about 50% of patients, there is an antecedent trauma. The traumatic event is not always direct trauma to the area, and there may be a lag of several months from the inciting trauma to the presentation of classic symptoms. The etiology of piriformis syndrome can even be total hip arthroplasty or spinal surgery.25 Other causes are quite variable and include true leg length discrepancy (and associated gait abnormality and pelvic tilt), idiopathic piriformis hypertrophy, and altered piriformis anatomy.26,27
On examination, piriformis tenderness can be elicited with deep palpation, and a spindle-shaped mass may be felt in the buttock.23 Although not specific for piriformis syndrome alone, symptoms are exacerbated by hip flexion, adduction, and internal rotation. Straight-leg raise results may or may not be positive based on whether or not the sciatic nerve is significantly affected. Sensory, motor, and reflex testing are almost always normal.23 Three tests that have more specificity for piriformis syndrome are the Pace sign, Lasègue sign, and Freiberg sign:
Anatomy
The proximal insertions of the piriformis muscle include the S2-S4 sacral vertebra, the sacroiliac joint capsule, and the posterior iliac spine.26 From these insertions, the muscle spans laterally through the greater sciatic foramen and attaches distally to the medical surface of the greater trochanter. Innervation to the piriformis muscle is provided by the L5, S1, and S2 spinal nerves. The sciatic nerve (either in divided or undivided form) passes directly through the muscle, under the muscle (most commonly), or above the muscle in very close proximity. The gluteal nerves and vessels and the posterior cutaneous nerve to the thigh also traverse below the muscle.23
Basic Science
Similar to most skeletal muscles, direct trauma to the buttock can result in muscle spasm and release of proinflammatory mediators. Proinflammatory prostaglandins, histamine, bradykinin, and serotonin are released into the inflamed muscle belly (further propagating local inflammatory processes). Furthermore, because the sciatic nerve is so close to the piriformis, these same mediators can cause a chemical irritation of the sciatic nerve.31 An inflamed and spastic piriformis muscle can also cause mechanical compression of the sciatic nerve.26
Imaging
Although magnetic resonance imaging (MRI) and computed tomography (CT) may show an enlarged piriformis muscle,32 piriformis syndrome still is truly a clinical diagnosis made with thorough history and physical examination. Depending on the cut of the MRI and the fluctuations in muscle swelling and reactivity, the imaging study results may be negative despite significant disease of the tissue.
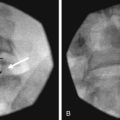
Technique
In the technique described by Benzon et al,31 the patient is placed prone on a fluoroscopy table, and the inferior margin of the sacroiliac joint is imaged and marked. Then an insulated block needle is inserted 1 to 2 cm caudad and 1 to 2 cm lateral to the inferior margin of the sacroiliac joint. The insulated needle should be advanced with the nerve stimulator on until a sciatic nerve–evoked motor response is achieved (dorsiflexion, plantarflexion, eversion, inversion). The needle is slightly withdrawn until the sciatic stimulation disappears. Steroid (40 mg of either methylprednisolone or triamcinolone) plus 5 mL of saline is injected perisciatically. The needle is pulled back 1 cm (into the belly of the piriformis muscle), and the contrast is injected (Fig. 22-4). The contrast should outline the piriformis muscle belly, which will either appear as one single muscle unit or two muscle bellies if the piriformis is split by the sciatic nerve. After the characteristic dye spread is achieved, local anesthetic solution and steroid are administered. Typically, good pain relief can be attained with an injection of 5 mL of 0.5% bupivacaine plus 40 mg of methylprednisolone (or triamcinolone).
A similar technique has been described using CT guidance, but the lack of readily available CT suites and the added radiation hazard limit this technique.33 Further, similar blind techniques have been described as well as a perisciatic stimulator approach without fluoroscopic guidance.34 Similarly, the piriformis muscle can be visualized with ultrasound although this requires a higher level of expertise with the ultrasound machine, especially in the obese patient.
Outcomes Evidence
Using the technique described, Benzon and colleagues31 were able to achieve some short- or long-term relief of symptoms in 16 of 19 patients. It should be noted that most of these patients had fairly severe and chronic pain with multiple pain generators (not isolated piriformis syndrome).
1 Simons DG, Travell J, Simons LLS. Travell and Simons’ myofascial pain and dysfunction: the trigger point manual, ed 2. Philadelphia: Lippincott Williams & Wilkins; 1999.
2 Han SC, Harrison P. Myofascial pain syndrome and trigger-point management. Reg Anesth. 1997;22:89-101.
3 Testa M, Barbero M, Gherlone E. Trigger points: update of the clinical aspects. Eur Med Phys. 2003;39:37-43.
4 Hubbard DR, Berkoff GM. Myofascial trigger points show spontaneous needle EMG activity. Spine. 1993;18:1803-1807.
5 Rivner MH. The neurophysiology of myofascial pain syndrome. Curr Pain Headache Rep. 2001;5:432-440.
6 Huguenin LK. Myofascial trigger points: the current evidence. Physical Ther Sports. 2004;5:2-12.
7 Cummings TM, White AR. Needling therapies in the management of myofascial trigger point pain: a systematic review. Arch Phys Med Rehabil. 2001;82:986-992.
8 Foster AH, Carlson BM. Myotoxicity of local anesthetics and regeneration of the damaged muscle fibres. Anesth Analg. 1980;58:727-736.
9 Wald JJ. The effects of toxins on muscle. Neurol Clin. 2000;18:695-717.
10 Hong CZ. Myofascial trigger points: pathophysiology and correlation with acupuncture points. Acupunct Med. 2000;18:41-47.
11 Salmons S. Muscle. In Gray’s anatomy, ed 38, St. Louis: Churchill Livingstone; 1995:737-900.
12 Ranson C, Burnett A, O’Sullivan P, et al. The lumbar paraspinal muscle morphometry of fast bowlers in cricket. Clin J Sport Med. 2008;18:31-37.
13 Phillips S, Mercer S, Bodguk N. Anatomy and biomechanics of quadratus lumborum. Proc Inst Mech Eng H. 2008;222(2):151-159.
14 Porterfield JA, DeRosa C. Lumbopelvic musculature: structural and functional considerations. In Mechanical low back pain: perspectives in functional anatomy, ed 2, Philadelphia: WB Saunders; 1998:53-119.
15 Knutson GA. Anatomic and functional leg-length inequality: a review and recommendation for clinical decision-making. Part II, the functional or unloaded leg-length asymmetry. Chiropr Osteopat. 2005;13:1-6.
16 Bogduk N. The lumbar muscles and their fascia. In: Twomey LT, Taylor JR, editors. Physical therapy of the low back. ed 3. Philadelphia: Churchill Livingston; 2000:105-139.
17 Kirchmair L, Entner T, Wissel J, et al. A study of the paravertebral anatomy for ultrasound-guided posterior lumbar plexus block. Anesth Analg. 2001;93:477-481.
18 Basmajian JV. Electromyography of the iliopsoas. Anat Rec. 1958;132(2):127-132.
19 Hip and thigh. In: Percina MM, Bojanic I, editors. Overuse injuries of the musculoskeletal system. ed 2. Boca Raton, FL: CRC Press; 2004:153-188.
20 LaBan MM. Iliopsoas weakness: a clinical sign of lumbar spinal stenosis. Am J Phys Med Rehabil. 2004;83:224-225.
21 Magee DJ. Hip. Orthopedic physical assessment, ed 5. St. Louis: Saunders Elsevier. 2008.
22 Bogduk N, Pearcy M, Hadfield G. Anatomy and biomechanics of psoas major. Clin Biomech. 1992;7:109-119.
23 Parziale JR, Hudgins TH, Fishman LM. The piriformis syndrome. Am J Orthop. 1996;25:819-823.
24 Barton PM. Piriformis syndrome: a rational approach to management. Pain. 1991;47:345-352.
25 Cameron HU, Noftal F. The piriformis syndrome. Can J Surg. 1988;31:210.
26 Hallin RP. Sciatic pain and the piriformis muscle. Postgrad Med. 1983;74:69-72.
27 Chen WS. Bipartite piriformis muscle: an unusual cause of sciatic nerve entrapment. Pain. 1994;58:269-272.
28 Cameron HU, Noftal F. The piriformis syndrome. Can J Surg. 1988;31:210.
29 Robinson D. Piriformis syndrome in relation to sciatic pain. Am J Surg. 1947;73:355-358.
30 Freiberg AH. Sciatic pain and its relief by operations on muscle and fascia. Arch Surg. 1937;34:337-350.
31 Benzon HT, Katz JA, Benzon HA, Iqbal MS. Piriformis syndrome: anatomic considerations, a new injection technique, and a review of the literature. Anesthesiology. 2003;98:1442-1448.
32 Jankiewicz JT, Hennrikus WL, Houkom JA. The appearance of the piriformis muscle in computed tomography and magnetic resonance imaging: a case report and review of the literature. Clin Orthop. 1991;262:205-209.
33 Porta M. A comparative trial of botulinum toxin type A and methylprednisolone for the treatment of myofascial pain syndrome and pain from chronic muscle spasm. Pain. 2000;85:101-105.
34 Hanania M, Kitain E. Perisciatic injection of steroid for the treatment of sciatica due to piriformis syndrome. Reg Anesth Pain Med. 1998;23:223-228.