Chapter 227 Management of Traumatic Bilateral Jumped Cervical Facet Joints in a Patient with Complete Myelopathy
Closed Traction Reduction Then Surgery
Experimental evidence in animals suggests that persistent compression of the spinal cord is a potentially reversible form of secondary injury and that earlier timing of decompression can lead to improved neurologic outcomes.1–3 The general conclusion is that the less severe the neurologic injury and the quicker the decompression and stabilization, the greater the chance and extent of recovery. These basic science data continue to be the foundation that supports many clinicians’ rationale for performing urgent decompression and fixation in patients with spinal cord injury (SCI). A recent systematic review of the literature failed to establish guidelines for timing of surgical decompression and fixation in the setting of SCI, owing to the lack of high-quality evidence.4 However, the authors concluded that the evidence supports guidelines for urgent closed reduction in patients with bilateral locked facets and an incomplete SCI to maximize the potential for enhanced neurologic outcome.4–9 While there may be no single best method of treatment for all patients with bilateral locked facets, this chapter discusses the goals of treatment and methods for reaching those goals, particularly in patients with complete SCI. Discussion is focused on early closed reduction followed by surgery. Evidence to support early closed reduction followed by surgery is presented. Traction and reduction techniques, as well as surgical treatment algorithms, are described.
Patients with complete, or grade A, American Spinal Injury Association (ASIA) SCIs are often considered to have little capacity for neurologic recovery. However, Frankel et al. reported on a cohort of over 600 patients that showed that almost 30% of the complete SCIs improved at least one grade and that the number of patients with neurologic deterioration was minimal.10 It might be more accurately stated that some patients with ASIA A injuries are likely to have neurologic recovery, the extent of which tends to be unpredictable or more limited than is the case for patients with incomplete injuries. It should also be noted that it is often difficult to be certain of the presence or absence of sacral sparing in the initial assessment of a patient because of confounding factors such as polytrauma, obtunded state, or spinal shock. Mirza et al. and others concluded that it is quite difficult to differentiate a complete and an incomplete SCI in the early postinjury time frame.8,11 Late conversion from complete to incomplete can also occur.11 Therefore, Mirza et al. recommended treating all SCIs as potentially incomplete SCIs.8
Patient Assessment
When a fracture or dislocation is diagnosed in the cervical spine, complete imaging of the spinal axis is recommended, owing to the relatively high risk of noncontiguous fractures.12 In the radiographic assessment of the patient, particular attention should be paid to assessing fracture or potential instability cephalad to the known injury. This is especially important if the use of traction or closed manipulation is planned for reduction. CT scan has gained wide acceptance for its ability to rapidly image the bony structures of the spine with excellent detail.13 Despite a general increase in frequency of CT scan usage for diagnostic cervical trauma imaging, it is still vitally important to appreciate the subtleties of radiologic findings on plain radiographs, as these images are often important in determining the effect of closed reduction attempts or intra-operative alignment.
The use of MRI in the setting of bilateral locked facets continues to be a source of considerable debate. While the diagnostic accuracy and information provided to the treating surgeon are not in question,14 the patient selection, timing, and application of treatment algorithms are still not completely standardized. In considering application of traction for attempted closed reduction, MRI or CT myelogram have been advocated.15,16 The primary concern is that an unrecognized cervical disc herniation, in the setting of bilateral facet dislocation, may produce spinal cord compression if closed reduction is attempted.17 The case reports of neurologic deterioration after closed reduction of facet dislocation, secondary to disc herniation, tended to involve reductions that were performed under general anesthesia or were done openly during operative reduction.16,18,19 Some authors suggest that performing an MRI prior to reduction not only delays time to reduction but also puts the patient at risk of further injury during transport.17,20 Ordonez et al. found that disc herniations occurred in up to 50% of patients with facet dislocations, but fewer than 1% sustained permanent neurologic deficit following reduction.21 Potential causes of worsening neurologic condition included overdistraction, failure to appreciate more rostral injuries, epidural hematoma, and spinal cord edema. Therefore, Ordonez et al. stated that an MRI does not need to be obtained prior to reduction in the alert, examinable patient. However, they did recommend MRIs in patients who cannot be examined during reduction or in patients that fail closed reduction. Vaccaro et al. documented a higher frequency of disc herniations after closed reduction in awake, alert patients, compared to patients who had prereduction imaging. In this series, they did not show any correlation with neurologic deterioration.14 Darsaut et al. performed traction on 17 patients under MRI guidance. Four of 17 patients initially had dorsal disc displacement, and 15 had disc disruption prior to attempted closed reduction. Darsaut et al. were able to show that canal dimension improved in 11 of 17 cases and that the process of reduction under traction and improvement of canal dimensions was a gradual one.22
Neurologic Case for Rapid Closed Reduction by Means of Traction
In 1987, Brunette and Rockswold presented a report of complete neurologic recovery following C3 on C4 fracture dislocation.23 Upon initial presentation, the patient was awake and alert and had slight difficulty breathing. He was initially able to flicker his left foot but was otherwise flaccid in both upper and lower extremities, had no sensation distal to the C4 distribution, and had absent rectal tone. The patient had gentle traction and immobilization applied on the scene by paramedics. Thirty minutes after the injury, the patient was no longer able to flicker his left foot.
Although these results are quite impressive, two factors must be considered. This patient did not have a complete cord injury at initial presentation, as is evident by the ability to flicker his left foot. Also, the patient underwent decompression and stabilization by traction extremely quickly at 90 minutes. Of note, traction was not delayed for a prereduction MRI, as the patient was alert and capable of reporting neurologic changes during traction. For a multitude of reasons, it is rarely possible to reduce patients so quickly; however, this study suggests that emergent traction management, when possible, may lead to improved neurologic recovery. In 1994, Lee et al. evaluated two mechanisms of closed reduction of facet dislocations in addition to the significance of time to reduction.24 They performed a retrospective review of 210 patients with either unilateral or bilateral facet dislocations. None of the patients received MRIs prior to reduction. Ninety-one patients underwent manipulation under anesthesia (MUA), while 119 underwent rapid traction, 5 pounds every 1 to 2 minutes up to 20 pounds followed by 10-pound increments up to 150 pounds until reduction was achieved, at which point the weight was reduced to 5 pounds. The average patient with bilateral facet dislocations was reduced at 81 pounds. MRI-compatible tongs bend and lose fixation at weights above 55 pounds; therefore, reductions requiring more than 55 pounds require consideration of four pins, halo, or double tongs. This study evaluated the timing of reduction via traction. Reduction within 12 hours led to improved Frankel grades (26%) as compared to reduction delayed more than 12 hours (8%). However, it is important to note that neurologic improvement was observed in both the immediate and delayed-reduction groups. Time to reduction did not affect neurologic recovery in the MUA group. Of failures of reduction in the traction group, 14 (12%) were related to associated fractures, delayed presentation, or tong pull-out. Seventy-three percent of MUA patients were successfully reduced. Six patients had deteriorating neurologic level after MUA, which is believed to be related to general anesthesia causing decreased blood supply to the cord in the acute phase of injury. The authors promote avoiding MUA in the conscious patient, as it increases the risk of worsening neurologic status and had a lower rate of successful reduction. They also argued that MRI/CT myelography or open ventral surgery is not necessary prior to reduction because neurologic deterioration after reduction occurs in fewer than 1% of cases. They state that the risk of delayed reduction is more detrimental than the risks of rapid reduction. Therefore, these authors advocated immediate rapid reduction, without prereduction MRI or CT myelography, with weights up to 150 pounds for the initial management of cervical spine dislocations.
The role of traction and the importance of timing were evaluated in 2002 in a systematic literature review.25 The authors concluded that early closed reduction by traction was safe and effective in awake patients with approximately an 80% success rate. The focus of this review was to suggest that obtaining MRI presents an unnecessary delay to reduction. While the evidence presented suggested that prereduction MRI was not valuable, no evidence was presented to suggest that the time delay of the MRI was relevant to neurologic recovery. Therefore, this study recommended early closed reduction with limited evidence of the significance of timing to reduction.
In 2004, Anderson et al. focused on the significance of time to reduction in a retrospective review of patients who sustained traumatic unilateral and bilateral facet dislocations.20 The medical records of 45 patients were reviewed to assess the significance of age, gender, initial motor score, and time to reduction in predicting neurologic recovery. In this analysis, 88.8% of patients were successfully reduced using closed traction. The authors reported that younger age (P = .01) and better initial summed motor score (P < .01) correlated significantly with greater motor recovery after traumatic facet dislocation. They also found an overall average improvement in motor score of approximately 30% after 6 months. This study did not find that time to reduction was a significant predictor of neurologic recovery. However, they acknowledge the limitation that the study evaluated only 45 patients and did not look at subsets of patients such as those with narrow therapeutic windows or specific ASIA scores. These studies show the controversial role of timing of reduction in facet dislocations.
Treatment Options
One of the early studies that attempted to define a treatment protocol was reported in 1981 when Sonntag published a case series of 15 patients treated for bilateral locked facets of the cervical spine.26 Ten patients were close reduced, six with manual reduction and four with traction. Five patients were managed with open dorsal reduction and fusion. This was because of a more rostral injury in one patient, fractures of the locked facets in two patients, and increasing neurologic deficit upon attempts at traction in two patients. All 15 patients, including those who were managed operatively and nonoperatively, had stable cervical spines at follow-up. The author recommends initial management of bilateral locked cervical facets with traction first. If that fails, the author recommends closed reduction via manipulation. Failure to reduce the patient with these mechanisms requires open management. This early study attempted to give recommendations of management for bilateral locked facets. Vaccaro et al. reiterate this sentiment on the basis of extensive clinical experience and pre/post reduction MRI data.14 Rapid cervical spine reduction with traction has been shown to be safe and effective in the awake and examinable patient.24,27,28 Hart explained the rationale for the role and timing of prereduction MRI as hinging significantly on the neurologic exam.17 If a patient is ASIA A, ASIA B, or a bad ASIA C, it can be assumed that the potential neurologic benefit of rapid reduction with traction outweighs the potential downside of delay that comes with getting an MRI.17
Traction Techniques
Once the halo or tongs have been applied, traction should be started at 5 to 10 pounds for the head and then increased gradually by about 5 pounds per level with a neurologic exam being performed as each weight increment is increased. Radiographic imaging should be used intermittently to assess for reduction. Weights upward of 140 pounds have been reported to be safe and effective to achieve reduction.28 Varying degrees of neck flexion (which can be achieved by placing a towel or roll under the head) may facilitate unlocking of the facets. Once the spine is sufficiently distracted or flexed and distraction and reduction have been achieved, the neck will eventually need to be slightly extended to maintain reduction, and typically, a portion of the traction weight can be removed. If reduction is accomplished, the clinician then has to decide how best to obtain definitive stabilization. If closed-reduction attempts fail, it is recommended that urgent surgical open reduction be performed. At this point, MRI may be helpful to aid in surgical planning. Some researchers argue that performing a ventral approach with discectomy obviates the need for preoperative MRI because the disc herniation that may be present will be removed surgically regardless. Others suggest that preoperative MRI may help for planning if disc fragments are behind the vertebral body and require partial or complete corpectomy.17
In 2000, Ordonez et al. reported an alternative to the classically described closed reduction of cervical facet dislocations.21 Ten patients with cervical facet dislocations were treated with open ventral reduction and stabilization without prior attempts at closed reduction. In this study, all patients underwent plain radiography, CT, and MRI prior to surgery. Five of the 10 patients had evidence of traumatic disc herniation. All 10 patients underwent ventral decompression, reduction, and stabilization. Discectomy was performed first, which occasionally required resection of the caudal margin of the rostral vertebral body for visualization purposes. Reduction was achieved by placing a distractor pin in each vertebral body at a 10- to 20-degree divergent angle. Pins can then be moved to create kyphosis and disengage the facets. Dorsal pressure is then applied to the rostral body to obtain sagittal realignment, and disc interspace spreaders are used to complete the reduction. Iliac crest bone graft and a ventral cervical fixation device were used to achieve fusion. Using this technique, eight of 10 patients had complete reduction and fusion, one had a persistent unilateral perched facet but fused and was asymptomatic, and the tenth was not able to be reduced ventrally and, after discectomy, underwent dorsal reduction and fusion. No patients suffered worsening of their preoperative neurologic state, and many patients improved. Payer examined five patients who were found to have bilateral locked facets.29 Four out of five had complete spinal cord injuries, ASIA A, while the fifth patient was neurologically intact. All five patients were awake and hemodynamically stable. Rather than attempting initial closed reduction, these patients were all brought directly, within 8 hours of injury, to the operating room for open ventral cervical discectomy, facet reduction, and circumferential fusion. The neurologically intact patient remained intact, and the four patients with grade A injuries each regained a single level of function. The author argues that closed reduction is unsuccessful 25% of the time, delaying operative management and causing significant patient discomfort. Also, the open ventral approach allows for disc removal in the event of traumatic herniated disc, eliminating the need for and delays of MRI.29
Synthesis of Treatment Algorithms
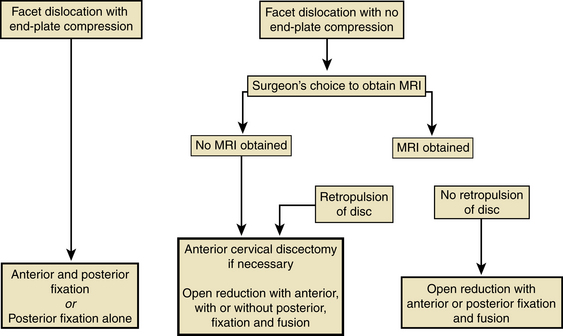
On the basis of the previously presented data and reports, a good case can be made for treating patients with complete SCI and bilateral locked facets, first with traction and closed reduction, then with surgical stabilization. Neurology and patient factors are key components that may help to guide initial treatment decisions in favor of other pathways to definitive management. On the basis of the Spine Trauma Study Group’s evidence-based evaluation of the literature, Dvorak et al. developed a surgical treatment algorithm for facet dislocation.30 If there is no preoperative dorsal disc herniation based on MRI, then the surgeon can choose to perform ventral or dorsal reduction and fusion. Decision making in this case is based on patient factors and surgeon preference. Surgeons may be more familiar or comfortable with one technique over another or may have certain equipment available that dictates or sways the decision making. The dorsal approach to the cervical spine involves a higher risk of infection, more pain, and a slightly longer hospital stay.31 Fehlings et al. found that dorsal fixation alone leads to higher degrees of segmental kyphosis, which is of uncertain clinical significance.32 Ventral surgical approaches tend to involve less pain and shorter hospital stay but have a higher likelihood of dysphonia and dysphagia. Patient factors are also important in the surgical decision-making process, and some factors such as previous or potential scarring, dysphagia or aspiration risk (which may be more exaggerated in the elderly), or potential dysphonia may be more important to some patients than to others. Although some biomechanical studies have shown that ventral discectomy and fusion alone are biomechanically inferior to dorsal fixation or ventral and dorsal fixation combined,30 most studies show that the use of ventral fixation alone returns the spine to at least the stability of the intact motion segment, and multiple clinical series have shown successful healing and clinical outcomes.30,33,34
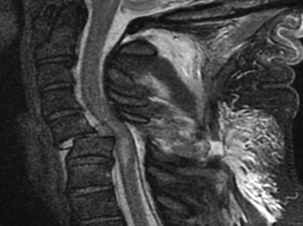
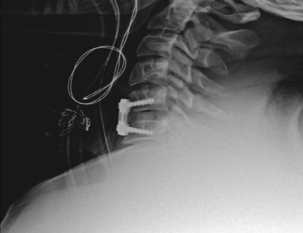
It is generally well accepted that if disc material is persistently displaced dorsal to the cortex of the more caudal vertebral level, especially if reduction has not been obtained, the surgeon’s choice, at least initially, should be to perform a ventral approach.30,35,36 If an all-ventral approach is performed, it is important to maximize the stability of the construct by generating lordosis and locking the facets back into maximum extension.29 Surgeon preference and judgment about stability will dictate the decision to supplement with dorsal fixation. As was stated previously, dorsal fixation can stand alone and provide adequate stability in this mainly dorsal ligamentous injury. A contraindication to stand-alone ventral cervical fixation would be present if the patient had a concomitant end-plate compression fracture (typically at the superior end plate of the caudal level).37 Johnson et al. found that when patients were fixed ventrally alone in the setting of an end-plate compression fracture and a facet fracture, subluxation, or dislocation, nearly two thirds had early mechanical failure.37 For this reason, Johnson and others have favored a combined ventral and dorsal or all-dorsal approach in the setting of end-plate compression fracture and facet dislocation.30,31,37 Figure 227-1 is the lateral cervical spine radiograph of a patient who was intoxicated and fell down the stairs. He presented as a C5 ASIA B with bilateral dislocated facets at C5-6. Figures 227-1, 227-2, and 227-3 show prereduction radiograph, CT, and MRI, respectively. A closed reduction attempt was unsuccessful; therefore, open reduction and ventral cervical discectomy and fusion with iliac crest bone graft were performed. Immediate postoperative supine images were obtained (Fig. 227-4). The patient’s neck pain was improving until postoperative day three, when he began to have an acute increase in neck pain. A radiograph revealed graft subsidence (Fig. 227-5), which, after closer inspection of the preoperative CT scan, appeared to be the result of a very subtle superior end-plate fracture of C6 that was not appreciable preoperatively or intraoperatvely (Fig. 227-6). The patient was brought back to the operating room for dorsal fixation (Fig. 227-7), and his pain improved.

FIGURE 227-1 Lateral radiograph of the cervical spine demonstrating bilateral facet dislocations at the C5-6 level.

FIGURE 227-2 Sagittal CT of the cervical spine demonstrating bilateral facet dislocations at the C5-6 level.
Conclusions
The flowchart in Figure 227-8 illustrates the decision-making process for operative treatment of bilateral locked facets with SCI using an evidence-based systematic review of the spine trauma literature.30 There are no definitive treatment guidelines to address the care of patients presenting with locked facets and SCI with respect to timing and exact method of treatment. However, it is clear that the spine should be decompressed and definitively stabilized at some point. The main arguments pertain to the timing and application of initial treatment strategies. Many researchers argue that prereduction MRIs represent a delay to decompression and stabilization without added benefit to the patient. Although it has been suggested that retropulsion of a herniated disc during reduction may lead to neurologic decompensation, the majority of studies now indicate that retropulsed discs rarely lead to neurologic decompensation and that MRIs may be unable to predict all of these circumstances. Therefore, MRIs do not appear to be necessary prior to reduction in the awake and alert patient. However, some studies indicate that they may be beneficial in patients who fail closed reduction or in patients who are undergoing immediate operative management without prior attempts at closed reduction. Still other studies indicate that immediate operative decompression and stabilization without MRI is a viable alternative to initial closed reduction. Many patients present to hospitals that are not equipped to perform immediate surgical management of these injuries, however. In this situation, initial decompression via manual reduction or traction is the preferred treatment until operative fixation can be obtained. In conclusion, there is not enough evidence to define a clear algorithm for presurgical treatment for patients with facet dislocations and SCI, but the goal of both initial and definitive treatment is clear: decompression and stabilization. The options presented in this chapter should form the basis for thoughtful choice and decision making to enhance neurologic recovery and obtain stable spine fixation.
Anderson G.D., Voets C., Ropiak R., et al. Analysis of patient variables affecting neurologic outcome after traumatic cervical facet dislocation. Spine J. 2004;4:506-512.
Darsaut T.E., Ashforth R., Bhargava R., et al. A pilot study of magnetic resonance imaging-guided closed reduction of cervical spine fractures. Spine (Phila Pa 1976). 2006;31:2085-2090.
Dvorak M.F., Fisher C.G., Fehlings M.G., et al. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976). 2007;32:2620-2629.
Fehlings M.G., Perrin R.G. The timing of surgical intervention in the treatment of spinal cord injury: a systematic review of recent clinical evidence. Spine (Phila Pa 1976). 2006;31:S28-S35. discussion S36
Kwon B.K., Fisher C.G., Boyd M.C., et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1-12.
Papadopoulos S.M., Selden N.R., Quint D.J., et al. Immediate spinal cord decompression for cervical spinal cord injury: feasibility and outcome. J Trauma. 2002;52:323-332.
1. Carlson G.D., Minato Y., Okada A., et al. Early time-dependent decompression for spinal cord injury: vascular mechanisms of recovery. J Neurotrauma. 1997;14:951-962.
2. Dimar J.R.2nd, Glassman S.D., Raque G.H., et al. The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine (Phila Pa 1976). 1999;24:1623-1633.
3. Delamarter R.B., Sherman J., Carr J.B. Pathophysiology of spinal cord injury: recovery after immediate and delayed decompression. J Bone Joint Surg [Am]. 1995;77:1042-1049.
4. Fehlings M.G., Perrin R.G. The timing of surgical intervention in the treatment of spinal cord injury: a systematic review of recent clinical evidence. Spine (Phila Pa 1976). 2006;31:S28-S35. discussion S36
5. Papadopoulos S.M., Selden N.R., Quint D.J., et al. Immediate spinal cord decompression for cervical spinal cord injury: feasibility and outcome. J Trauma. 2002;52:323-332.
6. Tator C.H., Fehlings M.G., Thorpe K., et al. Current use and timing of spinal surgery for management of acute spinal surgery for management of acute spinal cord injury in North America: results of a retrospective multicenter study. J Neurosurg. 1999;91:12-18.
7. Dall D.M. Injuries of the cervical spine. II. Does anatomical reduction of the bony injuries improve the prognosis for spinal cord recovery? S Afr Med J. 1972;46:1083-1090.
8. Mirza S.K., Krengel W.F.3rd, Chapman J.R., et al. Early versus delayed surgery for acute cervical spinal cord injury. Clin Orthop Relat Res. 1999;359:104-114.
9. Harris P., Karmi M.Z., McClemont E., et al. The prognosis of patients sustaining severe cervical spine injury (C2-C7 inclusive). Paraplegia. 1980;18:324-330.
10. Frankel H.L., Hancock D.O., Hyslop D., et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 1969;7:179-192.
11. Waters R.L., Yakura J.S., Adkins R.H., et al. Recovery following complete paraplegia. Arch Phys Med Rehabil. 1992;73:784-789.
12. Vaccaro A.R., An H.S., Lin S., et al. Noncontiguous injuries of the spine. J Spinal Disord. 1992;5:320-329.
13. Parizel P.M., van der Zijden T., Gaudino S., et al. Trauma of the spine and spinal cord: imaging strategies. Eur Spine J. 2009;19(Suppl 1):8-17.
14. Vaccaro A.R., Falatyn S.P., Flanders A.E., et al. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine (Phila Pa 1976). 1999;24:1210-1217.
15. Doran S.E., Papadopoulos S.M., Ducker T.B., et al. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993;79:341-345.
16. Eismont F.J., Arena M.J., Green B.A. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Joint Surg Am. 1991;73:1555-1560.
17. Hart R.A. Cervical facet dislocation: when is magnetic resonance imaging indicated? Spine (Phila Pa 1976). 2002;27:116-117.
18. Olerud C., Jonsson H.Jr. Compression of the cervical spine cord after reduction of fracture dislocations: report of 2 cases. Acta Orthop Scand. 1991;62:599-601.
19. Robertson P.A., Ryan M.D. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. J Bone Joint Surg [Br]. 1992;74-B:224-227.
20. Anderson D.G., Voets C., Ropiak R., et al. Analysis of patient variables affecting neurologic outcome after traumatic cervical facet dislocation. Spine J. 2004;4:506-512.
21. Ordonez B.J., Benzel E.C., Naderi S., Weller S.J. Cervical facet dislocation: techniques for ventral reduction and stabilization. J Neurosurg. 2000;92:18-23.
22. Darsaut T.E., Ashforth R., Bhargava R., et al. A pilot study of magnetic resonance imaging-guided closed reduction of cervical spine fractures. Spine (Phila Pa 1976). 2006;31:2085-2090.
23. Brunette D.D., Rockswold G.L. Neurologic recovery following rapid spinal realignment for complete cervical spinal cord injury. J Trauma. 1987;27:445-447.
24. Lee A.S., MacLean J.C., Newton D.A. Rapid traction for reduction of cervical spine dislocations. J Bone Joint Surg [Br]. 1994;76:352-356.
25. Initial closed reduction of cervical spine fracture-dislocation injuries. Neurosurgery. 2002;50:S44-S50.
26. Sonntag V.K. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1981;8:150-152.
27. Star A.M., Jones A.A., Cotler J.M., et al. Immediate closed reduction of cervical spine dislocations using traction. Spine (Phila Pa 1976). 1990;15:1068-1072.
28. Cotler J.M., Herbison G.J., Nasuti J.F., et al. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Spine (Phila Pa 1976). 1993;18:386-390.
29. Payer M. Immediate open anterior reduction and antero-posterior fixation/fusion for bilateral cervical locked facets. Acta Neurochir (Wien). 2005;147:509-513. discussion 513–514
30. Dvorak M.F., Fisher C.G., Fehlings M.G., et al. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976). 2007;32:2620-2629.
31. Kwon B.K., Fisher C.G., Boyd M.C., et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1-12.
32. Fehlings M., Cooper P.R., Errico T.J., et al. Posterior plates in the management of cervical instability: long term results in 44 patients. J Neurosurg. 1994;18:341-349.
33. Ianuzzi A., Zambrano I., Tataria J., et al. Biomechanical evaluation of surgical constructs for stabilization of cervical teardrop fractures. Spine J. 2006;6:514-523.
34. Dvorak M.F., Pitzen T., Zhu Q., et al. Anterior cervical plate fixation: a biomechanical study to evaluate the effects of plate design, endplate preparation, and bone mineral density. Spine (Phila Pa 1976). 2005;30:294-301.
35. Razack N., Green B.A., Levi A.D. The management of traumatic cervical bilateral facet fracture-dislocations with unicortical anterior plates. J Spinal Disord. 2000;13:374-381.
36. Lifeso R.M., Colucci M.A. Anterior fusion for rotationally unstable cervical spine fractures. Spine (Phila Pa 1976). 2000;25:2028-2034.
37. Johnson M.G., Fisher C.G., Boyd M., et al. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine (Phila Pa 1976). 2004;29:2815-2820.
Open Reduction
Bilateral jumped/locked facet injury in the cervical spine is usually the result of a flexion-distraction injury in which there is complete circumferential ligamentous disruption. The nature of these injuries predisposes a large percentage of the patients to have MRI evidence of substantial disc material ventral to the cord. In fact, Rizzolo et al.1 found evidence of disc disruption or herniation in 54% of patients with prereduction MRI. However, the clinical relevance of these findings has not yet been proven, as prereduction MRI has not been shown to improve the safety or efficacy of closed traction/reduction in an awake patient. Moreover, an analysis of closed reduction for subaxial cervical fracture-dislocation injuries reveals that failure of closed reduction is more common with facet dislocation injuries. Overall, 30% of these injuries had recurrent displacement or inadequate alignment during external immobilization or reduction.2
The risks of closed reduction, with concern for inadequate immobilization, overdistraction, unrecognized rostral injuries, and loss of reduction, have led many surgeons to opt for initial open reduction in patients with this type of injury. In a review of the literature, open reduction was achieved in all but 1 of 24 patients who were treated with ventral fusion procedures and in all but 7 of 167 patients who were treated with dorsal fusion.2 Delayed instability and later development of kyphotic angulation in patients who were treated with either ventral and/or dorsal instrumented fusions is uncommon. In general, patients with clinically significant ventral spinal cord compression, that is, disc herniation or epidural hematoma, should be treated initially with a ventral approach. Otherwise, the literature has not demonstrated a clear clinical benefit to ventral reduction/stabilization over dorsal reduction/stabilization.