45
Malpresentations and malpositions
Introduction
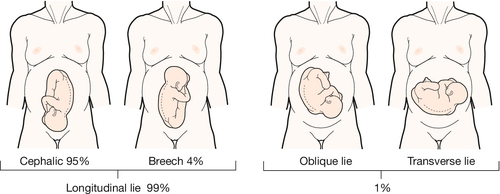
During pregnancy, abdominal palpation should aim to define the lie, presentation and position of the fetus. The lie refers to the long axis of the fetus in relation to the long axis of the uterus. Usually, the fetus is longitudinal, but occasionally it may be transverse or oblique. The presentation is that part of the fetus which is at the pelvic brim, in other words the part of the fetus presenting to the pelvic inlet. Normal presentation is the vertex of the fetal head and the word ‘malpresentation’ describes any non-vertex presentation. This may be of the face, brow, breech, or some other part of the body if the lie is oblique or transverse.
The position of the fetus refers to the way in which the presenting part is positioned in relation to the maternal pelvis. Strictly speaking this refers to any presenting part, but here it will be considered in relation to those fetuses presenting head first (cephalic). As we have seen, the head is usually occipitotransverse at the pelvic brim and rotates to occipitoanterior at the pelvic floor. ‘Malposition’ is when the head, coming vertex first, does not rotate to occipitoanterior, presenting instead as persistent occipitotransverse or occipitoposterior.
Malpresentation
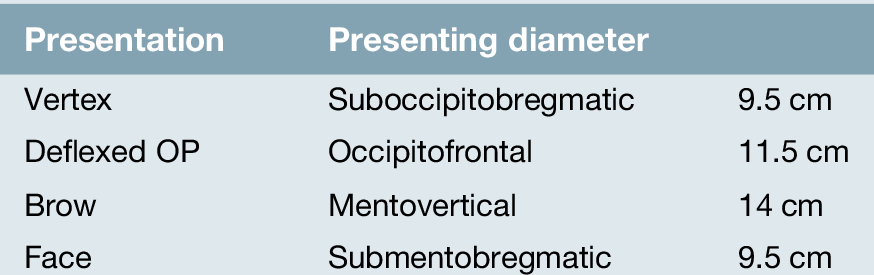
As described above, ‘malpresentation’ is a term used to describe any non-vertex presentation. Over 95% of fetuses are in cephalic presentation at term. Malpresentations include face presentation, brow presentation and breech presentation. When the fetus has a cephalic presentation, the presenting diameter is dependent on the degree of flexion or extension of the fetal head – deflexed and brow presentations offer a wide diameter to the pelvic inlet (Table 45.1 and Fig. 45.1).
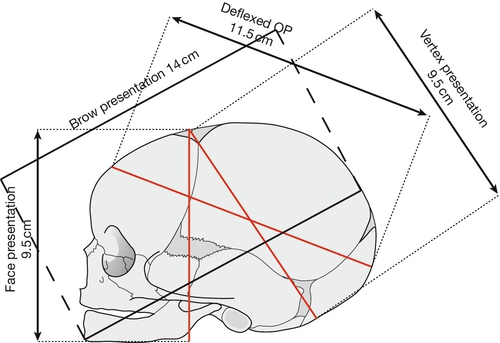
As the fetal skull is made up of individual bony plates (the occipital, sphenoid, temporal and ethmoid bones), which are joined by cartilaginous sutures (the frontal, sagittal, lambdoid and coronal sutures), it has the potential to be ‘moulded’ during labour. This allows the head to fit the birth canal more closely (Fig. 45.2). Moulding should be distinguished from caput succedaneum, which refers to oedema of the presenting part of the scalp. Both moulding and caput can occur in any cephalic presentation, but are more likely to occur in malpresentation. The presence or absence of moulding and caput should be documented during each vaginal examination in labour; excessive moulding and caput are suggestive of an obstructed labour due to cephalopelvic disproportion.
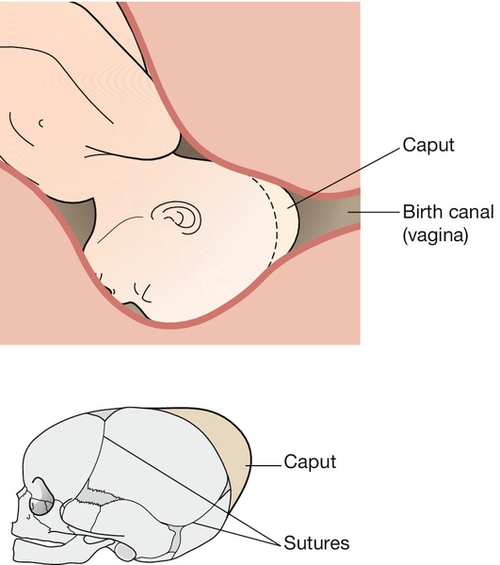
Caput refers to oedema of the presenting part of the scalp.
Face presentation
This occurs in about 1:500 births and occurs when the fetal head extends right back (hyperextended so that the occiput touches the fetal back) (Fig. 45.3 A). It is associated with prematurity, tumours of the fetal neck, loops of cord around the fetal neck, fetal macrosomia and anencephaly. Face presentation is usually only recognized after the onset of labour and, if the face is swollen (Fig. 45.3 B), it is easy to confuse this presentation with that of a breech. The position of the face is described with reference to the chin, using the prefix ‘mento’. The presenting diameter is submentobregmatic (9.5 cm) (Fig. 45.1).
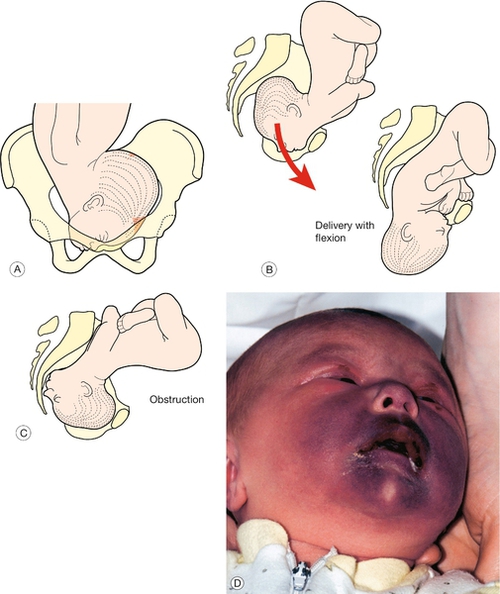
(A) The head enters the pelvic brim in the transverse position. (B) Most rotate to the mentoanterior position and deliver without problems. (C) Those that rotate to mentoposterior will obstruct. (D) Face presentation is often associated with oedema and bruising. This baby recovered without problems.
The face usually enters the pelvis with the chin in the transverse position (mentotransverse) and 90% rotate to mentoanterior so that the head is born with flexion (Fig. 45.3 C). If mentoposterior, the extending head presents an increasingly wider diameter to the pelvis, leading to worsening relative cephalopelvic disproportion and impacted obstruction (Fig. 45.3 D). A caesarean section is usually required.
Brow presentation
This occurs in only approximately 1:700 and 1:1500 births and is the least favourable for delivery (Fig. 45.4). The presenting diameter is mentovertical, measuring 14 cm. The supraorbital ridges and the bridge of the nose will be palpable on vaginal examination. The head may flex to become a vertex presentation or extend to a face presentation in early labour. If the brow presentation persists, a caesarean section will be required.
Breech presentation
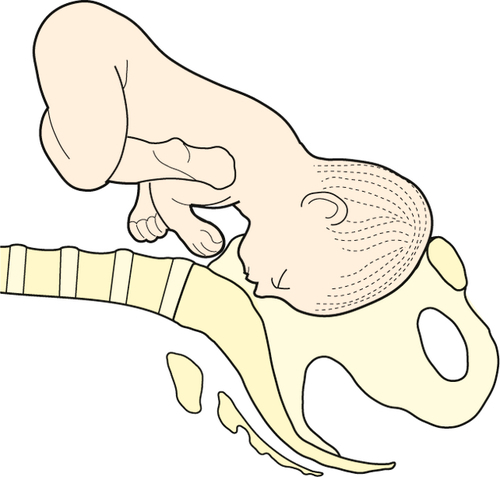
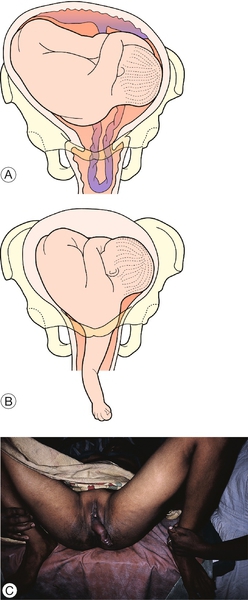
Breech presentation describes a fetus presenting bottom first. The incidence is around 40% at 20 weeks, 25% at 32 weeks and only 3–4% at term. The chance of a breech presentation turning spontaneously after 38 weeks is < 4%. Breech presentation is associated with multiple pregnancy, bicornuate uterus, fibroids, placenta praevia, polyhydramnios and oligohydramnios. It may also rarely be associated with fetal anomaly, particularly neural tube defects, neuromuscular disorders and autosomal trisomies. At term, 65% of breech presentations are frank (extended) with the remainder being flexed or footling (Fig. 45.5). Footling breech carries a 5–20% risk of cord prolapse (p. 367).
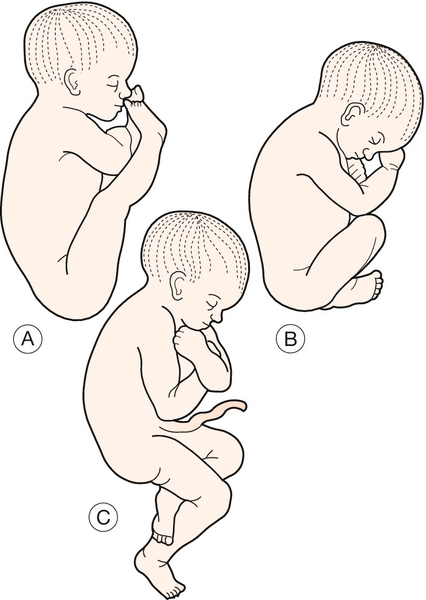
Those presenting by the breech may be (A) extended (or frank); (B) flexed; or (C) footling.
Mode of delivery
There has been extensive debate about the safest route of delivery – whether it should be vaginal or by caesarean section. The risks of vaginal delivery are small, but include intracranial injury, widespread bruising, damage to internal organs, spinal cord transection, umbilical cord prolapse and hypoxia following obstruction of the after-coming head. The risks of caesarean section are largely maternal and related to surgical morbidity and mortality. There is now evidence that planned caesarean section is associated with less perinatal mortality and less serious neonatal morbidity than planned vaginal birth at term. The risks of serious maternal complications are much about the same, partly because planned vaginal delivery often ends with an intrapartum caesarean section and such caesarean sections carry greater risks than planned elective sections. The problem of delivery can be removed if it is possible to turn the baby prior to the onset of labour. This process is called external cephalic version.
External cephalic version (ECV)
All women with an uncomplicated breech pregnancy at term should be offered ECV. It is good practice to offer ECV from 36 weeks in nulliparous women and from 37 weeks in multiparous women. There is no point in attempting ECV with a significant placenta praevia, as a caesarean section will still be required; other relative and absolute contraindications to ECV are outlined in Box 45.1.
Procedure
A cardiotocograph and ultrasound scan should be performed. Some obstetricians like the patient to be fasted and prepared for theatre, and although this is usually not necessary, it is reasonable to have access to theatre close at hand. ECV is most likely to be successful in parous women and when the presenting part is free, the liquor volume is normal, the head is easy to palpate and the uterus feels soft. A flexed breech is more likely to turn than an extended (frank) breech.
Ask the mother to lie flat with a 30° lateral tilt. The use of tocolysis, such as a betamimetic drug, to soften the uterus is associated with an increased success rate. Applying scanning gel to the abdomen allows easier manipulation and permits scanning during the procedure if required. Disengage the breech with the scan probe or hands, and then attempt to rotate in the direction in which the baby is facing (i.e. forward roll). Check the fetal heart every 2 min. If unsuccessful, a backward somersault can be tried. If the procedure is only partially successful (i.e. the fetus is converted to a transverse lie), return the fetus to breech rather than leave it transverse. Give anti-D 500 IU i.m. if rhesus negative and perform a CTG after the procedure is completed. The success rate of version is ~ 30% for primigravidae and ~ 50% for parous women.
Caesarean section for breech presentation
The evidence quoted above considers term pregnancies only. It is probably also advisable to carry out a caesarean section in pre-term deliveries, as there is the additional risk of the cervix closing around the neck after delivery of the breech. Whether caesarean section is also appropriate in extreme prematurity is more difficult to assess, as the delivery may still be traumatic for the baby. In this instance, the operation should be performed by an experienced obstetrician.
Vaginal delivery for breech presentation
This may occasionally be considered appropriate by some clinicians if the estimated fetal weight is < 3.8 kg and there is no fetal compromise, pre-eclampsia or placenta praevia. Ideally, the onset of labour should be spontaneous, the breech frank or flexed (but not footling) and the liquor volume normal. Those not assessed antenatally and presenting in advanced labour with an engaged breech usually deliver without adverse consequences.
The first stage is managed with caution. The role of epidural analgesia is particularly controversial – its use may facilitate manipulation of the fetus, but its presence may inhibit the desire to push, which is particularly important in breech delivery. Augmentation must only be used if disproportion has been excluded and even then with caution. There is no contraindication to a fetal ‘scalp’ electrode being applied to the breech, providing care is taken to avoid genital injury.
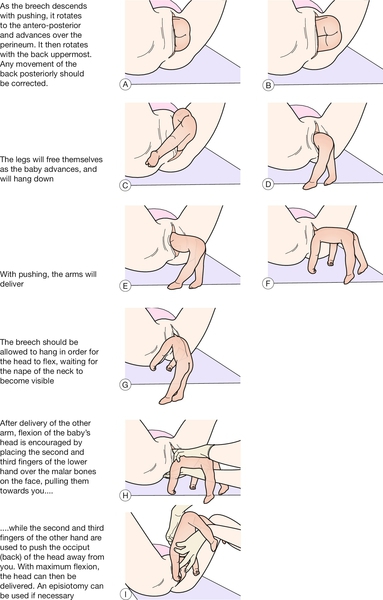
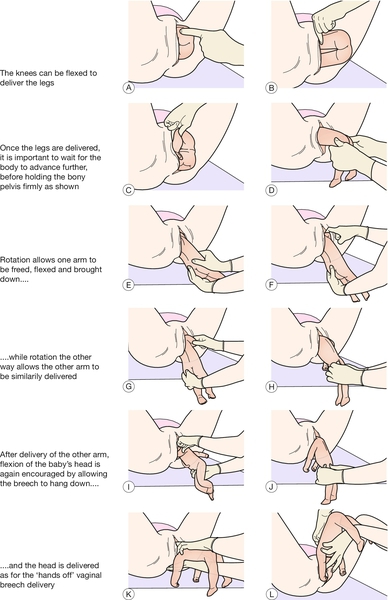
At full dilatation, the mother can be encouraged to push: the temptation to pull must be resisted. Ideally, the baby should be left alone to delivery itself (‘hands off’), taking care to ensure the back remains uppermost when advancing. If there is undue delay, or there are concerns about fetal well-being (e.g. movements stopping, baby becoming floppy, no response to stimuli), assisted delivery can be used to encourage a more rapid delivery. The techniques of ‘hands off’ and ‘assisted breech’ are illustrated in Figures 45.6 and 45.7. Breech extraction may be considered when delivering the second twin (p. 313).
One of the key risks of breech delivery is that pulling may lead the head to extend and therefore become stuck at the pelvic brim. The importance of maternal effort at this stage, rather than traction from below, cannot be overemphasized – it allows the head to flex and minimizes the risk of it becoming stuck at the pelvic brim.
Should the head of a pre-term breech become entrapped behind an incompletely dilated cervix, it should first be flexed as far as is possible to narrow the presenting diameter. Failing this, the options are then to incise the cervix at the 4 and 8 o’clock positions (risking massive, potentially fatal maternal haemorrhage) or to push the fetus back up and perform a caesarean section (a very difficult manoeuvre). Because such interventions are very risky to the mother, it may be preferable to await spontaneous delivery.
All babies presenting by the breech should be examined for developmental dysplasia of the hip (p. 406) and Klumpke paralysis (p. 407).
Transverse lie and oblique lie
These are uncommon, occurring in less than 1% of deliveries at term (Fig. 45.8). Usually there is no specific cause, but abnormal lie is more common in multiparous women, multiple pregnancies, pre-term labour and polyhydramnios. It may also be associated with placenta praevia, congenital abnormalities of the uterus, and lower uterine fibroids and other pelvic masses such as an ovarian cyst.
If transverse lie is identified antenatally, a scan should be undertaken to exclude placenta praevia, polyhydramnios, lower uterine fibroids and a pathologically enlarged fetal head. External cephalic version is usually possible (see above), and the mother should be reviewed a few days later to ensure that the lie is still cephalic. She should be advised to come to hospital if there is any suspicion of early labour, as it may still be possible to carry out an external cephalic version at that stage, providing the membranes are still intact. She should also be advised to present to the hospital immediately if there is any suspicion of membrane rupture, as there is a risk of cord prolapse or prolapse of a limb (Fig. 45.9A–C). In view of the small risk of cord prolapse, some clinicians advise that women with a transverse lie or unstable lie (see below) are admitted to hospital from 38 weeks’ to await birth or until a longitudinal lie is maintained (see Table 46.1).
If the lie is transverse in established labour, particularly after membrane rupture, a caesarean section will usually be required. These caesarean sections can be technically very difficult, and a vertical uterine incision may be necessary to allow adequate access for delivery.
Unstable lie
An unstable lie is one that varies from examination to examination. The options are:
![]() manage conservatively, with repeated ECVs as required, and await the spontaneous onset of labour. Should the membranes rupture with the fetus in a non-cephalic presentation there may be a risk of cord prolapse, and, as described above, inpatient management is considered appropriate by some
manage conservatively, with repeated ECVs as required, and await the spontaneous onset of labour. Should the membranes rupture with the fetus in a non-cephalic presentation there may be a risk of cord prolapse, and, as described above, inpatient management is considered appropriate by some
![]() arrange to turn the baby to cephalic presentation and then induce labour. This is sometimes referred to as a ‘stabilizing induction’. The disadvantage is that the induction itself is not without risks, and the lie may become unstable again even after the membranes have been ruptured
arrange to turn the baby to cephalic presentation and then induce labour. This is sometimes referred to as a ‘stabilizing induction’. The disadvantage is that the induction itself is not without risks, and the lie may become unstable again even after the membranes have been ruptured
![]() carry out a caesarean section.
carry out a caesarean section.
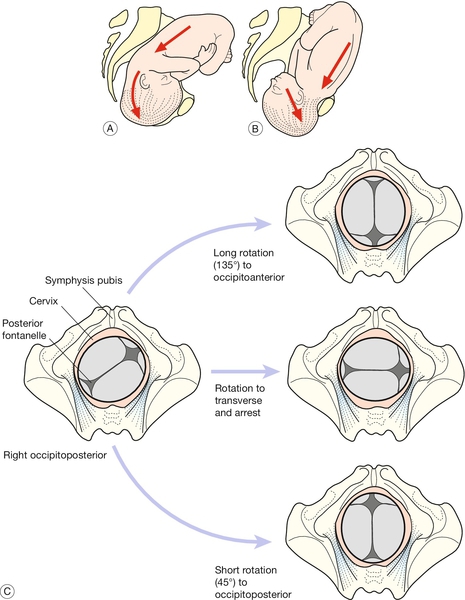
Malposition
Normally, the head engages at the pelvic brim in the occipitotransverse position, flexing as it descends into the pelvic cavity and rotating to occipitoanterior (OA) at the level of the ischial spines. The head then extends as it descends, distending the vulva until it is delivered. In about 10% of pregnancies, the fetal head enters the pelvis in a more occipitoposterior (OP) position than transverse or anterior, either by chance, or in association with an unfavourably shaped pelvis, particularly the long oval ‘anthropoid’ pelvis. The baby is then in a direct occipitoposterior position (DOP), or with the occiput to the right or left of the midline, referred to as right or left occipitoposterior (ROP or LOP).
There are then three main possibilities (Fig. 45.10 C):
![]() the occiput will rotate anteriorly (through approximately 135°) to occipitoanterior, and then (usually) deliver normally (65%)
the occiput will rotate anteriorly (through approximately 135°) to occipitoanterior, and then (usually) deliver normally (65%)
![]() it will partially rotate to occipitotransverse and not deliver (20%)
it will partially rotate to occipitotransverse and not deliver (20%)
![]() it will rotate more posteriorly to occipitoposterior (15%).
it will rotate more posteriorly to occipitoposterior (15%).
Those that remain OP have greater difficulty negotiating the birth canal and are less likely to deliver spontaneously. The normal mechanism of delivery involves extension of the head to OA, but extension is not possible in the OP position and a wider diameter is presented to the outlet (occipitofrontal 11.5 cm) (Table 45.1 and Fig. 45.10 A, B). With malposition, the first and second stages of labour are usually longer, partly because of the greater presenting diameter (relative cephalopelvic disproportion), and partly because the head is less well applied to the cervix and therefore less able to facilitate its dilatation. Back pain in labour appears to be more common with OP position. The mother is more likely to request an epidural, is more likely to experience secondary arrest due to relative cephalopelvic disproportion, and is more likely to require augmentation with syntocinon.
If the cervix does not reach full dilatation despite syntocinon, a caesarean section will be required. If full dilatation is reached, it is quite possible for a baby to deliver in the OP position (with the head coming out ‘face to pubis’), but, not uncommonly, manual rotation, rotational ventouse or Kielland’s rotational forceps delivery will be required (p. 380). Third and fourth degree perineal tears are more likely to occur when a baby delivers in an OP position.