Methicillin-resistant Staphylococcus aureus (MRSA)

Specific investigations
First-line therapy
Second-line therapy
A comparison of costs and hospital length of stay associated with intravenous/oral linezolid or intravenous vancomycin treatment of complicated skin and soft-tissue infections caused by suspected or confirmed methicillin-resistant Staphylococcus aureus in elderly US patients.
McCollum M, Sorensen SV, Liu LZ. Clin Ther 2007; 29: 469–77.
At least for hospitalized patients, linezolid therapy may be less expensive than vancomycin.
Multicenter evaluation of the in vitro activity of dalbavancin tested against staphylococci and streptococci in 5 European countries: results from the DECIDE Surveillance Program (2007).
Biedenbach DJ, Jones RN. Diagn Microbiol Infect Dis 2009; 64: 177–84.
Dalbavancin remains a viable second-line option for skin infections, including those caused by MRSA.
Clinical experience with daptomycin in Italy: results from a registry study of the treatment of Gram-positive infections between 2006 and 2009.
Utili R, Cogo A, Cristini F, Prisco V, Sagnelli E, Tascini, et al. J Chemother 2012; 24: 113–21.
Daptomycin continues to represent a viable second-line option for treatment of MRSA infections.

 Surgical drainage alone
Surgical drainage alone Surgical drainage plus
Surgical drainage plus Mupirocin
Mupirocin Tea tree oil
Tea tree oil Bleach baths
Bleach baths Chlorhexidine
Chlorhexidine Triclosan
Triclosan Tea tree oil soap
Tea tree oil soap Undecylenamidopropyltrimonium methosulphate/phenoxyethanol
Undecylenamidopropyltrimonium methosulphate/phenoxyethanol Octenidine dihydrochloride
Octenidine dihydrochloride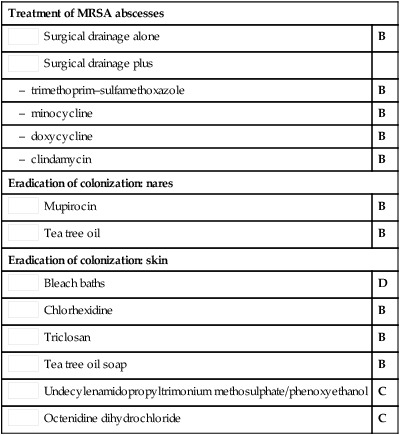
 Vancomycin ± rifampin
Vancomycin ± rifampin Linezolid
Linezolid Dalbavancin
Dalbavancin Telavancin
Telavancin Daptomycin
Daptomycin Retapamulin
Retapamulin Triple antibiotic ointment
Triple antibiotic ointment Silver sulfadiazine cream
Silver sulfadiazine cream Benzoyl peroxide soap
Benzoyl peroxide soap Zinc pyrithione soap
Zinc pyrithione soap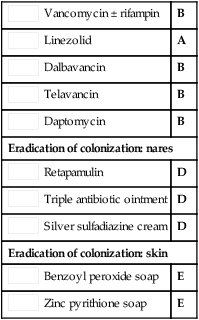
 Tigecycline
Tigecycline Ceptobiprole, ceftaroline
Ceptobiprole, ceftaroline Oritavancin
Oritavancin Honey
Honey Confectioner’s sugar
Confectioner’s sugar Sugar and povidone iodine
Sugar and povidone iodine Botanical extracts
Botanical extracts