Chapter 200 Management of Ulnar Nerve Compression
The ulnar nerve arises from the medial cord of the brachial plexus and innervates the muscles of both the forearm and parts of the hand. It also carries sensory neurons supplying the skin of the back of the forearm, the palm, and the fourth and fifth digits. Entrapment of the ulnar nerve at the elbow is the second most common neuropathy in adults, after entrapment of the median nerve at the carpal tunnel.1–3
History
Before surgical options were explored, conservative treatments employed included hydrotherapy, immobilization,4 electrotherapy/application of electric current,5,6 massage, and application of ointments and solutions.7 In 1818, Granger8 described a patient with ulnar palsy after fracture of the medial condyle of the humerus and advised nonsurgical management with anatomic repositioning and immobilization. The earliest known report of surgical treatment of ulnar nerve entrapment dates to 1816 when Henry Earle (1789–1838)5,9 attempted to alleviate pain caused by ulnar entrapment in a 14-year-old girl by nerve sectioning.
In the Archives Générales de Médecine,10 in 1878, Photinos Panas was the first to describe the relationship between ulnar nerve compression at the elbow and clinical ulnar nerve palsy, what has been called “tardy ulnar palsy.” He presented three cases in which either prior trauma or osteoarthritis gradually caused damage to the ulnar nerve and eventually clinical manifestations. The term tardy was applied to this scenario where deficits appeared late after an injury. Panas attempted to improve the “bed” for the ulnar nerve by deepening the epicondylar groove.
In 1888, Poncet11 performed the first definitive surgical treatment for a subluxed ulnar nerve by creating a groove or a sulcus in the bone, placed the ulnar nerve in it, and then sutured the periosteum over the nerve to create a roof over the tunnel. Benjamin Farquhar Curtis(1857–1924)12 in 1898 developed the technique that is known today as the anterior subcutaneous transposition.5 Albert Mouchet (1869–1963)13 in 1914, described ulnar neuropathy secondary to a fracture of the humerus (maladie de Mouchet), and developed the technique of supracondylar cuneiform osteotomy of the humerus for ulnar neuritis from cubitus valgus. Rudolf Klauser in 1917 described a technique of transposing the nerve in a muscular bed to prevent repetitive direct trauma to the relatively superficially placed nerve from a simple subcutaneous transposition and was the first to describe anterior “intramuscular” transposition.14 Decompression or “liberation” of the ulnar nerve (without transposition) was first suggested by Sir Edward Farquhar Buzzard, a British physician in the year 1922. In 1942, James Rögnvald Learmonth15 described the anterior “submuscular” transposition placing it deep to the flexor pronator group of muscles alongside the median nerve.16 Feindel and Stratford defined the cubital tunnel anatomically in 1958.17,18
In 1959, Geoffrey Vaughan Osborne19 postulated that a fibrous band bridging the two heads of the flexor carpi ulnaris and directly laying over the ulnar nerve may be responsible for compressing the ulnar nerve leading to ulnar neuritis rather than by the previously postulated friction or traction on nerve. This fibrous band later came to be known as “Osborne’s band.”5 King and Morgan20 proposed medial epicondylectomy as another surgical option for the treatment of this problem.
Anatomy
Arm
The ulnar nerve descends in the arm posterior to the pectoralis major muscle and medial or posteromedial to the brachial artery. At the inferior border of the pectoralis major, the nerve moves medially and pierces the medial intermuscular septum about 8 cm above the medial epicondyle. It descends medially on the anterior surface of the medial head of the triceps muscle and then enters the interval between the medial epicondyle of the humerus and the olecranon. As it descends the nerve is usually invested by some triceps fibers that are given the name “Struther’s arcade.”21–23 The arcade, located about 8 cm proximal to the medial epicondyle is a musculofascial band and is about 1.5 to 2 cm wide. Its anterior border is the medial intermuscular septum, and its lateral border is formed by the deep fibers of the medial head of the triceps. The arcade typically passes obliquely and superficial to the nerve. The Struthers’ arcade should not be confused with “Struthers’ ligament,” a rare finding that bridges the supracondylar spur on the medial aspect of the humerus to the junction of the medial epicondylar ridge and medial epicondyle.24 Struthers’ ligament is usually associated with compression of the median nerve.
Cubital Tunnel
The nerve passes into the ulnar groove on the dorsal aspect of the medial epicondyle, at the entrance to the so-called cubital tunnel, the term first coined by Feindel and Stratford in 1958.5,17,18
The nerve is most superficial here during its entire course down the length of the arm. Laying over a bony floor it is therefore most susceptible to trauma in this location. The nerve is surrounded by fat throughout the cubital tunnel except adjacent to the medial epicondyle. The roof of the cubital tunnel is formed by a fibrous aponeurosis that thickens to form the cubital tunnel retinaculum or the arcuate ligament of Osborne25 (also called triangular ligament, arcuate ligament, or humero-ulnar arch or humero-ulnar arcade/HUA) which connects the tendinous origin of the humeral and ulnar heads of the flexor carpi ulnaris. This fibrous band is approximately 4 mm wide and extends from the medial epicondyle to the tip of the olecranon. Its fibers are oriented transversely and are taut in elbow flexion. The walls of the cubital tunnel are formed by the medial epicondyle and the olecranon and the floor is formed by the medial collateral ligaments and the joint capsule. The proximal and mid-portions of the cubital tunnel alter with flexion from round to elliptical.1,26 Studies show that the pressure within the cubital tunnel rises up to 7-fold with elbow flexion and further up to 20-fold with contraction of the flexor carpi ulnaris muscle causing microvascular ischemia and pressure injury to the nerve.27 As it traverses through the cubital tunnel, the ulnar nerve passes from the extensor surface of the arm to the flexor surface of the forearm and the nerve gives off branches to the elbow joint. Anatomical and vascularization pattern studies demonstrate a consistent but segmental extraneural and intraneural vascular supply from the superior ulnar collateral, inferior ulnar collateral and posterior ulnar recurrent arteries. The inferior ulnar collateral artery which is typically sacrificed with ulnar nerve transposition procedures provides the only direct vascularization to the nerve in the region just proximal to the cubital tunnel.28
Wrist
Approximately 9 cm proximal to the wrist the ulnar nerve gives off the dorsal cutaneous sensory branch leaving the terminal motor and palmar sensory branches to traverse the wrist into the hand. The dorsal cutaneous nerve passes posteriorly, deep to the tendon of the flexor carpi ulnaris, pierces the deep fascia, and continues distally along the dorsomedial side of the wrist. It supplies sensation to the dorsal surface of the ulnar innervated fingers, that is, the fifth digit and medial half of the fourth digit. The remainder of the ulnar nerve continues into the wrist, traveling with the ulnar artery and vein as it passes lateral to the pisiform bone. Guyon’s canal, named after French surgeon Jean Casimir Félix Guyon (1831–1920), and also known as the ulnar canal or ulnar tunnel, is a space at the wrist between the pisiform bone and the hook of the hamate bone through which the ulnar artery and the ulnar nerve travel into the hand. In 1861, Guyon proposed that compression can occur in one of three zones. Zone 1 is in the most proximal portion of the canal, where the nerve is a single structure in one epineural sheath containing both motor and sensory fascicles. Zones 2 and 3 are further along the canal where the ulnar nerve has already bifurcated into motor and sensory branches. This lies just distal to the fibrous arch of the hypothenar muscles. The clinical picture will correlate with the zone in which compression is occurring.24 In some cases a fibrous arch overlying the motor branch of the ulnar nerve as it passes beneath the origin of the hypothenar muscles in Guyon’s canal is encountered. Awareness of this fibrous arch facilitates appropriate surgical management of ulnar-innervated intrinsic muscle weakness or wasting associated with ulnar compression at the wrist.24 In some cases a fibrous arch overlying the motor branch of the ulnar nerve as it passes beneath the origin of the hypothenar muscles in Guyon’s canal is encountered. Awareness of this fibrous arch facilitates appropriate surgical management of ulnar-innervated intrinsic muscle weakness or wasting associated with ulnar compression at the wrist.29
The nerve fibers cross beneath the pisohamate ligament and the fibrous arch of the hypothenar muscles. They then split off into sensory palmar digital nerves to the fifth and fourth digits, motor branches to the hypothenar muscles, deep branches to the interossei muscles, and a communicating branch to the median nerve. The ulnar nerve in the hand supplies motor function to the abductor digiti minimi, opponens digiti minimi, and flexor digiti minimi muscles of the fifth digit as well as the lumbricales III and IV. It also supplies the interossei, both dorsal and palmar, and finally the adductor pollicis and flexor pollicis brevis muscles.30
The sensory distribution of the nerve includes the palmar and dorsal medial aspects of the hand, including the fifth digit and half of the fourth digit. As the ulnar nerve crosses the extensor aspect of the elbow in a superficial site with little supporting epineurium, it is prone to injury after upper extremity trauma. The motor fibers that supply the intrinsic muscles of the hand occupy a more superficial location, and those that supply the flexor carpi ulnaris and ulnar half of the flexor digitorum profundus a deeper location. This fact is offered as an explanation of why intrinsic weakness of the hand muscles is a more often seen in patients with cubital tunnel syndrome. It then follows that as the sensory fibers are also located more superficially as the ulnar nerve traverses the extensor elbow, that paresthesias and sensory disturbances are the most common early features of cubital tunnel syndrome (Table 200-1).31
| MOTOR |
| Forearm, via the muscular branches of the ulnar nerve: |
Anatomic Variations
Numerous anatomic variations have been reported in the literature mainly between the median and the ulnar nerve in the forearm. The Martin-Gruber anastomosis is the most commonly encountered anatomical variation and was first described by the Swedish anatomist Martin32 in 1763 and later by Gruber33 in 1840. Here an anomalous neural pathway is seen in the proximal forearm where motor fibers from the median nerve cross over to the ulnar nerve. Another rare entity in the distal forearm, the Riche-Cannieu anomaly consists of the abnormal connection between the motor branch of the ulnar nerve and the recurrent motor branch of the median nerve.34
Etiology of Ulnar Nerve Compression
The ulnar nerve responds in a proportional manner by exhibiting increasingly altered intraneural microvascular blood flow, axonal transport and nerve function as the pressure exerted upon it increases.35 The main etiologies of ulnar nerve damage at the elbow joint are thought to be compression,17–1936 ischemia,1,37–40 traction,13,38,41 longitudinal strain, and friction.42 In previous studies25,43 increased cubital tunnel pressures up to 6 times have been reported with elbow flexion, wrist extension and shoulder abduction.1 Apfelberg in 1973 demonstrated that with elbow flexion, due to the increasing tension of the arcuate ligament and the bulging of the medial collateral ligament, there is change in the cross-sectional contour of the cubital tunnel from a smooth, round configuration to a flattened triangle, narrowing by approximately by 55%.1,17,40 Friction on the nerve may result from subluxation or dislocation of the nerve because of congenital or developmental laxity of the soft-tissue restraints that normally hold the ulnar nerve in its groove at the cubital tunnel.
Along its path around the elbow, five anatomic sites of potential entrapment/compression of the ulnar nerve exist.44 The Arcade of Struthers,22,24,45 the medial intermuscular septum,24 the cubital tunnel, the arcade of the flexor carpi ulnaris and the flexor-pronator aponeurosis have all been described. In the wrist, the motor branch of the ulnar nerve can also be compressed by the arch of origin of the adductor pollicis muscle. A well-defined band of tissue either at the point where the nerve crosses the third metacarpal or where it penetrates the adductor muscle46 can be found. Another potential site of ulnar compressive neuropathy, especially in cases of anterior dislocation of the nerve, is found as the nerve passes over the edge of the intermuscular septum. Compression can also develop as a postoperative complication of ulnar nerve transposition when the septum has not been excised or excised incompletely.
Constricting fascial bands, compression while under general anesthetic with inadequate padding, presence of an anomalous anconeus muscle (anomalous anconeus epitrochlearis muscle),47 a hypertrophied medial head of triceps as seen in some bodybuilders, ganglion cysts, subluxation of the ulnar nerve over the medial epicondyle,48 cubitus valgus, malunited supracondylar fracture, bony spurs and osteophytes, joint deformity in osteoarthritis or rheumatoid arthritis or gouty tophus,49 osteoarthritic or rheumatoid narrowing of the ulnar groove, constriction of the ulnar nerve as it passes behind the medial epicondyle causing frictional neuritis, medial epicondylitis (“golfer’s elbow”), tumors, postradiation,50 direct compression, repetitive strain, perineural adhesions, multiple intraneural hemangiomas,51 fractures, elbow dislocation, venepuncture, and severe hematoma are all additional described causes of ulnar neuropathy. Iatrogenic injuries to the nerve such as after total elbow replacement are also well described.52–54 Compression of the ulnar nerve in the ulnar groove is common in people who lean on their elbows, particularly in the flexed position (e.g., truck drivers leaning their arms on the edge of the window frame, people working on computers). Ulnar compressive neuropathy is also seen after suboptimal intraoperative padding to on the medial side of the arm and in patients confined to bed for acute55 or chronic illnesses.24 Chronic subluxation of the ulnar nerve in and out of the epicondylar groove, especially during extension and flexion of elbow, can result in friction neuritis and cause ulnar neuropathy.
The common causes of compression at the wrist at Guyon’s canal are repeated blunt trauma to the hypothenar region (e.g., bicycle riders) ganglionic cysts56 arising from the underlying carpus (usually from the triquetrohamate joint), lipoma,57 use of bilateral forearm crutches,58 vascular lesions,59 fractures of distal ulna or of carpal bones and fracture of the hook of the hamate.24
Diagnosis
Clinical Presentation
Cubital tunnel syndrome has been stratified by McGowan60 into three grades: grade I, sensory alteration only; grade II, muscle weakness/wasting of the interossei muscles; grade III, complete intrinsic muscle paralysis. Ulnar nerve palsy whether acute, subacute, or chronic, can cause wasting and weakness of the small muscles of the hand and partial clawing of the ring and little finger. The extent of the deformity and disability depends on the site of the lesion and the severity of the compression. Patients often have numbness and tingling along the fifth digit and the medial half of the fourth finger, often associated with a weakness of grip, and particularly when the patient rests on or flexes the elbow. Patients may experience pain and tenderness at the level of the cubital tunnel. The severity of pain is very variable and the distribution of pain may spread proximally and/or distally. Symptoms may be intermittent at first and then become more constant. Patients with chronic ulnar neuropathy may complain of loss of grip and pinch strength and loss of fine dexterity. Severe prolonged compression may present with intrinsic muscle wasting and clawing or abduction of the fifth digit at rest. The weakness is more pronounced in the intrinsic muscles of the hand than of the muscles of the forearm. This is due to the somatotopic organization of the fibers in the ulnar nerve. The motor fibers to the intrinsic muscles along with the sensory fascicles are situated more medially and more superficial therefore more likely to suffer physical trauma/friction or influence of compressive forces.61
Physical exam consists of a thorough inspection of the arm for any deformity, an abnormal mass and for any signs of a hyper mobile or subluxation of the ulnar nerve. On examination, the patient is asked to flex his/her elbow with full wrist extension for up to 3 minutes, and if this maneuver reproduces pain, numbness, or tingling symptoms, it can be considered a positive sign, analogous to Phalen’s test62 for carpal tunnel syndrome.
Froment’s sign may also be seen in the clinical examination of a patient with ulnar nerve entrapment. The patient holds a piece of paper between the thumb and the side of the adjacent index finger as the paper is pulled away. A patient with an ulnar nerve palsy will flex the thumb at the interphalangeal joint to try to keep hold of the paper due to the weakness of the adductor pollicis muscle.63
Imaging
The diagnosis of ulnar neuropathy is primarily associated with electrophysiologic testing and therefore routine imaging is not warranted. However in some cases plain x-rays, magnetic resonance imaging (MRI),64 computed tomography scan, or high-resolution ultrasonography65 at the elbow may be obtained to rule out an osteophyte, cyst, vascular anomaly, or any mass compressing the nerve. MRI with short tau inversion recovery (STIR) sequences, otherwise known as MR neurography,66,67 may show an increased signal in the nerve or denervation changes in the affected muscles. In ulnar entrapment at the elbow, however, electrophysiologic studies remain the gold standard for diagnosis.
Electromyography/Nerve Conduction Studies
The use of electrodiagnostic techniques to evaluate compression neuropathies was first described by Simpson68 in 1956. Preoperative electromyography (EMG) and nerve conduction velocities (NCVs) should be obtained on all patients. This information allows for confirmation of the entrapment as well as localization of the entrapment site. The test also serves to document the baseline conduction which can be especially useful to document recovery (or lack thereof) and for comparison for any future recurrence. Motor studies are more sensitive than mixed sensory studies at localizing ulnar neuropathy to the elbow.31,69
Recordings from the abductor digiti minimi and first dorsal interossei, which is the most distal muscle supplied by the ulnar nerve, give some of the most useful information to diagnose ulnar nerve entrapment.70–72 Measurements should be taken with both the elbow flexed and extended. The EMG typically shows low ulnar sensory amplitudes and slowed ulnar motor conduction velocities across the elbow.3 The median sensory/motor distal latencies are normal. Short-segment stimulation or “the inching technique”73,74 studies done at 1- to 2-cm intervals across the elbow give the most useful information, and with this technique and focal changes in amplitude or a waveform morphology change or conduction delay of more than 0.7 milliseconds across each 2 cm are considered abnormal.75 A decrease in amplitude of the ulnar sensory nerve action potential (SNAP) helps in the diagnosis. If both the ulnar and median conduction velocities are abnormal, the contralateral elbow as well as lower extremity NCVs should be performed to rule out a peripheral neuropathy.72
In cases of suspected ulnar neuropathy at the elbow, needle EMGs from abductor digiti minimi and first dorsal interossei should be performed even if the NCVs are within normal limits.70,72 There are, however, instances where the patient exhibits a clinical picture of ulnar nerve entrapment with normal EMG/NCV studies. It is up to the judgment of the clinician in these rare cases whether to offer surgical intervention. This decision is then based on the clinical examination.
Differential Diagnosis
The differential diagnosis of ulnar neuropathy includes any lesion along the entire length of the ulnar nerve from the root level C8–T1. This includes cervical radiculopathy due to a herniated disc or a bony spur, brachial neuritis, pancoast tumor involving C8–T1, and thoracic outlet syndrome. Through imaging, NCV/EMG testing, and clinical examination, the correct diagnosis can usually be discerned. EMG of the intrinsic muscles of the hand innervated by the median and the ulnar nerve (C8–T1) are helpful in differentiating lesions in the spine and brachial plexus from more distal compression neuropathies.
Treatment Options
Conservative Treatment
Conservative treatment should always be given an opportunity and surgical intervention considered only after failure of initial conservative treatment.76 Patients should be thoroughly counseled on the techniques of conservative management,76 including rest and avoiding pressure on the nerve, but if symptoms persist, split immobilization of the elbow and wrist may be warranted.24 The arm can be immobilized in a splint with the elbow at 70 degrees, the wrist neutral and the forearm in mid-position for short periods (2 weeks or less) without any untoward consequences. Pillows under the arm to support and cushion the area of the cubital tunnel, anti-inflammatory medications, and analgesics should also be employed. The patient should be cautioned to avoid activity that puts strain on the cubital tunnel, that is, prolonged elbow flexion, leaning on the elbows while working with the hands or on the computer. The addition of a steroid injection does not appear to provide further benefit in the treatment of cubital tunnel syndrome.77 A rapid neurologic decline and a picture consistent with ulnar nerve entrapment may warrant the omission of a period of conservative treatment; again the clinician’s judgment is required.
Surgical Treatment
General Considerations
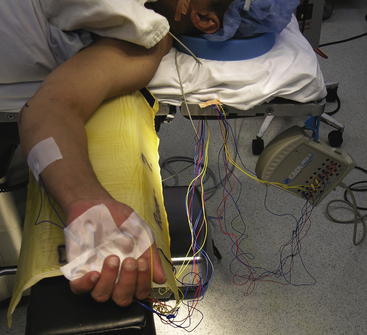
The patient is placed in the supine position with the arm abducted on an arm board (Fig. 200-1). The shoulder is abducted and externally rotated. The forearm is placed slightly flexed and in supination. The surgeon works from between the abducted arm and the patient’s body. A small ipsilateral shoulder roll may help facilitate this positioning. A seated position is often the most comfortable for operating. Although some surgeons prefer the use of a tourniquet during the surgery, it is not necessary to do so if attention is given to good hemostasis.
The authors use intraoperative electrophysiologic monitoring in all cases of ulnar nerve exploration (Fig. 199-1). It is critical to discuss the case with the anesthesia team and instruct them not to use paralytic anesthetic agents once the initial intubation is complete. Some surgeons prefer to perform this procedure under local anesthetic with sedation; however, the discomfort associated with manipulating the ulnar nerve directly can make this problematic. The electrophysiologist places the needles in the desired musculature, in this case the flexor carpi ulnaris, interossei, and hypothenar muscles, prior to the preparation and drape of the limb. Care should be taken so that the needles do not enter the operative field and a wide prepping for ulnar nerve exposure is recommended both proximally and distally.
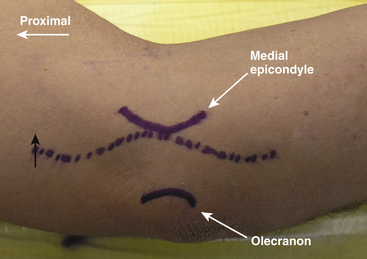
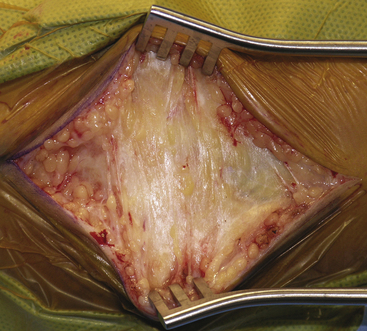
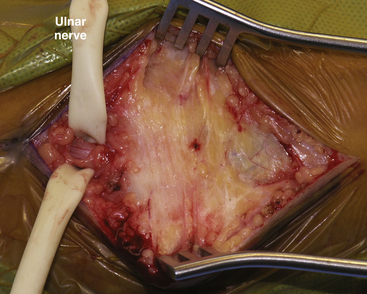
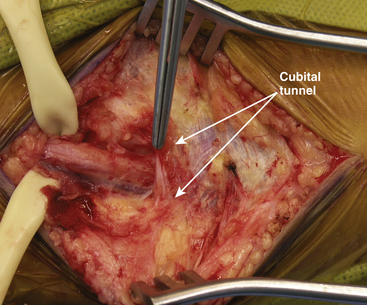
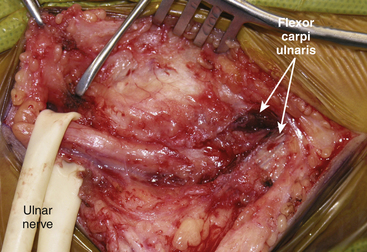
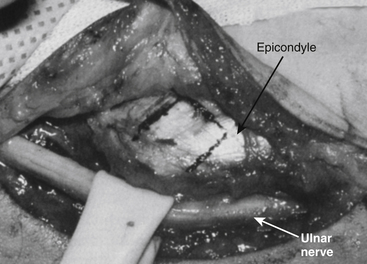
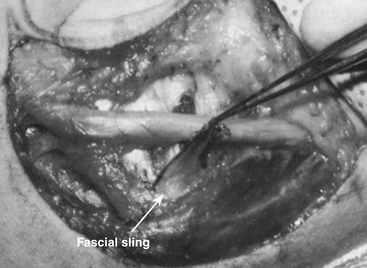
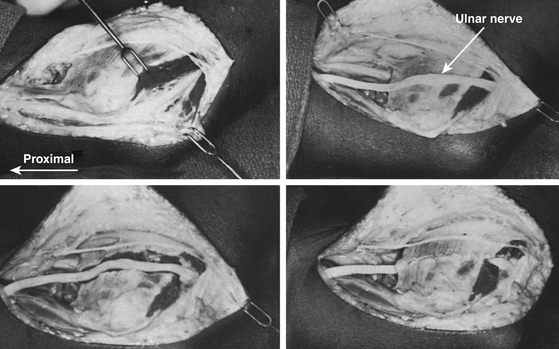
The medial epicondyle and olecranon are marked. Exposure of the nerve within the cubital tunnel begins with a skin incision 5 cm proximal to the medial epicondyle that curves gently up and over the condyle. This curvature avoids placing the incision directly over the joint flexion. The incision then continues distally onto the forearm for another 4 cm to 5 cm (Fig. 200-2). More recently smaller incisions are being used, and with endoscopic assistance the length of the incision can be shortened considerably. The skin is incised using a #10 or #15 surgical blade, after being infiltrated with 1% lidocaine with epinephrine in a 1:100,000 concentration. The subcutaneous tissue is divided with Metzenbaum scissors. The medial antebrachial cutaneous nerve or its anterior superior branch may cross the operative field. These nerves should be identified and protected if encountered. After the skin and subcutaneous tissue are retracted, the nerve is located beneath an investing fascia within the cubital tunnel (Fig. 200-3). Just underneath the fascia, the ulnar nerve is identified proximal to the postcondylar groove and anterior to the medial head of the triceps. The nerve is then followed distally into the postcondylar groove. The fascial roof between the medial epicondyle and olecranon (Osborne’s band) is sharply divided in a proximal-to-distal direction. The groove is the site of maximal nerve compression in most cases (Fig. 200-4). Distal to the postcondylar groove, the ulnar nerve is followed as it courses deep to the aponeurosis between the two heads of the flexor carpi ulnaris muscle. The aponeurosis between the two muscle heads is divided (Fig. 200-5). The nerve is also explored proximally, and if a transposition of the nerve is to be performed then care is taken to divide the medial intermuscular septum (Fig. 200-6). The nerve is examined for subluxation by moving the elbow through its range of motion. If there is significant subluxation, then a transposition procedure will be indicated. Meticulous hemostasis is achieved by use of bipolar cautery, hemostatic agents such as Fibrillar, and warm irrigation. The wound is closed in anatomic layers: the subcutaneous tissues are reapproximated with 3-0 interrupted, inverted Vicryl sutures (Ethicon, Inc., Somerville, NJ). The skin is closed with either simple running 4-0 nylon sutures or subcuticular absorbable 4-0 sutures. A soft compressive dressing is applied. If there has been a transposition of the nerve, a sling is advised for 2 weeks; if not, a sling may be recommended for comfort in the immediate postoperative period (24–48 hours). Early range of motion and physical therapy for the arm and hand are encouraged. Intraoperative flexion and extension of the arm and careful visualization that the ulnar nerve is free of compression and entrapment before closing skin and fascia should become part of the surgeon’s routine.
Procedures
In Situ Decompression
Simple decompression without transposition was first proposed by Farquhar Buzzard in 1922. By unroofing the cubital tunnel, a simple decompression of the ulnar nerve is accomplished. Performed by neurosurgeons more commonly than the other surgical options for the treatment of cubital tunnel syndrome,78 it has been shown to be the most satisfactory option for most cases of cubital tunnel entrapment of the ulnar nerve.2 It is not challenging technically and carries a low risk of vascular insult or injury to the nerve, issues that may be of concern in anterior transpositions.79 It is a localized decompression of the ulnar nerve as it passes between the two heads of the flexor carpi ulnaris24 and sectioning of the Osborne’s ligament also called the arcuate ligament. An incision is made posterior to the medial humeral epicondyle as explained in the general surgical approaches to the ulnar nerve. The epicondyle is palpated and dissection carried out to the bone. The nerve is identified proximal to the epicondyle and released completely from where it pierces the intermuscular septum to well beyond Osborne’s band. This involves cutting the intermuscular septum, the Struthers’s arcade (if present), the arcuate cubital ligament (Osborne’s ligament), and widely splitting open the aponeurotic bands between the two heads of the flexor carpi ulnaris. Circumferential dissection of the nerve is not required. Some authors suggest resuturing the ligament beneath the nerve to reduce scarring but this can result in recurrent compression and should be avoided.24 Heithoff cites studies that support the segmental nature of the ulnar nerve blood supply that is injured if the nerve is dissected a given distance.79,80 Inadvertent injury to the medial antebrachial cutaneous nerve81 may postoperatively cause painful neuroma with persistent elbow pain, numbness around the elbow, and scar tenderness.82 The main cause for failure of simple decompression83 is related to anterior subluxation, which occurs in 2.4% to 17% of cases.2,84–86
More recently endoscopic surgery for in-situ decompression87–94 and endoscopic neurolysis has been described.95 The procedure focuses on the division of Osborne’s arcuate ligament96,97 and performing a simple in-situ decompression. The outcome of endoscopic decompression has been shown to be good in cohort studies69,87,90 and in Dellon’s 111 patients98 appears equivalent to the reported outcome with open techniques,85,99,100 the success rate for which with careful patient selection ranges from 80% to 92%.2,101–104
Critics of in situ decompression have claimed that without transposition, the pathologic traction and compression forces from the ulnar nerve’s location at the posterior elbow axis of rotation would not be relieved.105,106 Recent literature has not supported this contention.
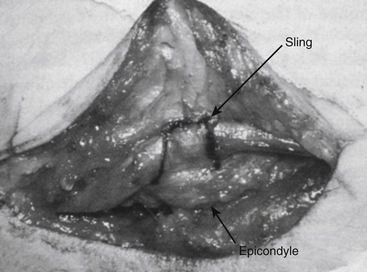
Subcutaneous Transposition
Until the beginning of the 20th century, anterior transposition was the treatment of choice for compressive ulnar neuropathy at the elbow.5,107,108 It is more commonly performed and the least complicated of the transposition procedures. Anterior transposition may be indicated if the patient is found to have nerve subluxation at the time of surgery.2 For many, it remains the procedure of choice for repositioning the nerve during surgical reductions of acute fractures, arthroplasties of the elbow, and secondary neurorrhaphies where a large length is needed to overcome a gap after excision of the neuroma.24 After exposure, the nerve is circumferentially dissected and lifted out of its cubital tunnel bed and placed below the subcutaneous fat of the arm and forearm. Sensory fibers to the elbow joints are by necessity severed, but this causes no motor or sensory deficits. Branches supplying the upper fibers of the flexor carpi ulnaris come off quite proximally and are dissected carefully to gain length to allow the nerve to be moved onto the anterior surface of the elbow flexor muscle tendons which lie anterior to the medial epicondyle. To avoid kinking the nerve at both ends of the transposition, the inter-muscular septum is divided at the proximal end, and the aponeurosis and muscle fibers between the heads of the flexor carpi ulnaris are split longitudinally. This is required for all transposition procedures regardless of the technique used. This prevents tethering of the nerve close to the epicondyle. The nerve is then gently placed in a subcutaneous bed under a preformed fasciodermal flap/sling as first described by Eaton,109 and fashioned by raising a layer from the flexor tendons found atop the medial epicondyle (Figs. 200-7 and 200-8). This flap is secured by suturing it to the subcutaneous tissue and in this way the nerve is prevented from reverting to its position in the ulnar groove (Fig. 200-9). The subcutaneous transposition has the advantage of a smaller incision, shorter operative time, less postoperative pain, fewer postoperative complications, and better outcome in some studies as compared to submuscular transposition.110 Disadvantages of the subcutaneous transposition include the new location’s relative avascularity and vulnerability to trauma, particularly in patients with scant subcutaneous tissue.111
Subfascial/Intramuscular Transposition
In 1917, Rudolf Klauser5,14 was the first to describe the technique of anterior intramuscular transposition. After dissection from the surrounding tissue as described above, the nerve is placed in a shallow muscular trough created in the pronator teres and flexor carpi ulnaris (Fig. 200-10). Proponents of this technique105,106 advocated that this technique requires less muscular dissection. Recurrent symptoms secondary to postoperative scarring within the intramuscular bed are more commonly seen in this procedure than in subcutaneous transpositions which are thought to be due to the nerve’s vulnerability to tensile stresses and cicatricial scarring because the nerve is positioned within the muscle at right angles to its fibers and therefore subjected to higher traction forces.111,112
Submuscular Transposition
Submuscular transposition was described by Learmonth in 1942. The anterior surface of the pronator teres is dissected free over a length of 4 cm beyond its origin, often necessitating a fibrous extension of the medial free edge of the biceps aponeurosis across the antecubital fossa. The pronator teres origin is then divided along with the origin of the flexor carpi ulnaris. The anteriorly transposed ulnar nerve is then placed under the divided muscles on a fascial bed over the flexor digitorum superficialis and brachialis.113 The cut ends of the divided tendons are reapproximated in the Z-plasty114,115 format. Although proponents of intramuscular transposition report that even though this is technically a more difficult surgery requiring extensive dissection,24 it is the only technique that addresses nerve compression at all five potential sites. However, the procedure can result in severe postoperative perineural scarring. It is suggested that it is the interaction of the transposed ulnar nerve with other fibrous anatomic structures proximal to, across, and distal to the elbow that causes failure in ulnar nerve transposition procedures, rather than an adverse reaction between the incised flexor-pronator muscle mass and the ulnar nerve.116 Moreover, the recommended postoperative immobilization of the elbow to allow for the incised flexor-pronator muscles to heal may cause a flexion contracture at the elbow. Therefore, the elbow should not be immobilized greater than 45 degrees and for no longer than 3 to 4 weeks. Submuscular transposition may be a more attractive option when prior surgery has been unsuccessful.24
Medial Epicondylectomy
Medial epicondylectomy was first described by Thomas King (1899–1973)20,117 in 1950. This was initially advocated to answer the criticisms of performing the subcutaneous and submuscular transpositions alone. Critics claimed that with subcutaneous transpositions, the nerve was still subject to irritation if it shifted posteriorly with elbow extension by simply slipping onto the apex of the medial epicondyle.24 With submuscular transposition alone, the nerve was still exposed to postoperative scarring. In this technique, after the ulnar nerve is exposed, it is decompressed in situ as outlined above. Then the medial epicondyle is subperiosteally exposed and rongeured away without disturbing the origin of the pronator teres. The soft tissues over the osteotomy bed are then reapproximated. Postoperative immobilization is not required after this procedure. Due to problems with osteomyelitis, pain, and the realization that the epicondyle need not be removed, this technique has lost favor and is now rarely performed.
A sling is used postoperatively if a transposition has been performed. This sling is usually kept in place for 2 weeks. A sling may also be utilized for 24 to 48 hours for comfort if a simple decompression has been performed. Gentle physical therapy is instituted at 2 to 3 weeks postoperatively to return the joint to full extension. Failed ulnar nerve release with persistence and/or worsening of symptoms may be due to inadequate release of the nerve proximally and/or distally, formation of a local postsurgical hematoma, overzealous/tight fascial closure, or improper diagnosis. Studies have shown that the most common complaint after primary surgery is increased symptoms in the ulnar distributions and pain in the medial antebrachial cutaneous nerve distribution. The most common findings at reoperation included a medial antebrachial cutaneous neuroma and a distal kink of the ulnar nerve.118 Continued ulnar-related deficits should warrant a follow-up EMG/NCS.
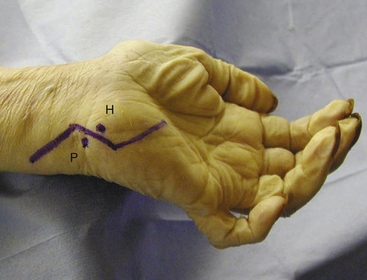
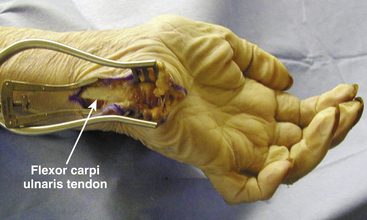
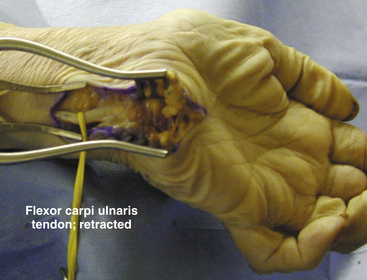
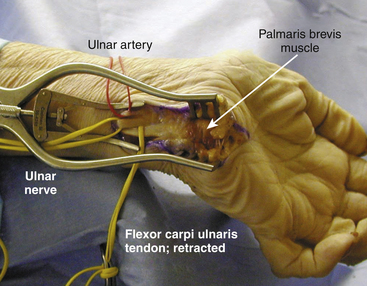
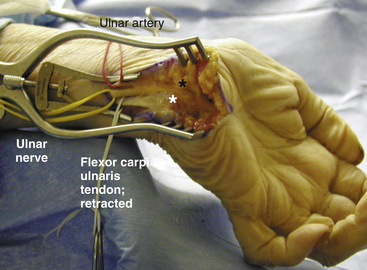
Surgery for Decompression at Guyon’s Canal
The patient is placed in the supine position with the arm on the arm board. The shoulder is abducted and externally rotated with the arm in full supination. A small rounded towel is placed under the wrist to elevate it and a lead hand may be used to keep the fingers in an extended position. The entire hand and the wrist are prepped. The surgeon works from a position between the abducted arm and patient’s body. A seated position is often the most comfortable for operating. The skin incision is designed to lie in the interval between the palmar cutaneous branches of the median nerve and ulnar nerve. The pisiform bone on the medial aspect of the distal wrist is palpated and marked. One centimeter distal and lateral to the pisiform, the hook of the hamate bone is palpated and marked. An incision is made beginning ~4 cm proximal to the wrist on a line midway between the parked pisiform bone and the midline of the wrist. It moves toward the wrist and crosses the distal wrist crease at an oblique angle. In general, crossing the wrist crease at right angles is avoided. The incision extends another 4 cm onto the ulnar aspect of the palm, moving between pisiform and hamate bones in an incision, moving gently towards the midline of the palm (Fig. 200-11). After the skin is divided, the flexor carpi ulnaris tendon is isolated (Fig. 200-12) and retracted in an ulnar (medial) direction (Fig. 200-13), exposing the ulnar nerve and the artery just deep to the tendon in a posterolateral direction. The artery is located to the radial side of the nerve. The nerve is then traced distally. The palmar carpal ligament, the Palmaris brevis muscle fibers, and the hypothenar fat and fibrous tissue is incised and retracted to expose the nerve fully along the course of Guyon’s canal (Fig. 200-14). Once exposed in the canal, the nerve may be traced out distally as it divides into its terminal branches (Figs. 200-15 and 200-16).
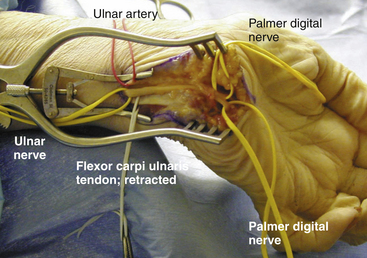
FIGURE 200-16 Guyon’s canal fully exposed including its terminal branches and palmar digital nerves.
In all of these procedures, it should be noted that advanced age, prolonged duration of symptoms, and weakness and/or atrophy of intrinsic hand musculature are associated with poorer outcomes regardless of ulnar nerve operation performed.119
Decision making regarding the appropriateness of type of surgery for the patient has evolved over the years. Dellon’s120 review of 50 papers from 1898 to 1988 concluded that treatment is most successful for mild neuropathies and excellent results are achieved in 50% of the patients with mild neuropathies who were treated nonsurgically and in more than 90% who were treated surgically (regardless of the type of procedure). He notes that for moderate neuropathies, nonsurgical treatments were unsuccessful as was simple decompression in situ. Anterior submuscular transposition yielded the best results and fewest recurrences. For the most severe neuropathies, internal neurolysis combined with anterior intermuscular transposition yielded the best results. However, more recently, the literature review from 1970 to 1997 by Bartels et al.,2 including over 3000 patients, is the largest thus far. The authors concluded that irrespective of their preoperative status, a simple decompression had the most favorable outcomes and that patients with subcutaneous and submuscular transpositions had the worst outcomes. They also concluded that if the preoperative status of the patient was considered, then a significant difference between procedures was not found for a preoperative McGowan grade 2. However, for more severe preoperative symptoms, that is, McGowan grade 3, patients with intramuscular transpositions had the best outcomes followed by simple decompressions and submuscular transpositions.
Reviews of recent literature and our own experience78 have shown that in a majority of the patients, simple decompression in situ achieves satisfactory outcomes without the need for a circumferential mobilization of the nerve. However, each case must be treated individually, defining the abnormality that is intrinsic to each, and the surgeon in consultation with the patient should decide on the optimal surgical technique/approach on the basis of the preoperative evaluation, electrodiagnostic studies, and intraoperative findings.121
Bartels R.H.. History of the surgical treatment of ulnar nerve compression at the elbow., Neurosurgery, 2001;49:391-399 discussion 399-400
Bartels R.H., Menovsky T., Van Overbeeke J.J., et al. Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. J Neurosurg. 1998;89:722-727.
Britz G.W., Haynor D.R., Kuntz C., et al. Ulnar nerve entrapment at the elbow: correlation of magnetic resonance imaging, clinical, electrodiagnostic, and intraoperative findings. Neurosurgery. 1996;38:458-465. discussion 465
Campbell W.W., Pridgeon R., Sahni K. Short segment incremental studies in the evaluation of ulnar neuropathy at the elbow. Muscle Nerve. 1992;15:1050-1054.
Dellon A.L., Coert J.H. Results of the musculofascial lengthening technique for submuscular transposition of the ulnar nerve at the elbow. J Bone Joint Surg Am. 2004;86-A(Suppl 1):169-179.
Eaton R.G., Crowe J.F., Parkes J.C.3rd. Anterior transposition of the ulnar nerve using a non-compressing fasciodermal sling. J Bone Joint Surg Am. 1980;62:820-825.
Goldfarb C.A., Sutter M.M., Martens E.J., et al. Incidence of re-operation and subjective outcome following in situ decompression of the ulnar nerve at the cubital tunnel. J Hand Surg Eur. 2009;34:379-383.
Heithoff S.J. Cubital tunnel syndrome does not require transposition of the ulnar nerve. J Hand Surg Am. 1999;24:898-905.
Hoffmann R., Meek M.F. Endoscopic decompression of the ulnar nerve at the elbow. J Hand Surg Am. 2008;33:615. author reply 615-616
Hong C.Z., Long H.A., Kanakamedala R.V., et al. Splinting and local steroid injection for the treatment of ulnar neuropathy at the elbow: clinical and electrophysiological evaluation. Arch Phys Med Rehabil. 1996;77:573-577.
Huang J.H., Samadani U., Zager E.L. Ulnar nerve entrapment neuropathy at the elbow: simple decompression. Neurosurgery. 2004;55:1150-1153.
Jaddue D.A., Saloo S.A., Sayed-Noor A.S. Subcutaneous vs submuscular ulnar nerve transposition in moderate cubital tunnel syndrome. Open Orthop J. 2009;3:78-82.
Janjua R.M., Fernandez J., Tender G., et al. Submuscular transposition of the ulnar nerve for the treatment of cubital tunnel syndrome. Neurosurgery. 2008;63:321-324. discussion 324-325
Kim D.H., Han K., Tiel R.L., et al. Surgical outcomes of 654 ulnar nerve lesions. J Neurosurg. 2003;98:993-1004.
Kleinman W.B., Bishop A.T. Anterior intramuscular transposition of the ulnar nerve. J Hand Surg Am. 1989;14:972-979.
Kline D., Hudson A. Nerve Injuries: Operative Results for Major Injuries, Entrapments, and Tumors. Philadelphia: WB Saunders, 1995.
Leffert R.D. Anterior submuscular transposition of the ulnar nerves by the Learmonth technique. J Hand Surg Am. 1982;7:147-155.
Mackinnon S.E., Novak C.B. Operative findings in reoperation of patients with cubital tunnel syndrome. Hand (NY). 2007;2:137-143.
Maniker A., Passannante M. Peripheral nerve surgery and neurosurgeons: results of a national survey of practice patterns and attitudes. J Neurosurg. 2003;98:1159-1164.
Nathan P.A., Keniston R.C., Meadows K.D. Outcome study of ulnar nerve compression at the elbow treated with simple decompression and an early programme of physical therapy. J Hand Surg Br. 1995;20:628-637.
Pasque C.B., Rayan G.M. Anterior submuscular transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Br. 1995;20:447-453.
Posner M.A. Compressive neuropathies of the ulnar nerve at the elbow and wrist. Instr Course Lect. 2000;49:305-317.
Stuffer M., Jungwirth W., Hussl H., et al. Subcutaneous or submuscular anterior transposition of the ulnar nerve? J Hand Surg Br. 1992;17:248-250.
Watts A.C., Bain G.I. Patient-rated outcome of ulnar nerve decompression: a comparison of endoscopic and open in situ decompression. J Hand Surg Am. 2009;34:1492-1498.
Youmans J.R. Neurological Surgery: A Comprehensive Reference Guide to the Diagnosis and Management of Neurosurgical Problems, 4th ed. Philadelphia: Saunders; 1996.
1. Apfelberg D.B., Larson S.J. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg. 1973;51:79-81.
2. Bartels R.H., Menovsky T., Van Overbeeke J.J., et al. Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. J Neurosurg. 1998;89:722-727.
3. Bradshaw D.Y., Shefner J.M.. Ulnar neuropathy at the elbow., Neurol Clin, 1999;17:447-461 v-vi
4. Granger B. On a particular fracture of the inner condyle of the humerus. Edinburgh Med Surg J. 1818;14:196-201.
5. Bartels R.H. History of the surgical treatment of ulnar nerve compression at the elbow. Neurosurgery. 2001;49:391-399. discussion 399-400
6. Bowlby A: Injuries and Diseases of Nerves and Their Surgical Treatment. London, 1889.
7. Ballet G. Accidents consécutifs a la compression habituelle du cubital chez un ouvrier employé a ouvrager le verre. Revue de Médecine. 1884;4:484-486.
8. Granger B. On a particular fracture of the inner condyle of the humerus. Edinburgh Med Surg J. 1818;14:196-201.
9. Earle H. Cases and observations, illustrating the influence of the nervous system in regulating animal heat. Medico-Chirurgical Transactions. 1816;7:173-194.
10. Panas J. Sur une cause peu connue de paralysie du nerf cubital. Arch Gen Med. 1878;2:5-15.
11. Poncet M. Luxation pathologique en avant du nerf cubital droit. La Semaine Médicale. 1888;8:93.
12. Curtis B. Traumatic ulnar neuritis: transplantation of the nerve. J Nerv Ment Dis. 1898;25:480-484.
13. Mouchet A. Paralysies tardives du nerf cubital à la suite des fractures du condyle externe de l’humérus. Journal de Chirurgie Revue Critique(Paris). 1914;12:437-456.
14. Klauser R. Verlagerung des Nervus ulnaris. Münchener Medizinische Wochenschrift. 1917;64:635.
15. Learmonth J. A technique for transplanting the ulnar nerve. Surg Gynecol Obstet. 1942;75:792-793.
16. Youmans J.R. Neurological Surgery: A Comprehensive Reference Guide to the Diagnosis and Management of Neurosurgical Problems, 4th ed. Philadelphia: Saunders; 1996.
17. Feindel W., Stratford J. Cubital tunnel compression in tardy ulnar palsy. CMA J. 1958;78:351-353.
18. Feindel W., Stratford J. The role of the cubital tunnel in tardy ulnar palsy. Can J Surg. 1958;1:287-300.
19. Osborne G. Ulnar neuritis. Postgraduate Med J. 1959;35:392-396.
20. King Morgan. Late results of removing the medial humeral epicondyle for traumatic ulnar neuritis. J Bone Joint Surg Br. 1959;41:51-55.
21. Bartels R.H. Redefining the “arcade of Struthers. J Hand Surg Am. 2004;29:335. author reply 335
22. Bartels R.H., Grotenhuis J.A., Kauer J.M. The arcade of Struthers: an anatomical study. Acta Neurochir (Wien). 2003;145:295-300. discussion 300
23. von Schroeder H.P., Scheker L.R. Redefining the “arcade of Struthers. J Hand Surg Am. 2003;28:1018-1021.
24. Posner M.A. Compressive neuropathies of the ulnar nerve at the elbow and wrist. Instr Course Lect. 2000;49:305-317.
25. Khoo D., Carmichael S.W., Spinner R.J. Ulnar nerve anatomy and compression. Orthop Clin North Am. 1996;27:317-338.
26. Patel V.V., Heidenreich F.P.Jr., Bindra R.R., et al. Morphologic changes in the ulnar nerve at the elbow with flexion and extension: a magnetic resonance imaging study with 3-dimensional reconstruction. J Shoulder Elbow Surg. 1998;7:368-374.
27. Werner C.O., Ohlin P., Elmqvist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand. 1985;56:404-406.
28. Yamaguchi K., Sweet F.A., Bindra R., et al. The extraneural and intraneural arterial anatomy of the ulnar nerve at the elbow. J Shoulder Elbow Surg. 1999;8:17-21.
29. Dellon A.L., Mackinnon S.E. Anatomic investigations of nerves at the wrist: II. Incidence of fibrous arch overlying motor branch of ulnar nerve. Ann Plast Surg. 1988;21:36-37.
30. Atkins S.E., Logan B., McGrouther D.A. The deep (motor) branch of the ulnar nerve: a detailed examination of its course and the clinical significance of its damage. J Hand Surg Eur. 2009;34:47-57.
31. Huang J.H., Samadani U., Zager E.L. Ulnar nerve entrapment neuropathy at the elbow: simple decompression. Neurosurgery. 2004;55:1150-1153.
32. Martin R. Tal om nervus allmanna egenskaper 1 mannsikans kropp. Stockholm: Lars Salvius; 1763.
33. Gruber W. Über die Verbindung des Nervus medianus mit dem Nervus ulnaris am Unterarme des Menschen und der Säugethiere. Archiv für pathologische Anatomie und Physiologie und für klinische Medizin. 1870;37:501-522.
34. Dumitru D., Walsh N.E., Weber C.F. Electrophysiologic study of the Riche-Cannieu anomaly. Electromyogr Clin Neurophysiol. 1988;28:27-31.
35. McCluskey L.F., Webb L.B. Compression and entrapment neuropathies of the lower extremity. Clin Podiatr Med Surg. 1999;16:97-125. vii
36. Eversmann W.W.Jr. Compression and entrapment neuropathies of the upper extremity. J Hand Surg Am. 1983;8:759-766.
37. Macnicol M.F. Extraneural pressures affecting the ulnar nerve at the elbow. Hand. 1982;14:5-11.
38. Pechan J., Julis I. The pressure measurement in the ulnar nerve. A contribution to the pathophysiology of the cubital tunnel syndrome. J Biomech. 1975;8:75-79.
39. Swenson J.D., Hutchinson D.T., Bromberg M., et al. Rapid onset of ulnar nerve dysfunction during transient occlusion of the brachial artery. Anesth Analg. 1998;87:677-680.
40. Vanderpool D.W., Chalmers J., Lamb D.W., et al. Peripheral compression lesions of the ulnar nerve. J Bone Joint Surg Br. 1968;50:792-803.
41. Pechan J. Ulnar nerve maneuver as diagnostic aid in its compression in the elbow region. Cesk Neurol. 1973;36:13-19.
42. Aoki M., Takasaki H., Muraki T., et al. Strain on the ulnar nerve at the elbow and wrist during throwing motion. J Bone Joint Surg Am. 2005;87:2508-2514.
43. Bozentka D.J. Cubital tunnel syndrome pathophysiology. Clin Orthop Relat Res. 1998:90-94.
44. Posner M.A. Compressive ulnar neuropathies at the elbow: I. Etiology and diagnosis. J Am Acad Orthop Surg. 1998;6:282-288.
45. Fragiadakis E.G., Lamb D.W. An unusual cause of ulnar nerve compression. Hand. 1970;2:14-16.
46. Ruder J.R., Wood V.E. Ulnar nerve compression at the arch of origin of the adductor pollicis muscle. J Hand Surg Am. 1993;18:893-895.
47. Bladt L., Vankan Y., Demeyere A., et al. Bilateral ulnar nerve compression by anconeus epitrochlearis muscle. JBR-BTR. 2009;92:120.
48. Heithoff S.J., Millender L.H., Nalebuff E.A., et al. Medial epicondylectomy for the treatment of ulnar nerve compression at the elbow. J Hand Surg Am. 1990;15:22-29.
49. Wang H.C., Tsai M.D. Compressive ulnar neuropathy in the proximal forearm caused by a gouty tophus. Muscle Nerve. 1996;19:525-527.
50. Al-Benna S., Schubert C., Steinau H.U., et al. Brachial neuropathy 22 years after radiation therapy for fibrosarcoma: a case report. Cases J. 2009;2:6838.
51. Kim D., Kang J., Park J. Multilevel ulnar neuropathy caused by multiple intraneural hemangiomas. Muscle Nerve. 2010;41:562-566.
52. Birch R., Bonney G., Dowell J., et al. Iatrogenic injuries of peripheral nerves. J Bone Joint Surg Br. 1991;73:280-282.
53. Nath R.K., Mackinnon S.E., Weeks P.M. Ulnar nerve transection as a complication of two-portal endoscopic carpal tunnel release: a case report. J Hand Surg Am. 1993;18:896-898.
54. Rispoli D.M., Athwal G.S., Morrey B.F. Neurolysis of the ulnar nerve for neuropathy following total elbow replacement. J Bone Joint Surg Br. 2008;90:1348-1351.
55. Kabayel L., Balci K., Turgut N., et al. Development of entrapment neuropathies in acute stroke patients. Acta Neurol Scand. 2009;120:53-58.
56. Pearce C., Feinberg J., Wolfe S.W. Ulnar neuropathy at the wrist. HSS J. 2009;5:178-185.
57. Rohilla S., Yadav R.K., Dhaulakhandi D.B. Lipoma of Guyon’s canal causing ulnar neuropathy. J Orthop Traumatol. 2009;10:101-103.
58. Ginanneschi F., Filippou G., Milani P., et al. Ulnar nerve compression neuropathy at Guyon’s canal caused by crutch walking: case report with ultrasonographic nerve imaging. Arch Phys Med Rehabil. 2009;90:522-524.
59. Kim S.S., Kim J.H., Kang H.I., et al. Ulnar nerve compression at Guyon’s canal by an arteriovenous malformation. J Kor Neurosurg Soc. 2009;45:57-59.
60. Mc G.A. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br. 1950;32-B:293-301.
61. Sunderland S. Nerves and Nerve Injuries, 2nd ed. Edinburgh, New York: Churchill Livingstone; 1978.
62. Amadio P.C., Beckenbaugh R.D. Entrapment of the ulnar nerve by the deep flexor-pronator aponeurosis. J Hand Surg Am. 1986;11:83-87.
63. Richardson C., Fabre G. Froment’s sign. J Audiov Media Med. 2003;26:34.
64. Pham M., Bendszus M. MRI as an additional diagnostic tool for the cubital tunnel syndrome. Handchir Mikrochir Plast Chir. 2009;41:18-22.
65. Kutlay M., Colak A., Simsek H., et al. Use of ultrasonography in ulnar nerve entrapment surgery—a prospective study. Neurosurg Rev. 2009;32:225-232. discussion 232
66. Britz G.W., Haynor D.R., Kuntz C., et al. Ulnar nerve entrapment at the elbow: correlation of magnetic resonance imaging, clinical, electrodiagnostic, and intraoperative findings. Neurosurgery. 1996;38:458-465. discussion 465
67. Hof J.J., Kliot M., Slimp J., et al. What’s new in MRI of peripheral nerve entrapment? Neurosurg Clin North Am. 2008;19:583-595. vi
68. Simpson J.A. Electrical signs in the diagnosis of carpal tunnel and related syndromes. J Neurol Neurosurg Psychiatry. 1956;19:275-280.
69. Taniguchi Y., Takami M., Takami T., et al. Simple decompression with small skin incision for cubital tunnel syndrome. J Hand Surg Br. 2002;27:559-562.
70. Jabre J., Wilbourn A. The EMG findings in 100 consecutive ulnar neuropathies. Acta Neurol Scand. 1979;60:91.
71. Stewart J.D. The variable clinical manifestations of ulnar neuropathies at the elbow. J Neurol Neurosurg Psychiatry. 1987;50:252-258.
72. Yuen E., Robinson L., Slimp J. Electrodiagnostic evaluation of peripheral nerves: electromyography, Somatosensory Evoked Potentials, Nerve Action Potentials. Vol.4, 5th ed, Philadelphia: Saunders, 1996.
73. Campbell W.W., Pridgeon R., Sahni K. Short segment incremental studies in the evaluation of ulnar neuropathy at the elbow. Muscle Nerve. 1992;15:1050-1054.
74. Miller R.G. The cubital tunnel syndrome: diagnosis and precise localization. Ann Neurol. 1979;6:56-59.
75. Kanakamedala R.V., Simons D.G., Porter R.W., et al. Ulnar nerve entrapment at the elbow localized by short segment stimulation. Arch Phys Med Rehabil. 1988;69:959-963.
76. Nakamichi K., Tachibana S., Ida M., et al. Patient education for the treatment of ulnar neuropathy at the elbow. Arch Phys Med Rehabil. 2009;90:1839-1845.
77. Hong C.Z., Long H.A., Kanakamedala R.V., et al. Splinting and local steroid injection for the treatment of ulnar neuropathy at the elbow: clinical and electrophysiological evaluation. Arch Phys Med Rehabil. 1996;77:573-577.
78. Maniker A., Passannante M. Peripheral nerve surgery and neurosurgeons: results of a national survey of practice patterns and attitudes. J Neurosurg. 2003;98:1159-1164.
79. Heithoff S.J. Cubital tunnel syndrome does not require transposition of the ulnar nerve. J Hand Surg Am. 1999;24:898-905.
80. Lim B.H., Toh C.L., Wong H.P., et al. Cadaveric study on the vascular anatomy of the ulnar nerve at the elbow—a basis for anterior transposition? Ann Acad Med Singapore. 1992;21:689-693.
81. Lowe J.B.3rd, Maggi S.P., Mackinnon S.E. The position of crossing branches of the medial antebrachial cutaneous nerve during cubital tunnel surgery in humans. Plast Reconstr Surg. 2004;114:692-696.
82. Dellon A.L., MacKinnon S.E. Injury to the medial antebrachial cutaneous nerve during cubital tunnel surgery. J Hand Surg Br. 1985;10:33-36.
83. Goldfarb C.A., Sutter M.M., Martens E.J., et al. Incidence of re-operation and subjective outcome following in situ decompression of the ulnar nerve at the cubital tunnel. J Hand Surg Eur. 2009;34:379-383.
84. Leffert R.D. Anterior submuscular transposition of the ulnar nerves by the Learmonth technique. J Hand Surg Am. 1982;7:147-155.
85. Nathan P.A., Keniston R.C., Meadows K.D. Outcome study of ulnar nerve compression at the elbow treated with simple decompression and an early programme of physical therapy. J Hand Surg Br. 1995;20:628-637.
87. Ahcan U., Zorman P. Endoscopic decompression of the ulnar nerve at the elbow. J Hand Surg Am. 2007;32:1171-1176.
88. Bultmann C., Hoffmann R. Endoscopic decompression of the ulnar nerve in cubital tunnel syndrome. Oper Orthop Traumatol. 2009;21:193-205.
88. Stuffer M., Jungwirth W., Hussl H., et al. Subcutaneous or submuscular anterior transposition of the ulnar nerve? J Hand Surg Br. 1992;17:248-250.
89. Hoffmann R., Meek M.F. Endoscopic decompression of the ulnar nerve at the elbow. J Hand Surg Am. 2008;33:615. author reply 615-616
90. Hoffmann R., Siemionow M. The endoscopic management of cubital tunnel syndrome. J Hand Surg Br. 2006;31:23-29.
91. Krishnan K.G., Pinzer T., Schackert G. A novel endoscopic technique in treating single nerve entrapment syndromes with special attention to ulnar nerve transposition and tarsal tunnel release: clinical application. Neurosurgery. 2006;59:ONS89-ONS100. discussion ONS189-100
92. Nakao Y., Takayama S., Toyama Y. Cubital tunnel release with lift-type endoscopic surgery. Hand Surg. 2001;6:199-203.
93. Tsai T.M., Bonczar M., Tsuruta T., et al. A new operative technique: cubital tunnel decompression with endoscopic assistance. Hand Clin. 1995;11:71-80.
94. Tsai T.M., Tsuruta T., Syed S.A., et al. A new technique for endoscopic carpal tunnel decompression. J Hand Surg Br. 1995;20:465-469.
95. Ward W.A., Siffri P.C. Endoscopically assisted ulnar neurolysis for cubital tunnel syndrome. Tech Hand Up Extrem Surg. 2009;13:155-159.
96. Mariani P.P., Golano P., Adriani E., et al. A cadaveric study of endoscopic decompression of the cubital tunnel. Arthroscopy. 1999;15:218-222.
97. Tsai T.M., Chen I.C., Majd M.E., et al. Cubital tunnel release with endoscopic assistance: results of a new technique. J Hand Surg Am. 1999;24:21-29.
98. Bultmann C. Results of endoscopic decompression of the ulnar nerve in the cubital tunnel syndrome. Handchir Mikrochir Plast Chir. 2009;41:28-34.
99. Dellon A.L., Coert J.H. Results of the musculofascial lengthening technique for submuscular transposition of the ulnar nerve at the elbow. J Bone Joint Surg Am. 2004;86-A(Suppl 1):169-179.
100. Watts A.C., Bain G.I. Patient-rated outcome of ulnar nerve decompression: a comparison of endoscopic and open in situ decompression. J Hand Surg Am. 2009;34:1492-1498.
101. Elhassan B., Steinmann S.P. Entrapment neuropathy of the ulnar nerve. J Am Acad Orthop Surg. 2007;15:672-681.
102. Filippi R., Farag S., Reisch R., et al. Cubital tunnel syndrome. Treatment by decompression without transposition of ulnar nerve. Minim Invasive Neurosurg. 2002;45:164-168.
103. Kim D.H., Han K., Tiel R.L., et al. Surgical outcomes of 654 ulnar nerve lesions. J Neurosurg. 2003;98:993-1004.
104. LeRoux P.D., Ensign T.D., Burchiel K.J. Surgical decompression without transposition for ulnar neuropathy: factors determining outcome. Neurosurgery. 1990;27:709-714. discussion 714
105. Kleinman W.B. Cubital tunnel syndrome: anterior transposition as a logical approach to complete nerve decompression. J Hand Surg Am. 1999;24:886-897.
106. Kleinman W.B., Bishop A.T. Anterior intramuscular transposition of the ulnar nerve. J Hand Surg Am. 1989;14:972-979.
107. Adson A. The surgical treatment of progressive ulnar paralysis. Collected Papers of the Mayo Clinic. 1918;10:944-951.
108. Shelden W. Tardy paralysis of the ulnar nerve. Med Clin North Am. 1921;5:499-509.
109. Eaton R.G., Crowe J.F., Parkes J.C.3rd. Anterior transposition of the ulnar nerve using a non-compressing fasciodermal sling. J Bone Joint Surg Am. 1980;62:820-825.
110. Jaddue D.A., Saloo S.A., Sayed-Noor A.S. Subcutaneous vs submuscular ulnar nerve transposition in moderate cubital tunnel syndrome. Open Orthop J. 2009;3:78-82.
111. Broudy A.S., Leffert R.D., Smith R.J. Technical problems with ulnar nerve transposition at the elbow: findings and results of reoperation. J Hand Surg Am. 1978;3:85-89.
112. Inserra S., Spinner M. An anatomic factor significant in transposition of the ulnar nerve. J Hand Surg Am. 1986;11:80-82.
113. Janjua R.M., Fernandez J., Tender G., et al. Submuscular transposition of the ulnar nerve for the treatment of cubital tunnel syndrome. Neurosurgery. 2008;63:321-324. discussion 324-325
114. Dellon A.L. Techniques for successful management of ulnar nerve entrapment at the elbow. Neurosurg Clin North Am. 1991;2:57-73.
115. Pasque C.B., Rayan G.M. Anterior submuscular transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Br. 1995;20:447-453.
116. Dellon A.L., MacKinnon S.E., Hudson A.R., et al. Effect of submuscular versus intramuscular placement of ulnar nerve: experimental model in the primate. J Hand Surg Br. 1986;11:117-119.
117. King T. The treatment of traumatic ulnar neuritis. Mobilization of the ulnar nerve at the elbow by removal of the medial epicondyle and adjacent bone. Aust N Z J Surg. 1950:33-42.
118. Mackinnon S.E., Novak C.B. Operative findings in reoperation of patients with cubital tunnel syndrome. Hand (NY). 2007;2:137-143.
119. Foster R.J., Edshage S. Factors related to the outcome of surgically managed compressive ulnar neuropathy at the elbow level. J Hand Surg Am. 1981;6:181-192.
120. Dellon A.L. Review of treatment results for ulnar nerve entrapment at the elbow. J Hand Surg Am. 1989;14:688-700.
121. Kline D., Hudson A. Nerve Injuries: Operative Results for Major Injuries, Entrapments, and Tumors. Philadelphia: WB Saunders, 1995.