Chapter 179 Management of Sacral Fractures
Anatomic and Biomechanical Considerations
The sacrum is the foundation of the spinal column, providing an anchor for the mobile lumbar spine. Compared to the remainder of the lumbar spine, the lumbosacral articulation is inherently more stable than more cephalad lumbar motion segments because of the presence of additional ligamentous stabilizers in the form of (1) the iliolumbar ligaments, which extend from the L5 transverse processes to the iliac crests, and (2) the sacrolumbar ligaments that originate contiguously with the iliolumbar ligament and insert into the anterosuperior aspect of the sacrum and sacroiliac joint.1
The sacrum has a forward inclination that is balanced by the usual lumbar lordosis, allowing a plumb line to normally extend from C7 to the posterior aspect of the L5-S1 intervertebral disc. The sacral inclination angle varies from 10 to 90 degrees and usually ranges between 45 and 60 degrees.2,3 Pelvic incidence, which measures the orientation of the lumbosacral junction relative to the pelvis, can be a valuable method for determining sagittal alignment when treating sacral fractures and is usually approximately 50 degrees.4 Sacral fractures that significantly alter spinal sagittal alignment may result in difficulty with maintaining an erect posture, compensatory lumbar malalignment, and associated pain and functional deficits.5
The sacrum also forms the posterior aspect of the pelvic ring and has therefore been described as the keystone of the pelvic ring,6 because it maintains stability while transmitting forces from the lumbosacral articulation across the sacroiliac joints to the pelvis. This keystone function is particularly true in the pelvic outlet plane, in which the orientation of the sacrum relative to the ilium is such that axial forces lock the sacrum into the pelvic ring and further stabilize the sacroiliac articulation. In the pelvic inlet plane, the sacrum is shaped like a “reverse keystone,” which is more inherently unstable and therefore requires substantial intrinsic and extrinsic ligamentous stabilization of the sacroiliac joints while permitting pelvic ring motion.7
The osseous sacral anatomy comprises five kyphotically aligned, fused vertebral segments, with significant variability in upper sacral anatomy in the form of transitional vertebrae and sacral dysplasia.8,9 Because upper sacral variability results in significant alteration in the relationships among the sacrum, pelvis, and spinal column relative to their adjacent neurovascular structures, these variations must be recognized, particularly if surgical treatment of sacral fractures is being considered.10
The upper sacral body has the densest sacral cancellous bone, particularly adjacent to the superior S1 end plate. The ventral aspect of the upper S1 body that projects anteriorly and superiorly into the pelvis is termed the sacral promontory. The sacral ala, the lateral portion of the sacrum that articulates with the ilium through the sacroiliac joints, is largely cancellous and is formed by the coalescence of the sacral transverse processes. The cancellous alar bone is hypodense, particularly in older individuals, and an alar void is a consistent finding in middle-aged and older adults.11,12 The relative difference in bone density between the upper and the lower sacral body predisposes this area to fracture. The hypodense ala is predisposed, particularly in older and osteopenic patients, to fracture line propagation. This problem is accentuated by the relative strength of the sacroiliac joint ligaments. Similarly, younger individuals injured before complete ossification of the sacrum are predisposed to disruption at the S1-2 level because of relative weakness at that interval. The suboptimal alar bone density must be taken into consideration when planning reconstructive procedures.
The posterior surface of the sacrum is convex and is formed by the coalescence of posterior elements. The middle sacral crest corresponds to the spinous processes, the intermediate sacral crests correspond to the zygapophyseal joints, and the area between corresponds to the laminae. The lowest one or two sacral segments have incompletely formed bony posterior elements, resulting in an aperture into the sacral spinal canal known as the sacral hiatus. Enlargement of the sacral hiatus may weaken the sacrum and predispose it to fracture.13
The dural sac typically ends at the S2 level, and the filum terminale attaches its caudal end to the coccyx. At the junction of the body and the sacral ala are four paired ventral and dorsal neuroforamina through which the ventral and dorsal rami of the sacral nerve roots pass. The relative space available to the sacral nerve roots in the ventral foramina is lowest at the S1 and S2 levels, where the nerve roots occupy one third to one fourth of the foraminal space, compared with the S3 and S4 levels, where the nerve roots occupy one sixth of the available foraminal space. The lower sacral roots are therefore less likely to be impinged upon in injuries involving displacement of the neuroforamina.14
The dorsal nerve roots exit through their respective posterior neuroforamina to supply motor branches to the paraspinous muscles and cutaneous sensory branches that form the cluneal nerves. Anteriorly, the L5 nerve root passes underneath the inferior edge of the sacrolumbar ligament and drapes over the anterosuperior aspect of the sacral ala.15 It anastomoses with the L4 ventral ramus and is joined by the exiting ventral sacral nerve roots as it passes caudally along the sacral ala to form the sacral plexus.16 The dual innervation of the perineal structures from both the left and the right sacral plexus is protective of bowel, bladder, and sexual function. These functions are largely preserved in the event of unilateral transection of the sacral nerve roots, whereas bilateral transection causes complete loss of function.17
The presacral area has an extensive and highly variable vascular network. The middle sacral artery typically courses ventrally along the midline of the L5 vertebral body and the sacrum after branching from the aorta at the common iliac bifurcation. The common iliac arteries subsequently give rise to the internal iliac arteries that lie anterior to the sacroiliac joints and give off both superior and inferior lateral sacral arteries. The superior lateral sacral artery courses caudally, just lateral to the sacral foramina, and supplies the spinal canal through the S1 and S2 ventral foramina, whereas the inferior lateral sacral artery traverses the inferior aspect of the sacroiliac joint before anastomosing with the middle sacral artery and giving off spinal arteries that pass through the S3 and S4 ventral foramina.9 The internal iliac veins lie posteromedial to the internal iliac arteries and course caudally. They are located medial to the sacroiliac joint directly adjacent to the sacral ala.15 The internal iliac veins give rise to an extensive presacral venous plexus, formed by anastomoses between the lateral and the middle sacral veins that communicate transforaminally with the epidural veins in the spinal canal.1,8,18 This extensive vascular network renders anterior exposures to the sacrum impractical and perilous.
Classification
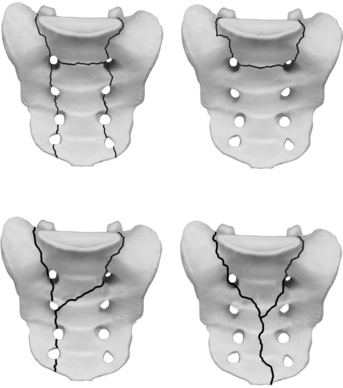
Although several sacral fracture classification systems have been proposed,19–21 none was widely adopted until 1988, when Denis et al. described an anatomic classification that correlated fracture location with the presence of neurologic injury.14 This classification divides the sacrum into three zones (Fig. 179-1). Zone I (alar zone) fractures remain lateral to the neuroforamina. Zone II (foraminal zone) fractures involve one or more neuroforamina while remaining lateral to the spinal canal. Zone III (central zone) fractures involve the spinal canal. Denis et al. observed a greater likelihood of neurologic injury as fractures occurred more medially. In their series, zone I fractures had a 5.9% incidence of neurologic injury, primarily to the L5 nerve root as it courses over the ala. Zone II fractures had a 28.4% incidence of neurologic injury due to either foraminal displacement, and resulting impingement on the exiting nerve root, or “traumatic far-out syndrome,” in which the L5 nerve root is caught between the L5 transverse process and the displaced sacral ala. Zone III fractures had a 56.7% incidence of neurologic deficits resulting from injury within the spinal canal, with 76.1% of these individuals having bowel, bladder, and sexual dysfunction. Although Denis et al. noted a broad spectrum of zone III sacral fracture–dislocations, including the presence of both transverse and longitudinal fracture line orientations, zone III sacral fractures were more formally characterized by other authors, as described next.
Gibbons et al. studied 44 cases of sacral fracture according to the Denis classification system and found a 34% incidence of neurologic injury. They used these results as a basis for classifying neurologic injury caused by sacral fractures,22 which they classified as 1, none; 2, paresthesias only; 3, motor loss with bowel and bladder intact; and 4, bowel and/or bladder dysfunction. They reported neurologic injury in 24% of zone I injuries, 29% of zone II injuries, and 60% of patients with zone III injuries. Neurologic deficits with zone I and II injuries involved primarily the L5 and S1 roots. While no patient with zone I or II injuries had bowel or bladder dysfunction, two of the three patients with zone III injuries and neurologic deficits had bladder dysfunction. Though useful, this classification system may be insufficiently detailed to be meaningful as a clinical outcomes measurement tool.
Because of their neurologic and biomechanical implications, Denis zone III fractures have been further categorized by several investigators. Review of various series and case reports reveals a high likelihood of neurologic deficit characterized as cauda equina injury affecting lower extremity, as well as bowel and bladder, function.20,21,23–36
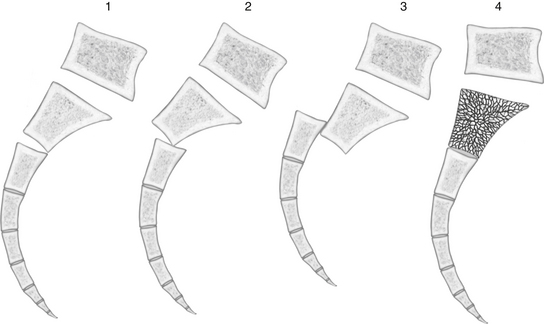
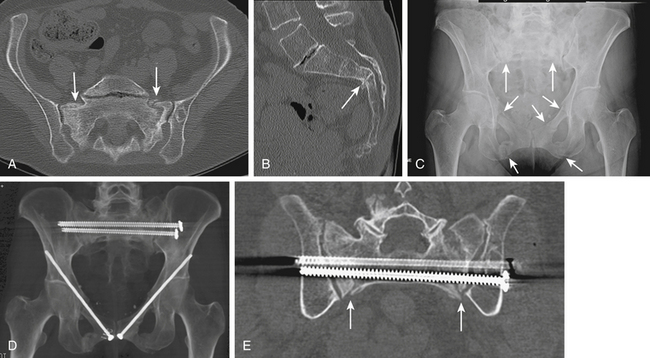
Early case reports often characterized the zone III injury pattern as solely a transverse fracture, possibly because of imaging limitations. Computed tomography (CT) demonstrates that most transverse fractures of the upper sacrum have complex, three-dimensional fractures patterns. The majority of these injuries are now understood to consist of a transverse fracture of the sacrum with associated “longitudinal” or “vertical” transforaminal and/or alar fractures that extend rostrally to the lumbosacral junction to form the so-called U fracture and its variations (e.g., H, Y, and lambda fracture patterns) (Fig. 179-2). These fractures are also characterized by a high incidence of L5 transverse process fractures, indicating disruption of the iliolumbar ligament.33
Roy-Camille et al. reported a series of 13 patients with transverse sacral fractures, which they classified as type 1, flexion deformity of the upper sacrum (angulation alone); type 2, flexion deformity with posterior displacement of the upper sacrum (angulation and posterior translation); and type 3, anterior displacement of the upper sacrum without angulation (anterior translation alone). Based on cadaveric studies, they hypothesized that types 1 and 2 were caused by impact with the lumbar spine in flexion, whereas type 3 fractures were caused by impact with the lumbar spine and hips in extension.37 Strange-Vognsen and Lebech added the type 4 injury, theorizing that comminution of the upper sacrum without significant angulation or translation was caused by impact with the lumbar spine in the neutral position38 (Fig. 179-3). A type 5 direct impalement–type injury has recently been proposed by Schildhauer et al.39
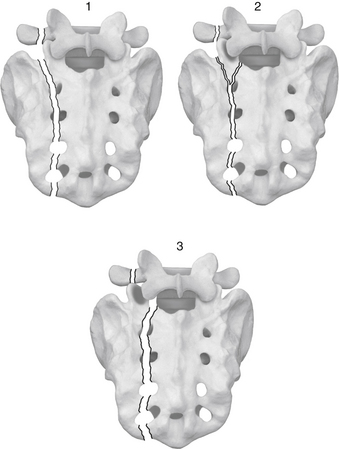
Other patterns of zone III sacral fractures have been identified as resulting from specific mechanisms or having predictable patterns of associated injuries. In contrast to transverse Denis zone III sacral fractures, midline longitudinal Denis zone III sacral fractures, in which the sacrum is disrupted through the sagittal plane, have a low incidence of neurologic injury (Fig. 179-4).40–42 This injury, was originally reported by Wiesel et al. in 1979, who suggested that the lower incidence of neurologic injury compared to transverse fractures is the result of nerve roots being subjected to a lateral displacement force rather than a shear force.42 Bellabarba et al. subsequently described this injury as a variant of the anteroposterior compression pelvic ring injury, in which none of their series of 10 patients had neurologic deficits, in contrast to the high incidence of neurologic injury reported in patients with predominantly transverse sacral fractures involving the spinal canal.40
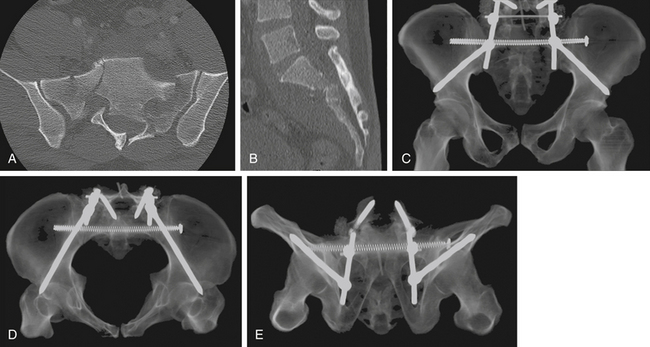
Isler demonstrated that, even in the absence of a transverse fracture line, sacral fractures can be associated with spinal column instability. He described variations of longitudinal sacral fractures through the S1 and S2 neuroforamina that result in L5-S1 instability because of facet joint disruption43 (Fig. 179-5). Injuries with the fracture line lateral to the S1 articular process are not associated with instability of the lumbosacral articulation since the L5-S1 articulation remains continuous with the stable component of the sacrum. Fractures that extend into or medial to the S1 articular process, however, may disrupt the associated facet joint and potentially destabilize the lumbosacral junction. Complete displacement of the facet joint can cause a locked facet joint, making sacral fracture reduction difficult with closed methods alone. Facet disruption may also cause post-traumatic arthrosis and late lumbosacral pain.
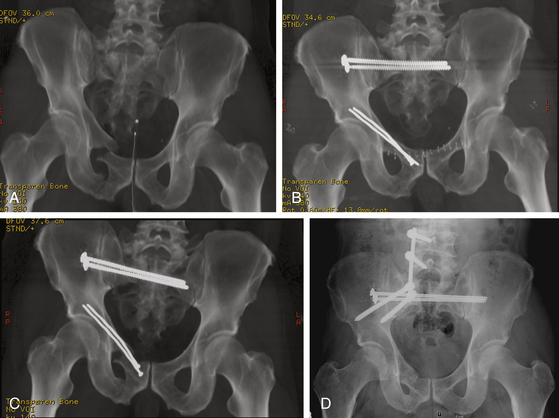
In contrast to sacral fractures that occur as a result of high-energy mechanisms of injury, the precipitating event in sacral insufficiency fractures is often not identifiable or may be related to a fall onto the buttocks from a standing or sitting position. These injuries typically occur in postmenopausal women due to osteoporosis. Conditions contributing to osteoporosis are often present, such as chronic corticosteroid use or a history of radiation therapy to the pelvis (Fig. 179-6).27,44 The presenting symptoms are often vague and consist of poorly localized low back pain that may be exacerbated by sitting and standing. These fractures are typically oriented vertically and occur through the ala adjacent to the sacroiliac joint. There may also be a transverse component resulting in more complex U-fracture variants. Although neurologic deficits are uncommon under these circumstances.45,46 cauda equina dysfunction has been reported and neurologic status must be carefully considered.47
Mechanical factors related to the transfer of forces from the lumbosacral spine to the pelvis may also cause sacral insufficiency fractures in patients with osteoporosis.38 Pelvic stress concentration as the result of lumbosacral spine fusion has been described,48 and sacral insufficiency fractures caudal to lumbosacral fusions are increasingly being reported. These fractures probably represent inability of the sacrum to withstand forces concentrated there as a result of the large cephalad lever arm.49–53 Unilateral sacral insufficiency fractures may also occur on the concave side of lumbar scoliosis.45
Evaluation
Although sacral fractures are increasingly being seen in patients with osteopenic bone disorders that predispose a patient to pathologic fractures, they are usually the result of high-energy trauma. Diagnosis is frequently delayed, which may result in further displacement or neurologic deterioration. In a study that predates more routine use of abdominopelvic CT for the evaluation of trauma patients, Denis et al. found that in neurologically intact patients, the diagnosis of sacral fracture was made during the initial hospitalization only 51% of the time. The presence of a neurologic deficit increased the diagnostic accuracy to only 70%. The etiology of missed sacral fractures is multifactorial and ranges from difficulty identifying these fractures on screening anteroposterior pelvis radiographs, combined with the presence of distracting injuries in the trauma patient, to low clinical suspicion in patients with insufficiency fractures.14,54
The transfer of energy resulting in a fracture of the sacrum often causes other injuries, including life-threatening head and thoracoabdominal trauma. In these trauma patients, emergent resuscitation is the top priority. Accordingly, resuscitation is focused on maintaining cardiopulmonary and hemodynamic stability.55 The secondary survey includes screening evaluation of both the spinal column and the pelvic ring. Precautions to maintain spinal column integrity are necessary, and patients should be initially maintained on a flat surface and log-rolled from side to side to prevent spinal column displacement. Evaluation includes inspection and palpation of the patient’s back from the occiput to the coccyx. Clinical findings associated with sacral fractures include skin discoloration or laceration, palpable step off or crepitus, and ballotable fluid in the lumbopelvic region. Significant soft-tissue contusion or internal degloving analogous to the Morel-Lavallée lesion can have important implications on subsequent treatment.56 Rectal and vaginal examination, including the use of a speculum and proctoscope, allows detection of open sacral fractures and unrecognized neurologic deficits.
If pelvic ring disruption is associated with significant intrapelvic hemorrhage, provisional pelvic ring stabilization may be necessary to reduce pelvic volume and provide temporary stability. Available methods include application of a circumferential pelvic antishock sheet,10 pelvic clamp, anterior external fixator, or skeletal traction. Associated vascular injury, particularly to the hypogastric arterial system, may require embolization to adequately control arterial hemorrhage.57
Early detection of neurologic deficits is of paramount importance in patients with sacral fractures.58–60 A rectal examination is performed early in the evaluation of all multiply injured patients, even in the absence of obvious sensorimotor deficits in the extremities, to evaluate perianal sensation, anal sphincter tone, and voluntary perianal contraction and to assess for the presence of anal wink and the bulbocavernosus reflex. A straight-leg raise test may detect lumbosacral entrapment in the cognitively unimpaired. Extremity motor function is graded on a scale of 0 to 5 according to the American Spinal Injury Association scoring system, and a sensory level is obtained.
Fracture displacement can cause neurologic injury from several mechanisms, including angulation, translation, and direct compression by displaced bone fragments. Delayed neurologic deficits can occur from epidural hematoma, late fracture displacement, or callus formation19 and should be reinvestigated to determine its cause.
Several adjunctive methods can be used to evaluate the neurologic status of a patient with a sacral fracture. Electrodiagnostic studies may be useful in cognitively impaired patients, in differentiating upper motor neuron injuries or spinal cord injury from cauda equina injury in patients with intracranial or more cephalad spinal column injury, in the evaluation of patients with urinary tract injury, and for intraoperative monitoring.61 Pudendal somatosensory evoked potentials and anal sphincter electromyography (EMG) allow for evaluation of the sacral roots below the S1 level. EMG is limited in the acute setting because abnormalities may take weeks to emerge. For patients with neurogenic bladder, serial postvoid residuals or cystometrography is a useful diagnostic aid.
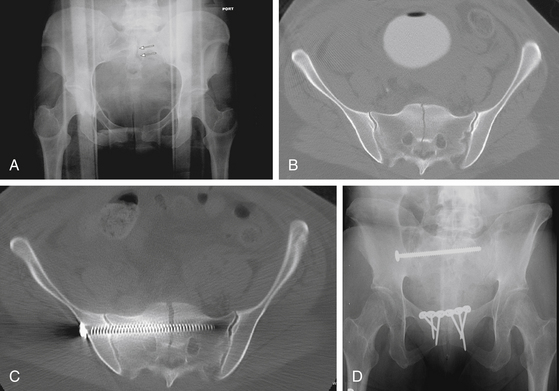
Increasingly common use of more sophisticated imaging techniques in the routine initial assessment of the trauma patient’s visceral injuries, such as CT of the abdomen and pelvis, has improved the early detection of sacral fractures. The identification of a sacral fracture on these studies mandates complete radiographic evaluation, including a dedicated fine-cut CT scan of the sacrum with sagittal and coronal reformations to allow the detail required for determining the fracture configuration, resulting instability pattern, and extent of sacral canal and neuroforaminal compromise (Fig. 179-7).66 Three-dimensionally reformatted CT scans may add insight into fracture morphology for less experienced clinicians or in the case of highly complex fracture patterns. Magnetic resonance imaging is not usually helpful except in cases of unclear neurologic deficits or discrepancies between skeletal and neurologic levels of injury, although it may provide early evidence of lumbosacral nerve root avulsion.67
General Treatment Principles
Decision making in the treatment of sacral fracture is primarily based on fracture pattern and neurologic status. Other key factors are the patient’s medical condition and additional injuries. The benefits of early mobilization in trauma patients with pulmonary injuries must be weighed against the risk of operating on patients with hemodynamic instability, compromised pulmonary function, or intracranial injuries.68,69 Surgical timing in patients with closed head injuries is particularly controversial and requires skilled perioperative management to prevent secondary brain injury.70,71
The goals of treatment include union of the fracture in physiologic alignment while optimizing the potential for recovery of neurologic deficits and minimizing the complications associated with prolonged recumbency. Achieving these goals may require operative fracture reduction, neural decompression, fracture stabilization with instrumentation, and possibly early mobilization and weight bearing. Conversely, nonoperative treatment may be selected as the most favorable method for achieving fracture union and recovery of neurologic deficits if acceptable alignment can be achieved and long-term immobilization is tolerated. To date, the literature on such injuries with neurologic deficits offers no clear treatment directive with regard to optimal management, which therefore remains the subject of considerable controversy. Neurologic improvement after sacral fracture–dislocations has been reported to approach 80%, regardless of operative or nonoperative treatment.6,34 However, wide variability in injury types, degree of improvement, and outcome criteria has lessened the significance and reliability of reported recovery rates.
Careful examination of the fracture pattern is essential in determining the presence of instability of the weight-bearing axis, whether at the level of the spinal column or that of the pelvic ring. The amount of initial fracture displacement and comminution are important determinants of the energy of the injury and the potential for subsequent displacement. Displaced fractures may be associated with disruption of the sacrotuberous and sacrospinous ligaments, predisposing the patient to further fracture displacement. Unilateral longitudinal fractures through the alar or foraminal zone maintain continuity of the contralateral weight-bearing axis, allowing weight bearing on the intact side (Fig. 179-8). Bilateral displaced longitudinal fractures, regardless of the presence of an associated transverse fracture, dissociate the spinal column from the pelvic ring and represent complete disruption of the weight-bearing axis.37,72–74 Weight bearing on either lower extremity, or even across the pelvis when in the sitting position, may cause displacement in these instances. Conversely, transverse fractures below the sacroiliac joint have no implication on the weight-bearing axis unless they are associated with secondary fracture lines extending rostrally.75
Neurologic deficits need to be correlated with fracture anatomy. Residual compression of nerve roots at the level of the spinal canal or neuroforamina due to the impingement of bony fragments or malalignment of the spinal canal at the fracture site with the cauda equina draping over a kyphotic ridge should be identified. Possible neurologic deterioration from persistent fracture instability should also be considered. A review of case reports of sacral fractures with neurologic deficit indicates that the effectiveness of operative decompression in facilitating neurologic recovery is unclear, and improvement has been reported with both operative and nonoperative management.14,20–22,28,33,34 Each case needs to be specifically considered, and in our opinion, surgical decompression (usually with stabilization) should be considered in the presence of a potentially reversible neurologic injury.
Nonoperative Treatment
Nonoperative treatment of displaced, high-energy sacral fractures can be problematic, however. Although surgical complications can be avoided, potential disadvantages include life-threatening pulmonary and thromboembolic events, decubitus ulcers, the inability to reliably address sacral canal and neuroforaminal compression, and the potential for late instability, causing neurologic deficits.76
Nonoperative treatment is most attractive in unilateral fractures that are minimally displaced and have no associated neurologic deficits. Mobilization is usually with a walker or crutches enabling toe-touch weight bearing on the injured side. These patients must be followed carefully for displacement, which may warrant surgical stabilization. Insufficiency or stress fractures are also usually amenable to nonoperative treatment despite their frequently bilateral involvement. Along with activity modification and correction of underlying metabolic conditions, nonoperative treatment has a high likelihood of success in the majority of insufficiency and stress fractures.47
Neural Decompression
Neural decompression can be achieved directly or indirectly. Indirect decompression can often be achieved with fracture reduction, which is best accomplished before consolidation of fracture hematoma.77 If neural impingement persists and is associated with a neurologic deficit, direct decompression should be considered.
In patients with sacral root deficits, direct decompression alone by laminectomy has been advocated to enhance the possibility of neurologic recovery while minimizing the potential for complications associated with a more extensive surgical stabilization procedure.28 Surgical exposure for decompression is generally through a straight posterior midline approach. Decompression can be performed focally for selective ventral forminal impingement or full laminectomy to achieve a more comprehensive decompression of the S1 to S4 neural elements. In the case of L5 root entrapment between the L5 transverse process and an alar bone fragment, decompression is performed by following the root laterally onto the shoulder of the ala and removing the offending fragment.
The possibility of significant epidural bleeding during direct decompression requires experience with techniques of epidural hemostasis. Similarly, experience with neural element repair is essential, and dural tears that are encountered should be repaired if possible. The dura at the sacral level is often relatively thin and friable, and direct repair is often best performed with fine (e.g., 6-0) monofilament suture. Augmentation with fibrin glue may be used to increase the strength of the repair. Often, a direct repair is not possible because of the severity of the disruption, and a patch with muscle graft, bovine pericardium, or DuraGen is necessary. In many cases, the disruption is through individual nerve roots caudal to the termination of the dural sac at the S2 level and is irreparable.
Surgical Stabilization Techniques
Surgical stabilization is performed to avoid prolonged recumbency in the critically injured patient, as an adjunct to neurologic decompression, and as the most effective method to correct or prevent displacement that might adversely affect postural alignment or predispose a patient to chronic pain or nerve compression. It has been hypothesized that restoration of appropriate sagittal alignment of the sacral fracture leads to decreased pain by establishing a more physiologic alignment of the lumbar spine.5 Pelvic incidence can therefore be a useful intraoperative guide to assess lumbopelvic alignment and adequacy of reduction. Recently published functional outcome studies indicate that a minority of sacral fracture patients returned to their preinjury vocational status more than a year after injury. The vast majority of patients sustained long-term physical and mental impairment, the severity of which correlated less with fracture characteristics than with associated injuries and sacral root function.78,79
If the sacral fracture results in pelvic instability, reduction and fixation of associated anterior pelvic instability, in collaboration with the orthopedic traumatologist, is an essential first step, providing indirect reduction of the sacral fracture, partial pelvic stability, and a helpful fulcrum during subsequent attempts at sacral fracture reduction. However, anterior pelvic ring stabilization alone is inadequate to stabilize an unstable fracture of the sacrum and posterior pelvic ring.80–82
Roy-Camille et al. described the use of sacral alar plates for direct osteosynthesis of sacral fractures.37 The vertical orientation of the plates lateral to the dorsal foramina is theoretically optimal for compression loading across a transverse fracture, but it does not adequately stabilize other fracture planes. Additional disadvantages include frequently compromised screw purchase in comminuted or osteopenic alar bone and inadequate strength of this construct to neutralize the enormous forces across the lumbopelvic junction, requiring a 2- to 4-month period of restricted weight bearing. It is therefore our opinion that sacral alar plating alone has few clinical applications. Its utility is usually in combination with methods of fixation that stabilize across the weight-bearing axis and unload the sacrum.80 Direct plating alone, however, may be useful in maintaining alignment of transverse sacral fractures below the sacroiliac joints, since these fractures are not subject to the high loads seen with fractures involving the weight-bearing axis and the goal in their treatment is primarily to avoid pain due to prominence or nonunion.75
Various methods of posterior pelvic ring fixation have been described, including sacral bars, tension band plating, and iliosacral screws.61,83 Simonian and Routt,82 in a cadaveric biomechanical study, found no difference in pelvic ring stability among these constructs. Because a considerable disadvantage of sacral bars and tension band plating is the potential for soft-tissue compromise that may occur due to their location superficial to the nearly subcutaneous dorsal sacrum,83 iliosacral screws have become the most widely used method for posterior pelvic ring fixation. In these methods of percutaneous posterior pelvic ring stabilization, however, fixation is perpendicular to the weight-bearing axis and is not considered to provide adequate stabilization for immediate weight bearing.84,85
Iliosacral screw fixation is usually performed percutaneously; consequently, blood loss is minimal. Success of the technique depends on the surgeon’s ability to achieve an anatomic reduction under adequate fluoroscopic visualization; otherwise, in addition to the problem of malreduction, a safe trajectory for iliosacral screw placement cannot be reliably established.61,86 It can be performed with the patient supine or prone, facilitating either concurrent anterior pelvic ring stabilization or posterior decompression, respectively. A pitfall of iliosacral screw fixation is the risk of overcompression of the foramina, causing nerve root injury in cases in which screw fixation of a comminuted transforaminal sacral fracture is done using interfragmentary compression.81 However, in experienced centers, the reported rate of neurologic injury is low, even without the use of electrodiagnostic monitoring.87 Like other methods of posterior pelvic ring stabilization, percutaneous iliosacral screw fixation carries the disadvantage of not allowing for reduction of sacral angulation. It also depends on screw purchase into the iliac wing and sacrum that may be compromised in the presence of comminution or osteoporosis. The orientation of the screw perpendicular to the fracture’s deforming forces may also contribute to a higher likelihood of fixation failure. Nevertheless, iliosacral screw fixation has been shown to be effective for stabilization of unstable longitudinal sacral fractures.88 A 3-month period of protected weight bearing is recommended with iliosacral screw fixation.
Iliosacral screws have also been used successfully in patients with minimally displaced sacral-U fracture variants. In a series of 13 patients who had fractures with minimal sacral angulation and displacement, Nork et al. found bilateral percutaneous iliosacral screw fixation with an 8- to 12-week period of immobilization in a thoracolumbosacral-hip orthosis to be safe and effective in treating this type of injury.89 However, this minimally invasive method does not allow for reduction of fracture angulation. Moreover, if a near-anatomic reduction cannot be achieved, the safe zone for iliosacral screw trajectory may be very small or absent, thus precluding its use in more complex and highly displaced injuries.86 Iliosacral screw fixation alone is therefore not recommended for patients with displaced sacral-U fractures and their variants if they are irreducible by closed manipulation, if neural decompression is required, or if sacral comminution is likely to significantly compromise iliosacral screw purchase.
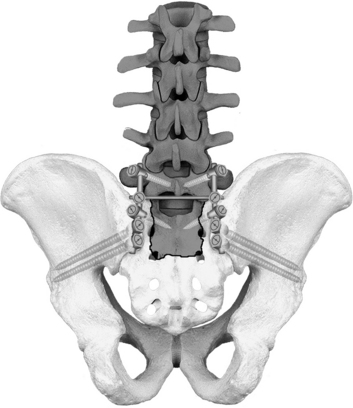
Lumbopelvic fixation provides the biomechanically strongest fixation of sacral fractures.90 This technique was derived from the Galveston method of anchoring the caudal end of long thoracolumbar rod constructs into the ileum (Fig. 179-9). Sacral fracture fixation is obtained rostrally by segmental pedicle screw fixation in the lumbosacral spine and caudally by long screw fixation in the ileum.91–101 The construct spans the sacrum and mimics the normal load transfer from the lumbar spine to the pelvis.53,90 The strength of the construct permits immediate weight bearing without external bracing (see Figs. 179-7 to 179-9).
Lumbopelvic fixation is performed through a dorsal approach with the patient in the prone position. The longitudinally oriented constructs are placed laterally, adjacent to the posterior iliac wings. The lateral placement also allows posterior decompression of the neural elements, as well as open reduction of the sacral fracture. Screw placement is performed under fluoroscopic guidance to ensure correct screw orientation. A thorough understanding of pelvic anatomy and facility with fluoroscopic positioning is necessary for verification of correct screw placement. Screw malposition can be catastrophic, potentially injuring neurovascular structures in the sciatic notch or the pelvic viscera or penetrating the acetabulum. If placed correctly, the hardware profile is low. Infection- and wound-related problems are common, however, and have been found to approach 20%.92,97 A formal sacroiliac joint arthrodesis is not usually performed, and in many instances the rod breaks from fatigue failure, an expected consequence of continued sacroiliac joint motion. Late rod fracture is asymptomatic in the majority of cases, and the need for routine hardware removal is questionable.92,97
The optimal stabilization of complex sacral fractures may require the use of multiple methods of fixation. Lumbopelvic fixation can be combined with iliosacral screw fixation, the so-called triangular osteosynthesis technique, to obtain optimal fixation in the vertical direction along the weight-bearing axis and the horizontal direction stabilizing the pelvic ring.90,96 Lumbopelvic fixation may also benefit from adjunctive sacral plating, utilized solely to fine-tune fracture realignment and prevent recurrent displacement and canal compromise, while the lumbopelvic fixations role is to neutralize the bulk of the loads being transferred across the sacrum.
Bellabarba C., Schildhauer T.A., Vaccaro A.R., Chapman J.R. Complications associated with surgical stabilization of high-grade sacral fracture–dislocations with spino-pelvic instability. Spine. 2006;31(Suppl 11):S80-S88.
Bellabarba C., Stewart J.D., Ricci W.M., et al. Midline sagittal sacral fractures in anterior–posterior compression ring injuries. J Orthop Trauma. 2003;17:32-37.
Denis F., Davis S., Comfort T. Sacral fractures: an important problem: a retrospective analysis of 236 cases. Clin Orthop. 1988;227:67-81.
Gardner M.J., Farrell E.D., Nork S.E., et al. Percutaneous placement of iliosacral screws without electrodiagnostic monitoring. J Trauma. 2009;66:1411-1415.
Gibbons K.J., Soloniuk D.S., Razack N. Neurological injury and patterns of sacral fractures. J Neurosurg. 1990;72:889-993.
Gunterberg B. Effects of major resection of the sacrum. Acta Orthop Scand Suppl. 1976;162:1-38.
Huittinen V.M. Lumbosacral nerve injury in fracture of the pelvis. Acta Chir Scand Suppl. 1972;429:7-43.
Isler B. Lumbosacral lesions associated with pelvic ring injuries. J Orthop Trauma. 1990;4:1-6.
Klineberg E., McHenry T., Bellabarba C., et al. Sacral insufficiency fractures caudal to instrumented posterior lumbosacral arthrodesis. Spine. 2008;33:1806-1811.
Nork S.E., Jones C.B., Harding S.P., et al. Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma. 2001;15:238-246.
Reilly M.C., Bono C.M., Litkouhi B., et al. The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma. 2003;17:88-94.
Routt M.L.Jr., Simonian P.T. Closed reduction and percutaneous skeletal fixation of sacral fractures. Clin Orthop. 1996;329:121-128.
Routt M.L., Simonian P.T., Agnew S.G., Mann F.A. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma. 1996;10:171-177.
Roy-Camille R., Saillant G., Gogna G., Mazel C. Transverse fracture of the upper sacrum: suicidal jumper’s fracture. Spine. 1985;10:838-845.
Sagi H.C. Technical aspects and recommended treatment algorithms in triangular osteosynthesis and spinopelvic fixation for vertical shear transforaminal sacral fractures. J Orthop Trauma. 2009;23:354-360.
Schildhauer T.A., Bellabarba C., Nork S.E., et al. Decompression and lumbopelvic fixation for sacral fracture–dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20:447-457.
Schildhauer T.A., Josten C., Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma. 1998;12:307-314.
Schildhauer T.A., Ledoux W.R., Chapman J.R., et al. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22-31.
Schildhauer T.A., McCullough P., Chapman J.R., Mann F.A. Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixations. J Spinal Disord Tech. 2002;15:199-205.
Strange-Vognsen H.H., Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma. 1991;5:200-203.
1. Gray’s Anatomy, American, New York, Churchill Livingstone, 1989
2. Jackson R.P., McManus A.C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. Spine. 1994;19:1611-1618.
3. Wiltse L.L., Winter R.B. Terminology and measurement of spondylolisthesis. J Bone Joint Surg Am. 1983;65:768-772.
4. Legaye J., Duval-Beaupere G., Hecquet J., et al. Pelvic incidence: a fundamental pelvic parameter for three dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99-103.
5. Hart R.A., Badra M.I., Madala A., Yoo J.U. Use of pelvic incidence as a guide to reduction of H-type spino-pelvic dissociation injuries. J Orthop Trauma. 2007;21:369-374.
6. Schmidek H.H., Smith D., Kristiansen T.K. Sacral fractures: issues of neural injury, spinal stability, and surgical management. In: Dunsker SB, et al, editors. The Unstable Spine. New York: Harcourt, 1986. . pp. 256-272
7. Tile M. Fractures of the Pelvis and Acetabulum, 2nd ed. Baltimore: Williams & Wilkins; 1995.
8. Morris H., Lond M.B. Human Anatomy. Philadelphia: P. Blakiston’s Son & Co, 1989.
9. Williams P., Warwick R., Dyson M. Gray’s Anatomy, 37th (British), Edinburgh: Churchill Livingstone, 1989.
10. Routt M.L., Simonian P.T., Agnew S.G., Mann F.A. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma. 1996;10:171-177.
11. Peretz A.M., Hipp J.A., Heggeness M.H. The internal bony architecture of the sacrum. Spine. 1998;23:971-974.
12. Smith S.A., Abitbol J.J., Carlson G.D., et al. The effects of depth of penetration, screw orientation and bone density on sacral screw fixation. Spine. 1993;18:1006-1010.
13. Carter S.R. Stress fracture of the sacrum: brief report. J Bone Joint Surg. 1987;69:843-884.
14. Denis F., Davis S., Comfort T. Sacral fractures: an important problem: a retrospective analysis of 236 cases. Clin Orthop. 1988;227:67-81.
15. Mirkovic S., Abitbol J.J., Steinman J., et al. Anatomic consideration for sacral screw placement. Spine. 1991;16:S289-S294.
16. Esses S.I., Botsford D.J., Huler R.J., Rauschning W. Surgical anatomy of the sacrum: a guide for rational screw fixation. Spine. 1991;16:S283-S288.
17. Gunterberg B. Effects of major resection of the sacrum. Acta Orthop Scand Suppl. 1976;162:1-38.
18. Grant’s Atlas of Anatomy, 8th ed. Baltimore, Williams & Wilkins, 1983
19. Bonnin J.G. Sacral fractures. J Bone Joint Surg Am. 1945;27:113-127.
20. Sabiston C.P., Wing P.C. Sacral fractures. Classification and neurologic implications. J Trauma. 1986;26:1113-1115.
21. Schmidek H.H., Smith D.A., Kristiansen T.K. Sacral fractures. Neurosurgery. 1984;15:735-746.
22. Gibbons K.J., Soloniuk D.S., Razack N. Neurological injury and patterns of sacral fractures. J Neurosurg. 1990;72:889-893.
23. Huittinen V.M. Lumbosacral nerve injury in fracture of the pelvis. Acta Chir Scand Suppl. 1972;429:7-43.
24. Purser D.W. Displaced fracture of the sacrum: report of a case. J Bone Joint Surg Br. 1969;51:346-347.
25. Bucknill T.M., Blackburne J.S. Fracture–dislocations of the sacrum: report of three cases. J Bone Joint Surg Br. 1976;58:467-570.
26. Weaver E.N., England G.D., Richard D.E. Sacral fracture: case presentation and review. Neurosurgery. 1981;9:725-728.
27. Nicoll E.A. Fractures of the dorsolumbar spine. J Bone Joint Surg Br. 1949;31:376.
28. Fountain S.S., Hamilton R.D., Jameson R.M. Transverse fractures of the sacrum: a report of six cases. J Bone Joint Surg Am. 1977;59:486-489.
29. Carl A., Delman A., Engler G. Displaced transverse sacral fractures: a case report, review of the literature, and the CT scan as an aid in management. Clin Orthop. 1985;194:195-198.
30. Ebraheim N.A. Zone III fractures of the sacrum. Spine. 1996;21:2390-2396.
31. Fardon D.F. Displaced fracture of the lumbosacral spine with delayed cauda equina deficit: report of a case and review of literature. Clin Orthop. 1976;120:155-158.
32. Ferris B. Anteriorly displaced transverse fracture of the sacrum at the level of the sacroiliac joint: a report of two cases. J Bone Joint Surg Am. 1983;65:407-409.
33. Fisher R.G. Sacral fracture with compression of cauda equina: surgical treatment. J Trauma. 1988;28:1678-1680.
34. Phelan S.T., Jones D.A., Bishay M. Conservative management of transverse fractures of the sacrum with neurological features: a report of four cases. J Bone Joint Surg Br. 1991;73:969-971.
35. Rao S.H. Traumatic transverse fracture of sacrum with cauda equine injury: a case report and review of literature. J Postgrad Med. 1998;44:14-15.
36. Rodriguez-Fuentes A.E. Traumatic sacrolisthesis S1-S2. Spine. 1993;18:768-771.
37. Roy-Camille R., Saillant G., Gogna G., Mazel C. Transverse fracture of the upper sacrum: suicidal jumper’s fracture. Spine. 1985;10:838-845.
38. Strange-Vognsen H.H., Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma. 1991;5:200-203.
39. Schildhauer T.A., Chapman J.R., Mayo K.A. Multisegmental open sacral fracture due to impalement. J Orthop Trauma. 2005;19:134-139.
40. Bellabarba C., Stewart J.D., Ricci W.M., et al. Midline sagittal sacral fractures in anterior–posterior compression ring injuries. J Orthop Trauma. 2003;17:32-37.
41. Hatem S.F., West O.C. Vertical fracture of the central sacral canal: plane and simple. J Trauma. 1996;40:138-140.
42. Wiesel S.W., Zeide M.S., Terry R.L. Longitudinal fracture of the sacrum: case report. J Trauma. 1979;19:70-71.
43. Isler B. Lumbosacral lesions associated with pelvic ring injuries. J Orthop Trauma. 1990;4:1-6.
44. Herman M.P., Kopetz S., Bhosale P.R., et al. Sacral insufficiency fractures after preoperative chemoradiation for rectal cancer: incidence, risk factors, and clinical course. Int J Radiat Oncol Biol Phys. 2009;74:818-823.
45. Gotis-Graham I., McGuigan L., Diamond T., et al. Sacral insufficiency fractures in the elderly. J Bone Joint Surg Br. 1994;76:882-886.
46. Weber M., Haster P., Gerber H., et al. Insufficiency fractures of the sacrum: twenty cases and review of the literature. Spine. 1993;18:2507-2512.
47. Jacquot J.M., Finiels H., Fardjad S., et al. Neurological complications in insufficiency fractures of the sacrum: three case reports. Rev Rhum Engl Ed. 1999;66:109-113.
48. Wood K.B., Geissele A.E., Ogilvie J.W. Pelvic fractures after long lumbosacral spine fusions. Spine. 1996;21:1357-1362.
49. Elias W.J., Shaffrey M.E., Whitehill R. Sacral stress fracture following lumbosacral arthrodesis: case illustration. J Neurosurg. 2002;96(Suppl 1):135.
50. Fourney D.R., Prabhu S.S., Cohen Z.R., et al. Early sacral stress fractures after reduction of spondylolisthesis and lumbosacral fixation: case report. Neurosurgery. 2002;51:1510-1511.
51. Klineberg E., McHenry T., Bellabarba C., et al. Sacral insufficiency fractures caudal to instrumented posterior lumbosacral arthrodesis. Spine. 2008;33:1806-1811.
52. Mathews V., McCance S.E., O’Leary P.F. Early fracture of the sacrum or pelvis: an unusual complication after multilevel instrumented lumbosacral fusion. Spine. 2001;26:E571-E575.
53. Wood K.B., Schendel M.J., Ogilvie J.W., et al. Effect of sacral and iliac instrumentation on strains in the pelvis. Spine. 1996;21:1185-1191.
54. Laasonen E.M. Missed sacral fractures. Ann Clin Res. 1977;9:84-87.
55. . ATLS manual, Crosby L.A., Lewallen D.O. Emergency Care and Transportation of the Sick and Injured, 6th ed, American Academy of Orthopedic Surgeons, 1995. p.11
56. Kellam J.F., McMurtry R.Y., Paley D., Tile M. The unstable pelvic fracture: operative treatment. Orthop Clin North Am. 1987;18:25-41.
57. Ben-Menachem Y., Coldwell D.M., Young J.W., Burgess A.R. Hemorrhage associated with pelvic fractures: causes, diagnosis, and emergent management. AJR Am J Roentgenol. 1991;157:1005-1014.
58. Byrnes D.P., Russo G.L., Duckert T.B., Cowley R.A. Sacrum fractures and neurological damage: report of two cases. J Neurosurg. 1977;47:459-462.
59. Goodell C.L. Neurological deficits associated with pelvic fractures. J Neurosurg. 1966;24:837-842.
60. Lam C.R. Nerve injury in fractures of the pelvis. Ann Surg. 1936;104:945-951.
61. Routt M.L.Jr, Simonian P.T. Closed reduction and percutaneous skeletal fixation of sacral fractures. Clin Orthop. 1996;329:121-128.
62. Cohen B.A., Major M.R., Huizenga B.A. Pudendal nerve evoked potential monitoring in procedures involving low sacral fixation. Spine. 1991;16:S375-S378.
63. Helfet D.L., Koval K.J., Hissa E.A., et al. Intraoperative somatosensory evoked potential monitoring during acute pelvic fracture surgery. J Orthop Trauma. 1995;9:28-34.
64. Kothbauer K., Schmid U.D., Seiler R.W., Eisner W. Intraoperative motor and sensory monitoring of the cauda equina. Neurosurgery. 1994;34:702-707.
65. Slimp J.C. Electrophysiologic intraoperative monitoring for spine procedures. Phys Med Rehabil Clin North Am. 2004;15:85-105.
66. Kuklo T.R., Potter B.K., Ludwig S.C., et al. Spine Trauma Study Group. Radiographic measurement techniques for sacral fractures consensus statement of the Spine Trauma Study Group. Spine. 2006;31:1047-1055.
67. Sasaka K.K., Phisitkul P., Boyd J.L., et al. Lumbosacral nerve root avulsions: MR imaging demonstration of acute abnormalities. AJNR Am J Neuroradiol. 2006;27:1944-1946.
68. Bone L.B., Johnson K.D., Weigelt J., Scheinberg R. Early versus delayed stabilization of femoral fractures: a prospective randomized study. J Bone Joint Surg Am. 1989;71:336-340.
69. Johnson K.D., Cadambi A., Seibert G.B. Incidence of adult respiratory distress syndrome in patients with multiple musculoskeletal injuries: effect of early operative stabilization of fractures. J Trauma. 1985;25:375-384.
70. Jaicks R.R., Cohn S.M., Moller B.A. Early fracture fixation may be deleterious after head injury. J Trauma. 1997;42:1-5.
71. Scalea T.M., Scott J.D., Brumback R.J., et al. Early fracture fixation may be “just fine” after head injury: no difference in central nervous system outcomes. J Trauma. 1999;46:839-846.
72. Marcus R.E., Hansen S.T. Bilateral fracture–dislocation of the sacrum: a case report. J Bone Joint Surg Am. 1984;66:1297-1299.
73. Pennal G.F., Tile M., Waddell J.P., Garside H. Pelvic disruption: assessment and classification. Clin Orthop. 1980;151:12-21.
74. Wild J., Hanson G.W., Tullas H.S. Unstable fractures of the pelvis treated by external fixation. J Bone Joint Surg Am. 1982;64:1010-1020.
75. Sommer C. Fixation of transverse fractures of the sternum and sacrum with the locking compression plate system: two case reports. J Orthop Trauma. 2005;19:487-490.
76. Latenser B.A., Gentilello L.M., Tarver A.A., et al. Improved outcome with early fixation of skeletally unstable pelvic fractures. J Trauma. 1991;31:28-31.
77. Pohlemann T., Angst A., Schneider E., et al. Fixation of transforaminal sacrum fractures: a biomechanical study. J Orthop Trauma. 1993;2:107-117.
78. Tötterman A., Glott T., Søberg H.L., et al. Pelvic trauma with displaced sacral fractures: functional outcome at one year. Spine. 2007;32:1437-1443.
79. Tötterman A., Glott T., Madsen J.E., Røise O. Unstable sacral fractures: associated injuries and morbidity at 1 year. Spine. 2006;31:E628-E635.
80. Templeman D., Goulet J., Dawelius P.J., et al. Internal fixation of displaced fractures of the sacrum. Clin Orthop. 1996;329:180-185.
81. Routt M.L.C., Simonian P.T., Swiontkowski M.F. Stabilization of pelvic ring disruptions. Orthop Clin North Am. 1997;28:369-388.
82. Simonian P.T., Routt M.L.Jr. Biomechanics of pelvic fixation. Orthop Clin North Am. 1997;28:351-368.
83. Suzuki T., Hak D.J., Ziran B.H., et al. Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury. 2009;40:405-409.
84. Suzuki K., Mochida J. Operative treatment of a transverse fracture–dislocation at the S1-S2 level. J Orthop Trauma. 2001;15:363-367.
85. Taguchi T., Kawai S., Kaneko K., Yugue D. Operative management of displaced fractures of the sacrum. J Orthop Sci. 1999;4:347-352.
86. Reilly M.C., Bono C.M., Litkouhi B., et al. The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma. 2003;17:88-94.
87. Gardner M.J., Farrell E.D., Nork S.E., et al. Percutaneous placement of iliosacral screws without electrodiagnostic monitoring. J Trauma. 2009;66:1411-1415.
88. Routt M.L.C., Nork S.E., Mills W.J. Percutaneous fixation of pelvic ring disruptions. Clin Orthop. 2000;375:15-29.
89. Nork S.E., Jones C.B., Harding S.P., et al. Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma. 2001;15:238-246.
90. Schildhauer T.A., Ledoux W.R., Chapman J.R., et al. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17:22-31.
91. Acharya N.K., Bijukachhe B., Kumar R.J., Menon V.K. Ilio-lumbar fixation: the Amrita technique. J Spinal Disord Tech. 2008;21:493-499.
92. Bellabarba C., Schildhauer T.A., Vaccaro A.R., Chapman J.R. Complications associated with surgical stabilization of high-grade sacral fracture–dislocations with spino-pelvic instability. Spine. 2006;31(Suppl 11):S80-S88.
93. O’Brien J.R., Yu W.D., Bhatnagar R., Sponseller P., Kebaish K.M. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine. 2009;34:E439-E442.
94. Sagi H.C. Technical aspects and recommended treatment algorithms in triangular osteosynthesis and spinopelvic fixation for vertical shear transforaminal sacral fractures. J Orthop Trauma. 2009;23:354-360.
95. Schildhauer T.A., McCullough P., Chapman J.R., Mann F.A. Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixations. J Spinal Disord Tech. 2002;15:199-205.
96. Schildhauer T.A., Josten C., Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma. 1998;12:307-314.
97. Schildhauer T.A., Bellabarba C., Nork S.E., et al. Decompression and lumbopelvic fixation for sacral fracture–dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20:447-457.
98. Schildhauer T.A., Bellabarba C., Selznick H.S., et al. Unstable pediatric sacral fracture with bone loss caused by a high-energy gunshot injury. J Trauma. 2007;63:E95-E99.
99. Strange-Vognsen H.H., Kiaer T., Tondevold E. The Cotrel-Dubousset instrumentation for unstable sacral fractures: report of 3 patients. Acta Orthop Scand. 1994;65:219-220.
100. Vilela M.D., Gelfenbeyn M., Bellabarba C. U-shaped sacral fracture and lumbosacral dislocation as a result of a shotgun injury: case report. Neurosurgery. 2009;64:E193-E194.
101. Lebwohl N.H., Cunningham B.W., Dmitriev A., et al. Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine. 2002;27:2312-2320.