96
Mastocytosis
• Spectrum of disorders caused by proliferation and accumulation of mast cells in the skin and/or other tissues (Table 96.1).
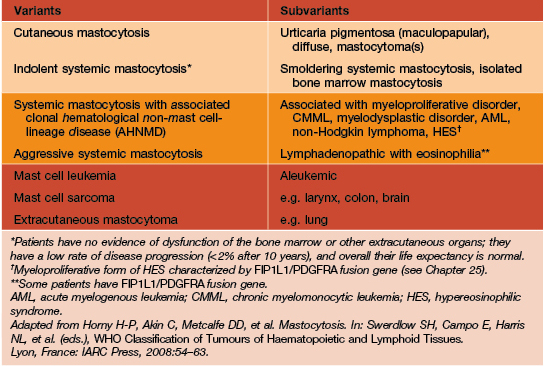
Table 96.1
WHO classification of mastocytosis.
Patients with disorders in the bottom two rows usually do not have cutaneous lesions.
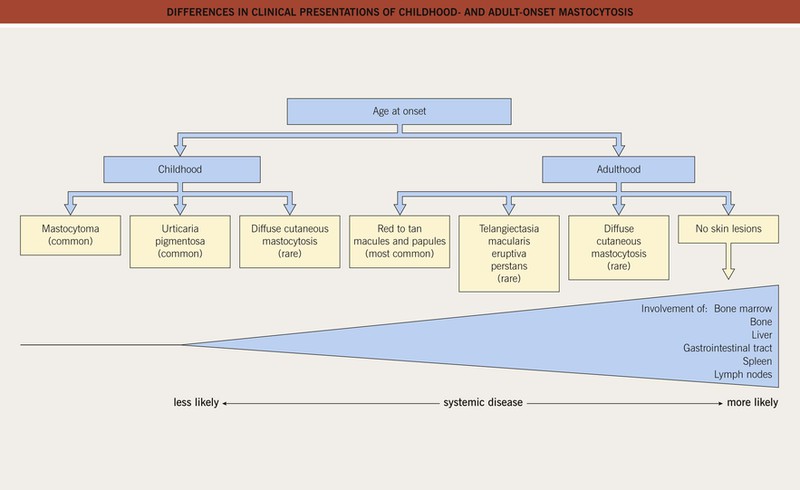
• Childhood-onset mastocytosis generally has a benign course with spontaneous remission prior to puberty, whereas adult-onset mastocytosis typically persists and may be associated with systemic involvement (Fig. 96.1).
Clinical Features of Cutaneous Mastocytosis
• Firmly rubbing or stroking cutaneous lesions of mastocytosis often causes urtication (Darier’s sign) (Fig. 96.2); this is generally more pronounced in children.


Fig. 96.2 Darier’s sign in mastocytosis. An infant with extensive cutaneous involvement (A) and an adult with macular and papular lesions (B). A, Courtesy, Julie V. Schaffer, MD; B, Courtesy, Thomas Horn, MD.
• In approximately half of patients, hiving develops after stroking clinically uninvolved skin (dermatographism).
Mastocytomas (Solitary or Multiple)
• Typically present at birth or appear during infancy.
• One to several papules, nodules, or plaques with a yellow-tan to red-brown color and leathery (peau d’orange) texture (Fig. 96.3).

Fig. 96.3 Mastocytoma in an infant. Note the leathery appearance of the skin and the two erosions. Courtesy, Michael Tharp, MD.
• Can occur anywhere on the skin surface, including acral sites.
Urticaria Pigmentosa (UP; Maculopapular or Plaque-Type Cutaneous Mastocytosis)
• Occurs in children and adults.
• Multiple (often numerous) pink-tan to red-brown macules, papules, and/or (particularly in infants/young children) plaques (Fig. 96.4).



Fig. 96.4 Urticaria pigmentosa. Papular (A) and papulonodular (B) lesions can be seen in children. The degree of associated hyperpigmentation as well as the size of the lesions varies. C Adult urticaria pigmentosa typically presents with small, red-brown macules and papules. A, Courtesy Julie V. Schaffer, MD; B, C, Courtesy, Michael Tharp, MD.
• Hyperpigmentation is less prominent in patients with lightly colored skin.
• Favors the trunk and proximal extremities, usually sparing the central face, palms, and soles.
Diffuse Cutaneous Mastocytosis
• Occurs primarily in infants, with rare reports in adults.
• Flushing, blistering, and erosions are common (Fig. 96.5).


Fig. 96.5 Diffuse cutaneous mastocytosis in infants. A Diffuse infiltration with multiple erosions. B Spontaneous blister superimposed on a plaque; note the leathery appearance of the lesions on the shin.
• DDx: epidermolysis bullosa, autoimmune bullous dermatoses.
Telangiectasia Macularis Eruptiva Perstans (TMEP)
• Rare variant that occurs primarily in adults.
• Telangiectatic macules and patches without significant hyperpigmentation (Fig. 96.6).

Fig. 96.6 Telangiectasia macularis eruptiva perstans. Multiple lesions composed of telangiectasias are present.
• Lower density of mast cells than other forms of mastocytosis, so Darier’s sign may not be present.
• DDx: photodamage, poikiloderma, multiple spider telangiectasias (e.g. in the setting of cirrhosis) and other telangiectatic conditions (see Chapter 87).
Systemic Manifestations of Mastocytosis
• In patients with a higher mast cell burden (e.g. extensive cutaneous disease, a large mastocytoma, extracutaneous involvement), release of mast cell mediators such as histamine can lead to systemic symptoms, which range from flushing to abdominal pain and diarrhea to lightheadedness and syncope (Fig. 96.7).
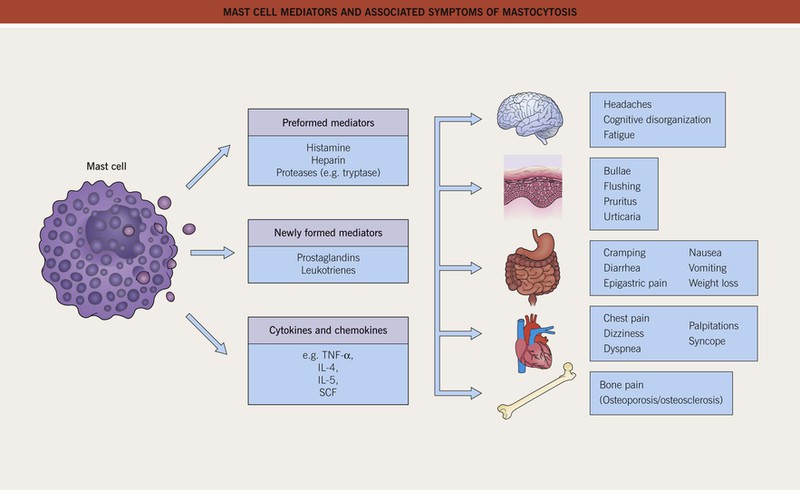
Fig. 96.7 Mast cell mediators and associated symptoms of mastocytosis. SCF, stem cell factor (binds to KIT receptor).
• Although the bone marrow is frequently involved in adult patients with cutaneous mastocytosis, hematologic sequelae are uncommon (see Table 96.1).
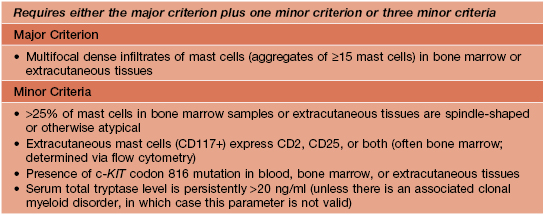
• Criteria for the diagnosis of systemic mastocytosis are presented in Table 96.2.
Evaluation and Treatment
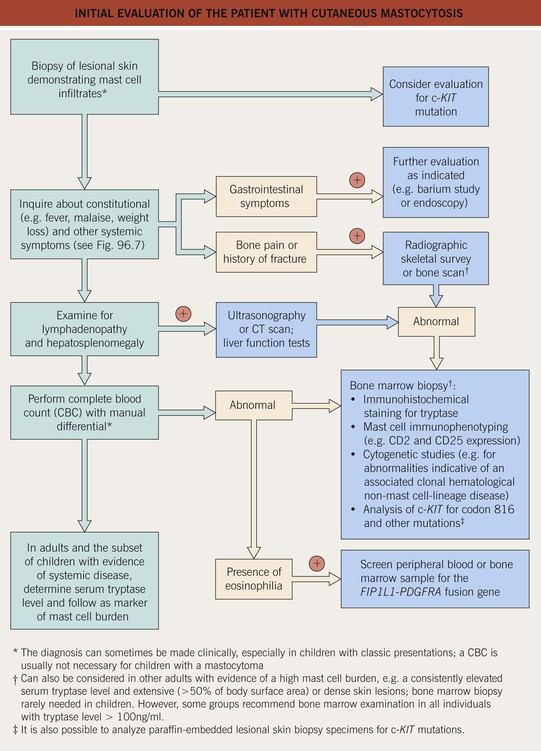
• An approach to the evaluation of a patient with cutaneous mastocytosis is presented in Fig. 96.8.
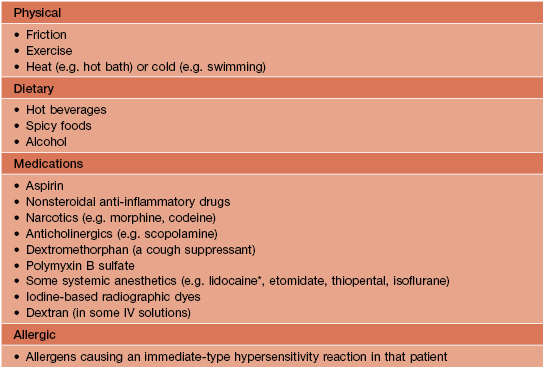
• Triggers of mast cell degranulation (Table 96.3) should be avoided when possible.
• An Epipen® or Epipen Jr® for emergency use can be given to patients with a high mast cell burden.
For further information see Ch. 118. From Dermatology, Third Edition.