CHAPTER 45 Medial Epicondylitis
INTRODUCTION
Medial epicondylitis is the most common cause of medial elbow pain but is only 15% to 20% as common as lateral epicondylitis. The relative infrequency of medial epicondylitis has resulted in a paucity of information on medial epicondylitis, but work by Vangsness and Jobe,28 Gabel and Morrey,5 Ollivierre and associates,18 and Kurvers and Verhaar11 has clarified the pathology, treatment, and outcomes in medial epicondylitis. The significance of associated ulnar neuropathy at the elbow has also been assessed and is the primary component of the classification of medial epicondylitis. The results of nonoperative management, including corticosteroid injections, have been reported by Stahl and Kaufman.25 The compilation of information in these studies6 has resulted in a clearer understanding of medial epicondylitis and its management, allowing more appropriate patient care.
ANATOMY
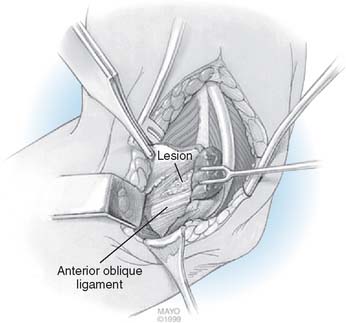
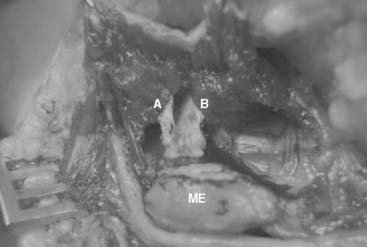
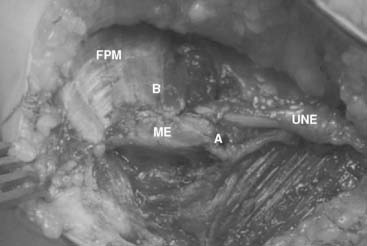
The pronator teres origin off the MCT occupies the proximoradial side of this vertically oriented septum (Fig. 45-1). The flexor carpi radialis, which also has a very small direct muscular epicondylar origin, finds its primary origin off the distoulnar aspect of the MCT. Although additional muscular or tendinous origins off the epicondyle are seen, the critical lesion of medial epicondylitis consists of this MCT and its associated pronator teres and flexor carpi radialis origins. This septum bifurcates 2 to 3 cm distal to the epicondyle (Fig. 45-2) with the pronator teres radially, the flexor carpi radialis between the septa and the digital flexors ulnarly.
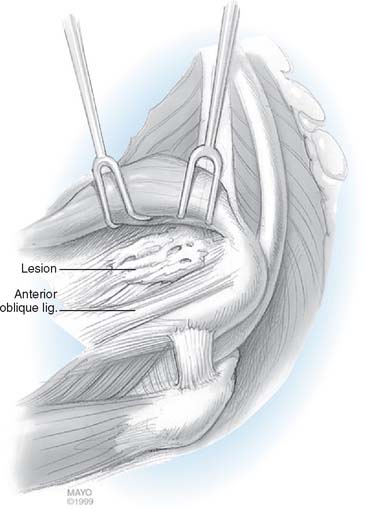
Although it plays a central mechanical role in medial epicondylitis, the MCT serves surgically as a landmark for the pathology of medial epicondylitis as well as a means of identification and avoidance of the AOL proper. The MCT rises off the anterior inferior epicondyle with an oblique parasagittal orientation extending approximately 12 cm into the proximal forearm. Immediately posterior to the proximal 3 to 4 cm of the MCT is the AOL (see Fig. 45-1). There is a surgical interval between the MCT and AOL, but anatomically, they are contiguous over the proximal 50% to 75% of the AOL. The distal 25% to 50% of the AOL is separate from the MCT’s posterior margin, an interval that allows for independent surgical manipulation of MCT and AOL distally. Any surgical elevation of the MCT off the medial epicondyle, posterior to the MCT, by definition, violates the origin of the AOL.
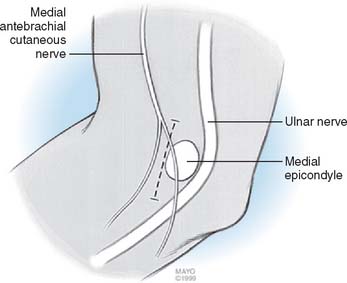
The neural concerns in medial epicondylitis consist of the medial antebrachial cutaneous nerve (MABCN) and the ulnar nerve. The MABCN courses in the subcutaneous tissue in the anteromedial arm13 until just proximal to the medial epicondyle, where it divides into an anterior branch, which travels distally, and a posterior branch,2 which travels directly over the flexor pronator mass to the posterior medial forearm. The ulnar nerve rests on the posterior aspect of the medial intermuscular septum in the arm. As it approaches the medial epicondyle, it is covered by a retinaculum,15 which maintains its position preventing subluxation. It enters the forearm through the two heads of the flexor carpi ulnaris at the cubital tunnel. At entry into the cubital tunnel, the ulnar nerve lies immediately adjacent to the posterior margin of the flexor pronator mass.
PRESENTATION
Medial epicondylitis presents with medial elbow pain, which is related to activity, especially repetitive or forceful pronation. It has a peak incidence in the third through fifth decade, with a 2:1 male-to-female ratio. It occurs in the dominant elbow in 60% of cases and is associated with an acute injury (direct or indirect) in 30%, whereas 70% of cases have a more insidious onset. Associated ulnar neuropathy is seen in approximately 50% of cases, whereas associated diagnoses at a separate level (lateral epicondylitis, 30%; carpal tunnel syndrome, 25%; rotator cuff pathology, 20%) are also frequently seen on past medical history. A vocational contribution to the patient’s symptoms may be seen in more than 50% of cases; an avocational contribution is seen in 10% to 20% of patients (hence, the eponym golfer’s elbow). The prevalence of medial epicondylitis is approximately one half of 1%, with smoking, obesity, repetitive, and forceful activities being significant risk factors.20
Physical examination demonstrates direct tenderness over the anterior aspect of the medial epicondyle in essentially all cases. Some patients may have maximum tenderness just distal to the epicondyle in the proximal flexor pronator mass. Resisted pronation tenderness is seen in 90% and resisted wrist palmar flexion tenderness in 70% of patients. Range of motion is typically normal. Associated medial collateral ligament insufficiency may be tested with valgus stress testing, as described by Jobe and associates9 (valgus stress at 30 degrees of flexion with palpation of the AOL) or the moving valgus stress test, as described by O’Driscoll and associates.17 The ulnar nerve should be evaluated, including testing for the presence of Tinel’s sign, elbow flexion test, nerve compression test, and ulnar nerve subluxation. Distal objective function (two-point discrimination, intrinsic strength, and dorsal cutaneous nerve status) completes the ulnar nerve examination. The classification of medial epicondylitis5 is based on the presence and severity of concomitant ulnar neuropathy at the elbow. Type I medial epicondylitis includes those patients with no associated ulnar nerve symptoms. Type II medial epicondylitis is divided based on the degree of ulnar nerve involvement. Type IIA has ulnar nerve symptoms with no objective deficit, whereas type IIB has objective deficits on physical exam or electromyography.
EVALUATION
Radiographic evaluation should include plain radiographs to rule out associated lesions (e.g., osteoarthritis) as well as valgus stress radiographs23 if medial instability is suspected (Fig. 45-3). Medial epicondylar calcification is seen in 10% to 20% of cases but is not prognostic. Magnetic resonance imaging (MRI) has concentrated on lateral epicondylitis,12,19 but within these series and medial epicondylitis–specific series,10 it has a high sensitivity and specificity. Because medial epicondylitis is primarily a clinical diagnosis, MRI should be reserved for more complex situations such as reoperation or associated medial collateral ligament concerns.
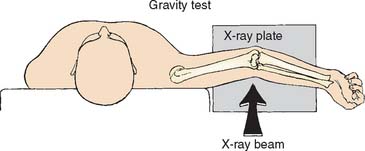
FIGURE 45-3 Valgus stress radiograph for assessment of valgus instability as a cause of medial elbow pain.
(From Woods, G. W., and Tullos, H. S.: Elbow instability and medial epicondyle fractures. Am. J. Sports Med. 5:23, 1977.)
The differential diagnosis of medial elbow pain includes proximal neurogenic sources (cervical radiculopathy, thoracic outlet syndrome) as well as shoulder-level musculoskeletal sources, each of which can be excluded with appropriate evaluation. Local causes of medial elbow discomfort are limited but should be evaluated as well. A snapping medial head of the triceps24 and subluxation of the ulnar nerve usually give a history of a palpable “popping” sensation and may have an associated ulnar neuropathic condition. On examination, tendon and nerve subluxation are found with elbow flexion. Triceps tendinitis presents with more posterior elbow discomfort, reproduced with resisted elbow extension. Radiographs usually reveal an olecranon spur. Medial collateral insufficiency is typically seen in chronic valgus activities and is evaluated as previously mentioned. Medial collateral ligament deficiency may coexist with medial epicondylitis. Isolated ulnar neuropathy may manifest not only with distal neurologic symptoms but also with medial elbow discomfort from the neuro nervorum. Examination demonstrates reproduction of local pain with the elbow flexion and nerve compression tests. Postoperative medial elbow pain may emanate from any of these diagnoses but also may include injury to the MABCN. Hyperesthesia or hypesthesias at the medial forearm along with the presence of Tinel’s sign along the MABCN confirm this diagnosis.
TREATMENT
NONOPERATIVE MANAGEMENT
A wrist splint to rest the wrist flexors, as well as a padded counter-force brace is prescribed.27 The pad of the counter-force brace should be anteromedial on the flexor pronator mass, not medial or posteromedial over the ulnar nerve (Fig. 45-4). If ulnar nerve symptoms are increased with appropriate use of the brace, then the brace needs to be discontinued.
Concomitant ulnar neuropathy at the elbow is managed with avoidance of repetitive or prolonged elbow flexion and leaning on the elbow. Nighttime extension splinting, if tolerated, may be useful. Ultrasound, iontophoresis,3 acupuncture,14 laser,29 and extracorporeal shock wave therapy22 have no proven independent efficacy in medial epicondylitis. Blood or platelet-rich plasma injection reportedly has a role in patients in whom other nonoperative measures have failed, but requires further definitive study.26
SURGICAL INTERVENTION
The operative treatment of medial epicondylitis is considered in patients who fail to respond to conservative management (one to two injections over a 6- to 9-month period) or in patients who demonstrate a progression of the ulnar neuropathy. The surgical management of medial epicondylitis is guided by the classification. Type I cases require epicondylar débridement. Type IIA cases require epicondylar débridement, and cubital tunnel decompression or transposition. Type IIB cases require débridement with submuscular transposition of the ulnar nerve.
The surgical technique of medial epicondylar débridement involves a 3-cm longitudinal incision just anterior to the medial epicondyle (Fig. 45-5). The MABCN is consistently encountered in the subcutaneous tissue and should be protected. The flexor pronator fascia is discretely identified on the medial epicondyle and is incised, leaving a 2-mm rim of the superficial fascia attached to the medial epicondyle for later repair. The underlying muscle is elevated to allow identification of the longitudinally oriented MCT. A nidus is usually found within the origin of the MCT (Fig. 45-6). The proximal MCT is fully exposed, with care taken on its posterior margin to identify and protect the AOL. A 3- to 4-cm section of the MCT including the nidus is then resected, in essence disconnecting the MCT septum within the flexor pronator mass from the epicondyle. The flexor pronator fascia is repaired back to the retained rim of fascia at its original position or in a slightly (1 cm) lengthened position.
In Type IIA cases, with limited ulnar nerve involvement, MCT débridement as in type I cases addresses the tendinosis. Although cubital tunnel release may be used for management of ulnar nerve compression, submuscular transposition is more definitive and may yield better results.11 If any anatomic concern relating to the ulnar nerve is encountered (e.g., subluxation or adhesions), submuscular transposition is indicated.
Cubital tunnel release is accomplished without extension of the débridement incision. Subcutaneous dissection posteriorly allows identification of the fascia overlying the ulnar nerve. The fascia is opened at the inferior tip of the medial epicondyle distal to the cubital tunnel retinaculum and incised distally, releasing the flexor carpi ulnaris (FCU) arcade. There are two components to the arcade, the superficial and the deep epimysium, both of which need to be released. After release of the superficial FCU fascia, the two muscle bellies (humeral and ulnar origin) are bluntly separated. The deep FCU fascia, directed over the ulnar nerve, is released with tenotomy scissors. The ulnar nerve itself is not disturbed. The proximal retinaculum, as described by O’Driscoll and colleagues,15 is preserved if possible to minimize the risk of iatrogenic subluxation. The nerve is assessed with flexion and, if subluxation is induced, transposition is performed.
In type IIA cases that require transposition or type IIB cases, submuscular transposition is preferred. An incision over the ulnar nerve is created. Care is taken to protect the MABCN distally. The flexor pronator mass and ulnar nerve are identified. Flexor pronator elevation and MCT débridement are performed as previously described. Ulnar nerve transposition is accomplished with decompression, mobilization, and transposition of the nerve. Decompression involves proximal release of the arcade of Struthers and brachial fascia for approximately 10 to 12 cm proximal to the epicondyle. The medial intermuscular septum is discretely exposed and the inferior 4 to 6 cm excised. The FCU arcade is released as with a cubital tunnel release and the deep flexor pronator aponeurosis is bluntly released with Metzenbaum scissors. Mobilization of the ulnar nerve requires preservation of the longitudinal blood supply throughout and segmental blood supply where possible. The nerve is mobilized from its bed for approximately 8 to 10 cm proximally and 3 to 4 cm distally. The distal mobilization may be impeded by the first motor branch of the FCU. This branch can be mobilized by dissection within the ulnar head muscle, gaining approximately 2 cm in length, sufficient to allow transposition without angulation.
After the MCT has been resected, the flexor pronator mass is further prepared by incising any additional small septae within the muscle. The posterior fascia of the humeral head of the FCU along the posterior margin of the mass is incised distally for 3 to 4 cm to prevent iatrogenic impingement with transposition. The nerve is then brought anteriorly to its submuscular position and examined for any acute angulation or impingement by any residual fascia bands. The prepared flexor pronator mass is then repaired over the nerve in a transposed position. The repair should begin proximally with the proximal margin of the fascia translated 1.5 to 2 cm distally from its original position (Fig. 45-7). A running braided nonabsorbable suture with the initial knot buried is used. The suture runs distally, suturing the FP mass back down to the epicondyle and then closing the FCU release interval to strengthen the FP mass repair. Once transposition is complete, the nerve is again examined with flexion and extension.
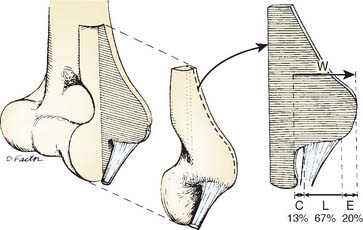
Percutaneous medial epicondylar release1 is contraindicated because of concerns with the MABCN and ulnar nerve as well as incomplete management of the medial epicondylitis. Formal medial epicondylectomy8 may compromise the AOL origin16 (Fig. 45-8) and is not recommended. Because the pathology in medial epicondylitis is musculotendinous and not osseous, epicondylar removal offers no pathophysiologic advantage. Endoscopic medial epicondylar débridement7 has not been reported.
RESULTS
Nonoperative measures are successful in the majority of patients with medial epicondylitis. Conservative treatment fails in only 5% to 10% of patients5 owing to persistent epicondylitis or persistent progressive ulnar neuropathy.
Surgical results correlate with the type of medial epicondylitis. Type IA or IIA medial epicondylitis has 95% good or excellent results, as reported in two studies5,28 and slightly lower success rates in two additional series.11,18 The time to attainment of a good or excellent level is approximately 6 months in two thirds of patients and up to 2 years in the remaining one third.5
Type IIB medial epicondylitis, with more involved associated ulnar neuropathy, has a much poorer prognosis. The poorer results in type IIB medial epicondylitis relate primarily to the failure of ulnar neuropathy to respond to surgical management. Cubital tunnel release alone as a means of management of associated ulnar neuropathy in medial epicondylitis has been shown by Kurvers and Verhaar11 to potentially be suboptimal. Failure to quantify the degree of ulnar nerve involvement and treat accordingly results in persistent ulnar nerve symptoms. Ulnar neuropathy in medial epicondylitis may be related to a “mass effect” at the anterior cubital tunnel from the flexor pronator mass. Although this “mass effect” may be treated by medial epicondylar débridement, fixed changes in the ulnar nerve or cubital tunnel may prevent resolution of the ulnar neuropathy. The management of concomitant ulnar neuropathy in medial epicondylitis requires independent management of the ulnar nerve and medial epicondylitis except in select mild cases of ulnar neuropathy.
COMPLICATIONS
Complications of operative treatment are uncommon. Restricted elbow range of motion is minimized by early protected range of motion. Neurologic complications include neurogenic pain from injury to the MABCN and ulnar nerve deficiencies. Identification and protection of the MABCN2 is essential. If the nerve is injured intraoperatively or if recognized postoperatively, this may be surgically addressed by placement of the medial antebrachial cutaneous neuroma into the brachialis muscle belly.
Persistent ulnar neuropathy at the elbow can be managed by revision with submuscular transposition, except in cases that have had a prior submuscular transposition, in which case the results of revision are less predictable.4 The results with a patient specific approach are approximately 80% good or excellent, but appropriate selection criteria are critical and the patient should be advised of the possibility of no improvement in status.
Iatrogenic medial elbow instability is a recognized complication of medial epicondylar débridement and can be avoided as described earlier. Reconstruction at the AOL9,21 has a high success rate but requires a prolonged period of recovery.
1 Baumgard S.H., Schwartz D.R. Percutaneous release of the epicondylar muscles for humeral epicondylitis. Am. J. Sports Med. 1982;10:233.
2 Dellon A.L., MacKinnon S.E. Injury to the medial antebrachial cutaneous nerve during cubital tunnel surgery. J. Hand Surg. Br. 1985;10:33.
3 Demirtas R.N., Oner C. The treatment of lateral epicondylitis by iontophoresis of sodium salicylate and sodium diclofenac. Clin. Rehab. 1998;12:23.
4 Gabel G.T., Amadio P.C. Reoperation for failed decompression of the ulnar nerve in the region of the elbow. J. Bone Joint Surg. Am. 1990;72:213.
5 Gabel G.T., Morrey B.F. Operative treatment of medial epicondylitis. Influence of concomitant ulnar neuropathy at the elbow. J. Bone Joint Surg. 1995;77A:1065.
6 Gabel G.T., Morrey B.F. Tennis elbow. Instruct. Course Lect. 1998;47:165.
7 Grifka J., Boenke S., Kramer J. Endoscopic therapy in epicondylitis radialis humeri. Arthroscopy. 1995;11:743.
8 Heithoff S.J., Millender L.H., Nalebuff E.A., Petruska A.J. Medial epicondylectomy for the treatment of ulnar nerve compression at the elbow. J. Hand Surg. Am. 1990;15:22.
9 Jobe F.W., Stark H., Lombardo S.T. Reconstruction of the ulnar collateral ligament in athletes. J. Bone Joint Surg. 1986;68A:1158.
10 Kijowski R., De Smet A.A. Magnetic resonance imaging findings in patients with medial epicondylitis. Skeletal Radiol. 2005;34:196.
11 Kurvers H., Verhaar J. The results of operative treatment of medial epicondylitis. J. Bone Joint Surg. Am. 1995;77:1374.
12 Martin C.D., Schweitzer M.E. MR imaging of epicondylitis. Skel. Radiol. 1998;27:133.
13 Masear V.R., Meyer R.D., Pichora D.R. Surgical anatomy of the medial antebrachial cutaneous nerve. J. Hand Surg. Am. 1989;14:267.
14 Molsberger A., Hille E. The analgesic effect of acupuncture in chronic tennis elbow pain. Br. J. Rheum. 1994;33:1162.
15 O’Driscoll S.W., Horii G., Carmichael S.W., Morrey B.F. The cubital tunnel and ulnar neuropathy. J. Bone Joint Surg. 1991;73B:613.
16 O’Driscoll S.W., Horii E., Morrey B.F. Anatomy of the attachment of the medial ulnar collateral ligament. J. Bone Joint Surg. 1992;17:164.
17 Shawn W.M., O’Driscoll S.W., Lawton R.L., Smith A. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am. J. Sports Med. 2005;33:231.
18 Ollivierre C.O., Nirschl R.P., Pettrone F.A. Resection and repair for medial tennis elbow. A prospective analysis. Am. J. Sports Med. 1995;23:214.
19 Potter H.G., Hannafin J.A., Morwessel R.M., Dicarlo E.F., O’Brien S.J., Altchek D.W. Lateral epicondylitis: correlation of MR imaging, surgical, and histopathologic findings. Radiology. 1995;196:43.
20 Rahman S., Viikari-Juntura E., Varonen H., Heliovaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am. J. Epidemiol. 2006;164:1065.
21 Rohrbough J.T., Altchek D.W., Hyman J., Williams R.J., Botts J.D. Medial collateral ligament reconstruction of the elbow using the docking technique. Am. J. Sports Med. 2002;30:541.
22 Rompe J.D., Hope C., Kullmer K., Heine J., Burger R. Analgesic effect of extracorporeal shock wave therapy on chronic tennis elbow. J. Bone Joint Surg. 1996;78B:233.
23 Schwab G.H., Bennett J.B., Woods G.W., Tullos M.S. Biomechanics of elbow instability. The role of the medial collateral ligament. Clin. Orthop. Relat. Res. 1980;146:42.
24 Spinner R.J., Gabel G.T. Iatrogenic snapping of the medial head of the triceps after ulnar nerve transposition. J. South. Orthop. Assoc. 2001;10:236.
25 Stahl S., Kaufman T. Ulnar nerve injury at the elbow after steroid injection for medial epicondylitis. J. Hand Surg. Br. 1997;21:69.
26 Suresh S.P.S., Kaline E.A., Jones H., Connell D. Medial epicondylitis: is ultrasound guided autologous blood injection an effective treatment? Br. J. Sports Med. 2006;40:935.
27 Walther M., Kirschner S., Koenig A., Barthel T., Gohlke F. Biomechanical evaluation of braces used for the treatment of epicondylitis. J. Shoulder Elbow Surg. 2002;11:265.
28 Vangsness C.T., Jobe F.W. Surgical management of medial epicondylitis. J. Bone Joint Surg. 1991;73B:409.
29 Vassellen O.Jr., Hoeg N., Kjeldstad B., Johnsson A., Larsen S. Low level laser versus placebo in the treatment of tennis elbow. Scand. J. Rehabil. Med. 1992;24:37.