41
Monitoring of the fetus in labour
Introduction
The purpose of monitoring the fetus in labour is to try and identify those which might be at risk of hypoxic injury so that delivery can be expedited and potential problems prevented. This process of monitoring usually involves some form of fetal heart rate assessment, either with intermittent auscultation or by continuous electronic measurement (cardiotocography, CTG) and analysis of the fetal ECG waveform. Intermittent auscultation of the fetal heart is appropriate for monitoring fetal condition in low-risk labour, with electronic fetal monitoring being used either in high-risk labour or if concern is raised by intermittent auscultation in low-risk patients. The CTG is good at identifying the normal healthy fetus but there is a high false positive rate and many fetuses labelled as ‘distressed’ are actually not hypoxic. As a consequence, the rate of obstetric intervention may be increased in return for no neonatal benefit. Analysis of the ECG waveform in association with the CTG can improve its predictive ability for hypoxia.
Fetal physiology
Fetal oxygenation depends on a number of factors.
Maternal blood supply to the placenta
During a contraction, the intramural vessels supplying the placenta are constricted by the smooth muscle fibres of the uterus. Providing the contractions are not too long or too frequent, the placental blood supply has time to recover before the next contraction begins. In hyperstimulation, when the uterus is contracting too frequently, placental oxygenation may be impaired. In other circumstances, there may be placental hypoperfusion, for example following the distal sympathetic blockade and associated hypotension, which can occur with spinal or epidural anaesthesia.
Functional capacity of the placenta
A small, poorly-formed placenta is less capable of adequate oxygen transfer than a larger placenta. In this condition, the fetus may already be growth restricted prior to the onset of labour and therefore more susceptible to a hypoxic stress. In abruptio placentae, it is obvious that the resulting partial placental separation leaves a reduced surface area for vascular communication, and is therefore less efficient at oxygen exchange.
Fetal blood supply
This is dependent on adequate fetal cardiac output. The fetus responds to hypoxic stress with peripheral vasoconstriction and redistribution of the blood to the heart and the brain. Prolonged vasoconstriction may lead to damage in other organs, particularly the gastrointestinal tract (necrotizing enterocolitis), the lungs (respiratory distress) and kidneys (acute renal failure).
Hypoxia also leads to anaerobic metabolism and acidosis. Acidosis is therefore a reflection of the degree of oxygenation, and this forms the basis of intrapartum fetal blood sampling.
Risk assessment
Some form of monitoring is appropriate for all labours, but whether this should be continuous or intermittent is unclear. As noted above, the use of continuous electronic monitoring in ‘low-risk’ labours may increase the rate of intervention for no demonstrable neonatal benefit. It is therefore important to consider which babies are ‘high risk’ and which are ‘low risk’. Some of these factors are outlined in Box 41.1. It is important to take these background factors into consideration before interpreting a heart rate problem.
Meconium staining of the liquor
Meconium (fetal stool) staining of the liquor is present in 15% of all deliveries at term and in about 40% at 42 weeks. The mechanism may be stimulation of the vagus (parasympathetic) nerves in utero causing the fetal gut to contract and the anal sphincter to relax. This often happens for no particular reason but it also may occur as a response to fetal hypoxia. While often not of clinical significance, the presence of meconium staining increases the likelihood that there is underlying fetal compromise. A normal cardiotocograph (CTG) provides reassurance, but an abnormal CTG becomes more significant in the presence of meconium and should lower the threshold for investigation or intervention.
As well as being a sign of fetal distress, meconium is found below the vocal cords postnatally in about one-third of cases in which it is present, and may give rise to the meconium aspiration syndrome. This is a form of neonatal pneumonitis. Clinical features range from mild neonatal tachypnoea to severe respiratory compromise. The incidence is probably unrelated to fetal hypoxia (and indeed the majority of babies with meconium aspiration syndrome are not acidotic at delivery) but the syndrome is more likely to be severe if there is associated hypoxia/acidosis. It is also more severe when the meconium is thick. There is no evidence to support early delivery in the absence of fetal distress, as it is likely that the aspiration occurs in utero rather than at delivery itself.
Meconium can be graded as follows:
Grade 1: good volume of liquor stained lightly with meconium
Grade 2: reasonable volume of liquor with heavy suspension of meconium
Grade 3: thick undiluted meconium of ‘pea-soup’ consistency.
The higher the grade, the more likely it is to be associated with metabolic acidosis and the meconium aspiration syndrome. It is appropriate to consider continuous electronic fetal heart rate recording if meconium is found to be present.
Fetal heart rate recording
Intermittent monitoring
Assessment of the fetal heart rate can be used to provide some information about fetal well-being. In ‘low-risk’ labours, it is recommended to auscultate the fetal heart every 15 min before and after a contraction during the first stage of labour, and every 5 min between contractions in the second stage of labour. A baseline tachycardia or bradycardia, and the presence of decelerations are indications for further evaluation with continuous CTG monitoring. The heart can be auscultated using either a manual Pinard stethoscope or an electronic Doppler detector.
Continuous monitoring (cardiotocography)
A cardiotocograph (CTG) provides a continuous printed record of the fetal heart rate and uterine contractions. The contractions are registered by a pressure monitor supported on the mother’s abdomen by an elastic belt, and the fetal heart rate is measured using either:
![]() an abdominal ultrasonic transmitter–receiver Doppler probe, which detects fetal cardiac movements and hence the heart rate, or
an abdominal ultrasonic transmitter–receiver Doppler probe, which detects fetal cardiac movements and hence the heart rate, or
![]() a clip, known as a fetal scalp electrode (FSE), which is attached to the baby’s scalp and detects the R–R wave of the fetal ECG. It is usually used if the external abdominal monitoring is unsatisfactory.
a clip, known as a fetal scalp electrode (FSE), which is attached to the baby’s scalp and detects the R–R wave of the fetal ECG. It is usually used if the external abdominal monitoring is unsatisfactory.
The important features of a CTG are given in Table 41.1. Normally, the baseline fetal heart rate is between 110 and 160 beats per minute (bpm). This rate represents a balance between the sympathetic and parasympathetic systems. Sustained tachycardia is associated with prematurity, and the rate slows physiologically with advancing gestation. It may also be associated with fetal acidosis (probably as a response to increased sympathetic stimulation), maternal pyrexia and the use of exogenous beta-sympathomimetics. Baseline bradycardia is associated with severe fetal acidosis (e.g. abruption or uterine rupture) but is more commonly found with hypotension. Congenital heart block is rare, but can occur especially in association with maternal systemic lupus erythematosus. Cardiac dysrhythmias are also rare but can cause extremes of heart rate, either fast or slow, with tachycardia usually being the more frequently encountered.
Table 41.1
Features of a cardiotocograph
| Normal heart rate | 110–160 bpm | Reassuring |
| Baseline variability | 5–25 bpm | Reassuring |
| Accelerations | Reassuring | |
| Decelerations | Early | These occur at the time of the contraction and are rarely of more than 40 bpm They are probably related to parasympathetic stimulation associated with head compression, and are unlikely to be of clinical significance |
| Variable | These are variable in their timing in relation to the timing of the contraction They are associated with cord compression and may lead to fetal hypoxia |
|
| Late | These occur after the contraction, may be of low amplitude and are suggestive of fetal hypoxia |
Baseline variability is the variation in the fetal heart rate and is due to the balance between the parasympathetic and the sympathetic nervous systems. Since the nervous system of the baby develops as pregnancy advances, the baseline variability is reduced at earlier gestations. Baseline variability is described as normal, reduced or absent, and it gives a relatively good indication of well-being. The normal is 5–25 bpm (according to NICE). The commonest reason for loss of baseline variability is the ‘sleep’ or ‘quiet’ phase of the fetal behavioural cycle, which may last up to 40 min. Loss of variability is also associated with prematurity, acidosis and drugs (e.g. opiates or benzodiazepines). Fetal acidosis is much more likely if there is reduced variability in the presence of late decelerations.
Accelerations of the fetal heart rate are a sign of a healthy fetus but their absence in advanced labour is not unusual. Antenatally, there should be at least two accelerations per 15 min, each with an amplitude > 15 bpm and lasting for at least 15 s.
Decelerations are of at least 15 bpm and last for more than 15 s. Early decelerations occur with contractions. If decelerations occur more than 15 s after the contraction, they are termed ‘late’. ‘Variable’ decelerations vary in both timing and shape:
![]() early decelerations reflect increased vagal tone (intracranial pressure rises during a contraction) and are probably physiological
early decelerations reflect increased vagal tone (intracranial pressure rises during a contraction) and are probably physiological
![]() variable decelerations may represent cord compression (particularly in oligohydramnios). A small increase in FHR at the beginning and end of a deceleration (shouldering) suggests that the fetus is coping well with the stress of the intermittent compressions. Variable decelerations may resolve if the mother’s position is changed
variable decelerations may represent cord compression (particularly in oligohydramnios). A small increase in FHR at the beginning and end of a deceleration (shouldering) suggests that the fetus is coping well with the stress of the intermittent compressions. Variable decelerations may resolve if the mother’s position is changed
![]() late decelerations suggest reduced placental perfusion and hypoxia during that period. Shallow late decelerations in a non-reactive trace with absent baseline variability may be particularly ominous.
late decelerations suggest reduced placental perfusion and hypoxia during that period. Shallow late decelerations in a non-reactive trace with absent baseline variability may be particularly ominous.
A true sinusoidal trace is rare. This is a smooth undulating sine-wave-like baseline with no variability. It may represent fetal anaemia but can be a feature of fetal physiological behaviour. It should be considered to be serious until proven otherwise.
Fetal ECG
Analysis of the fetal ECG in labour can improve the specificity (i.e. reduce the number of false positives) of the CTG. A fetal scalp electrode (FSE) is required to obtain the ECG, the signal from which is a reflection of the electrical activity in the heart (the myocardium). The P wave corresponds to contraction of the atria, the QRS complex contraction of the ventricles and the T wave regeneration of myocardial membrane potentials prior to the next contraction.
Myocardial hypoxia leads to changes in the ECG waveform:
![]() an increased amplitude of the T wave – the ratio between the height of the T wave and the QRS amplitude (T/QRS ratio) gives an accurate measurement of changes in T wave height and its increase can be episodic (rises and returns with each contraction) or a steady rise in baseline T/QRS. The elevated T wave is the result of potassium release in association with the mobilization of stored glucose (glycogen) within the myocardium
an increased amplitude of the T wave – the ratio between the height of the T wave and the QRS amplitude (T/QRS ratio) gives an accurate measurement of changes in T wave height and its increase can be episodic (rises and returns with each contraction) or a steady rise in baseline T/QRS. The elevated T wave is the result of potassium release in association with the mobilization of stored glucose (glycogen) within the myocardium
![]() changes in the shape of the ST segment, characteristically the appearance of a biphasic pattern, is thought to be the result of the depressant effect of hypoxia on myocardial function.
changes in the shape of the ST segment, characteristically the appearance of a biphasic pattern, is thought to be the result of the depressant effect of hypoxia on myocardial function.
Used in conjunction with the CTG, fetal ECG analysis has been shown to result in fewer babies with severe metabolic acidosis at birth, fewer babies with neonatal encephalopathy, and fewer operative vaginal deliveries. The use of fetal ECG with CTG also reduces the need for fetal blood sampling (as described below).
Fetal blood sampling (FBS)
This is also known as fetal scalp sampling (FSS) and is a diagnostic test for fetal acidosis. As mentioned above, CTGs are used as a screening test to detect babies who may be developing ‘distress’ as measured by metabolic acidosis. CTGs are highly sensitive (good at detecting true positives) but very poorly specific (there are many false positives). In other words, when the CTG is normal, the baby is very likely to be well, but the majority of pathological CTGs occur in babies who are not distressed. CTGs used on their own, lead to an approximately four-fold increase in caesarean section rates for presumed fetal distress, a figure much reduced if fetal blood sampling is used to identify a normal pH in the false positives.
Using an amnioscope, a tiny amount of blood is removed from the scalp (see below) and both pH and base excess are measured. Normal maternal pH is 7.38 but the normal range of fetal pH is broader, extending to as low as 7.20. In the presence of hypoxia the fetus compensates by anaerobic glycolysis. This leads to an accumulation of lactic acid and a fall in the pH. FBS carries a very small risk of fetal scalp haemorrhage and infection.
Indications for fetal blood sampling
1. Persistent late or atypical variable decelerations on CTG
2. Persistent fetal tachycardia
3. Prolonged and persistent decelerations
4. Significant meconium-stained liquor (Grade 2 or 3) along with any CTG abnormality
5. Prolonged period of loss of baseline variability.
FBS is contraindicated where there is a risk of infection transmitted from the mother (e.g. HIV, hepatitis B, herpes), a fetal bleeding diathesis (e.g. Von Willebrand disease) and before 34 weeks’ gestation.
Method of fetal blood sampling
The mother is placed in the lithotomy position with 15° lateral tilt (or in the left lateral position if approaching full dilatation). An amnioscope appropriate for the dilatation is inserted and the scalp is dried with a sponge or swab on long sponge-holders. The scalp is then sprayed with ethyl chloride to induce hyperaemia and the area is covered with a thin layer of paraffin jelly (so that the blood will form a blob and not run). A blade is used to make a small nick in the scalp and the blob is touched with the capillary tube. Where possible, three samples are taken to ensure consistency of results.
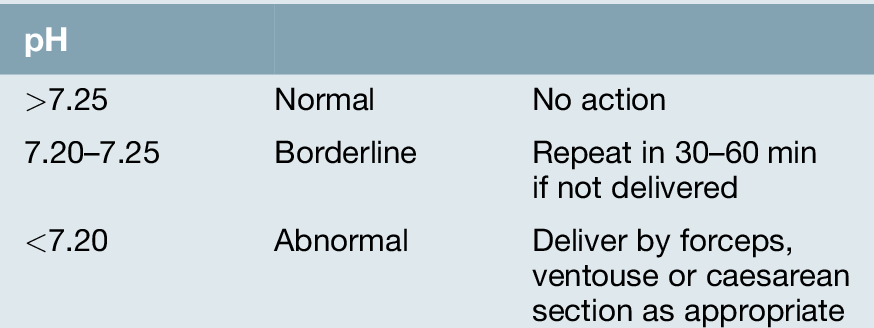
Interpretation of results
The scalp blood pH reflects the state of the fetus only at the time of the sample, while the ‘base excess’ reflects a change over a longer period. The pH is plotted on a logarithmic scale, whereas base excess is on a linear scale, e.g. a fetus with a pH of 7.22 and a base excess of − 12 mEq/L is more likely to be at risk than one with a similar pH and base excess of − 6 mEq/L. The correlation between CTGs and scalp pH is not precise but as a general rule:
![]() if all four components of the CTG are normal, the risk of a pH < 7.20 is ~ 2%
if all four components of the CTG are normal, the risk of a pH < 7.20 is ~ 2%
![]() with one or two components of the CTG abnormal, the risk of a pH < 7.20 is ~ 20%
with one or two components of the CTG abnormal, the risk of a pH < 7.20 is ~ 20%
![]() with two to four components of the CTG abnormal, the risk of a pH < 7.20 is ~ 50%.
with two to four components of the CTG abnormal, the risk of a pH < 7.20 is ~ 50%.
It is common practice to deliver the baby if the pH is < 7.20, although it may be the rate of fall in pH rather than the absolute value which is relevant. See Tables 41.2 and 41.3.
Table 41.3
Base excess results following fetal blood sampling
| Base excess | |
| <−6 mEq/L | Normal |
| − 6.1 to − 7.9 mEq/L | Borderline |
| >−8 mEq/L | Metabolic acidosis |
Clinical examples of fetal monitoring scenarios with corresponding CTGs
The cervix was 3 cm dilated and fully effaced, but there was thick meconium staining. The CTG was reassuring, however, with a baseline of 130 bpm, good baseline variability and accelerations. She was given diamorphine 7.5 mg for pain relief.
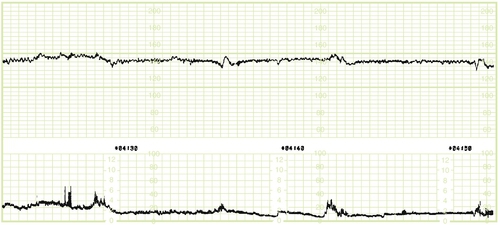
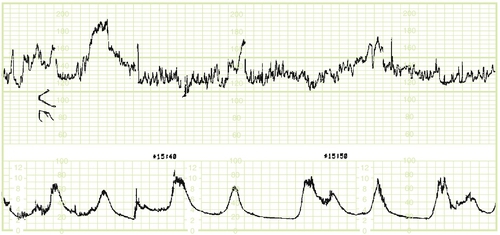
Fig. 41.2After a further 2 h, however, there was loss of baseline variability.
Although there were no decelerations, it was recognized that meconium is a marker for fetal compromise and it was decided to perform fetal blood sampling. The pH was within the normal range at 7.31 and she went on to have a normal delivery 3 h later.
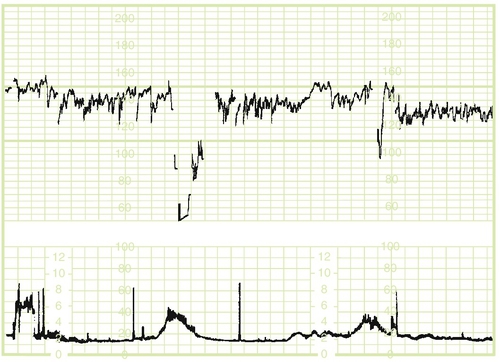
Fig. 41.3A 40-year-old primigravida was admitted after spontaneous rupture of membranes.
The liquor was clear and she was having mild contractions once every 8 min. The CTG baseline was 130–140 bpm with good reactivity but there were variable decelerations. These are not uncommon after membrane rupture as liquor cushions the baby and cord compression is less likely. Because the rest of the CTG was reassuring, she was allowed to establish in labour spontaneously. The decelerations resolved, but she required a caesarean section for failure to progress beyond 8 cm, despite syntocinon. The baby was in an occipitoposterior position.
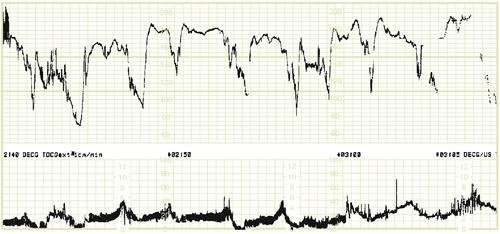
Fig. 41.4A 27-year-old primigravida who was induced at 40 weeks + 12 days, as she was ‘post-dates’.
After prostaglandin gel was given vaginally, the cervix was suitable for membrane rupture and the induction was continued with syntocinon. This trace is at 6 cm and it shows a baseline around 180 bpm with reduced variability and late decelerations. Fetal blood sampling showed a pH of 7.28, but on repetition 30 min later, the pH was 7.19. By this stage, the cervix was fully dilated and she had an uneventful ventouse delivery.
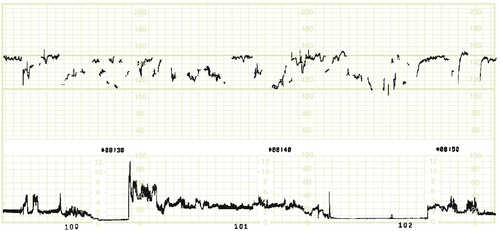
Fig. 41.5A 19-year-old primigravida, who weighed 105kg at booking, was admitted in early labour.
The CTG shows poor pick-up from the abdominal Doppler probe and, after the membranes were ruptured, a scalp clip was applied. The subsequent traces were reassuring and she had a normal delivery.
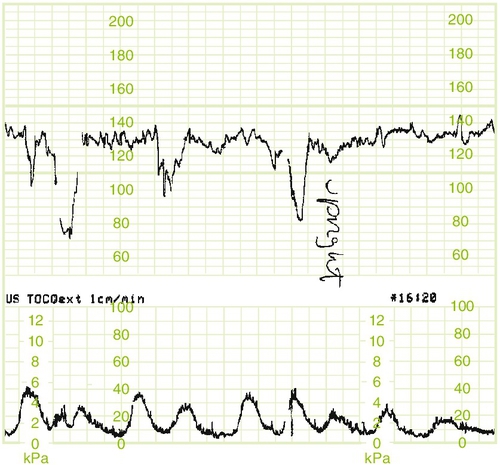
Fig. 41.6A 26-year-old primigravida was induced at 33 weeks for worsening pre-eclampsia.
The baby’s estimated weight was on the 10th centile but liquor volume, biophysical profile and CTG were all normal; 8 h after administration of the prostaglandin gel, with the cervix still closed, there were three unprovoked variable decelerations. While the relatively reassuring baseline variability might have warranted more conservative management in a normally grown term fetus, the underlying factors were felt sufficient to warrant caesarean section. The baby, weighing 1.6 kg, had Apgar scores of 9 and 10 at 1 and 5 min and made uneventful progress.

Fig. 41.7A 34-year-old primigravida at 4 cm who had just had an epidural sited.
After epidural top-up there was a baseline bradycardia, which recovered to a tachycardia and settled again to normal. It is recognized that the peripheral hypotension associated with regional anaesthesia leads to placental hypoperfusion and fetal bradycardia. The bradycardia usually resolves spontaneously.
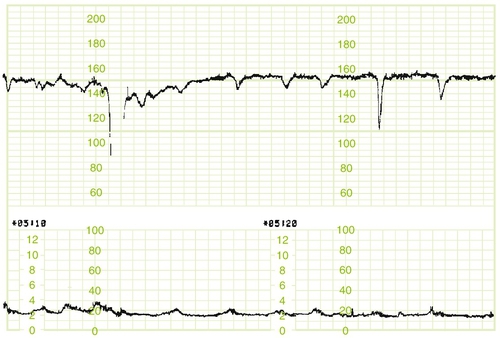
Fig. 41.8A primigravida who was admitted from home at 8 cm dilatation.
She had been quite sore at home, but was not expecting to be at such an advanced stage of labour. The CTG had virtually no baseline variability and there were shallow late decelerations. A fetal blood sample showed a pH of 7.09 and a caesarean section was carried out. The baby had Apgar scores of 3 at 1 min and 7 at 5 min, and weighed only 2.23 kg at 37 weeks’ gestation. The baby made excellent progress.
Long-term prognosis following delivery
There are two key issues to be considered here:
1. Whether a particular infant, born with apparent compromise, will later turn out to be neurologically normal, i.e. prospective prediction
2. Whether an infant, later discovered to be affected by cerebral abnormality, sustained its injury prior to the onset of labour or as the result of some intrapartum insult, i.e. retrospective evaluation.
Before considering these two overlapping issues, it should be noted that the term ‘birth asphyxia’ is best avoided unless there is evidence of a pale baby with no tone and not breathing with evidence of metabolic acidosis on cord arterial blood.
Prospective prediction
The actual length of time and degree of hypoxia required to produce cerebral palsy in a previously healthy fetus are unknown but there are specific mechanisms which protect the fetus for considerably longer than an adult with similar blood gas concentrations. Nonetheless, hypoxia, whether of antenatal or intrapartum origin, can cause cerebral injury, and attempts have been made to correlate status at delivery with long-term neurological outcome. CTG abnormalities, Apgar scores, neonatal behaviour and neonatal brain imaging have all been evaluated.
CTGs and Apgar scores are of very limited value in assessing long-term prognosis. There is a high incidence of non-reassuring CTGs in what are later shown to be normal infants. The same is true for Apgar scores, which are intended as a guide to the need for resuscitation rather than a reflection of the degree of hypoxic injury. Low Apgar scores do not indicate the cause of the baby’s poor condition, and are a reflection of its immediate status. Prolonged low values, however, are a more useful guide. Of those babies with an Apgar score < 3 at 10 min, two-thirds usually die within 1 year, and of the survivors, a significant proportion are normal.
Abnormal neonatal behaviour, referred to as ‘neonatal encephalopathy’, is considerably more useful. This is a clinically defined syndrome of disturbed neurological function occurring during the first week after birth characterized by difficulty with initiating and maintaining respiration, depression of tone and reflexes, altered level of consciousness, and seizures. There are three grades:
1. Hyper-alert and jittery with reduced tone and dilated pupils. This usually resolves within 24 h without long-term sequelae
2. Lethargic, with seizures and a weak suck. There is a 15–27% chance of severe sequelae
3. Flaccid, no suck, no Moro reflex and prolonged seizures. The chance of severe sequelae is nearly 70–80%.
The prognosis is generally good if the baby does not develop Grade 3 neonatal encephalopathy or if Grade 2 neonatal encephalopathy lasts less than 5 days.
Radiological assessment is also of value in assessing long-term neurological function. The prognosis is good if a CT or MRI scan appears normal but is less good if there is evidence of cerebral damage. At term, partial but prolonged hypoxia (as indicated by repeated decelerations with loss of variability over a prolonged period) may give rise to motor cortical atrophy and quadriplegia; if the hypoxia is sudden and profound (as with a prolonged bradycardia), it is more likely to result in injury to the thalamus giving rise to an athetoid or dyskinetic type of cerebral palsy.
Early cerebral oedema suggests a recent event, as oedema usually appears within 6–12 h of an insult and clears by 4 days afterwards. Further clinical evaluation may be available from an electroencephalograph (EEG). The incidence of death or handicap is low if the EEG is normal. Often, however, despite these measures, the prognosis cannot be defined with accuracy and only long-term follow-up will reveal the true clinical picture.
Retrospective evaluation
Cerebral palsy, which is characterized by non-progressive abnormal control of movement or posture, is usually not diagnosed until months or years after birth and it is often at this point that questions are asked about whether the cause lay in some difficulty with the delivery. In many instances, it is impossible to say whether the cerebral insult was antenatal in origin or whether it truly occurred in labour, but this apparently academic point has two important implications. First, if most cases of cerebral palsy are antenatal in origin, then no amount of intrapartum monitoring will affect the eventual outcome. Second, there may be major medicolegal ramifications. If a cerebral insult is found to have occurred as the result of negligence during labour, a potentially very large sum of money may need to be paid in compensation.
Epidemiological studies suggest that in about 90% of cases, the cerebral injury is antenatal in origin, and that in the remaining 10%, the problems may have been the result of either antenatal or intrapartum difficulties. In particular, there is a strong association with prematurity, fetal growth restriction, intrauterine infection, fetal coagulation disorders, antepartum haemorrhage and chromosomal or congenital anomalies. Many are idiopathic. Intrapartum complications appear to play only an infrequent role in the causation of cerebral palsy. Reduced CTG variability in early labour from time of admission, meconium staining, low Apgar scores and neonatal encephalopathy may suggest possible pre-existing cerebral injury from some earlier antenatal event.
There are many conflicting views about the criteria required to implicate intrapartum events as the cause of cerebral injury. One set of views is expressed in Box 41.2, but, while accepted by many, they are not the universal views of all clinicians.
In summary, therefore, research strongly suggests that the large majority of neurological pathologies causing cerebral palsy occur as a result of multifactorial and mostly unpreventable reasons during either fetal development or the neonatal period. This, however, should not be an excuse for careless intrapartum care and every effort should still be made to identify and act upon identifiable causes of potential cerebral injury.