Medical emergencies
Medical emergencies occurring in the radiology department may be due to:
Patients may develop cardiac arrhythmias, hypotension, inadequate ventilation or adverse drug/radiographic contrast reactions. Complications arise from sedative drug administration, invasive procedures and human error; poor monitoring and organizational failings may contribute.
The basic principles are summarized in the ABC of resuscitating the acutely ill patient:
1. Airway – ensuring a patent airway
2. Breathing – providing supplemental oxygen and adequate ventilation
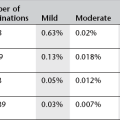
These early interventions should proceed in parallel with diagnosis and definitive treatment of the underlying cause. If cardiac arrest is suspected, the adult advanced life support algorithm in Figure 19.1 should be followed.
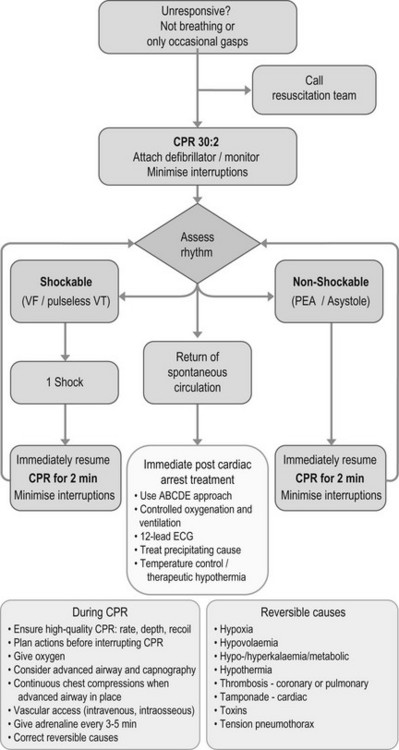
Figure 19.1 Adult advanced life support algorithm. Reproduced with the kind permission of the Resuscitation Council (UK).
Equipment
2. A positive pressure breathing device (Ambu bag) and mask
3. Supplemental oxygen and oxygen delivery devices
5. An intubation tray with airways, laryngoscopes and endotracheal tubes
6. Intravenous (i.v.) cannulas and i.v. fluids
(a) Sedative reversal drugs including naloxone and flumazenil
(b) Resuscitation drugs including adrenaline (epinephrine), atropine and hydrocortisone
9. Non-invasive blood pressure device and appropriately sized brachial cuffs
Respiratory emergencies
Respiratory depression
1. Decreased, shallow, laboured breathing
2. Decreased oxygen saturations
3. In partial airway obstruction; snoring and paradoxical chest wall movement.
The patient should immediately be placed in the supine position. If the airway is compromised it can be maintained by opening the mouth, tilting and extending the head, and lifting the chin. Supplemental oxygen must be provided. If respiratory depression is due to sedative drugs then reversal agents should be considered.
Bronchospasm
Treatment includes high-flow oxygen, nebulized salbutamol 2.5–5 mg, nebulized ipratropium bromide 0.25–0.5 mg and i.v. hydrocortisone 100–200 mg.
Aspiration
The patient should be placed on their side in the head-down position, high-flow oxygen should be administered, airway adjuncts should be removed and the airway suctioned.
Pneumothorax
This is likely to be related to a procedure such as lung biopsy (see also Chapter 7). Presentation is with unilateral pleuritic chest pain and dyspnoea:
1. For asymptomatic small pneumothorax the patient should be observed.
2. For symptomatic small pneumothorax simple aspiration should be performed and the patient subsequently observed.
3. If the pneumothorax is >2 cm in depth (which is equivalent to 49% of the volume of the hemithorax) an intercostal chest drain should be inserted.
4. If the dyspnoea increases rapidly and the patient becomes cyanosed, tension pneumothorax should be suspected and air should be aspirated immediately by insertion of a 16G cannula through the second intercostal space in the mid-clavicular line.
Cardiovascular emergencies
Hypotension
The treatment depends on cause; pressure should be applied to any developing haematoma, the patient placed in the Trendelenburg position and oxygen administered. In the case of haemorrhage or haematoma, normalization of blood pressure is not the initial priority until bleeding is controlled. Hypotension is treated at first by the administration of an i.v. fluid bolus such as Hartmann’s solution 10 ml kg–1 and the patient immediately re-assessed.
Tachycardia
Heart rates of up to 160 beats min–1 are generally well tolerated, but tachycardia-induced hypotension or myocardial ischaemia require urgent treatment.
Bradycardia
1. If the patient is non-symptomatic, monitor closely.
2. If hypotension or bradycardia <40 beats min–1 is present an anticholinergic drug such as atropine 0.3–0.6 mg may be given i.v.
3. If the patient develops asystole, pulseless electric activity or ventricular fibrillation then confirm diagnosis – unconscious, apnoeic, absent carotid pulse. Call for help, defibrillator and cardiac arrest team, and follow the advanced life support algorithm outlined in Figure 19.1.
Adverse drug reactions
Contrast media reaction
This is also discussed in detail in Chapter 2. Suggested management is as follows:
1. Nausea/vomiting – patient reassurance. Retain i.v. access and observe
2. Urticaria – retain i.v. access and observe. If troublesome give an antihistamine by slow i.v. injection, e.g. chlorphenamine maleate 10–20 mg. If severe urticaria add i.v. hydrocortisone 100 mg
3. Hypotension with bradycardia (vasovagal reaction)
5. Anaphylaxis – rare, most often mild, but may be life-threatening. Iodinated i.v. contrast media are the commonest cause of anaphylaxis in the radiology department; however, other possible causes include gadolinium agents, opioid drugs, antibiotics, aspirin, latex and local anaesthetics. Anaphylaxis is a hypersensitivity reaction which causes a range of symptoms and signs including: oedema of face and airway, wheeze, cyanosis, tachycardia, hypotension, erythema and urticaria. Anaphylaxis is likely when all of the following three criteria are met:
(a) Sudden onset and rapid progression of symptoms
(b) Life-threatening Airway ± Breathing ± Circulation problems
(c) Skin or mucosal changes (flushing, urticaria, angio-oedema)
The recommended management plan for anaphylaxis is the UK Resuscitation Council algorithm in Figure 19.2
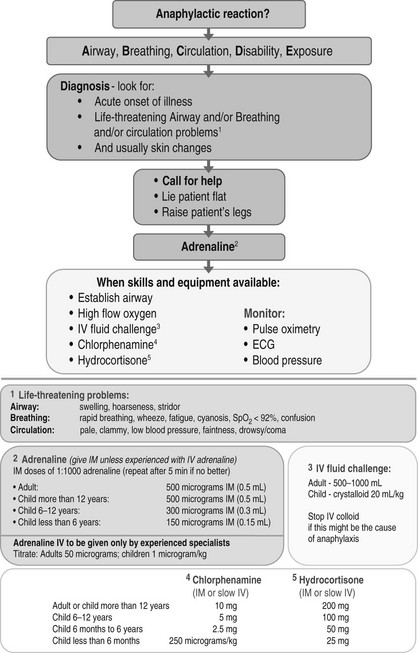
Figure 19.2 Anaphylaxis algorithm. Reproduced with the kind permission of the Resuscitation Council (UK).
6. Unconscious/unresponsive/pulseless/collapse – see Figure 19.1.
Local anaesthetic toxicity
1. Early signs of toxicity are tingling around mouth and tongue, light-headedness, agitation and tremor.
2. More severe reactions include sudden loss of consciousness, with or without tonic-clonic convulsions and cardiovascular collapse.
The immediate management includes stopping injection, calling for help, maintaining airway (including securing the airway with intubation if required), 100% oxygen, ensuring adequate i.v. access, ventilator and cardiovascular support, and control of seizures. In the event of a cardiac arrest, resuscitation should be prolonged.