Surgical Management of Hereditary Nonpolyposis Colorectal Cancer
Hereditary nonpolyposis colorectal cancer (HNPCC), often called Lynch syndrome, may be described as a hereditary predisposition to developing colorectal and extracolonic cancers. Accounting for approximately 3% of all colorectal malignancies, it is the most common cause of hereditary colorectal cancer [1]. The diagnosis is based on clinical criteria related to family history of certain HNPCC-defining cancers, such as those of the colorectum, uterus, stomach, ovaries, urinary epithelium, and small bowel. The syndrome is characterized by early onset of cancer, and an elevated clinical suspicion is needed to make a timely diagnosis so that appropriate surveillance and intervention can be performed to decrease deaths from cancer. This review provides a brief background on HNPCC and reviews the surgical management of the disease.
Clarification of terms: HNPCC and Lynch syndrome
The terms HNPCC and Lynch syndrome have often been used synonymously; however, a greater understanding of the molecular mechanisms underlying cancer development in this disease has led to more precise definitions. In 1985, Henry Lynch introduced the term HNPCC to describe a syndrome that he thought was characterized by an autosomal dominant inheritance pattern, early onset of cancers, multiple colorectal cancers, and extracolonic cancers, most notably those of the endometrium and ovaries [2,3]. As clinical cancer registries began to form, the need for standardized definitions to facilitate communication and clinical research became apparent. Subsequently, the Amsterdam I criteria (Box 1) were proposed in 1991 to define families that were considered to have HNPCC [4]. These criteria did not capture the full extent of the syndrome and were later revised in 1999 (Amsterdam II) to include extracolonic cancers in an effort to improve sensitivity [5]. More recently, some groups have broadened the clinical criteria (Amsterdam-like) to allow for inclusion of high-risk adenomas as a surrogate for colorectal cancer to correct for the phenotype attenuation secondary to the increasing use of colonoscopic surveillance and polypectomy [6].
Box 1 Amsterdam criteria that define HNPCC
The underlying genetic cause of cancers associated with HNPCC was identified in 1993 as a heritable mutation in the DNA mismatch repair (MMR) mechanism [7–9]. As genetic and molecular laboratory techniques developed, this finding allowed for a more accurate identification of kindred with truly increased risk of developing malignancy. Importantly, among patients with known hereditary MMR deficiency, only approximately 40% meet the Amsterdam criteria [1]. Conversely, only approximately 50% to 60% of patients that meet the Amsterdam criteria will carry a known MMR defect [10]. Therefore, to be more precise, it has been suggested that Lynch syndrome moniker be reserved for patients with an MMR gene mutation [11]. In lieu of genetic testing, patients meeting the Amsterdam criteria who develop a cancer that is microsatellite unstable are putatively considered to have Lynch syndrome because MMR deficiency results in tumor microsatellite instability. Thus, the Amsterdam criteria are used to define HNPCC and can, then, be used as a guide to help clinicians determine those who may benefit from genetic counseling and testing to identify true Lynch syndrome, defined as a family that harbors a germline defect in the MMR mechanism. Patients who meet the Amsterdam criteria (and thus HNPCC) but have microsatellite stable tumors have been coined as familial colorectal cancer type X [12], which is briefly discussed later.
The late pathologist Jeremy Jass clarified the confusing nomenclature in the following way: “The Lynch syndrome is best understood as a hereditary predisposition to malignancy that is explained by a germline mutation in a DNA MMR gene. The diagnosis does not depend in an absolute sense on any particular family pedigree structure or age of onset of malignancy. If present, these are merely useful clinical pointers that have been accorded undue importance when considered in isolation of other facts. No simple set of clinical criteria can serve as a diagnostic label for Lynch syndrome. At the same time, the careful appraisal of clinical, pathologic and molecular features can achieve an accurate working diagnosis before the demonstration of a pathogenic germline mutation in a DNA mismatch repair gene” [11].
Cancer risk in Lynch syndrome
It is well-known that patients with Lynch syndrome are at increased risk for developing cancer compared with the general population. For MMR mutation carriers, the incidence of colorectal cancer is approximately 60% to 80% and the incidence of uterine cancer is approximately 40% to 60% [13–17]. Cancers of the stomach and ovaries are the next most common, with incidence of approximately 7% to 19% and 9% to 13%, respectively [14,18]. Less common tumors but still with increased incidence compared with the general population include those of the hepatobiliary tract (2%–7%), urinary epithelium (4%–5%), small bowel (1%–4%), pancreas (3%–4%), and brain or central nervous system (1%–3%).
Surveillance for colorectal cancer
The goal of surveillance is to detect precursor lesions before they develop into cancer and thus prevent cancer-related deaths. Multiple studies have shown that surveillance by colonoscopy in patients with Lynch syndrome decreases the development of, and the number of deaths from, colorectal cancer [15,19–21]. Patients with cancer before 20 years of age are extremely rare, and thus, the first colonoscopy is recommended at age 20 to 25 or 10 years younger than the earliest cancer in the family with subsequent surveillance every 1 to 2 years [19,22,23].
Surgical indications and surgical management
Colon and colon cancer
Prophylactic colectomy in Lynch syndrome is not a common practice, nor is it recommended. Prospective clinical studies evaluating potential survival advantages of prophylactic colectomy in Lynch syndrome have not been performed. A decision analysis–based statistical model suggests a survival benefit of 1.8 years for patients undergoing a subtotal colectomy at 25 years of age compared with surveillance by colonoscopy, with decreasing benefit when surgery is performed at increasing age [24]. It is the author’s opinion that prophylactic colectomy outside the setting of colorectal cancer should only be offered in special circumstances. Examples of these situations include patients who have a colon that is technically difficult to examine endoscopically, those with poor compliance to screening recommendations, and those who have severe psychological fear of developing colorectal cancer and choose to undergo colectomy rather than surveillance. Consideration for early intervention and prophylactic surgery may also be given for patients in families with severe penetrance of disease or early age onset of colorectal cancer. Another instance in which prophylactic colectomy may be considered is when a female patient with uterine cancer is undergoing abdominal hysterectomy. Given the lifetime risk of developing colon cancer is 80%, simultaneous prophylactic colectomy and ileorectal anastomosis (IRA) at the time of hysterectomy is a reasonable option.
The most common indication for colonic resection in patients with Lynch syndrome is the treatment of colon cancer. Although uncommon, a patient with an adenoma burden that cannot be effectively controlled endoscopically justifies a decision for colectomy. Because the entire colorectal mucosa is unstable and at risk for developing cancer, the preferred surgical option in Lynch syndrome is complete colectomy with an IRA [6,23,25], which involves the concept of both therapeutic resection to treat the cancer and prophylactic surgery via removal of the remainder of the colon that carries the risk of metachronous malignancy. Although no prospective trials have been undertaken to demonstrate a survival benefit for colectomy and IRA compared with segmental colectomy, the metachronous cancer risk and mathematical models favor total colectomy. A Markov decision model revealed increased life expectancy of 2.3 years if the cancer was treated by total colectomy compared with segmental colectomy at 27 years of age. When cancer was diagnosed and treated at later ages, the life expectancy benefit persisted but decreased in magnitude with age [26]. The risk of developing a metachronous colon cancer after partial colectomy has been reported between 11% and 45%, with a moderate follow-up of 8 to 13 years [6,15,16,27–30]. It is reasonable to assume increasing rates of metachronous disease with longer follow-up, and risks have been estimated to be as high as 72% at 40 years [16]. The true cancer risk may be higher than reported because high-risk adenomas are found and removed, and thus preventing cancer, in 33% of patients after segmental colectomy [6]. Although colectomy removes most mucosa at risk for cancer, the remaining rectum still requires yearly surveillance. The risk of metachronous rectal cancer after IRA has been reported between 3% and 12% at 10 to 12 years [6,15,28].
Despite recommendations for colectomy and IRA, most colorectal cancers in the United States are still treated by segmental colectomy [6,29]. First, a diagnosis of HNPCC may not be recognized at the time of surgery, and thus, the indications for extended colectomy are not realized. Second, although patients may be accurately diagnosed, they may choose not to undergo a more extensive operation. Third, patients with significant comorbidities, those with low life expectancy, or those who have poor anal muscle tone may be better served by a more limited operation that also preserves more colon for better function. Regardless of the rationale for surgical choice, patients and clinicians need to be aware of the expectations and future cancer risk.
As a word of caution, interval cancers still develop between scheduled colonoscopies even with strict surveillance regimens of every 1 to 2 years [6,19,31]. Possible explanations include a faster adenoma-to-carcinoma progression in Lynch syndrome [31–33], a higher prevalence of adenomas with high-grade dysplasia and villous histology in Lynch syndrome, and difficulty detecting these often flat adenomas [34]. One study reports a missed adenoma rate of up to 55% using conventional colonoscopy in patients with Lynch syndrome [34]. Despite these factors, there are no data that prophylactic completion colectomy after a segmental colectomy improves survival, and it is not recommended unless a second cancer is found.
One concern regarding a more extensive surgery such as total colectomy compared with segmental colectomy is an increased number of bowel movements and patients’ quality of life. One study specifically looking at this issue in HNPCC evaluated 22 patients who underwent total colectomy and IRA and analyzed the frequency of bowel movements, rate of incontinence, and quality of life using the Short Form-36. The control group consisted of 22 patients with HNPCC who were treated by left or right hemicolectomy. At 24 months follow-up, the bowel frequency was greater for patients undergoing total colectomy (4 vs 2 bowel motions daily, P<.05), but this was not associated with any difference in continence or quality of life [35]. In addition, total colectomy is safe and has been shown to have similar perioperative mortality compared with a right colectomy, even in elderly populations [36,37].
The increasing use of laparoscopic surgery to perform colectomy has made the concept of total colectomy more acceptable to patients and referring physicians. The laparoscopic approach is less invasive and results in smaller incisions, less postoperative pain, quicker discharge from the hospital, and quicker overall return to normal activity compared with an open procedure. Several studies have now demonstrated oncologic equivalence using a laparoscopic approach [38,39], and one study even suggests that oncologic outcomes are improved using laparoscopy [40].
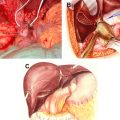
Rectal cancer
Rectal cancer in patients with HNPCC is common, because approximately 20% to 30% of patients will develop rectal cancer, including 15% of patients presenting with rectal cancer as their index cancer [41,42]. Treatment of rectal cancer requires special consideration, and surgical choice remains a pertinent and challenging clinical question. Patients may be treated by proctosigmoidectomy and colorectal or coloanal (with colonic J pouch) anastomosis, abdominoperineal proctectomy, or total proctocolectomy with ileal pouch-anal anastomosis (IPAA). The choice depends on the location of the tumor in relation to the anal sphincters, the existence of colonic disease, the age and comorbidity of the patient, the phenotype expressed in the family (aggressive or mild), and surgeons’ experience and expertise. Using similar reasoning for extended resection in colon cancer, the definitive therapeutic and prophylactic treatment of rectal cancer would involve total proctocolectomy with creation of an IPAA if the cancer permits sphincter preservation. Although no one argues the need for proctectomy, there is often debate about the use of simultaneous prophylactic colectomy. Proctectomy alone with colorectal anastomosis yields less frequent bowel movements and more normal function than an IPAA. However, this option leaves an entire colon at risk for the development of metachronous cancer and leads to the need for fastidious annual surveillance. Surgical decision making relies on multiple factors as stated earlier and also includes patient reliability for compliance. All these factors must be weighed against the risk of developing cancer in the remaining colon that is prone to further neoplasia. The natural history of the colon after proctectomy in Lynch syndrome is scarcely described in the literature. In a study from the Roswell Park Cancer Institute, 18 patients either meeting the Amsterdam criteria or with a documented germline MMR mutation presented with an index rectal cancer and were treated by proctectomy without colectomy. One patient died of advanced disease, and 3 of 17 patients (18%) developed metachronous cancer at a median of 203 months after the initial surgery [41]. A report from Germany described 6 of 11 patients with HNPCC (54%) developing metachronous colon cancer at a median of 7.4 years after proctectomy [42]. Recently presented but yet unpublished data from the Cleveland Clinic (by Matthew F. Kalady, 2010) examined 31 patients with HNPCC in follow-up after proctectomy. At a median follow-up of 106 months, 5 patients developed metachronous colon cancer and an additional 9 patients developed high-risk adenomas. Thus, 14 of 31 patients (45%) developed significant colonic neoplasia. The cumulative risk will increase over time in all these patients because cancer development increases with age in the setting of an inherent unstable colonic mucosa caused by an inherited MMR deficiency. Until more extensive natural history studies become known, informed decisions are made based on the best available information. Because the risk of subsequent colon cancer is high, proctocolectomy should be considered and is recommended for rectal cancer in Lynch syndrome in medically fit patients. If patients undergo less than total proctocolectomy, annual endoscopic surveillance of the colon is mandatory.
Management of the uterus and ovaries in Lynch syndrome
Women with Lynch syndrome carry an approximate 40% and 10% cancer risk of the uterus and ovaries, respectively, with a mean age of onset in the fifth decade of life. Screening for endometrial cancer suggests the ability to detect premalignant lesions at an earlier stage [43], although no direct evidence has shown a decrease in cancer rates. Some guidelines recommend that women with Lynch syndrome begin annual endometrial cancer screening at 30 to 35 years of age by transvaginal ultrasonography and endometrial biopsy [44]. The National Comprehensive Cancer Network recommends gynecologic oncologist referral for screening for gynecologic tumors and encourages patient education regarding the need to evaluate endometrial cancer symptoms [22]. If a patient is undergoing surgery for colon cancer beyond their reproductive years or the woman has decided that she has completed childbearing, it is generally recommended to perform a prophylactic hysterectomy and bilateral oophorectomy at the time of colectomy, especially if there is uterine cancer in the family [45].
Familial colorectal cancer type X
As stated previously, approximately 50% of patients fulfilling the Amsterdam criteria do not carry an MMR germline mutation. These families have microsatellite-stable tumors and have different clinical characteristics and decreased cancer risks compared with the families with Lynch syndrome [12]. Families with clustering of colorectal cancers but without documented MMR defect are at a higher risk for developing colon cancer than the average population. This group likely represents a heterogeneous mix of families with varying genetic predispositions that we do not yet fully understand or realize. Some groups recommend colonoscopic surveillance to start 10 years earlier than the first colorectal cancer in the family or at 45 years of age and subsequently at 3- to 5-year intervals [46]. Because the risk of metachronous colorectal cancer is not defined, these cancers are generally treated surgically like sporadic cancers. There is no known increased risk of endometrial or other extracolonic cancers, and increased screening or prophylactic resections are not recommended.