Molluscum contagiosum

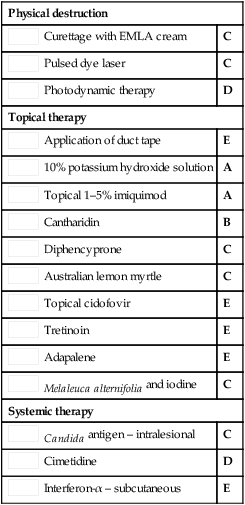
Second-line therapies
Third-line therapies
Curettage of molluscum contagiosum in children: analgesia by topical application of a lidocaine/prilocaine cream (EMLA).
Rosdahl L, Edmar B, Gisslen H, Nordin P, Lillieborgs S. Acta Derm Venereol 1988; 68: 149–53.
EMLA cream provided effective local anesthesia for the curettage of MC in 55 children.


 Await spontaneous resolution
Await spontaneous resolution Manual extrusion with gloved fingers or fine forceps
Manual extrusion with gloved fingers or fine forceps Topical 5% acidified nitrite co-applied with 5% salicylic acid
Topical 5% acidified nitrite co-applied with 5% salicylic acid Topical salicylic acid gel 12%
Topical salicylic acid gel 12% Topical 10% povidone-iodine and 50% salicylic acid
Topical 10% povidone-iodine and 50% salicylic acid Topical 40% silver nitrate paste
Topical 40% silver nitrate paste Topical 0.5% podophyllotoxin
Topical 0.5% podophyllotoxin Cryotherapy
Cryotherapy Curettage with EMLA cream
Curettage with EMLA cream Pulsed dye laser
Pulsed dye laser Photodynamic therapy
Photodynamic therapy Application of duct tape
Application of duct tape 10% potassium hydroxide solution
10% potassium hydroxide solution Topical 1–5% imiquimod
Topical 1–5% imiquimod Cantharidin
Cantharidin Diphencyprone
Diphencyprone Australian lemon myrtle
Australian lemon myrtle Topical cidofovir
Topical cidofovir Tretinoin
Tretinoin Adapalene
Adapalene Melaleuca alternifolia and iodine
Melaleuca alternifolia and iodine Candida antigen – intralesional
Candida antigen – intralesional Cimetidine
Cimetidine Interferon-α – subcutaneous
Interferon-α – subcutaneous