Lung ultrasound: Protocols in acute dyspnea
Instrumentation and technique
Use of a microconvex transducer with a 4- to 8-MHz frequency range is recommended. In general, the microconvex transducer is used for the evaluation of the lung and the pleural space, but a high-frequency probe also can be used for the specific diagnosis of a pneumothorax when using ultrasound for vascular access. The intubated patient is almost always examined in the semirecumbent or supine position (Figure 24-1).

Figure 24-1 Patient positioning. The intubated patient is almost always examined in supine position. Check all six anatomic regions: upper and lower sections of the anterior, lateral, and posterior chest wall.
1. Expose the thorax and place ultrasound gel on the six regions of the chest.
2. Start the examination with the transducer in the first intercostal space in the upper anterior region of the chest, with the ultrasound marker pointing toward the head of the patient.
3. Continue the examination by sliding the ultrasound probe in a longitudinal direction, from the head toward the toes of the patient.
4. Visualization is performed in each intercostal space, concentrating on the image between the two rib shadows, and should last for at least one complete respiratory cycle.
5. Repeat the process in the lateral and posterior chest walls in the same manner.
6. The following lung findings are evaluated:
7. In addition to lung findings, the following can be evaluated to supplement the examination:
In 2008, Daniel Lichtenstein evaluated the potential of lung ultrasound in diagnosing acute dyspnea.1 Ultrasonography was performed on patients with acute respiratory failure, comparing lung ultrasonography results on initial presentation with the final diagnosis by the ICU team. The study developed the BLUE Protocol (Bedside Lung Ultrasound in Emergency Protocol) as a diagnostic tool (Figure 24-2). The following patterns and profiles were established:
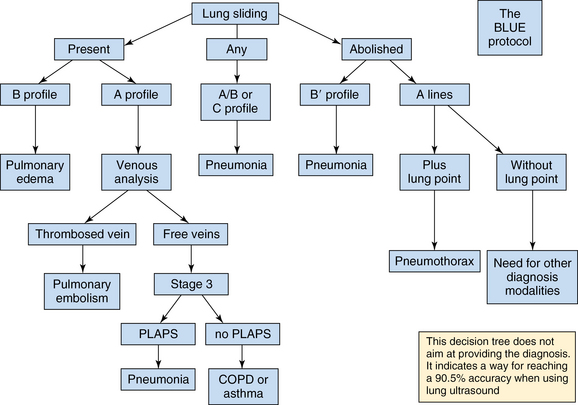
Figure 24-2 The BLUE Protocol: A decision tree using lung ultrasonography to guide diagnosis of severe dyspnea. (From Lichtenstein D, Mezière G: Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE Protocol. Chest 134(1):117-125, 2008.)
1. Predominance of A-lines in the presence of lung sliding indicated an exacerbation of asthma or chronic obstructive pulmonary disease (COPD) (89% sensitivity and 97% specificity).
2. Multiple, anterior diffuse B-lines in the presence of lung sliding indicated pulmonary edema (97% sensitivity and 95% specificity).
3. Normal anterior profile in the presence of a deep venous thrombosis indicated pulmonary embolism (81% sensitivity and 99% specificity).
4. Anterior absence of lung sliding in the presence of A-lines and lung point indicated pneumothorax (81% sensitivity and 100% specificity).
5. Anterior alveolar consolidations, anterior diffuse B-lines with abolished lung sliding, anterior asymmetric interstitial patterns, posterior consolidations, or effusions in the absence of anterior diffuse B- lines indicated pneumonia (89% sensitivity and 94% specificity).
The use of these profiles provided an accurate diagnosis in 90.5% of cases of acute respiratory failure.1 We recommend looking for the following signs and findings to organize a diagnostic approach while evaluating a patient with acute dyspnea:
1. Localize and observe the relationship between the lung surface, the pleural line, and the upper and lower rib. The lack of normal relationship may indicate subcutaneous emphysema.
2. Then look for the presence of lung sliding. Abolished lung sliding is indicative of pneumothorax if accompanied by the “lung point sign.”
3. In the presence of lung sliding, then look for the A-lines, which indicate presence of air. It can be physiologic or pathologic. For further analysis, it is recommended to perform an ultrasound venous examination. The interpretation of the findings can be as follows:
a. Presence of A-lines and a thrombosed vein suggest pulmonary embolism.
b. Presence of A-lines and the absence of deep vein thrombosis suggest pneumonia in the presence of a posterior lateral alveolar/pleural syndrome (PLAPS) or COPD/asthma in the absence of PLAPS.
4. Then check for the presence of B-lines. The presence of one B-line is enough for ruling out the diagnosis of pneumothorax where the transducer is applied. The presence of B-lines and other accompanying signs need further analysis for correct interpretation.
a. Diffuse, bilateral B-lines (at least in four points of the anterior chest wall) may indicate cardiogenic or noncardiogenic pulmonary edema. Performing echocardiography may be helpful in this case.
5. The last step is to look for the “sinusoid sign” to identify the presence of any kind of pleural effusion. This sign diagnoses pleural effusion, regardless of its echogenicity, and indicates the possibility of using a small needle for withdrawing fluid.
How to interpret the thoracic ultrasound findings in the workup for dyspnea
Acute dyspnea is a common challenging scenario that requires an appropriate diagnosis and early medical therapy. Management of critically ill patients very frequently requires imaging tools that are essential for optimizing diagnostic and therapeutic procedures.2 In this section, we will explore the statistical analysis that supports the thoracic ultrasound findings in the diagnosis and management of acute dyspnea.
Gavi et al3 studied the concordance of the pre-ultrasound physician diagnoses versus the ultrasonic diagnoses while approaching acute dyspnea. They found that the ultrasound diagnoses are more often in concordance with final diagnoses (66%) than the pre-ultrasound physician diagnoses (50%), and in about 30% of the cases, the ultrasound findings may correctly change the initial therapeutic management. During this study, the diagnostic ultrasound was performed in a very short period of time, ranging from 60 to 270 seconds.3 After recognizing ultrasound as a fast and useful diagnostic tool in the evaluation of acute dyspnea, the following are the most common abnormal findings in the thoracic ultrasonography.
Alveolar-interstitial syndrome: Using a standard ultrasound probe, it is possible to differentiate a thickened interlobular septum representing interstitial edema (seen as multiple B-lines at least 7 mm apart) from a ground-glass area representing an alveolar edema (observed as multiple B-lines 3 mm or less apart). In a European study, Gargani et al found that in patients with acute dyspnea, the presence of pulmonary congestion (sonographically seen as B-lines) is significantly correlated to N-terminal pro-brain natriuretic peptide (NT-proBNP) values (r = .69, P < .0001, sensitivity 97%, specificity 92.6%), and this finding is highly accurate in predicting the cardiac origin of dyspnea.4 In another study published by Stefanidis et al,5 lung ultrasound showed high sensitivity and specificity values (ranging from >80% for the lower lung fields up to >90% for the upper lung fields) in detection and localization of the alveolar-interstitial syndrome in the critically ill.
Pleural effusions: In a prospective study comparing the diagnostic accuracy of both bedside chest radiography and lung ultrasound versus thoracic computed tomography (CT), Lichtenstein et al6 showed that lung ultrasound had a diagnostic accuracy of 93% for pleural effusion, 97% for alveolar consolidation, and 95% for alveolar-interstitial syndrome versus 47%, 75%, and 72%, respectively, with bedside chest radiography. Interobserver agreement for the ultrasound findings was satisfactory: 0.74, 0.77, and 0.73 for detection of alveolar-interstitial syndrome, alveolar consolidation, and pleural effusion, respectively.
Pneumonia: Lung consolidations are described as the presence of B-lines with absent lung sliding. It appears as poorly defined hypoechoic lung tissue structure. Also, with ultrasound it is possible to visualize air bronchograms within consolidated lung. Lung ultrasound has been shown to provide the possibility of assessing quantitatively the lung re-aeration resulting from antimicrobial therapy in critically ill patients with ventilator-associated pneumonia.2 Although more studies are needed in this field, a tight correlation was found between pulmonary re-aeration measured by lung CT and the change in the “ultrasound score.”
Pneumothorax: There are two different signs that can suggest the presence of a pneumothorax. First, there is the lack of sliding lung resulting from a parietal–pleura air interface. This sign has a sensitivity of 92% when compared with the gold standard CT scan of the chest. Always look for loculated posterior, mediastinal, and apical pneumothoraces. Second, the presence of a lung point, described as the place where it is possible to observe an anterior movement of the pleura and a posterior displacement of the lung, is a specific sign of pneumothorax. This sign is seen when alternating lung sliding and abolished lung sliding are at the same location. In general, the sensitivity and specificity of lung ultrasound for diagnosing pneumothorax were 86% and 97%, respectively, whereas conventional chest radiography had sensitivity and specificity of 28% and 100%, respectively.7 In his study, Dulchavsky et al7 demonstrated that bedside lung ultrasound is more efficient than bedside chest radiography for diagnosing pneumothorax in emergency conditions.
Pearls and pitfalls
• Lung ultrasound is an operator-dependent imaging modality. Focused, supervised training is needed to ensure that the operator correctly interprets the ultrasonographic findings. Inadequate training may increase the risk of misinterpretation and complications.
• For obese patients and multiple trauma patients with subcutaneous emphysema, the visualization of lung parenchyma might be difficult.
• The use of established lung ultrasound profiles provides correct diagnoses in 90.5% of acute dyspnea cases.
• The ultrasonographic diagnosis of pneumothorax is considered one of the most difficult parts of training.8 When possible, the use of higher emission frequencies (up to 12 MHz) facilitates the recognition of lung sliding abolition. The diagnosis is even more difficult in the presence of partial pneumothorax. The patient should lie strictly supine to allow location of pleural gas effusion in nondependent lung regions.
• Although ultrasound is among the most useful tests for the evaluation of acute dyspnea, it should always be interpreted in the context of the clinical information and other tests.
References
1. Lichtenstein, D, Mezière, G, Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE Protocol. Chest. 2008;134(1):117–125.
2. Bouhemad, B, Zhang, M, Lu, Q, Rouby, JJ, Clinical review: bedside lung ultrasound in critical care practice. Crit Care. 2007;11(1):205.
3. Gavi, E, Eisen, LA, Mayo, P. Utility of an ultrasound driven algorithm in rapid response scenarios due to acute life threatening dyspnea. Chest. 2007; 132(4):567–657.
4. Gargani, L, Frassi, F, Oldati, F, et al, Ultrasound lung comets for the differential diagnosis of acute cardiogenic dyspnoea: a comparison with natriuretic peptides. Eur J Heart Fail. 2008;10(1):70–77.
5. Stefanidis, K, Dimopoulos, S, Kolofousi, C, et al. Sonographic lobe localization of alveolar-interstitial syndrome in the critically ill. Crit Care Res Pract. 2012; 2012:179719.
6. Lichtenstein, D, Goldstein, G, Mourgeon, E, et al. Comparative diagnostic performances of auscultation, chest radiography and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004; 100:9–15.
7. Dulchavsky, SA, Schwarz, KL, Kirkpatrick, AW, et al. Prospective evaluation of thoracic ultrasound in the detection of pneumothorax. J Trauma. 2001; 50:201–205.
8. Lichtenstein, D, Hulot, JS, Rabiller, A, et al. Feasibility and safety of ultrasound-aided thoracentesis in mechanically ventilated patients. Intensive Care Med. 1999; 25:955–958.







