38
Mucinoses
In this group of disorders, there is deposition of glycosaminoglycans, previously referred to as mucopolysaccharides (‘mucin’), within the skin, especially the dermis. Most frequently, the deposit is composed of hyaluronic acid. While several of the entities are idiopathic, underlying disorders include autoimmune thyroid disease, a monoclonal gammopathy, and diabetes mellitus.
Scleredema
• Symmetric diffuse induration of the skin, usually limited to the upper back and posterior neck, that may require palpation to be appreciated; a peau d’orange appearance may be present with prominent follicular orifices, and occasionally there is blanching erythema in the sites of involvement (Fig. 38.1).

Fig. 38.1 Scleredema in association with diabetes mellitus. Diffuse induration of the upper back and neck with overlying erythema.
• DDx: systemic sclerosis (diffuse form), scleromyxedema, and other sclerodermoid disorders (see Table 35.4); occasionally, cellulitis if erythema is present.
Scleromyxedema/Papular Mucinosis
• A spectrum of clinical findings that varies from multiple linear arrays of firm, 2- to 3-mm, waxy, skin-colored papules (Fig. 38.2) to diffuse induration of the skin with thickened folds, including leonine facies (Fig. 38.3; Table 38.1); involvement is symmetric and often widespread.
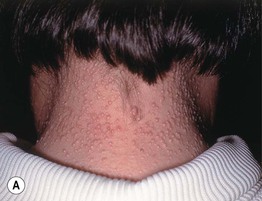

Fig. 38.2 Scleromyxedema/papular mucinosis. A, B Numerous monomorphic, firm, skin-colored papules which can have a linear arrangement (most obvious on the upper back).


Fig. 38.3 Scleromyxedema/papular mucinosis. Thickening of the skin of the forehead (A) and trunk (B), leading to deep furrows and folds. Scleromyxedema is one of the causes of leonine facies. Courtesy, Joyce Rico, MD.
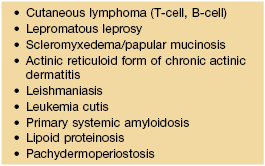
Table 38.1
Leonine facies – associated dermatologic diseases.
Additional causes include sarcoidosis, mastocytosis, multicentric reticulohistocytosis, and progressive nodular histiocytosis.
• Rx: similar to that of multiple myeloma (see primary systemic amyloidosis, Chapter 39), systemic retinoids, PUVA, UVA1.
Pretibial Myxedema
• Favors the shins but can involve the foot and presents as indurated, waxy nodules or plaques that vary from skin-colored to red-brown (Fig. 38.4); there can be a prominence of follicular openings (peau d’orange appearance) and occasionally elephantiasis develops.

Fig. 38.4 Pretibial myxedema. Purple-brown plaques on the shins of a patient with Graves’ disease. A peau d’orange appearance is present due to prominent follicular openings. Courtesy, Franco Rongioletti, MD, and Alfredo Rebora, MD.
• Additional clinical findings include exophthalmos, goiter, and thyroid acropachy.
• Rx: although lesions may clear spontaneously over a period of several years, treatment of the underlying thyroid disease usually has no effect; anecdotal therapies include topical and intralesional CS, pneumatic compression, surgical shave removal, octreotide.
Generalized Myxedema
Self-Healing Cutaneous Mucinosis
Reticular Erythematous Mucinosis (REM)
• Persistent erythematous papules of the central chest and central back that can form a net-like pattern and/or coalesce into plaques (Fig. 38.5); may be photo-aggravated.

Fig. 38.5 Reticular erythematous mucinosis (REM). Grouped pink papules on the central chest with no surface changes; there is a subtle annular and reticulated configuration. Note the significant tan.
• Rx: topical or intralesional CS, antimalarials, e.g. hydroxychloroquine, chloroquine, sunscreens.
Cutaneous Lupus Mucinosis/Papulonodular Mucinosis (of Gold)
• Skin-colored to erythematous papules and nodules that may require side-lighting to appreciate; favors the back, V of the chest and upper extremities (Fig. 38.6).

Fig. 38.6 Cutaneous lupus mucinosis/papulonodular mucinosis. Skin-colored papules and nodules leading to a ‘lumpy’ appearance to the skin that is best appreciated by side-lighting. Courtesy, Franco Rongioletti, MD, and Alfredo Rebora, MD.
• Rx: antimalarials, e.g. hydroxychloroquine, chloroquine, topical or intralesional CS, sunscreens.
Follicular Mucinosis (Alopecia Mucinosis)
• In the primary form, there are pink to violet-brown plaques, primarily in the head and neck region, that have associated alopecia and sometimes scale (Fig. 38.7A); in some patients, there are grouped follicular papules (Fig. 38.7B), and in patients with darkly pigmented skin, lesions may be hypopigmented.


Fig. 38.7 Follicular mucinosis. A Pink plaque containing follicular papules in a young boy. B Grouped follicular papules on the leg of an older adult in association with violet-brown plaques; note the associated alopecia. The hemorrhagic crust is the site of a previous biopsy. A, Courtesy, Lorenzo Cerroni, MD.
• Rx: for primary, observation until spontaneous resolution, topical or intralesional CS, antimalarials; if associated with mycosis fungoides, treat the latter (see Chapter 98).
Other Entities
Digital mucous cyst is covered in Chapter 90. Cutaneous mucin deposits can also be seen within tumors (e.g. basal cell carcinomas, cutaneous metastases) and inflammatory disorders (e.g. granuloma annulare, cutaneous LE, dermatomyositis).
For further information see Ch. 46. From Dermatology, Third Edition.







