Chapter 68 Maxillofacial and upper-airway injuries
MAXILLOFACIAL INJURIES
Life-threatening haemorrhage and airway obstruction are common complications accompanying severe blunt or penetrating maxillofacial and neck injury. Injuries may be isolated or part of multisystem trauma. Up to 20% of people with facial injury will have life-threatening associated injuries: 15% with closed head injury, 3.5% with airway obstruction and 1.5% with pulmonary contusion and/or aspiration.1–3 Urgent skilled airway management and awareness of other commonly associated injuries to the brain, cervical spine, thorax and oesophagus are paramount in preventing adverse outcomes. This chapter outlines the basic anatomy, pathology, complications and common pitfalls in the emergency management of maxillofacial, upper-airway and non-bony neck trauma.
EPIDEMIOLOGY
Maxillofacial trauma occurs most frequently in the 20–25 years age group, decreasing in frequency either side of this age group. It is three to five times more likely to occur in males than in females. Blunt injury is by far the commonest mechanism, accounting for nearly 97% of all maxillofacial injuries.4 Motor vehicle accidents (MVAs) account for nearly three-quarters of blunt injuries, with falls, physical assault, contact sports and industrial accidents accounting for the remainder. Legislative changes and preventative measures involving drink-driving, seatbelt and airbag use have seen a reduction in the incidence of MVA-related maxillofacial injury.5,6 In multiple trauma patients with an injury severity score (ISS) > 12, maxillofacial injury occurs in up to 17%, with a corresponding mortality rate of 13%.4
ANATOMICAL ASPECTS
Fractures, haemorrhage, soft-tissue damage and oedema are the commonest manifestations of blunt facial trauma. The severity of facial injury is directly related to the velocity of force applied.7 Common fractures of facial bones are maxilla (23%), orbital region (22%), zygoma (16%), nasal bones (15%), mandible (13%), teeth (8%), alveolar ridge (2%) and temporomandibular joint (TMJ) 1%.4
MANDIBULAR FRACTURES
The mandible is a unique, horseshoe-shaped bone that is tubular and weakest where the cortices are thinnest; most fractures occur at vulnerable points, regardless of the point of impact.8 Common sites are the ramus (condylar neck and angle of the mandible) and body at the level of the first or second molar. Multiple fractures are common (64%),8 with body of mandible fractures often being accompanied by fractures of the opposite angle or neck, due to transmitted forces. Mandibular fragments are often distracted due to the action of the lower jaw muscles. Respiratory obstruction may occur after bilateral mandibular angle or body fractures due to the posterior displacement of the tongue – the ‘Andy Gump’ fracture.9,10
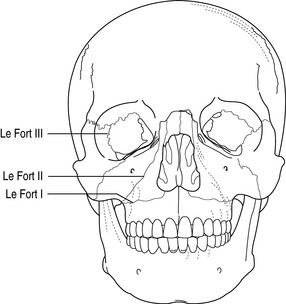
MIDFACIAL FRACTURES
The bones of the middle third of the face are relatively thin and poorly reinforced. Fracture dislocations occur through the bones and suture lines and the facial skeleton acts as a compressible energy-absorbing mass that gives on impact. The series of compartments (nasal cavity, paranasal sinuses and orbits) within the bony framework collapse progressively, absorbing energy and protecting the brain, spinal cord and other vital structures.11 Multiple complex facial fractures usually result and isolated facial bone fractures are rare. Le Fort described three great lines of weakness in the facial skeleton and thus derived the Le Fort classification of fractures12 (Figure 68.1). Le Fort fractures are perpendicular to the three main vertical buttresses of the facial skeleton – the nasomaxillary, zygomaticomaxillary and pterygomaxillary ‘pillars’. Le Fort fractures rarely occur in their pure form with mixed patterns prevailing (e.g. right hemifacial Le Fort I and left hemifacial Le Fort II). Airway obstruction from posterior movement of the soft palate against the tongue and the posterior pharyngeal wall may occur. Oral secretions, blood, bone and tooth debris and pharyngeal wall haematomas may worsen airway compromise.
LE FORT I (ALSO KNOWN AS GUERIN’S FRACTURE)
This fracture involves only the maxilla at the level of the nasal fossa. It follows a horizontal plane at the level of the nose. The fracture separates the palate from theremainder of the facial skeleton (i.e. palate–facial disjunction) and is usually caused by direct low-maxillary blows or by a lateral blow to the maxilla.
LE FORT II
This is the most common midface fracture.13 The maxilla, nasal bones and medial aspect of the orbit are involved which results in a freely mobile, pyramidal-shaped portion of the maxilla (i.e. pyramidal disjunction). The fracture line extends from the lower nasal bridge through the medial wall of the orbit, and crosses the zygomaticomaxillary process. It is caused by direct blows to the mid-alveolar area, or by lateral impacts and inferior blows to the mandible when the mouth is closed.
LE FORT III
This is known as craniofacial disjunction because the fracture line runs parallel to the base of the skull, separating the midfacial skeleton from the cranium. The fracture extends through the upper nasal bridge and most of the orbit and across the zygomatic arch. It involves the ethmoid bone, and thus may transect the cribriform plate at the base of the skull.13,14 These fractures result from superiorly directed blows to the nasal bones.13
TEMPOROMANDIBULAR JOINT
Mechanical TMJ impairment may result from condylar or zygomatic arch fractures and can prevent jaw opening even after muscle relaxants have been administered.15
ZYGOMATIC, ORBITAL AND NASAL FRACTURES
Zygomatic fractures are uncommon, but its attachments to the maxilla, frontal and temporal bones are vulnerable and may be disrupted. When the zygoma is displaced, disruption of the lateral wall and floor of the orbit may ensue. Orbital injury is commonly associated with midface trauma. The severity of injury in the orbital region varies from oedema and ecchymosis of the periosteal soft tissue to subconjunctival haemorrhage and loss of visual acuity or ocular rupture. Blinding injuries reported with facial fractures occur in 3–12% and most are secondary to globe perforation rather than optic nerve injury.16 Orbital blowout fractures occur when pressure is directly applied to the eye, and is hydraulically transmitted via the globe to the interior bony structures. The weaker inferior wall usually fractures, causing enophthalmos, diplopia, impaired eye movement and infraorbital hypoaesthesia. Nasal fractures are common, with epistaxis and septal haematoma being the prime concerns.
HAEMORRHAGE
Haemorrhage following blunt maxillofacial injury is extremely common. Life-threatening bleeding is fortunately rare. Various series have reported the incidence to be between 1 and 10%.1,17–19 Most severe haemorrhage is associated with midfacial fractures although soft-tissue lacerations alone can cause significant blood loss. Swallowing of large quantities of blood may conceal haemorrhage and predispose to aspiration.20
The origin of bleeding in facial trauma is complicated, as the vascular supply is derived from both the internal and external carotid arteries, with anastomoses occurring between them as well as between both halves of the face. The internal maxillary artery, especially the intraosseous branches, is the main source of bleeding in facial injury, because the artery passes within the common Le Fort fracture borders.16 The comminuted nature of maxillary fractures makes the detection of an exact site of vessel damage nearly impossible.16 Branches of the internal carotid artery such as the lacrimal and zygomatic branches, as well as the anterior and posterior ethmoidal arteries, may contribute to bleeding.
ASSOCIATED INJURIES
Basilar skull fracture
The anterior cranial fossa is often involved in craniofacial injuries. Fractures involving the frontal bone, frontal sinus, nasoethmoid complex or fronto-orbital complex result in bone defects in the skull base and can cause dural tears with resultant leakage of cerebrospinal fluid (CSF). CSF fistulae occur in 10–30% of basilar skull fractures.21 The clinical finding of CSF rhinorrhoea is not diagnosticfor anterior cranial fossa lesions, as this represents only the site of exiting CSF. The origin may be from a temporal bone fracture, because CSF from the middle ear discharges into the nose via the Eustachian tube. A middle cranial fossa defect can produce rhinorrhoea through the sphenoid sinus. The vast majority of fistulae present within 1 week of injury. Meningitis in patients with midface fractures is uncommon, despite the fact that approximately 36% of patients sustaining Le Fort fractures with anterior cranial fossa fractures have CSF leaks.22,23
Head and cervical spine injury
The incidence of head injury in those with maxillofacial trauma has been variably reported to be between 15% for severe head injury, increasing to 80% if all grades of head injuries are included.1,4,24 Cervical spine injury has been reported in up to 11% of patients.
The association between maxillofacial and cervical spine injury depends on the mechanism of injury. Falls and motor vehicle accident victims are more likely to have cervical injury than sporting or personal assault victims.25 Cervical spine fracture occurs with mandibular injury in 3%16 and is attributed to forces exerted directly or indirectly from the facial skeleton to the neck. C1/C2 and C5–C7 are at particular risk.
Other injuries
Thoracic (9–40%) and abdominal (5–40%) trauma and limb fractures (30%) are other common coexistent injuries.24,26 Traumatic occlusion of the internal carotid artery (ICA) is a rare complication of maxillofacial trauma occurring in less than 0.5% of patients presenting with blunt maxillofacial injury.27,28 It is usually recognised when a patient develops an unexplained neurological deficit, most often hemiplegia, subsequent to trauma or surgery of the head, face or neck. Assessment of the carotid circulation by CT angiography is a useful investigation if carotid injury is suspected.
ASSESSMENT OF INJURY
INVESTIGATION
Radiographic studies include a posterior–anterior, lateral oblique, stereo Water’s view, stereo Caldwell’s view and Panorex views. However, use of CT scanning, especially with the three-dimensional reconstructive ability, is now the preferred and most accurate method of imaging. In addition to bony distortion, fluid in the paranasal sinuses, optic nerve integrity and soft-tissue distortion, the brain, upper cervical spine and other body areas can be visualised concurrently. Other investigations such as colour Doppler ultrasound studies, CT angiography or standard angiography of the great vessels in the neck may be required in cases of possible carotid dissection or carotido-cavernous fistulae. Nasal discharge should be tested to determine the presence of a CSF fistula. Assay for β-2 transferrin is more valuable than the traditional glucose assay for CSF leak detection.29
AIRWAY MANAGEMENT
Airway management in maxillofacial injury is potentially complex due to multiple concurrent compromising factors (Table 68.1).
| General problems | Management |
| Haemorrhage/debris | Suction, volume replacement |
| Impaired laryngoscopy | Head down |
| Aspiration risk from blood swallowing | Definitive control of haemorrhage (see text) |
| Clot inhalation/obstruction | |
| Teeth, bone fragments | |
| Oedema soft tissue haematomas | Monitor airway closely |
| Increases over 48 hours | Head up 30° |
| Mask fit can be poor | Maintain spontaneous ventilation during airway manipulation; laryngeal mask ventilation |
| Specific problems | |
| Bilateral mandibular body/angle fractures | Anterior traction on tongue or jaw, towel clip or suture through tongue and elevate |
| Posterior displacement of tongue | |
| TMJ impairment | |
| Mandibular condyle, zygomatic arch | Nasotracheal intubation (blind/fibreoptic) or surgical airway may be required (see text) |
| Mouth opening limited | |
| Midfacial fracture | |
| Mask seal poor | Anterior traction on mobile segment |
| Soft palate collapses against pharynx | |
| Basilar skull | |
| Nasotracheal intubation contraindicated | Avoid nasal intubation |
| Pneumocephalus from mask ventilation | |
| Cervical spine injury | Orotracheal intubation with in-line stabilisation; fibreoptic intubation; surgical airway |
IMMEDIATE PRIORITIES
Occasionally, patients may assume positions that lessen airway obstruction (e.g. sitting forward or even prone).30 Simple measures such as suction and clearing the airway and insertion of an oropharyngeal airway may suffice.
In midfacial injuries, anterior digital traction on the mobile mid-segment may relieve obstruction. In bilateral mandibular fractures of the angle or body, a towel clip or suture through the tongue may allow anterior traction on the unsupported tongue and relieve obstruction.
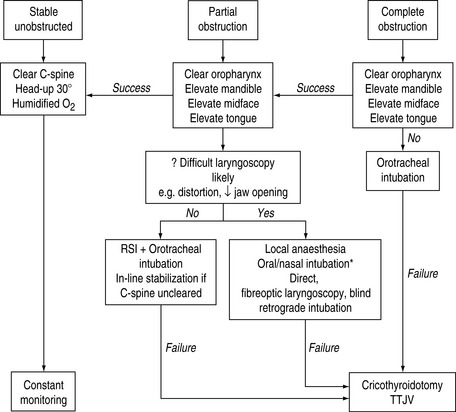
TECHNIQUES (Figure 68.2)
Analgesia can be achieved with a combination of sprayed or nebulised lidocaine (4%) to the posterior pharynx as well as a transcricoid injection of 2–4 ml lidocaine (2%). Adjunctive superior laryngeal and glossopharyngeal nerve blocks can be used.31,32 The orotracheal route for intubation is the route of choice in the presence of basal skull fracture.
If cervical spine injury is present or suspected, in-line stabilisation is mandatory. A variety of intubation techniques can be used – for example, direct laryngoscopy, fibreoptic guided laryngoscopy (oral/nasal), use of a light wand stylet, blind nasal and retrograde intubation techniques.33,34 The operator should use the technique with which he/she is most comfortable. Excessive bleeding may render fibreoptic techniques useless.
Failure to intubate in the presence of airway obstruction necessitates emergency cricothyroidotomy. Tracheostomy may be required in those likely to need prolonged ventilatory support (e.g. multiple facial fractures combined with a head injury), and is best performed as a semi-elective procedure in the operating room.16
MANAGEMENT OF HAEMORRHAGE
Topical vasoconstrictors may not be effective with ongoing nasal haemorrhage. Anterior nasopharyngeal packs are sometimes effective at reducing blood loss. Foley catheters passed into the posterior nasopharynx with the balloons filled with air may stem blood loss, especially if anterior traction is applied.20 Plastic or maxillofacial surgical opinion should be sought regarding operative reduction and stabilisation of fractures and direct ligation of bleeding vessels if haemorrhage is persistent. External carotid ligation and angiographic embolisation can be used as a last resort.
DEFINITIVE MANAGEMENT
Definitive surgery is generally delayed 4–10 days to allow swelling to subside. The timing of surgery may be further delayed if a severe head injury coexists. Early surgery may be warranted if orbital injury with optic nerve compromise is present. The use of high dose steroids in optic nerve compression is controversial and good data do not exist regarding its efficacy.16 Irrigation and debridement of open wounds, closure of facial lacerations and removal of foreign bodies must be undertaken as soon as is practicable, preferably within 24 hours.
The use of prophylactic antibiotics in the presence of basilar skull fracture and CSF leak is controversial and local protocols should be followed.21 Persistent CSF leaks (> 2 weeks) or those complicated by meningitis or pneumocephalus are repaired surgically.21 Appropriate tetanus prophylaxis must be given.
The use of modern internal fixation techniques have reduced the need for intermaxillary fixation following elective facial fracture repair, with only unstable comminuted fractures requiring this form of fixation. Submental intubation during fracture repair is now being used as an alternative to tracheostomy.35
INJURIES TO THE LARYNX AND TRACHEA
Direct trauma to the airway is rare, accounting for less than 1% of traumatic injury seen in most major centres.15,36 The bony protection afforded to the airway by the sternum and mandible and death from asphyxia at the accident scene account for the rarity of the injury. Laryngotracheal injury can be classified as blunt or penetrating. Failure to recognise these injuries, their complications and specific pitfalls in airway management can lead to death.37,38
MECHANISM OF INJURY
BLUNT INJURY
Common causes include motor vehicle accidents where the extended neck impacts with the steering wheel or dashboard. The ‘clothesline injury’ occurs when a cyclist or horse rider collides with a cable or wire causing direct injury to the upper airway. Assaults and strangulation account for the remainder of blunt injuries. Direct blows are more likely to injure the cartilages of the larynx while flexion/extension injuries are most commonly associated with tracheal tears and laryngotracheal transection.37 The larynx above the cricoid cartilage is injured in 35%, manifesting as oedema, contusions, haematomas, lacerations, avulsion and fracture dislocation, most commonly of the thyroid and arytenoid cartilages.
The cricoid cartilage itself is injured in 15%, which may cause recurrent laryngeal nerve dysfunction.36 The cervical trachea is injured in 45%.38 Tracheal transection most often occurs at the junction between the cricoid cartilage and trachea.39 Oedema fluid and air dissecting within submucosal layers of the larynx and trachea may causeairway obstruction. Air in the soft tissues can cause epiglottic emphysema and narrowing of the supraglottic airway.40 Straining, talking and coughing may worsen the oedema.
PENETRATING INJURY
Penetrating injuries usually result from stab or gunshot wounds. The anterior triangle of the neck is the most common site of entry. The cervical trachea is most commonly involved in stab wounds. The larynx is injured in about one-third of those with upper-airway injuries.38
ASSOCIATED INJURIES
Common associations with blunt laryngotracheal injury include cervical spine, head injury and multisystem trauma. Of those with penetrating neck trauma, major vascular injuries (carotid, jugular, subclavian, vertebral arteries) occur in 25–50%, pharyngeal or oesophageal injury in 30%, neural injury (spinal cord, brachial plexus) in 12% and apical thoracic injury in 10%.7
ASSESSMENT OF INJURY
Definitive investigation and management depend on the airway status and presence of associated injury. The degree of injury is not readily assessable on the basis of any one clinical symptom or sign (Table 68.2) and delayed diagnosis is common. Plain radiography (CXR, cervical spine) is performed in all cases. CT scanning demonstrates fractures of cartilages, haematomas and other injuries and is used in stable patients with laryngeal tenderness, endolaryngeal oedema and small haematomas. When obvious signs of injury are not present and there is a satisfactory airway, fibreoptic laryngotracheoscopy under local anaesthesia can demonstrate vocal cord dysfunction, integrity of the cartilaginous framework and laryngeal mucosa. Rigid laryngoscopy can be used when adequate visualisation is not achieved with the former. Pharyngo-oesophagoscopy, contrast studies, open exploration and angiography may be required to exclude aerodigestive tract and major vascular injuries.
| Symptoms |
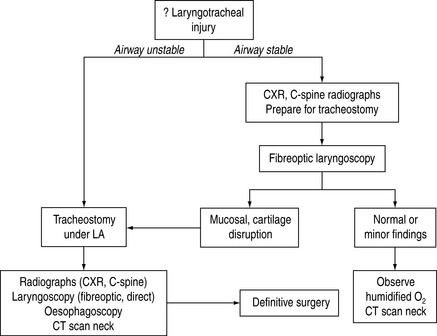
AIRWAY MANAGEMENT
Major complications from airway manipulation can occur after laryngotracheal trauma. Blind intubation can lead to complete airway obstruction due to creation of false passages and mucosal disruption.15 Cricoid pressure can lead to laryngotracheal separation and is contraindicated. Positive pressure ventilation can rapidly worsen air leaks and wherever possible the patient should maintain spontaneous respiration until a tube has been placed distal to the site of injury. Cricothyroidotomy is not recommended as it may compound laryngeal injury. Gaping airway wounds can be intubated under direct vision pending subsequent surgery.38 The optimal mode of intubation is thus tracheostomy under local anaesthesia (Figure 68.3). Excessive movement of the cervical spine during airway manipulation should be avoided in cases of blunt trauma.
1 Gwyn PP, Carraway JH, Horton CE. Facial fractures: associated injuries and complications. Plast Reconstr Surg. 1971;47:225-230.
2 Tung T, Tseng WS, Chen CT, et al. Acute life threatening injuries in facial trauma patients. A review of 1025 patients. J Trauma. 2000;49:420-424.
3 Luce EA, Tubb TD, Moore AM. Review of 1000 major facial fractures and associated injuries. Plast Reconstr Surg. 1979;63:26-30.
4 Hogg NJ, Stewart TC, Armstrong JE, et al. Epidemiology of maxillofacial injuries at trauma hospitals in Ontario, Canada, between 1992 and 1997. J Trauma. 2000;49:425-432.
5 Telfer MR, Jones GM, Shepherd JP. Trends in the aetiology of maxillofacial fractures in the United Kingdom (1977–1997). Br J Oral Maxillofac Surg. 1991;29:250-255.
6 Hussain KW, Wijetunge DB, Grubnic S, et al. A comprehensive analysis of craniofacial trauma. J Trauma. 1994;36:34-37.
7 Miller RH, Duplechain JK. Penetrating wounds of the neck. Otolaryngol Clin North Am. 1991;24:15-29.
8 Halazonetis JA. The weak regions of the mandible. Br J Oral Surg. 1968;6:37-48.
9 Bavitz JB, Collicott PE. Bilateral mandibular fractures contributing to airway obstruction. Int J Oral Maxillofac Surg. 1995;24:273-275.
10 Seshul MB, Sinn DP, Gerlock AJJr. The Andy Gump fracture of the mandible: a cause of respiratory obstruction or distress. J Trauma. 1978;18:611-612.
11 Wenig BL. Management of panfacial fractures. Otolaryngol Clin North Am. 1991;24:93-101.
12 Le Fort R. Experimental study of fractures of the upper jaw. Rev Chir Paris. 1901;23:208-227. 360–79 (Reprinted in Plast Reconstr Surg 1972; 50: 497–506)
13 Manson PN, Hoopes JE, Su CT. Structural pillars of the facial skeleton: an approach to the management of Le Fort fractures. Plast Recontr Surg. 1980;66:54-61.
14 Cruise CW, Blevins PK, Luce EA. Naso-ethmoidal-orbital fractures. J Trauma. 1980;20:551-556.
15 Crosby R. The difficult airway 2. Anesthesiol Clin North Am. 1997;13:495-749.
16 Ardekian L, Rosen D, Peled M, et al. Life-threatening complications and irreversible damage following maxillofacial trauma. Injury. 1998;29:253-256.
17 Ardekian L, Samet N, Shoshani Y. Life threatening bleeding following maxillofacial trauma. J Cranio-Maxillofac Surg. 1993;21:336-340.
18 Thaller SR, Beal SL. Maxillofacial trauma: a potentially fatal injury. Ann Plastic Surg. 1991;27:281-290.
19 Buchanan RT, Holtmann B. Severe epistaxis in facial fractures. Plast Reconstr Surg. 1983;71:768-790.
20 Murakami WT, Davidson TM, Marshall LF. Fatal epistaxis and craniofacial trauma. J Trauma. 1983;23:57-61.
21 Marentette LJ, Valentino J. Traumatic anterior fossa cerebrospinal fluid fistulae and craniofacial considerations. Otolaryngol Clin North Am. 1991;24:151-163.
22 Maxwell JA, Goldware SI. Use of adhesive in surgical treatment of cerebrospinal fluid leaks. J Neurosurg. 1973;39:322-336.
23 Laun A. Traumatic cerebrospinal fluid fistulae in the anterior and middle cranial fossae. Acta Neurochir. 1982;84:215-222.
24 Adams C, Januszkiewicz J, Judson J. Changing patterns of severe craniomaxillofacial trauma in Auckland over eight years. Aust N Z J Surg. 2000;70:401-404.
25 Davidson JSD, Birdsell BD. Cervical spine injury in patients with skeletal trauma. J Trauma. 1989;29:1276-1278.
26 Schultz RC, Oldham RJ. An overview of facial injuries. Surg Clin North Am. 1977;57:987-1010.
27 Punjabi AP, Plaisier BR, Haug RH, et al. Diagnosis and management of blunt carotid artery injury in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1997;55:1388-1395.
28 Marciani RD, Israel S. Diagnosis of blunt carotid artery injuries in patients with facial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:5-9.
29 Skedros DG, Cass SP, Hirsch BE, et al. Beta-2 transferrin assay in clinical management of cerebral spinal fluid and perilymphatic fluid leaks. J Otolaryngol. 1993;22:341-344.
30 Neal MR, Groves J, Gell IR. Awake fibreoptic intubation in the semi-prone position following facial trauma. Anaesthesia. 1996;51:1053-1054.
31 Webb AR, Fernando SS, Dalton HR, et al. Local anaesthesia for fibreoptic bronchoscopy: transcricoid injection or the spray as you go technique. Thorax. 1990;45:474-477.
32 Gotta AW, Sullivan CA. Superior laryngeal nerve block: an aid to intubating the patient with a fractured mandible. J Trauma. 1984;24:83-85.
33 King H, Huntington C, Wooten D. Translaryngeal guided intubation in an uncooperative patient withmaxillofacial injury: a case report. J Trauma. 1994;36:885-886.
34 Verdile VP, Chang JL, Bedger R. Nasotracheal intubation using a flexible lighted stylet. Ann Emerg Med. 1990;19:506-510.
35 Chandu A, Smith ACH, Gebert R. Submental intubation: an alternative to short-term tracheostomy. Anaesth Intensive Care. 2000;28:193-195.
36 Gussack GS, Jurkovich GJ, Luterman F. Laryngotracheal trauma: a protocol approach to a rare injury. Laryngoscope. 1986;96:660-665.
37 Mathison DJ, Grillo H. Laryngotracheal trauma. Ann Thorac Surg. 1987;43:254-263.
38 Cicala RS, Kudsk KA, Butts A, et al. Initial evaluation and management of upper airway injuries in trauma patients. J Clin Anesth. 1991;3:91-98.
39 Trone TH, Schaefer SD, Carder HM. Blunt and penetrating laryngeal trauma: a 13 year review. Otolaryngol Head Neck Surg. 1980;88:257-261.
40 Sacco JJ, Halliday DW. Submucosa epiglottic emphysema complicating bronchial rupture. Anesthesiology. 1987;66:555-557.