17 Medical Acupuncture
Brief History
Acupuncture is a complex therapeutic process that has its roots in prehistory and is undergoing constant evolution as its use in the conventional modern healthcare setting expands and understanding of its mechanism grows. Now, having existed for almost forty years in the public consciousness of the general population of the United States and scientific community, there is considerable familiarity with the basics of acupuncture as a therapeutic modality. Most are aware that acupuncture is the use of thin, solid needles in various patterns on the body. Although this is taken for granted in 21st century America, prior to July 26, 1971, outside of Asian communities, acupuncture was a wholly unknown entity in the United States. On that date, James Reston’s landmark article describing his experience with acupuncture in China was published in The New York Times.1 Mr. Reston was a reporter for the “Times” who had traveled to China in 1971 in preparation for Richard Nixon’s historic diplomatic visit. Mr. Reston required an emergency appendectomy in Peking and had his postappendectomy pain successfully treated with acupuncture. This experience was recounted to the American people in The New York Times publication and served as the first major exposure of the English speaking U.S. population to acupuncture. Shortly after Nixon’s trip, physicians began formal and informal trips to China where they witnessed surgical anesthesia using only acupuncture needles. Whereas Reston’s article ignited popular interest in acupuncture, these reports began to fuel curiosity in the medical and scientific communities and served to spark scientific exploration of the bizarre “new” technique. As the specifics of the endorphin theory of acupuncture analgesia were discovered in the late 1970s, respect within the scientific community grew proportionately.
Economic necessity and political expediency led to the simplification and systemization of the variegated forms of classical acupuncture under Mao in the second half of the 20th century in China. After Mao came to power, it became clear that the cadre of newly trained Western physicians, numbering roughly 40,000, was grossly inadequate to care for the more than 500 million Chinese citizens. Mao’s declaration that “Chinese medicine is a great treasure-house” came in 1958 and served as the theoretical basis for the barefoot doctor movement that was initiated in 1969. During this period, Mao called on previously marginalized practitioners of acupuncture and classical Chinese medicine to create a simplified system of Chinese medicine that could be easily taught and disseminated among his corps of barefoot doctors whose aim would be to care for rural villages. This new system eventually became known as Traditional Chinese Medicine (TCM). Ironically, this system is a 20th century creation and omits many of the complexities and nuances of pre-Mao classical Chinese medicine.2–6 Interestingly, the pre-Mao classical forms of acupuncture find their most authentic preservation outside of China, in Europe, Japan, and America.
Primitive experimentation with acupuncture began in Europe during the early 19th century as translations of the Da Cheng reached England, France, and Germany via military and missionary physicians returning from China. More serious integration with modern Western medicine did not occur until the middle of the 20th century in Europe and later in the United States.2
A Brief Primer of Acupuncture Techniques
Auricular acupuncture is a microsystem technique that involves the insertion of various types of needles into predetermined points and points with altered bioelectrical conductance on the external ear. As a microsystem, all aspects of the body are postulated to have representation on the external ear in a holographic fashion. Chinese scalp acupuncture (see Chapter 19) is also a microsystem technique and is characterized by the threading of needles along the scalp according to the underlying functional characteristics of the brain.
Medical Acupuncture is the Unification of Classical Acupuncture and Modern Medicine
Medical acupuncture is the practice of acupuncture by physicians; as a discipline it represents the integration of classical acupuncture with modern medicine. Medical acupuncture has evolved since the middle of the 19th century initially in Western Europe, then in Japan, and most recently in the United States. It has found its most refined expression in the work of Joseph Helms, MD. Helms has developed a robust and elegant integration of classical acupuncture with diverse modern acupuncture techniques such as neuroanatomic acupuncture, PNT, auricular acupuncture, and scalp acupuncture. It is this integrated system of acupuncture that is referred to by the term medical acupuncture in this chapter.
What are the Effects of Medical Acupuncture?
As a comprehensive therapeutic system with a variety of techniques, medical acupuncture has wide-ranging effects including pain reduction, improvement in sleep, improvement in anxiety and depression, a reduction in pain medication, improvement in function, and an improvement in energy and vitality.7–13 Conversely, most therapies in conventional medicine have narrowly defined effects such as pain reduction from an epidural steroid injection or improved sleep from a sedative-hypnotic drug. Acupuncture that is used to treat a pain problem can be expected to have multiple effects simultaneously. This is particularly important because many pain problems represent a vicious cycle of pain, dysfunction, psychoemotional disturbances, fatigue, and sleep problems. Part of the robust nature of medical acupuncture is the ability to affect all of these seemingly disparate problems.
Medical Acupuncture View of the Human Organism
The accumulation of knowledge about human physiology, biochemistry, and pathophysiology within the sphere of modern medicine has been prodigious in the last 50 years. Much of this progress has relied on the ever improving ability to focus on the ever more exact building blocks of the human body. Much of medical therapeutics derives from this scientific process, but also remains incompletely understood. For example, tricyclic antidepressants are effective in treating many chronic pain states and are widely used for this purpose. We know that these medications have many mechanisms of action including the inhibition of presynaptic reuptake of serotonin and norepinephrine as well as blockade of sodium and voltage-dependent calcium channels.14 We do not know, however, the mechanism of action responsible for analgesia,15 nor do we know why some patients respond and others do not. Powerful reductionistic science has identified the mechanisms of these medications and part of the pathophysiology of chronic pain, but will unlikely reveal the unanswered questions of in vivo analgesic mechanisms and individual variability of response. Modern scientific paradigms from modern physics such as systems theory and quantum mechanics will likely be required to propel modern medicine into the next stages of advancement. Scientific approaches to reality require both reductionistic and synthetic processes of investigation. Systems theory is an excellent example of a synthetic scientific approach.
Systems theory teaches us that complex systems as primitive as unicellular organisms behave in ways that defy reductionistic, linear laws. Whereas reductionistic models of scientific investigation have proved invaluable for determining many of the components of living systems, this approach to science is suboptimal in providing information about how these components interact in the living organism.16 Systems theory instructs that complex systems, of which the human body is a quintessential example, have emergent properties. Emergent properties are unique properties of complex systems that are not present in any of the more simple parts of the whole, but arise only when all parts interact to form the complex whole. A laudable yet nascent drive in modern medicine is the administration of individualized care. The doctrine of conventional modern medicine is that the specific disease entity must be identified and the pharmaceutical or intervention that is most appropriate to the disease entity must be delivered. That is, all patients with knee osteoarthritis ought to receive the same treatment, all patients with insomnia ought to receive the same treatment, all patients with depression ought to receive the same treatment, and any patient with all three diseases ought to receive all three treatments.
Systems theory teaches us that this is a rudimentary approach to the complex system of the human body. First, not all humans with the same disease process will respond the same way to the same treatment. We know that there are individual differences in the pharmacokinetics of medication metabolism and individual differences in the healing process after surgery.17–19 Thus, the best principles of modern science tell us what Dr. Osler told us more than 100 years ago—“It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.” The goal, then, is individualized approaches that take the complexity of the person’s constitution as well as the disease process into account. The specific science and ability to do this in clinical practice is developing, but still poorly defined.
Interestingly, medical acupuncture presents clinicians with an approach that follows these ideals. Part of the nonspecific effects that are attributed to acupuncture’s effectiveness in RCTs may in fact be due to the systematic approach of acupuncture that seeks to identify constitutional factors for a patient and individual treatment for a presenting complaint based on that person’s identity and constitution. The classical framework of acupuncture has developed an empirical system that, in essence, looks for emergent properties. Through the thousands of years of empirical observations and subsequent pattern definition, acupuncture has sought to answer the following types of questions: What unique characteristics arise when a person complaining of knee pain also is a competitive, hard driving, leader without other medical problems, versus an overweight, jovial man who also suffers from chronic, debilitating allergic rhinitis? While the conventional approach to treating knee pain in these two patients would be identical, with likely variable results, the acupuncture approach for each would be unique, likely with good results based on large RCTs.20,21
Medical Acupuncture and the Treatment of Complex Chronic Pain
Medical acupuncture is a versatile modality that interacts with psychological, neurologic, endocrine, immunologic, and musculoskeletal aspects of the human organism.22–27 With these multiple points of input, medical acupuncture is ideally suited for the treatment of pain, which by nature manifests in the psychoneuromusculoskeletal sphere of humans.
The Neuromatrix Theory of Pain
“The neuromatrix theory of pain proposes that pain is a multidimensional experience produced by characteristic “neurosignature” patterns of nerve impulses generated by a widely distributed neural network—the “body-self neuromatrix”—in the brain. These neurosignature patterns may be triggered by sensory inputs, but they may also be generated independently of them. Acute pains evoked by brief noxious inputs have been meticulously investigated by neuroscientists, and their sensory transmission mechanisms are generally well understood. In contrast, chronic pain syndromes, which are often characterized by severe pain associated with little or no discernible injury or pathology, remain a mystery. Furthermore, chronic psychological or physical stress is often associated with chronic pain, but the relationship is poorly understood. The neuromatrix theory of pain provides a new conceptual framework to examine these problems. It proposes that the output patterns of the body-self neuromatrix activate perceptual, homeostatic, and behavioral programs after injury, pathology, or chronic stress. Pain, then, is produced by the output of a widely distributed neural network in the brain rather than directly by sensory input evoked by injury, inflammation, or other pathology. The neuromatrix, which is genetically determined and modified by sensory experience, is the primary mechanism that generates the neural pattern that produces pain. Its output pattern is determined by multiple influences, of which the somatic sensory input is only a part, that converge on the neuromatrix.”28
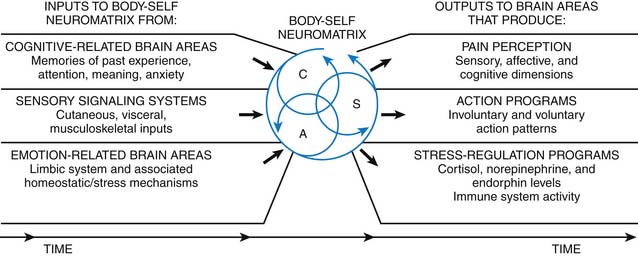
Figure 17-1 illustrates the sensory inputs that influence the genetically determined neuromatrix: cognitive, sensory, and emotional. Medical acupuncture targets all of these inputs, the neuromatrix itself, and also the output programs that are often dysfunctional. Classical acupuncture often focuses on psychoemotional disturbances, whereas modern neuroanatomic acupuncture aims at treating musculoskeletal sources of dysfunctional inputs to the neuromatrix as well as spinal cord regions involved in spinal modulation. Scalp and auricular acupuncture are directed at affecting the neuromatrix itself. Acupuncture has also been shown to influence the stress regulation output program of the neuromatrix.22,29 While Melzack emphasizes the genetic contribution to the neuromatrix, classical acupuncture always strives to understand and treat the constitution of an individual, which can be understood as the genetically determined phenotype of an individual.
The medical acupuncture approach to pain not only recognizes the value of treating all three groups of inputs to the neuromatrix (see Fig 17-1), but also focuses on an expanded set of tissues in the periphery capable of stimulating the neuromatrix. As such, medical acupuncture not only evaluates and treats dysfunctional joints, nerves, and tendons, but also muscle, ligaments, and fascia. Furthermore, medical acupuncture directs therapy at the neuromatrix itself and the stress response output program of the neuromatrix.
Mechanisms
Twentieth Century Mechanisms
Since its introduction to the American scientific community in the 1970s, acupuncture has often been perceived as a therapeutic modality whose mechanism is mysterious and unknown at best, and inert in terms of modern physiology at worst. Researchers who sought to prove the latter hypothesis as well as those who were curious about discovering possible physiologic mechanisms produced a prolific body of basic science data in the 1970s and 1980s. This research led to the endorphin and monoamine hypothesis of acupuncture analgesia which has since been supported by an enormous collection of animal and human studies. Bruce Pomeranz, PhD, was one of the most prominent researchers in this area. He, indeed, set out to prove that acupuncture had no measurable physiologic effects. After publishing 66 papers investigating the mechanism of acupuncture analgesia, his conclusion was that the evidence supporting the endorphin hypothesis for acupuncture analgesia was stronger than that for almost any other therapeutic agent used in conventional medicine (Fig. 17-2).
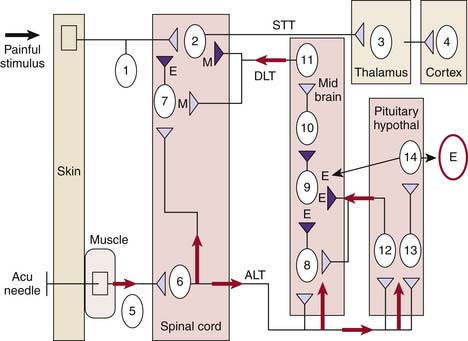
Figure 17-2 Model developed from research by Dr. Pomeranz.
(Adapted from Stux G, Pomeranz B (eds): Basics of Acupuncture: Berlin, 2005, Springer p27.
An acupuncture needle entering the skin and muscle in the arms or legs will activate unmyelinated C-fibers and small diameter myelinated A-delta fibers in the periphery that synapse onto cells of the anterolateral tract in the dorsal horn of the spinal cord. These cells give rise to two sets of projections. One set travels rostrally to eventually synapse on the midbrain, pituitary, and hypothalamus. The other set synapses on inhibitory interneurons in the spinal cord where dynorphin and enkephalin are released presynaptically to block ascending neurotransmission of painful signals along the spinothalamic tract. Meanwhile, the rostrally projecting cells of the anterolateral tract will stimulate cells in the periaqueductal gray causing the release of enkephalin, which will disinhibit cells of the raphe nucleus. The raphe nucleus is part of an endogenous descending analgesic pathway. Disinhibition of these cells activates this descending analgesic pathway, which causes the release of monoamines such as serotonin onto cells of the spinothalamic tract in the spinal cord that carry painful stimuli to the brain. Serotonin postsynaptically inhibits these cells, thereby dampening down the neurotransmission of painful signals from the periphery to the brain along the spinothalamic tract. Thus, the original acupuncture stimulus activates multiple neurochemical pathways in the brain and spinal cord and decreases the neuronal transmission of painful stimuli from the periphery to the brain.30 The ascending anterolateral tract neurons also stimulate the pituitary to release ACTH and β-endorphin into the bloodstream.30
Twenty-First Century Mechanisms
Whereas 20th century research of the mechanism of acupuncture paralleled the discovery of the endorphin receptors and the gate control theory of pain, 21st century research is focusing on the brain, neuroimmunology, and connective tissue.
How Does Acupuncture Interact with Fascia and Loose Connective Tissue?
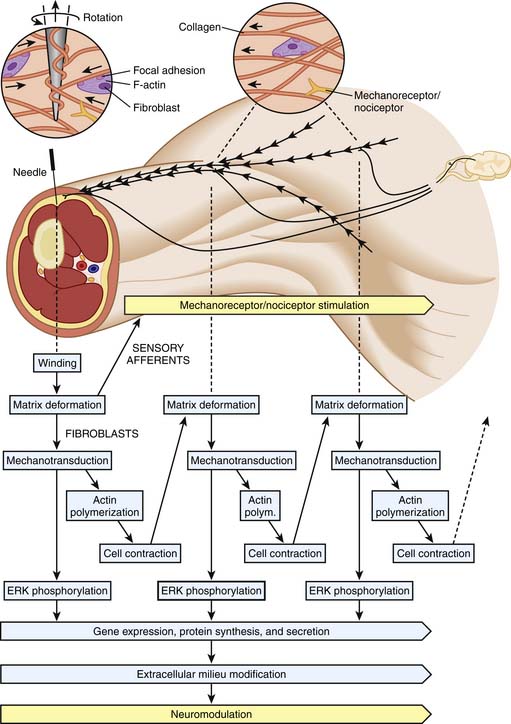
The research of Langevin and colleagues has demonstrated that the twirling of the acupuncture needle that is typical in clinical practice creates mechanical changes in the collagen and fibroblast network of the extracellular matrix. In fact, her work using histologic sections and specialized ultrasonography has shown that the manipulation of the acupuncture needle produces characteristic changes in the surrounding loose connective tissue such as the wrapping of collagen fibers. She has demonstrated that these mechanical changes in the connective tissue are accompanied by active cellular changes such as lamellapodia formation and fibroblast spreading. Although not yet conclusive, this research supports the hypothesis that acupuncture needling activates diverse biological processes such as gene transcription, protein synthesis, and neuromodulation through the mechanism of mechanotransduction (Fig. 17-3). These biochemical phenomena may underlie many of the unknown mechanisms of the therapeutic effects of acupuncture.31–34
Biochemical Milieu of Trigger Points
Although the subject is not as novel as the work of Langevin and colleagues, the research of Jay Shah, MD is equally fascinating and instructive. Clinicians have long relied on the pioneering work of Janet Travell, MD in treating myofascial pain. Trigger point needling with and without local anesthetic is used by medical acupuncturists to treat many types of myofascial pain. However, until recently, convincing basic science research characterizing the qualities of trigger points has been lacking. In the January 2008 publication of The Archives of Physical Medicine and Rehabilitation, Dr. Shah describes an innovative technology that allows the real time biochemical assay of the trigger point milieu. A 30-gauge microdialysis needle is used to noninvasively sample 11 histochemicals in clinically identified trigger points. This study confirms that biochemicals associated with pain and inflammation (protons, substance P, TNF-α, bradykinin, and many others) are present in higher concentration in active trigger points than in latent trigger points and control muscle points. Furthermore, after needling the trigger points, concentrations of substance P, and CGRP are shown to decline. Though requiring additional study, this work offers a convincing basic science explication for the mechanisms underlying the dry needling of trigger points that is an integral part of medical acupuncture.35,36
Acupuncture Effects on the Brain
Nonpainful stimulation of peripheral nerves using transcutaneous electrical stimulation causes an increase in activation of the somatosensory, motor, premotor, posterior parietal, and cingulate cortices, as well as the thalamus and cerebellum as measured by fMRI.37,38 Painful stimuli produce activation in multiple regions of the brain including the primary and secondary somatosensory cortices, the insular cortex, the anterior cingulate cortex, the thalamus, and the prefrontal cortex.39
Reproducible data show that acupuncture modulates an extensive network of cortical, subcortical, and brainstem regions in the brain.40 Numerous fMRI studies have demonstrated that acupuncture elicits a response in multiple cortical regions including the primary and secondary somatosensory cortices, the insular cortex, and the prefrontal cortex when compared to a variety of needle and nonneedle controls.40 A robust limbic network, including the hippocampus, amygdala, hypothalamus, and anterior cingulate cortex is also modulated.41 Brainstem structures involved in endogenous descending analgesia such as the periaqueductal gray are recruited by acupuncture therapy.42 Whereas nonacupuncture transcutaneous stimulation of peripheral nerves and painful peripheral stimuli generally produce an increase in signaling in the brain’s pain matrix, acupuncture therapy produces a modulation or a decrease in signaling intensity in the same regions of the brain.22
Interestingly, acupuncture stimulates widespread deactivation of brain regions involved in the affective and cognitive aspects of pain, and also is able to influence the brain structures that control the physiologic stress response. The amygdala translates somatosensory stimuli into affective states. The amygdala exhibits patterns of sensitization and hyperactivation in response to chronic pain states.43 Acupuncture therapy elicits deactivation of the amygdala in healthy controls and in patients with chronic pain. Additional limbic structures involved in consolidation of somatosensory memory and the interface of cognitive and emotional mentation are also affected by acupuncture.22,29 The hypothalamus receives and integrates diverse information about the internal and external environment and produces a coordinated output program. A major aspect of hypothalamic output is orchestration of the body’s response to physiologic and psychological stress through the hypothalamic-pituitary-adrenal axis. The classical descriptions of acupuncture encouraging a return to homeostasis in the body are interesting in light of recent fMRI research demonstrating modulation of the hypothalamus in pain states.22,29,41
Napadow and colleagues have also explored the effects of acupuncture on the dysfunctional neuroplasticity that develops in chronic pain patients. This dysfunctional central neuroplasticity may be part of the basis for their persistent pain, and its correction may underlie some of the therapeutic effects of acupuncture in chronic pain states.29,44,45
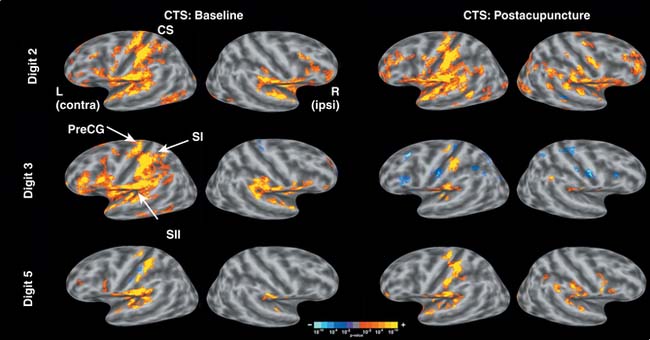
A fascinating set of studies by this group has evaluated the brain effects of acupuncture on carpal tunnel syndrome (CTS) patients versus healthy controls. For the patients with CTS, the region of the sensorimotor cortex subserving the first three digits of the affected hand demonstrated hyperexcitability to nonnoxious stimuli when compared to healthy controls. After 13 acupuncture treatments performed over 5 weeks, the dysfunctional cortical hyperexcitability seen in the carpal tunnel patients diminished significantly. Healthy controls did not exhibit a similar rearrangement in cortical activity. These studies are an excellent example of the beneficial neuroplasticity that can be induced by acupuncture therapy.22,44,45
Figure 17-4 illustrates group-averaged difference mapping of the contralateral sensorimotor cortex for CTS patients before and after acupuncture. Hyperactivity to nonnoxious stimuli in the contralateral sensorimotor cortex was exhibited in the median nerve innervated third digit at baseline. This hyperactivity in the third digit diminished after acupuncture treatment.
Activation of Neuronal Networks
Central nervous system disorders such as Parkinson disease, chronic pain, and depression are thought to involve the disruption of key neuronal networks. Faingold hypothesizes that electrical stimulation therapies such as deep brain stimulation, vagus nerve stimulation, electroconvulsive therapy, and acupuncture exert their therapeutic effects by recruiting dormant neuronal networks that compete with and override the pathologic networks mediating disease. It is suggested that the overall manifestation of symptoms by the individual is determined by which neuronal network (pathologic or therapeutic) prevails and achieves control of the affected brain function. Thus, Faingold postulates that the mechanism of electrical stimulation therapies such as acupuncture involves the stimulation of potentially therapeutic dormant neuronal networks that subsequently manifest as elimination or diminution in symptoms.46
Does Needling of Acupuncture Points Produce Different Brain Activation Patterns than Needling of Nonclassically Defined Body Locations?
Why is this an interesting question? On the one hand, practitioners of classical acupuncture are eager to demonstrate that the needling of classically defined acupuncture points produces significantly different effects from the needling of nonclassically defined locations. On the other hand, several large and well done clinical studies of acupuncture have yielded similar clinical benefits for patients treated with classical acupuncture and minimal acupuncture, which is variably defined as superficial needling at classical acupuncture points and needling at nonclassical locations, when compared to patients receiving standard conventional treatments.47–49
Data from fMRI Studies
Wu and colleagues observed that electroacupuncture at a nonacupuncture point (sham acupuncture) produced some of the same cortical changes as electroacupuncture at a classical acupuncture point (real acupuncture). Both sham and real acupuncture produced similar effects in the caudal segment of the anterior cingulate cortex, insula, secondary somatosensory cortex, thalamus, and cerebellum. However, real acupuncture produced additional effects in the limbic system not observed with sham acupuncture. Specifically, difference mapping demonstrated activation of the hypothalamus and deactivation of the anterior cingulate cortex with real acupuncture versus sham acupuncture.50
Optimal Acupuncture Therapy for Pain
Neuromusculoskeletal Diagnosis
One important aspect of systems of classification, such as medical diagnosis, is identifying clinical entities that are likely to respond to particular treatments. With this in mind, the physician acupuncturist explores the NMS matrix of the pain patient for clinical syndromes that respond to NMS acupuncture inputs. For example, the physician acupuncturist does not rely solely on pathodiagnostic classifications such as herniated lumbar disc or lateral epicondylitis. Rather, these diagnoses are used as starting points and additional contributing factors are sought. Commonly, muscular trigger points and tightness of the superficial fascia will complicate and exacerbate pain considered to be neuropathic in origin. Similarly, abnormal regional and spinal segmental neuronal processing will often accompany muscular, ligamentous, and tendinopathic pain. Recognizing these interrelated dysfunctions of pain problems is particularly important and germane because acupuncture is well suited to address muscular, fascial, neuronal, tendinous, ligamentous, and visceral dysfunctions.24,31,35,52
Pain is a Mind Body Problem and Medical Acupuncture is a Mind Body Treatment
Pain is a unique medical problem that cuts across virtually all areas of medicine. At its core it epitomizes all of the subtleties and complexities of mind-body holism. It is now clear that any model seeking to explain the experience and pathogenesis of pain is incomplete if it omits the impact of our thoughts and feelings, actions, social relationships, or biomedical makeup. The arena of pain medicine matches these multifaceted aspects of pain with the multidisciplinary pain clinic that houses—under one roof—biomedical pain specialists emphasizing interventional and pharmaceutical approaches, psychologists addressing the psychoemotional component of pain, physical therapists with expertise in reconditioning and manual techniques, and a hodge-podge of complementary techniques primarily based on market demand. Unfortunately, the economic situation of modern medicine in the United States at the beginning of the 21st century fosters fragmented, intervention-based medical care even within multidisciplinary pain clinics. In fact, economic necessity is now the organizing principle of many multidisciplinary pain clinics compared to the original founding goal of offering truly holistic pain medicine based on the biopsychosocial model. Although many interventional approaches have little evidence for efficacy,53–55 they are reimbursed by third party payers at high rates and therefore generate the majority of revenue at multidisciplinary pain clinics. Because of this, these invasive therapies are often used more frequently than less expensive, conservative therapies based on the biopsychosocial model of pain that are supported by stronger evidence.56
Safety
A systematic review of nine surveys of the safety of acupuncture involving more the 250,000 treatments found that feelings of faintness and syncope occurred in less than 0.3% of treatments. Feelings of relaxation were common and occurred in almost all patients (86%).57 Of the serious adverse effects, pneumothorax is one of the most common. The large Acupuncture Safety and Health Economic Studies (ASH) in Germany involved more than 1.6 million acupuncture sessions and reported two pneumothoraces for an occurrence rate per session of less than 0.0001%.58 This same research initiative reported local infection in 0.3% of patients.58
Cost Effectiveness of Acupuncture
In the largest clinical investigation of acupuncture to date, German researchers evaluated the cost effectiveness of acupuncture for the treatment of headache, chronic neck pain, low back pain, and osteoarthritis of the knee and hip in the Acupuncture in Routine Care Studies (ARC).47 ARC included nearly 8500 patients for economic analysis and found acupuncture to be effective for all diagnoses studied with an average increase in expenditure of 319 euros per treatment course.47,58 The cost effectiveness was found to be between 10,526 euros per QALY for low back pain and 17,854 euros per QALY for knee and hip osteoarthritis. Thus, acupuncture for all diagnoses was found to be well within accepted standards for cost effectiveness.
British researchers evaluated the cost effectiveness of acupuncture for the treatment of chronic headache and found that acupuncture improved quality of life for a relatively small incremental cost. They estimated that acupuncture treatment resulted in a cost of 9180 pounds per QALY which compares favorably to medication treatment of migraine headaches. Substituting oral sumatriptan for oral caffeine plus ergotamine results in a cost of 16,000 pounds per QALY.59,60 Other studies have found acupuncture to be cost effective for chronic neck pain with a cost of 12,469 euros per QALY61 and low back pain with a cost of 4241 pounds per QALY.62
Clinical Research
Challenges of Studying Acupuncture
Since the 1950s the randomized, double blind, placebo controlled trial (RDBPCT) has become the standard methodology for evaluating the effectiveness of pharmaceutical therapies. Although going to great lengths to exclude bias, this methodology also has its limitations. Perhaps the most vexing problem of the RDBPCT is the discordance between what is studied (homogeneous patients without comorbid conditions) and real life (complex patients with multiple medical problems).63–65 Furthermore, the RDBPCT may not be the best method to evaluate complex medical interventions such as surgery, physical therapy, psychotherapy, and acupuncture. In contrast to pharmaceutical therapy, the substance of these interventions cannot be divorced from the mode of delivery. Because of this, controls that allow clear isolation of the “specific” effects of the intervention from the “nonspecific” effects of the delivery mode are virtually impossible to devise. For example, it is impossible to magically remove a gallbladder without going through the lengthy and ritualized preoperative intake, intraoperative anesthesia, and postoperative recovery process.
In the case of acupuncture, we know that sham acupuncture is a myth. Sham acupuncture or minimal acupuncture is generally defined as the insertion of needles at so called “nonacupuncture” points or at shallow depths over classically defined acupuncture points, and is considered to be physiologically and clinically inert. Sham needling at “nonacupuncture” locations is problematic for several reasons. From classical as well as modern reasoning, it is virtually impossible to find a location on the body that will not produce a physiologic action in response to acupuncture needling. There are roughly 360 body locations called “meridian points” that are avoided to find “nonacupuncture” points. Interestingly, there are several thousand “extra-meridian” acupuncture points and a multitude of points that are located based on the specific manifestation of symptoms of each person, making the selection of “nonacupuncture” points challenging at best from the classical perspective. Likewise, modern fMRI research has demonstrated that while needle stimulation at acupuncture points produces more robust brain modulation than needle stimulation at “nonacupuncture” points, nonacupuncture points are physiologically active.50
A more useful methodology for studying complex interventions such as acupuncture may be the pragmatic randomized controlled trial (PRCT).66 The PRCT evaluates actual questions facing the practicing clinician. For example, in a patient with refractory depression managed by the primary care physician, does referral for collaboration with a psychiatrist result in improved patient outcomes?67 Or will a patient with chronic low back pain receiving conventional management from the primary care provider derive additional incremental benefit from a referral to medical acupuncture?
Key features of the PRCT are minimizing exclusion criteria in an attempt to match the study population more closely with the heterogeneous types of patients encountered in clinical medicine as well as using pragmatically selected control groups such as a “treatment as usual group”.66 Although marked improvements have been attributed to placebo interventions such as the “sugar pill,” the actual improvement beyond treatment as usual groups may be minimal or nil. A 2004 Cochrane review of placebo interventions for all clinical conditions concluded “There was no evidence that placebo interventions in general have clinically important effects. A possible small effect on continuous patient-reported outcomes, especially pain, could not be clearly distinguished from bias,” and further “It has been widely believed that placebo treatments are associated with substantial effects on a wide range of health problems. However, this belief is not based on evidence from randomized trials that use a placebo treatment for one group of people, while another group receives no treatment. The effect of placebo treatments was studied by reviewing more than 150 such trials covering many types of health care problems. Placebo treatments caused no major health benefits, although they possibly had a small effect on outcomes reported by patients, for example, pain.”68
When evaluating the effectiveness of a therapeutic intervention, it is imperative to use control groups to account for spontaneous improvement in symptoms and the fluctuation in symptoms that is inherent to the natural course of a disease process. When the evaluated therapy is simple, such as pharmacotherapy, and the substance of the intervention can easily be separated from the process of the intervention, using a placebo pill may be useful to account for additional bias such as expectancy. However, when evaluating the relative clinical effectiveness of complex interventions such as psychotherapy, surgery, and acupuncture where the substance and process of the therapy are inextricable, use of control groups that consist of treatment as usual or an alternate therapy [acupuncture versus physical therapy or percutaneous coronary intervention (PCI) versus coronary artery bypass grafting (CABG)]69 may provide more clinically relevant information.
Spine Pain
A Cochrane review of acupuncture and dry needling for low back pain including 35 RCTs through 2003 concluded that acupuncture is effective for pain relief and functional improvement of chronic low back pain when compared to either usual treatment or sham acupuncture. Improvement was noted immediately after a course of acupuncture and for up to 3 months after the cessation of treatments. Acupuncture was also found to offer incremental benefit in pain reduction when added to standard treatments for chronic low back pain.70
Three large German RCTs published after the Cochrane review demonstrated a substantial reduction in low back pain for acupuncture relative to standard conventional treatments for periods extending to 6 and 12 months. Haake and colleagues randomized 1162 patients with back pain to acupuncture according to classical concepts, superficial acupuncture needling at nonacupuncture points, or usual care consisting of drugs, physical therapy, and exercise. The primary outcome was improvement in pain or function at 6 months. Both needling groups were almost twice as likely to improve when compared to usual conventional care. There was little difference between the two acupuncture groups suggesting that point selection may be less important than proposed by classical acupuncturists.49 Brinkhaus and coworkers found similar results in a rigorously designed RCT with improvement maintained through 12 months.71 Witt and associates included 11,630 patients in a study evaluating clinical and economic effectiveness of acupuncture for low back pain. Of 3093 patients who consented to randomization, 1549 patients were allocated to receive immediate acupuncture and 1544 patients were allocated to a waiting list control group that would receive acupuncture 3 months later. The remaining 8537 who did not agree to randomization generally had more severe baseline symptoms and were included in a nonrandomized cohort. In the randomized arm, acupuncture was found to be effective at reducing pain and function when compared to routine care with an absolute risk reduction of 25.8%, yielding a number needed to treat of four. Interestingly, the nonrandomized acupuncture cohort with more severe baseline symptoms experienced improvement in pain and function similar to the randomized group receiving acupuncture.48
Fewer studies have been conducted for neck pain, however a high-quality meta-analysis has been performed. A Cochrane review of acupuncture for neck disorders including 10 RCTs through 2006 found moderate evidence that acupuncture was more effective at relieving pain than sham treatments for both mechanical neck pain and neck pain with radicular symptoms for up to 3 months.72
Headache
In 2009, The Cochrane Collaboration published two meta-analyses evaluating the use of acupuncture for prophylaxis of migraine and tension-type headaches. Their review of acupuncture for migraine prophylaxis included 22 RCTs through April 2008. The authors concluded that “…Available studies suggest that acupuncture is at least as effective as, or possibly more effective than, prophylactic drug treatment, and has fewer adverse effects. Acupuncture should be considered a treatment option for patients willing to undergo this treatment.” They also state “…There is no evidence for an effect of ‘true’ acupuncture over sham interventions, though this is difficult to interpret, as exact point location could be of limited importance.”73
The same authors reviewed the effects of acupuncture for tension-type headache and included 11 RCTs through January 2008. They concluded that “…acupuncture could be a valuable non-pharmacological tool in patients with frequent episodic or chronic tension-type headaches…”. They report that two large RCTs compared acupuncture to usual care and found 47% of patients receiving acupuncture experienced a reduction in headache frequency by at least 50% compared to 16% of the patients in the control group. They also describe six RCTs that compared ‘true’ acupuncture to ‘fake’ acupuncture in which needles are either inserted at ‘incorrect’ points or did not penetrate the skin. The pooled analysis of these RCTs revealed a small, but statistically significant improvement of the patients receiving ‘true’ acupuncture versus ‘fake’ acupuncture. That is, 50% of patients receiving true acupuncture reported a reduction of at least 50% in headache frequency versus 41% of patients receiving ‘fake’ acupuncture.74
A 2007 German review concluded that a 6-week course of acupuncture treatments is equivalent to a 6-month course of prophylactic drug treatment. This review also suggested that traditional concepts of needle location and stimulation are not as important as had been thought, and recommended “that acupuncture should be integrated into existing migraine therapy protocols.”75
Several RCTs have also evaluated the use of acupuncture for acute migraine headache. A recent RCT published in Headache in 2009 randomized 175 patients to receive true acupuncture or one of two sham acupuncture groups who received needling at various nonacupuncture points. The true acupuncture group experienced a greater decease in pain versus the sham acupuncture groups at 2 and 4 hours after treatment. In addition, 40.7% of those receiving true acupuncture experienced a complete resolution of pain within 24 hours versus 16.7% and 16.4% in the two sham acupuncture groups.76
Melchart and colleagues randomized 179 migraine patients to receive acupuncture, subcutaneous sumatriptan, or a placebo injection at the first sign of a migraine headache. Acupuncture and sumatriptan were equally effective in preventing a full migraine attack. Acupuncture resulted in a 21% absolute risk reduction and sumatriptan resulted in a 22% absolute risk reduction when compared to the placebo injection. If a full attack could not be prevented, sumatriptan was more effective than acupuncture in reducing pain. Side effects were more common in patients who received sumatriptan (40%) than in acupuncture patients (23%) or patients who received the placebo injection (16%).77
Knee Pain
White and colleagues published a 2007 meta-analysis in the journal Rheumatology which reviewed 13 RCTs investigating the effect of acupuncture on pain and function in patients with chronic knee pain. This review concluded that acupuncture improves pain and function in patients with chronic knee pain when compared to sham acupuncture and usual care.78
A second meta-analysis published by Manheimer in the Annals of Internal Medicine in 2007 included 11 RCTs and concluded that, when compared to waiting list controls, acupuncture results in clinically relevant benefits in patients with osteoarthritis of the knee. Short term benefits were also found in trials that used sham control groups, but these were deemed to be not clinically relevant.79
Two of the largest high-quality RCTs were conducted in Germany and published in 200520 and 2006.21 Both of these trials showed incremental benefit for acupuncture in patients with knee osteoarthritis when compared to conventional treatment. The trials yielded conflicting results regarding differences between classical acupuncture and minimal acupuncture.
Shoulder Pain
Fewer large, high-quality trials are available to evaluate the effectiveness of noninvasive therapies for chronic shoulder pain. Cochrane reviews for acupuncture, physical therapy, and corticosteroid injections have concluded that insufficient evidence exists to guide therapy for these interventions.80–82 Subsequent to the publication of the Cochrane meta-analysis for acupuncture, Guerra de Hoyos and coworkers published the largest RCT to date in 2004.83 This study randomized 130 patients with chronic shoulder pain to active acupuncture or nonpenetration control acupuncture and demonstrated an improvement in pain intensity and every secondary outcome measure 3 and 6 months after treatment. A 2005 RCT published in the journal Physical Therapy evaluated the effectiveness of ultrasound or acupuncture added to exercise therapy in 85 patients with impingement syndrome. This study included follow-up data for 12 months and concluded that the addition of acupuncture to home exercises was more effective than the addition of ultrasound.84 The largest high-quality RCT was published in the journal Rheumatology in 2008 and evaluated the effect of adding a single acupuncture point to physical therapy in 425 patients with shoulder pain. The acupuncture group experienced reduced pain as well as a reduction in analgesic medication consumption in comparison to the control group which received only physical therapy.85
Elbow Pain
A 2004 meta-analysis published in the journal Rheumatology included 6 RCTs evaluating the effectiveness of acupuncture for lateral epicondylar pain. All six of the studies demonstrated that acupuncture was effective at relieving lateral epicondylar pain for up to 3 months after a course of treatments. Five of the six studies demonstrated superiority of acupuncture when compared to control treatments.86 A systematic review investigating the effectiveness of conservative therapies in the rehabilitation of lateral epicondylitis was published in the Journal of Hand Therapy in 2004 and came to similar conclusions.87
Hip Pain
Few high-quality RCTs have been conducted to evaluate the effectiveness of acupuncture for hip pain. A small RCT published in the Clinical Journal of Pain in 2004 compared electroacupuncture to patient education in patients with osteoarthritis related hip pain. Electroacupuncture was significantly more effective at reducing pain and improving functional status and quality of life when compared to patient education at all three assessment periods: immediately after a course of treatment, as well as 3 and 6 months after a course of treatment.88
A much larger high-quality study was published by Witt and colleagues in Arthritis and Rheumatism in 2006 as part of the colossal German Acupuncture trials. In this study 712 patients with hip or knee osteoarthritis (45% had hip osteoarthritis) were randomized to receive acupuncture or standard medical therapy. In addition, a nonrandomized cohort of 2921 patients with identical baseline characteristics was included in the study. In the randomized group, patients receiving acupuncture experienced a marked clinical improvement compared to patients receiving standard medical therapy. These improvements were maintained up to 6 months after treatment. Interestingly, the outcomes for the large nonrandomized group receiving acupuncture were similar to those experienced by the group randomized to receive acupuncture.89
Fibromyalgia
Evidence for the effectiveness of acupuncture for fibromyalgia is sparse and conflicting. A 2006 literature review included five RCTs, of which three demonstrated effectiveness of acupuncture versus sham treatment and two showed a lack of effectiveness. Because of the heterogeneity of the abstracted data, meta-analysis was not possible. Number of treatments did not seem to affect the likelihood of positive response. Interestingly, all of the RCTs that demonstrated effectiveness for the acupuncture group used electroacupuncture, whereas the two RCTs that failed to demonstrate effectiveness used manual stimulation only. This review concludes that acupuncture for the symptomatic treatment of fibromyalgia is not supported by unanimous results from RCTs.90
Temporomandibular Joint Pain
High-quality research investigating the efficacy of acupuncture for temporomandibular joint related pain is limited. A literature review published in 2001 evaluated 14 studies. The three RCTs that met inclusion criteria evaluated acupuncture versus occlusal splints with two studies also including usual care control groups. All three RCTs that were included found acupuncture to be effective in a variety of metrics including the visual analog scale, mandibular function, and number of tender points on examination. The degree of effectiveness, however, was not quantified.91
A small RCT published in 2006 evaluated true acupuncture versus noninsertional sham acupuncture using a single needle on the face. Multiple endpoints were recorded and found to favor true acupuncture. The group receiving true acupuncture reported a 53% reduction in pain on the visual analog scale versus a 6% reduction reported by the sham group. Likewise, the true acupuncture group reported a 55% reduction in functional impairment versus a 6% reduction reported by the sham group.92
Postoperative Pain
A systematic review of 15 RCTs evaluating acupuncture for postoperative pain was published in The British Journal of Anaesthesia in 2008. The data were analyzed for postoperative opioid consumption, postoperative pain intensity, and opioid-related side-effects. Acupuncture was found to have an opioid-sparing effect at 8 hours, 24 hours, and 72 hours corresponding to a respective 21%, 23%, and 29% reduction of morphine consumption, respectively. A moderate and statistically significant reduction in pain intensity was found at 8 and 72 hours in the acupuncture treatment groups. A statistically significant reduction in opioid-related adverse affects was also found. Treatment by acupuncture was associated with a 33% reduction in the incidence of nausea, a 35% reduction in dizziness, a 22% reduction in sedation, a 25% reduction in pruritus, and a 71% reduction in urinary retention.93
Auricular acupuncture has also been studied in the postoperative period. Usichenko and associates studied 54 patients undergoing total hip arthroplasty and compared four acupuncture press tacks in the ear at acupuncture points versus nonacupuncture points. The group that received acupuncture at acupuncture points of the ear used 31% less opioid administered by a patient-controlled analgesia pump and had similar pain intensity scores measured by the visual analog scale.94
Taguchi and coworkers studied the effect of acupuncture on anesthetic requirement in healthy volunteers in a rigorous double-blind experiment. This group found that healthy volunteers who received auricular acupuncture at four points required 8.5% less desflurane anesthesia to prevent movement in response to noxious stimuli when compared to healthy volunteers who did not receive auricular acupuncture.95
Miscellaneous
Preliminary evidence from small but well done RCTs suggests that acupuncture is effective at relieving symptoms in patients with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). The most recent study recruited 63 patients who met the U.S National Institutes of Health (NIH) consensus criteria for CP/CPPS in a three arm RCT. The electroacupuncture group received acupuncture according to classical and neuroanatomic principles with electrical stimulation, advice, and exercise. The sham acupuncture group received superficial needling at nonacupuncture points, advice, and exercise, and the final group received advice and exercise only. Symptoms were assessed using the NIH Chronic Prostatitis Symptom Index (NIH-CPSI) and the primary outcome was change in symptoms using this index. All patients receiving electroacupuncture experienced at least a 6 point reduction in the NIH-CPSI total score compared to 16.7% of the sham acupuncture group and 25% of the advice and exercise group. Additionally prostaglandin E2 levels in the urine after prostatic massage decreased in the electroacupuncture group, whereas the levels increased in the other two groups.96
Lee SW and colleagues found that 32 of 44 (72%) CP/CPPS patients receiving acupuncture experienced at least a 6 point decrease in the NIH-CPSI score compared to 21 of 45 (47%) of patients receiving superficial acupuncture at nonacupuncture points.97 Chen and coworkers reported that 10 of 12 CP/CPPS patients who were refractory to antibiotics, α-blockers, antiinflammatory agents, and phytotherapy experienced a greater than 50% reduction in the NIH-CPSI with acupuncture at an average of 33 weeks after treatment.98
A systematic review of acupuncture for the management of labor pain was published in The American Journal of Obstetrics and Gynecology in 2004 and included three RCTs. Two RCTs compared acupuncture with usual care and found that intrapartum acupuncture resulted in lower usage of meperidine and epidural analgesia. One RCT compared acupuncture to superficial needling at nonacupuncture points and found that the classical acupuncture group reported less intrapartum and postpartum pain, requested meperidine and epidural analgesia less often, and required oxytocin augmentation less often.99
1. Reston J. Now, about my operation in Peking. New York Times. 1971 Jul 26. Sect. A
2. Helms J.M. An overview of medical acupuncture. Altern Ther Health Med. 1998;4:35-45.
3. Helms J. Acupuncture Energetics, A Clinical Approach for Physicians. Berkeley: Medical Acupuncture Publishers; 1995. 3-17
4. Unschuld P. Medicine in China. Berkeley: University of California Press; 1985. 229-262
5. Birch S. Understanding Acupuncture. New York: Churchill Livingstone; 1999. 43-85
6. Bauer M. An Interview with Dr. Paul Unschuld, Part 2. Acupuncture Today. 5, 2004. 8
7. Karst M., Winterhalter M., Münte S., et al. Auricular acupuncture for dental anxiety: A randomized controlled trial. Anesth Analg. 2007;104:295-300.
8. Kober A., Scheck T., Schubert B., et al. Auricular acupressure as a treatment for anxiety in prehospital transport settings. Anesthesiology. 2003;98:1328-1332.
9. Wang S.M., Kain Z.N. Auricular acupuncture: A potential treatment for anxiety. Anesth Analg. 2001;92:548-553.
10. Spence D.W., Kayumov L., Chen A., et al. Acupuncture increases nocturnal melatonin secretion and reduces insomnia and anxiety: A preliminary report. J Neuropsychiatry Clin Neurosci. 2004;16:19-28.
11. Balk J., Day R., Rosenzweig M., et al. Pilot, randomized, modified, double-blind, placebo-controlled trial of acupuncture for cancer-related fatigue. J Soc Integr Oncol. 2009;7:4-11.
12. Hsieh R.L., Wang L.Y., Lee W.C. Additional therapeutic effects of electroacupuncture in conjunction with conventional rehabilitation for patients with first-ever ischaemic stroke. J Rehabil Med. 2007;39:205-211.
13. da Silva J.B., Nakamura M.U., Cordeiro J.A., et al. Acupuncture for dyspepsia in pregnancy: A prospective, randomised, controlled study. Acupunct Med. 2009;27:50-53.
14. Sindrup S.H., Otto M., Finnerup N.B., Jensen T.S. Antidepressants in the treatment of neuropathic pain. Basic Clin Pharmacol Toxicol. 2005;96:399-409.
15. Saarto T., Wiffen P.J. Antidepressants for neuropathic pain. Cochrane Database Syst Rev. 3, 2005. CD005454
16. Villoslada P., Steinman L., Baranzini S.E. Systems biology and its application to the understanding of neurological diseases. Ann Neurol. 2009;65:124-139.
17. Huang R.S., Ratain M.J. Pharmacogenetics and pharmacogenomics of anticancer agents. CA Cancer J Clin. 2009;59:42-55.
18. Searle R., Hopkins P.M. Pharmacogenomic variability and anaesthesia. Br J Anaesth. 2009;103:14-25.
19. Limdi N.A., Veenstra D.L. Warfarin pharmacogenetics. Pharmacotherapy. 2008;28:1084-1097.
20. Witt C., Brinkhaus B., Jena S., et al. Acupuncture in patients with osteoarthritis of the knee: A randomised trial. Lancet. 2005;366:136-143.
21. Scharf H.P., Mansmann U., Streitberger K., et al. Acupuncture and knee osteoarthritis: A three-armed randomized trial. Ann Intern Med. 2006;145:12-20.
22. Hui K.K., Liu J., Marina O., et al. The integrated response of the human cerebro-cerebellar and limbic systems to acupuncture stimulation at ST 36 as evidenced by fMRI. Neuroimage. 2005;27:479-496.
23. Kou W., Bell J.D., Gareus I., et al. Repeated acupuncture treatment affects leukocyte circulation in healthy young male subjects: A randomized single-blind two-period crossover study. Brain Behav Immun. 2005;19:318-324.
24. Zhao Z.Q. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008;85:355-375.
25. Kavoussi B., Ross B.E. The neuroimmune basis of anti-inflammatory acupuncture. Integr Cancer Ther. 2007;6:251-257.
26. Han J.S. Acupuncture and endorphins. Neurosci Lett. 2004;361:258-261.
27. Pyne D., Shenker N.G. Demystifying acupuncture. Rheumatology. 2008;47:1132-1136.
28. Melzack R. Evolution of the neuromatrix theory of pain. The Prithvi Raj Lecture: Presented at the Third World Congress of World Institute of Pain, Barcelona 2004. Pain Pract. 2005;5:85-94.
29. Napadow V., Kettner N., Liu J., et al. Hypothalamus and amygdala response to acupuncture stimuli in carpal tunnel syndrome. Pain. 2007;130:254-266.
30. Stux G., Berman B., Pomeranz B. Basics of Acupuncture. New York: Springer-Verlag; 2003. 7-27
31. Langevin H.M., Churchill D.L., Cipolla M.J. Mechanical signaling through connective tissue: A mechanism for the therapeutic effect of acupuncture. FASEB J. 2001;15:2275-2282.
32. Langevin H.M. Connective tissue: A body-wide signaling network? Med Hypotheses. 2006;66:1074-1077.
33. Langevin H.M., Churchill D.L., Wu J., et al. Evidence of connective tissue involvement in acupuncture. FASEB J. 2002;16:872-874.
34. Langevin H.M., Bouffard N.A., Churchill D.L., Badger G.J. Connective tissue fibroblast response to acupuncture: Dose-dependent effect of bidirectional needle rotation. J Altern Complement Med. 2007;13:355-360.
35. Shah J.P., Danoff J.V., Desai M.J., et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. 2008;89:16-23.
36. Simons D.G. New views of myofascial trigger points: Etiology and diagnosis. Arch Phys Med Rehabil. 2008;89:157-159.
37. Smith G.V., Alon G., Roys S.R., et al. Functional MRI determination of a dose-response relationship to lower extremity neuromuscular electrical stimulation in healthy subjects. Exp Brain Res. 2003;150:33-39.
38. Korvenoja A., Huttunen J., Salli E., et al. Activation of multiple cortical areas in response to somatosensory stimulation: Combined magnetoencephalographic and functional magnetic resonance imaging. Hum Brain Mapp. 1999;8:13-27.
39. Moisset X., Bouhassira D. Brain imaging of neuropathic pain. Neuroimage. 2007;37:S80-S88.
40. Lewith G.T., White P.J., Pariente J. Investigating acupuncture using brain imaging techniques: The current state of play. Evid Based Complement Alternat Med. 2005;2:315-319.
41. Dhond R.P., Kettner N., Napadow V. Neuroimaging acupuncture effects in the human brain. J Altern Complement Med. 2007;13:603-616.
42. Liu W.C., Feldman S.C., Cook D.B., et al. fMRI study of acupuncture-induced periaqueductal gray activity in humans. Neuroreport. 2004;15:1937-1940.
43. Neugebauer V., Li W., Bird G.C., Han J.S. The amygdala and persistent pain. Neuroscientist. 2004;10:221-234.
44. Napadow V., Kettner N., Ryan A., et al. Somatosensory cortical plasticity in carpal tunnel syndrome—A cross-sectional fMRI evaluation. Neuroimage. 2006;31:520-530.
45. Napadow V., Liu J., Li M., et al. Somatosensory cortical plasticity in carpal tunnel syndrome treated by acupuncture. Hum Brain Mapp. 2007;28:159-171.
46. Faingold C.L. Electrical stimulation therapies for CNS disorders and pain are mediated by competition between different neuronal networks in the brain. Med Hypotheses. 2008;71:668-681.
47. Witt C.M., Brinkhaus B., Reinhold T., et al. Efficacy, effectiveness, safety and costs of acupuncture for chronic pain—results of a large research initiative. Acupunct Med. 2006;24:S33-S39.
48. Witt C.M., Jena S., Selim D., et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol. 2006;164:487-496.
49. Haake M., Müller H.H., Schade-Brittinger C., et al. German acupuncture trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892-1898.
50. Wu M.T., Sheen J.M., Chuang K.H., et al. Neuronal specificity of acupuncture response: A fMRI study with electroacupuncture. Neuroimage. 2002;16:1028-1037.
51. Li G., Cheung R.T., Ma Q.Y., Yang E.S. Visual cortical activations on fMRI upon stimulation of the vision-implicated acupoints. Neuroreport. 2003;14:669-673.
52. Shiotani A., Tatewaki M., Hoshino E., et al. Effects of electroacupuncture on gastric myoelectrical activity in healthy humans. Neurogastroenterol Motil. 2004;16:293-298.
53. Kroeling P., Gross A.R., Goldsmith C.H., et al. A Cochrane review of electrotherapy for mechanical neck disorders. Spine. 2005;30:E641-E648.
54. Peloso P., Gross A., Haines T., et al. Medicinal and injection therapies for mechanical neck disorders. Cochrane Database Syst Rev. 3, 2007. CD000319
55. van Tulder M.W., Koes B., Seitsalo S., et al. Outcome of invasive treatment modalities on back pain and sciatica: An evidence-based review. Eur Spine J. 2006;15:S82-S92.
56. van Tulder M.W., Koes B., Malmivaara A. Outcome of non-invasive treatment modalities on back pain: An evidence-based review. Eur Spine J. 2006;15:S64-S81.
57. Ernst E., White A.R. Prospective studies of the safety of acupuncture: A systematic review. Am J Med. 2001;110:481-485.
58. Witt C.M., Pach D., Brinkhaus B., et al. Safety of acupuncture: Results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed. 2009;16:91-97.
59. Wonderling D., Vickers A.J., Grieve R., et al. Cost effectiveness analysis of a randomised trial of acupuncture for chronic headache in primary care. BMJ. 2004;328:747.
60. Evans K.W., Boan J.A., Evans J.L., Shuaib A. Economic evaluation of oral sumatriptan compared with oral caffeine/ergotamine for migraine. Pharmacoeconomics. 1997;12:565-577.
61. Willich S.N., Reinhold T., Selim D., et al. Cost-effectiveness of acupuncture treatment in patients with chronic neck pain. Pain. 2006;125:107-113.
62. Ratcliffe J., Thomas K.J., MacPherson H., Brazier J. A randomised controlled trial of acupuncture care for persistent low back pain: Cost effectiveness analysis. BMJ. 2006;333(7569):626.
63. van Weel C., Knottnerus J.A. Evidence-based interventions and comprehensive treatment. Lancet. 1999;353:916-918.
64. Mant D. Can randomised trials inform clinical decisions about individual patients? Lancet. 1999;353:743-746.
65. Feinstein A.R., Horwitz R.I. Problems in the ‘‘evidence’’ of ‘‘evidence-based medicine’’. Am J Med. 1997;103:529-535.
66. Hotopf M. The pragmatic randomised controlled trial. Adv Psychiatr Treat. 2002;8:326-333.
67. Katon W., Von Korff M., Lin E., et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psych. 1999;56:1109-1115.
68. Hróbjartsson A., Gøtzsche P.C. Placebo treatment versus no treatment. Cochrane Database Syst Rev. 1, 2003. CD003974
69. Serruys P.W., Morice M.C., Kappetein A.P. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-972.
70. Furlan A.D., van Tulder M.W., Cherkin D.C., et al. Acupuncture and dry-needling for low back pain. Cochrane Database Syst Rev. 1, 2005. CD001351
71. Brinkhaus B., Witt C.M., Jena S., et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006;166:450-457.
72. Trinh K.V., Graham N., Gross A.R., et al. Acupuncture for neck disorders. Cochrane Database Syst Rev. 3, 2006. CD004870
73. Linde K., Allais G., Brinkhaus B., et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 1, 2009. CD001218
74. Linde K., Allais G., Brinkhaus B., et al. Acupuncture for tension-type headache. Cochrane Database Syst Rev. 1, 2009. CD007587
75. Endres H.G., Diener H.C., Molsberger A. Role of acupuncture in the treatment of migraine. Expert Rev Neurother. 2007;7:1121-1134.
76. Li Y., Liang F., Yang X., et al. Acupuncture for treating acute attacks of migraine: A randomized controlled trial. Headache. 2009;49:805-816.
77. Melchart D., Thormaehlen J., Hager S., et al. Acupuncture versus placebo versus sumatriptan for early treatment of migraine attacks: A randomized controlled trial. J Intern Med. 2003;253:181-188.
78. White A., Foster N.E., Cummings M., et al. Acupuncture treatment for chronic knee pain: A systematic review. Rheumatology. 2007;46:384-390.
79. Manheimer E., Linde K., Lao L., et al. Meta-analysis: Acupuncture for osteoarthritis of the knee. Ann Intern Med. 2007;146:868-877.
80. Green S., Buchbinder R., Hetrick S. Acupuncture for shoulder pain. Cochrane Database Syst Rev. 2, 2005. CD005319
81. Green S., Buchbinder R., Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2, 2003. CD004258
82. Buchbinder R., Green S., Youd J.M. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev. 1, 2003. CD004016
83. Guerra de Hoyos J.A. Andrés Martín Mdel C, Bassas y Baena de Leon E, et al. Randomised trial of long term effect of acupuncture for shoulder pain. Pain. 2004;112:289-298.
84. Johansson K.M., Adolfsson L.E., Foldevi M.O. Effects of acupuncture versus ultrasound in patients with impingement syndrome: Randomized clinical trial. Phys Ther. 2005;85:490-501.
85. Vas J., Ortega C., Olmo V., et al. Single-point acupuncture and physiotherapy for the treatment of painful shoulder: A multicentre randomized controlled trial. Rheumatology. 2008;47:887-893.
86. Trinh K.V., Phillips S.D., Ho E., Damsma K. Acupuncture for the alleviation of lateral epicondyle pain: A systematic review. Rheumatology. 2004;43:1085-1090.
87. Trudel D., Duley J., Zastrow I., et al. Rehabilitation for patients with lateral epicondylitis: A systematic review. J Hand Ther. 2004;17:243-266.
88. Stener-Victorin E., Kruse-Smidje C., Jung K. Comparison between electro-acupuncture and hydrotherapy, both in combination with patient education and patient education alone, on the symptomatic treatment of osteoarthritis of the hip. Clin J Pain. 2004;20:179-185.
89. Witt C.M., Jena S., Brinkhaus B., et al. Acupuncture in patients with osteoarthritis of the knee or hip: a randomized, controlled trial with an additional nonrandomized arm. Arthritis Rheum. 2006;54:3485-3493.
90. Mayhew E., Ernst E. Acupuncture for fibromyalgia—a systematic review of randomized clinical trials. Rheumatology. 2007;46:801-804.
91. Rosted P. Practical recommendations for the use of acupuncture in the treatment of temporomandibular disorders based on the outcome of published controlled studies. Oral Dis. 2001;7:109-115.
92. Smith P., Mosscrop D., Davies S., et al. The efficacy of acupuncture in the treatment of temporomandibular joint myofascial pain: A randomised controlled trial. J Dent. 2007;35:259.
93. Sun Y., Gan T.J., Dubose J.W., et al. Acupuncture and related techniques for postoperative pain: A systematic review of randomized controlled trials. Br J Anaesth. 2008;101:151-160.
94. Usichenko T.I., Dinse M., Hermsen M., et al. Auricular acupuncture for pain relief after total hip arthroplasty—a randomized controlled study. Pain. 2005;114:320-327.
95. Taguchi A., Sharma N., Ali S.Z., et al. The effect of auricular acupuncture on anaesthesia with desflurane. Anaesthesia. 2002;57:1159-1163.
96. Lee S.H., Lee B.C. Electroacupuncture relieves pain in men with chronic prostatitis/chronic pelvic pain syndrome: Three-arm randomized trial. Urology. 2009;73:1036-1041.
97. Lee S.W., Liong M.L., Yuen K.H., et al. Acupuncture versus sham acupuncture for chronic prostatitis/chronic pelvic pain. Am J Med. 2008;121:79. e1-e7
98. Chen R., Nickel J.C. Acupuncture ameliorates symptoms in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2003;61:1156-1159.
99. Skilnand E., Fossen D., Heiberg E. Acupuncture in the management of pain in labor. Acta Obstet Gynecol Scand. 2002;81:943-948.