Chapter 679 Management of Musculoskeletal Injury
679.1 Mechanism of Injury
Overuse Injuries
The goals of treatment are to control pain and spasm to rehabilitate flexibility, strength, endurance, and proprioceptive deficits (Table 679-1). In many overuse injuries, the role of inflammation in the process is minimal. For most injuries to tendons, the term tendinitis is obsolete because there is little or no inflammation on histopathology of tendons. Instead, there is evidence of microscopic trauma to the tissue. Most of these entities are now more appropriately called tendinosis and, when the tendon tissue is scarred and very abnormal, tendinopathy. There is little role for anti-inflammatory medication in the treatment except as an analgesic.
| GRADE | GRADING SYMPTOMS | TREATMENT |
|---|---|---|
| I |
Transition From Immediate Management to Return to Play
Rehabilitation of a musculoskeletal injury should begin on the day of the injury.
Khan KM, Cook JL, Kannua P, et al. Time to abandon the “tendonitis” myth. Br Med J. 2002;324:626-627.
Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87:187-202.
Van Tulder M, Malmivaara A, Koes B. Repetitive strain injury. Lancet. 2007;369:1815-1822.
679.1 Growth Plate Injuries
About 20% of pediatric sports injuries seen in the emergency department are fractures, and 25% of those fractures involve an epiphyseal growth plate or physis (Chapter 675). Growth in long bones occurs in 3 areas and is susceptible to injury. Immature bone can be acutely injured at the physis (Salter-Harris fractures), the articular surface (osteochondritis dissecans), or the apophysis (avulsion fractures). Boys suffer about twice as many physeal fractures as girls; the peak incidence of fracture is during peak height velocity (girls, 12 ± 2.5 yr; boys, 14 ± 2 yr). The physis is a pressure growth plate and is responsible for longitudinal growth in bone. The apophysis is a bony outgrowth at the attachment of a tendon and is a traction physis. The epiphysis is the end of a long bone, distal or proximal to the long bone, and contains articular cartilage at the joint.
The most common physeal injuries are to the distal radius, followed by phalangeal and distal tibial fractures. About 94% of forearm fractures in skateboarding, roller skating, and scooter riding involve the distal radius. Physeal injuries at the knee (distal femur, proximal tibia) are rare. Growth disturbance following a growth plate injury is a function of location and the part of the physis fractured. These factors influence the probability a physeal bar will form, resulting in growth arrest. The areas making the largest contribution to longitudinal growth in the upper extremities are the proximal humerus and distal radius and ulna; in the lower extremities, they are the distal femur and the proximal tibia and fibula. Injuries to these areas are more likely to cause growth disturbance compared with physeal injuries at the other end of these long bones. The type of the physis fracture relative to risk of growth disturbance is described by the Salter-Harris classification system (see Table 675-1). A grade I injury is least likely to result in growth disturbance, and grade V is the most likely fracture to result in growth disturbance.
Osteochondritis dissecans (OCD) affects the subchondral bone and overlying articular surface (Chapter 669.3). With avascular necrosis of subchondral bone, the articular surface can flatten, soften, or break off in fragments. The etiology is unknown but may be related to repetitive stress injury in some patients. In children and adolescents, 51% of lesions occur on the lateral aspect of the medial femoral condyle, 17% occur on the lateral condyle, and 7% occur on the patella. Bilateral involvement is reported in 13-30% of cases. Other joints where OCD lesions are also seen are the ankle (talus), elbow (usually involving the capitellum), and radial head. OCD classically affects athletes in their 2nd decade. The most common presentation is poorly localized vague knee pain. There is rarely a history of recent acute trauma. Some OCD lesions are asymptomatic (diagnosed on “routine” radiographs), whereas others are manifested as joint effusion, pain, decreased range of motion, and mechanical symptoms (locking, popping, catching). Activity usually worsens the pain.
Physical examination might show no specific findings. Sometimes tenderness over the involved condyle can be elicited by deep palpation with the knee flexed. Diagnosis is usually made with plain radiographs (Fig. 679-1). A tunnel view radiograph should be obtained to better view the posterior two thirds of the femoral condyle. Patients with OCD should be referred to an orthopedic surgeon for further evaluation.

Figure 679-1 Osteochondritis dissecans in the elbow.
(From Anderson SJ: Sports injuries, Curr Prob Pediatr Adolesc Health 35:105–176, 2005.)
Avulsion fractures occur when a forceful muscle contraction dislodges the apophysis from the bone. They occur most commonly around the hip (Fig. 679-2) and are treated nonsurgically. Acute fractures to other apophyses (knee and elbow) require urgent orthopedic consultation. Chronically increased traction at the muscle-apophysis attachment can lead to repetitive microtrauma and pain at the apophysis. The most common areas affected are the knee (Osgood-Schlatter and Sindig-Larsen-Johannson disease), the ankle (Sever disease) (Fig. 679-3), and the medial epicondyle (Little League elbow). Traction apophysitis of the knee and ankle can potentially be treated in a primary care setting. The main goal of treatment is to minimize the intensity and incidence of pain and disability. Exercises that increase the strength, flexibility, and endurance of the muscles attached at the apophysis, using the relative rest principle, are appropriate. Symptoms can last for 12-24 mo if untreated. As growth slows, symptoms abate.

Figure 679-2 Anterior inferior iliac spine avulsion.
(From Anderson SJ: Lower extremity injuries in youth sports, Pediatr Clin North Am 49:627–641, 2003.)
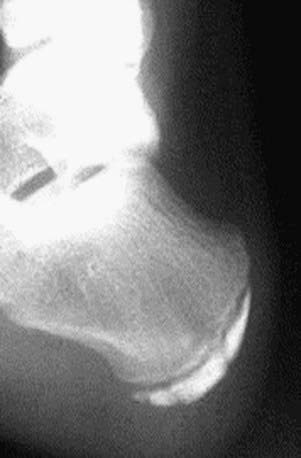
Figure 679-3 Calcaneal apophysitis (Sever disease).
(From Anderson SJ: Sports injuries, Curr Prob Pediatr Adolesc Health 35:105–176, 2005.)
Caine D, DiFiori J, Maffulli N. Physeal injuries in children’s and youth sports: reasons for concern? Br J Sports Med. 2006;40:749-760.
Wall E, Von Stein D. Juvenile osteochondritis dissecans. Orthop Clin North Am. 2003;34:341-353.
Zalavras C, Nikolopoulou G, Essin D, et al. Pediatric fractures during skateboarding, roller skating, and scooter riding. Am J Sports Med. 2005;33:568-573.
679.2 Shoulder Injuries
Acromioclavicular Separation
An acromioclavicular (AC) separation most commonly occurs when an athlete sustains a direct blow to the acromion with the humerus in an adducted position, forcing the acromion inferiorly and medially. Patients have discrete tenderness at the AC joint and can have an apparent step off between the distal clavicle and the acromion (Fig. 679-4).
Bradley JP, Elkousy H. Decision-making: operative versus nonoperative treatment of acromioclavicular joint injuries. Clin Sports Med. 2003;2:277-290.
Luime JJ, Verhagen AP, Miedema HS, et al. Does this patient have an instability of the shoulder or a labrum lesion? JAMA. 2004;292:1989-1998.
Sciascia A, Kibler WB. The pediatric overhead athlete: what is the real problem? Clin J Sport Med. 2006;16:471-477.
Wasserlauf BL, Paletta GAJr. Shoulder disorders in the skeletally immature throwing athlete. Orthop Clin North Am. 2003;34:427-437.
679.3 Elbow Injuries
Acute Injuries
Supracondylar humeral fractures can result from the same mechanism of injury as elbow dislocations and can be complicated by coexisting injury to the brachial artery and, to a lesser extent, the median, radial, and ulnar nerves. An acute compartment syndrome can develop after these fractures (Fig. 679-5).

Figure 679-5 Deflection of the coronoid fat pad with a joint effusion (fat pad sign) showing evidence of a fracture.
(From Gomez JE: Upper extremity injuries in youth sports, Pediatr Clin North Am 49:593–626, 2002.)
Chronic Injuries
Medial elbow pain is a common complaint of young throwers, resulting from repetitive valgus overload of the wrist flexor-pronator muscle groups and their attachment on the medial apophysis. In preadolescents who still have maturing secondary ossification centers, traction apophysitis of the medial epicondyle is likely. Patients have tenderness along the medial epicondyle; this is exacerbated by valgus stress or resisted wrist flexion and pronation. Treatment includes no throwing for 4-6 wk, pain-free strengthening, and stretching of the flexor-pronator group, followed by 1-2 wk of a progressive functional throwing program with accelerated rehabilitation. This problem has to be treated with rest because of the risk of nonunion of the apophysis and chronic pain. If pain occurs acutely, avulsion fracture of the medial epicondyle must be considered. Radiographs should be taken in any thrower with acute elbow pain (Fig. 679-6). If the medial epicondyle is avulsed, orthopedic consultation is indicated.

Figure 679-6 Medial epicondylitis.
(From Anderson SJ: Sports injuries, Curr Prob Pediatr Adolesc Health 35:105–176, 2005.)
Lateral elbow pain can be caused by compression during the throwing motion at the radiocapitellar joint. Panner disease is osteochondrosis of the capitellum that occurs between ages 7 and 12 yr (Fig. 679-7). OCD of the capitellum occurs at age 13-16 yr (see Fig. 679-1). These two entities might represent a continuum of the same disease. Although patients with both conditions present with insidious onset of lateral elbow pain exacerbated by throwing, patients with OCD have mechanical symptoms (popping, locking) and, more commonly, decreased range of motion. Patients with Panner disease have no mechanical symptoms and often have normal range of motion. The prognosis of Panner disease is excellent, and treatments consist of relative rest (no throwing), brief immobilization, and repeat radiographs in 6-12 wk to assess bone remodeling. OCD requires orthopedic consultation.

Figure 679-7 Panner disease. Note fragmentation of the humeral capitellum and flattening of the articular surface (arrow).
(Courtesy of Ralph J. Curtis, MD. From Gomez JE: Upper extremity injuries in youth sports, Pediatr Clin North Am 49:593–626, 2002.)
Elbow injuries might not be prevented by preseason stretching and strengthening exercises. The most important consideration for preventing elbow injuries in throwers is limitation of the number of pitches and advising players, coaches, and athletes that they should stop immediately when they experience elbow pain. If it persists, they need medical evaluation. It has been recommended that a young pitcher have age-specific limits on pitch counts. A good rule of thumb is the maximal number of pitches per game should be approximately 6 times the pitcher’s age in years. For more information, consult the Little League Baseball website at www.littleleague.org/media/newsarchive/03_2006/06pitch_count_08-25-06.htm.
Assendelft W, Green S, Buchbinder R, et al. Tennis elbow. BMJ. 2003;327:329-330.
Petty DH, Andrews JR, Fleisig GS, et al. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32:1158-1164.
Samuel J, Olsen SJII, Fleisig GS, et al. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34(6):905-912.
679.4 Low Back Injuries
Spondylolysis, Spondylolisthesis, and Facet Syndrome
Spondylolysis
Spondylolysis, a common cause of back pain in athletes, is a stress fracture of the pars interarticularis (Chapter 671.6). It can occur at any vertebral level but is most likely at L4 or L5. Prevalence in adolescent athletes evaluated for low back pain is 13-47%. Besides acute hyperextension that causes an acute fracture, the mechanism of injury is either a congenital defect or hypoplastic pars, which is exacerbated by lumbar extension loading, or a stress fracture due to repetitive extension loading. Ballet, weight lifting, gymnastics, and football are examples of sports in which repetitive extension loading of the lumbar spine occurs; it occurs in any activity in which there is repetitive extension loading, including swimming.
Spondylolisthesis and Facet Syndrome
Spondylolysis, spondylolisthesis, and facet syndrome are injuries posterior to vertebral bodies. Spondylolisthesis occurs when bilateral pars defects exist and forward displacement or slippage of a vertebra occurs on the vertebra inferior to it (Chapter 671.6). Facet syndrome has a similar history and physical examination findings as spondylolysis. It is caused by instability or injury to the facet joint, posterior to the pars interarticularis and at the interface of the inferior and superior articulating processes. Facet syndrome can be established by identifying facet abnormalities on CT or by exclusion, requiring a nondiagnostic radiograph and nuclear scan to rule out spondylolysis.
Lumbar Disk Herniation, Strain, and Contusion
Lumbar disk herniation manifests as back pain that is worse with forward flexion, lateral bending, and prolonged sitting, especially in an automobile. It is less likely to produce sciatica in children and adolescents compared to adults (Chapter 671.8). Physical examination findings may be minimal but usually include pain with forward flexion and lateral bending. It is unusual to have a positive straight leg test or any neurologic deficit in young athlete with an injured disk. There may be tenderness of the vertebral spinous process at the level of the disk. MRI usually confirms the clinical diagnosis. Assuming the herniation is not large and the pain is not intractable, the treatment of choice is analgesia and physical therapy. Bed rest or surgery is rarely necessary.
Jones GT, Macfarlane GJ. Epidemiology of low back pain in children and adolescents. Arch Dis Child. 2005;90:312-316.
Micheli LJ, Robert Wood R. Back pain in young athletes: significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995;149(1):15-18.
Standaert CJ. Low back pain in the adolescent athlete. Phys Med Rehabil Clin North Am. 2008;19(2):287-304. ix
679.5 Hip and Pelvis Injuries
Legg-Calvé-Perthes disease (avascular necrosis of the femoral head) also manifests in childhood with insidious onset of limp and hip pain (Chapter 670.3).
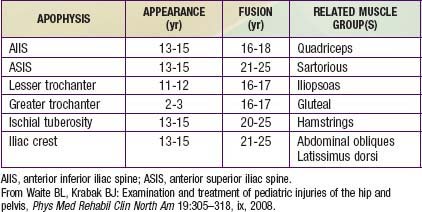
Until the skeleton matures (Table 679-2), younger athletes are susceptible to apophyseal injuries (e.g., the anterior superior iliac spine). Apophysitis develops from overuse or from direct trauma. Avulsion fractures occur in adolescents playing sports requiring sudden, explosive bursts of speed (Fig. 679-8). Large muscles contract and create force greater than the strength of the attachment of the muscle to the apophysis. The most common sites of avulsion fractures (and the attaching muscles) are the anterior superior iliac spine (sartorius), anterior inferior iliac spine (rectus femoris), lesser femoral trochanter (iliopsoas), and ischial tuberosity (hamstrings). Symptoms include localized pain and swelling, with decreased strength and range of motion. Radiographs are required. Initial treatment includes ice, analgesics, rest, and pain-free range-of-motion exercises. Crutches are usually needed for ambulation. Surgery is usually not indicated because most of these fractures—even large or displaced ones—heal well. Contact to the bone around the hip and pelvis causes exquisitely tender subperiosteal hematomas called hip pointers. Symptomatic care includes rest, ice, analgesia, and protection from reinjury.

Figure 679-8 Apophyseal avulsion, pelvis.
(From Anderson SJ: Sports injuries, Curr Prob Pediatr Adolesc Health 35:105–176, 2005.)
Slipped capital femoral epiphysis usually occurs in the 11-15 yr age range during the time of rapid linear bone growth (Chapter 670.4).
Bahr R, Khan K. Management of lateral hip pain. BMJ. 2009;338:961-962.
Metzmaker JN, Pappas AM. Avulsion fractures of the pelvis. Am J Sports Med. 1985;13:349-358.
Waite BL, Krabak BJ. Examination and treatment of pediatric injuries of the hip and pelvis. Phys Med Rehabil Clin North Am. 2008;19:305-318. ix
679.6 Knee Injuries
The knee is the most common musculoskeletal site for complaints among adolescents; some youth may be more prone to such injuries (Table 679-3). Acute knee injuries that cause immediate disability are likely to be due to fracture, patellar dislocation, anterior cruciate ligament (ACL) injury, or meniscal tear. The mechanism of injury is usually a weight-bearing event. After injury, if a player cannot bear weight within a few minutes, a fracture or significant internal derangement is more likely. If a player is able to bear weight and return to play after the injury, a serious injury is less likely to have occurred. If the knee swells within several hours of the injury, the swelling is likely due to a hemarthrosis and a more severe injury.
Table 679-3 SUMMARY OF MODIFIABLE AND NONMODIFIABLE INTRINSIC RISK FACTORS RELATED TO INCREASED RISK OF INJURY OF THE ANTERIOR CRUCIATE LIGAMENT
| MODIFIABLE RISK FACTORS | NONMODIFIABLE RISK FACTORS | POTENTIAL CONTROL OR TREATMENT TECHNIQUE |
|---|---|---|
| ANATOMIC | ||
| BMI | Monitor and control relative body mass | |
| Femoral notch index (ACL size) | NM training targeted to decrease other risk factors | |
| Knee recurvatum | NM training targeted to improve dynamic knee flexion | |
| General joint laxity | NM training targeted to improve joint stiffness | |
| Family history (genetic predisoposition) | NM training targeted to decrease other risk factors | |
| Prior injury history | Full physical rehabilitation following injury | |
| DEVELOPMENTAL AND HORMONAL | ||
| Sex, female | NM training prior to onset of risk factors | |
| Pubertal and post-pubertal maturation status | NM training during pre-puberty | |
| Preovulatory menstrual status | Oral contraceptives in female patients* | |
| ACL tensile strength | NM training targeted to decrease other risk factors | |
| Neuromuscular shunt | NM training targeted to improve neuromuscular control | |
| BIOMECHANICAL | ||
| Knee abduction | NM training targeted to improve coronal plane loads | |
| Anterior tibial shear | NM training targeted to improve dynamic knee flexion | |
| Lateral trunk motion | NM training targeted to improve trunk strength and control | |
| Tibial rotation | NM training targeted to control transverse motions and influence sagittal plane deceleration mechanics | |
| Dynamic foot pronation | Foot orthoses | |
| Fatigue resistance | Strength and conditioning training | |
| Ground reaction forces | NM training targeted to improve force absorption strategies | |
| NEUROMUSCULAR | ||
| Relative hamstring recruitment | NM training targeted to improve hamstring strength and recruitment | |
| Hip abduction strength | NM training targeted to improve high strength and recruitment | |
| Trunk proprioception | NM training targeted to improve trunk strength and control | |
ACL, anterior cruciate ligament; BMI, body mass index; NM, neuromuscular.
* Pilot evidence indicates it might be a potential control strategy.
From Alentorn-Geli E, Myer GD, Silvers HJ, et al: Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: mechanisms of injury and underlying risk factors, Knee Surg Sports Traumatol Arthrosc 7:705–709, 2009.
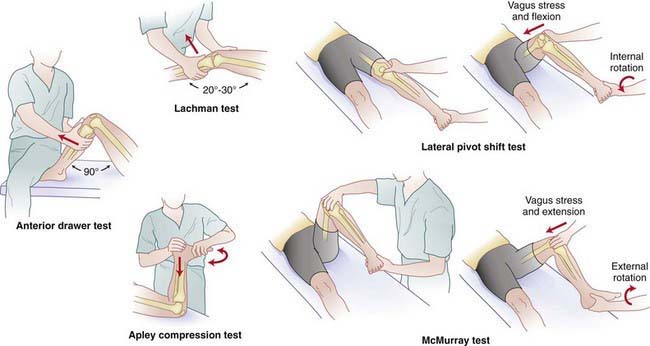
Initial Treatment of Acute Knee Injuries
The physician should inspect for an effusion and obvious deformities; if any deformity is present, the physician should assess neurovascular status and transfer the patient for emergency care. If no gross deformities are present and neurovascular integrity is intact, initial maneuvers include full passive extension and gentle valgus stress to the knee while it is in extension. If there is laxity of the knee with valgus stress in full extension, both the ACL and MCL have been injured. The patient’s ability to contract the quadriceps muscles should be noted. Pain occurring with quadriceps contraction or inability to contract the quadriceps muscle implies an injury to the extensor mechanism. Tenderness over the medial patella, medial retinaculum, and/or above the adductor tubercle is associated with a patellar dislocation. Point tenderness is consistent with fracture or injury to the underlying structure; a medial meniscal tear can manifest as tenderness along the medial joint line, but medial joint line tenderness is not specific for a medial meniscus tear. Pain or limitation in either passive flexion or extension while rotating the tibia implies a meniscal injury, as do other maneuvers (Fig. 679-9). Ligament injury is manifested as pain or laxity with the appropriate maneuver.
Chronic Injuries
Patellofemoral Stress Syndrome
Patellofemoral stress syndrome (PFSS) is the most common cause of anterior knee pain. PFSS is also known as patellofemoral pain syndrome or patellofemoral dysfunction (Chapter 669.5). It is a diagnosis of exclusion used to describe anterior knee pain that has no other identifiable pathology. Pain is usually difficult to localize. Patients indicate a diffuse area over the anterior knee as the source, or they might feel as if the pain is coming from behind the patella. Bilateral pain is common, and pain is often worse going up stairs, after sitting for prolonged periods, or after squatting or running. There should be negative history for significant swelling, which would indicate a more serious injury. History of change in activity is common, such as altered training surface or terrain, increased training regimen, or performance of new tasks.
Osgood-Schlatter Disease
Osgood-Schlatter disease is a traction apophysitis occurring at the insertion of the patellar tendon on the tibial tuberosity (Chapter 669.4). Because it is also related to overuse of the extensor mechanism, Osgood-Schlatter disease is treated like PFSS. A protective pad to protect the tibial tubercle from direct trauma can be used. The most common complication is cosmetic; the tibial tubercle on the affected side (or both if bilateral) may be slightly more prominent. Patients only need to take time from sports if they are limping.
Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33:524-530.
Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;7:705-709.
Frobell RB, Roos EM, Roos HP, et al. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363:331-342.
LaBotz M. Patellofemoral syndrome: diagnostic pointers and individualized treatment. Phys Sportsmed. 2004;32:7.
Macmull S, Skinner JA, Bentley G, et al. Treating articular cartilage injuries of the knee in young people. BMJ. 2010;340:587-592.
Spindler KP, Wright RW. Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135-2142.
Van Linschoten R, van Middelkoop M, Berger MY, et al. Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open label randomized controlled trial. BMJ. 2009;339:1010-1013.
Vaquero J, Vidal C, Cubillo A. Intra-articular traumatic disorders of the knee in children and adolescents. Clin Orthop. 2005;432:97-106.
679.8 Ankle Injuries
Examination and Injury Grading Scale
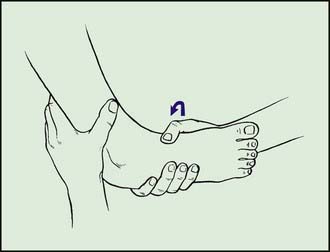
Provocative testing attempts to evaluate the integrity of the ligaments. In a patient with a markedly swollen, painful ankle, provocative testing is difficult because of muscle spasm and involuntary guarding. It is more useful on the field before much bleeding and edema have occurred. The anterior drawer test assesses for anterior translation of the talus and competence of the anterior talofibular ligament. The inversion stress test examines the competence of the anterior talofibular and calcaneofibular ligaments (Fig. 679-10). In the acute setting, the integrity of the tibiofibular ligaments and syndesmosis is examined by the syndesmosis squeeze test. Pain with squeezing the lower leg implies injury to the interosseous membrane and syndesmosis between the tibia and fibula, making a severe injury more suspicious. Athletes with this injury cannot bear any weight and also have severe pain with external rotation of the foot. Occasionally the peroneal tendon dislocates from the fibular groove simultaneously with an ankle sprain. To assess for peroneal tendon instability, the examiner applies pressure from behind the peroneal tendon with resisting eversion and plantar flexion, and the tendon pops anteriorly. If either a syndesmotic injury or an acute peroneal dislocation is suspected, orthopedic consultation should be sought.
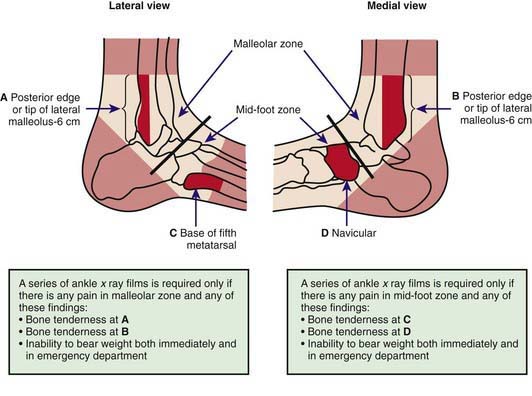
Radiographs
AP, lateral, and mortise views of the ankle are obtained when patients have pain in the area of the malleoli, are unable to bear weight, or have bone tenderness over the posterior distal tibia or fibula. The Ottawa ankle rules help define who requires radiographs (Fig. 679-11). A foot series (AP, lateral, and oblique views) should be obtained when patients have pain in the area of the midfoot or bone tenderness over the navicular or 5th metatarsal. It is important to differentiate an avulsion fracture of the proximal 5th metatarsal from the Jones fracture of the proximal 5th metatarsal (a lucency about 2 cm from the proximal end). The former is treated as an ankle sprain; the latter fracture has an increased risk of nonunion and requires orthopedic consultation. The talar dome fracture is manifested as an ankle sprain that does not improve. Radiographs on initial presentation can have subtle abnormalities. Any suspicion on the initial radiographs of a talar dome fracture warrants orthopedic consultation and further imaging. In the early adolescent, always look carefully at the tibial epiphysis. Nondisplaced Salter III fractures can be subtle and need to be recognized early and referred to an orthopedic surgeon promptly.
679.9 Foot Injuries
Sever disease (calcaneal apophysitis) occurs at the insertion of the Achilles tendon on the calcaneus and manifests as activity-related pain (see Fig. 679-3). It is more common in boys (2 : 1), is often bilateral, and usually occurs between ages 8 and 13 yr. Tenderness is elicited at the insertion of the Achilles tendon into the calcaneus, especially with squeezing the heel (positive squeeze test). Sever disease is associated with tight Achilles tendons and midfoot hyperpronation that puts more stress on the plantar flexors of the foot. Treatment includes relative rest, ice, massage, stretching, and strengthening the Achilles tendon. Correcting the midfoot hyperpronation with orthotics, arch supports, or better shoes is important in most athletes with Sever disease. If the foot is neutral or there is mild hyperpronation,  -in heel lifts will be helpful to unload the Achilles tendon and its insertion. With optimal management, symptoms improve in 4-8 wk. Generally, if there is no limp during the athletic activity, young athletes with Sever disease should be allowed to play.
-in heel lifts will be helpful to unload the Achilles tendon and its insertion. With optimal management, symptoms improve in 4-8 wk. Generally, if there is no limp during the athletic activity, young athletes with Sever disease should be allowed to play.
Bachmann LM, Kolb E, Koller MT, et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot; systematic review. BMJ. 2003;326:417-419.
Bessen T, Clark R, Shakib S, et al. A multifaceted strategy for implementation of the Ottawa ankle rules in two emergency departments. BMJ. 2009;339:b3056.
Beynnon BD, Renström PA, Haugh L, et al. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. Am J Sports Med. 2006;34:1401-1412.
Buchbinder R. Plantar fasciitis. N Engl J Med. 2004;350:2159-2166.
Glazer JL, Brukner P, Haverstock BD. Stress fractures of the foot and ankle. Clin Podiatr Med Surg. 2001;18:273-284.
Hertel J. Immobilization for acute severe ankle sprain. Lancet. 2009;373:524-526.
Heyworth J. Ottawa ankle rules for the injured ankle. Br Med J. 2003;326:405-406.
Hupperets MDW, Verhagen EALM, van Mechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomized controlled trial. BMJ. 2009;339:276-278.
Kennedy JG, Knowles B, Dolan M, et al. Foot and ankle injuries in the adolescent runner. Curr Opin Pediatr. 2005;17:34-42.
Lamb SE, Marsh JL, Hutton JL, et al. Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomized controlled trial. Lancet. 2009;373:575-581.
Malanga GA, Ramirez-Del Toro JA. Common injuries of the foot and ankle in the child and adolescent athlete. Phys Med Rehabil Clin North Am. 2008;19(2):347-371. ix
Mayer D. The injured ankle and foot. BMJ. 2009;339:400-401.
Nilsson-Helander K, Silbernagel KG, Thomee R, et al. Acute Achilles tendon rupture. Am J Sports Med. 2010;38(11):2186-2193.
Pihlajamäki H, Hietaniemi K, Paavola M, et al. Surgical versus functional treatment for acute ruptures of the lateral ligament complex of the ankle in young men. J Bone Joint Surg Am. 2010;92:2367-2374.
Van Rijn RM, van Ochten J, Luijsterburg PAJ, et al. Effectiveness of additional supervised exercises compared with conventional treatment alone in patients with acute lateral ankle sprains: systematic review. BMJ. 2010;341:c5688.
Verhagen EA. Neuromuscular training after acute lateral ankle sprain. BMJ. 2010;341:c5722.
Waterman BR, Belmont PJ, Cameron KL, et al. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010;38:797-803.


 speed,
speed,  speed, and finally to sprints. The athlete must stop if there is significant pain or limp. Finally, before returning to sport, the athlete must be able to sprint and change directions off the injured ankle comfortably. Performing some sport-related tasks is also helpful in determining readiness for return to play.
speed, and finally to sprints. The athlete must stop if there is significant pain or limp. Finally, before returning to sport, the athlete must be able to sprint and change directions off the injured ankle comfortably. Performing some sport-related tasks is also helpful in determining readiness for return to play.





