Lung ultrasound in trauma
Overview
The great potential of ultrasound in the study of lung parenchyma lies in its ability to detect alterations in parenchymal density resulting from loss of alveolar air with or without increase of interstitial fluids.1 Moreover, pleural disorders can be studied by direct visualization or indirect detection of abnormal fluids or air collected in the pleural space. Ultrasound abilities are based not only on the capacity to visualize real images of disorders (e.g., direct visualization of pleural effusion or lung consolidations) but also on analyzing various artifacts. The latter are generated by the acoustic interface created between parietal pleura and lung parenchyma and enable the detection of pneumothorax and various interstitial disorders. In trauma patients, bedside lung ultrasound readily identifies life-threatening disorders, such as hemothorax and/or pneumothorax, thus facilitating prompt treatment.2,3 In trauma patients who present without any life-threatening conditions, lung ultrasound can detect lesions that appear radio-occult on radiography (e.g., lung blast), thus optimizing the selection of patients undergoing whole-body computed tomography (CT) scans.4
The technique
In a trauma scenario, the lung can be examined by any transducer, from high-frequency transducers well-suited for surface scanning to microconvex transducers that facilitate scanning between the tiny acoustic bone windows of the thoracic cage. Convex transducers represent the optimal mixture between a large spatial visualization and penetration depth achieved by low frequencies. Apart from lung scanning, microconvex transducers enable the examination of the abdomen, heart, veins, and so on, which is a time-saving feature in trauma cases.5
Trauma patients usually lie supine and cannot be moved; hence emergency lung ultrasound can access the chest through its anterior and lateral areas. Scanning these areas is sufficient in most cases, but sometimes it is necessary to sweep the transducer above the diaphragm or toward the posterior aspect of chest. Initially, scanning is performed on longitudinal planes because the latter allow identification of the pleural line between two adjacent ribs.6 By slightly rotating the transducer along intercostal spaces, oblique views are obtained that allow visualization of a larger portion of the pleura and of the underlying lung parenchyma.
The normal pattern
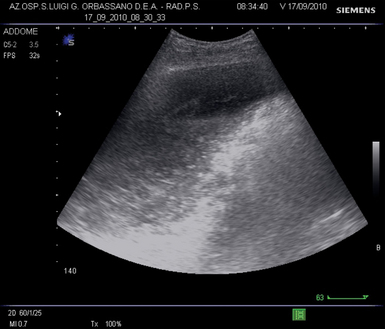
Scanning a normally aerated lung permits visualization of the entire chest wall from skin to parietal pleura. The alveolar air creates an interface with the pleura and the soft tissues of the chest wall because of differences in acoustic impedance (air is an acoustic barrier). Hence visualization of the lung parenchyma below the pleural line is not feasible. The image corresponding to the normal lung is made by artifacts that represent chest wall’s reflections below the pleural line (“mirror effect” of the lung) (Figure 21-1).1 A-lines are horizontal lines visualized at constant intervals in the zone of artifacts and represent multiple reflections of the pleural line.7
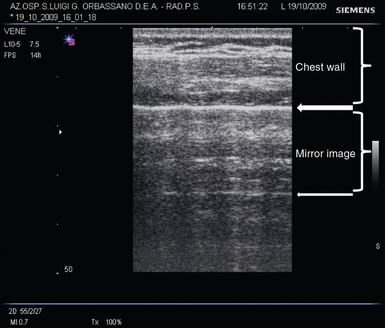
Figure 21-1 Oblique scan of a normally aerated lung. The image above the pleural line (thick arrow) is a real anatomic reconstruction of the chest wall. From the pleural line to the A-line (thin arrow), the image represents a reflection of the chest wall (mirror effect) that moves synchronously with respiration.
Pneumothorax
Air in the interpleural space cannot be visualized because it limits the penetration of the ultrasound beam. In case of pneumothorax, the static ultrasonographic lung image is similar to that of the normally aerated lung that adheres to the parietal pleura (Figure 21-2). The only difference is dynamic, because air between the two pleural layers does not allow visualization of any lung movement.
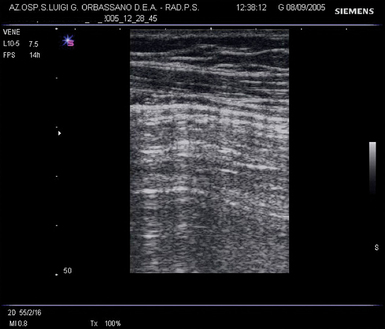
Figure 21-2 Oblique scan in pneumothorax. The still image of the lung is not distinguishable from the normal pattern (mirror effect) of Figure 21-1. Dynamic analysis allows appreciation of absence of any movement of the mirror image against the chest wall.
Ultrasonographic signs
Lung sliding: Although visualization of lung sliding rules out pneumothorax (high negative predictive value), its absence has no sufficient diagnostic accuracy to rule in pneumothorax.8 This is mainly because lung sliding can be equally observed in other disorders, such as atelectasis, acute respiratory distress syndrome (ARDS), or selective intubation. Hence, in case of absent sliding, operators should always check for other basic ultrasound signs.5,9
B lines: Changes in normal air/fluid balance in lung zones (loss of air) generates vertical laser-like artifacts (B-lines).10 B-lines blur, or even completely erase, the “mirror effect.”1 Depiction of multiple and diffuse B-lines indicates loss of the lung’s aeration and increase of interstitial fluids.11 However, presence of air in the pleural space prevents B-line visualization.10 Thus even one isolated B-line rules out the diagnosis of pneumothorax. Absence of B-lines is not only observed in pneumothorax. In case of absence of lung sliding and B lines, other signs also should be evaluated to definitively rule in pneumothorax.
Lung point: A partially collapsed lung resulting from pneumothorax usually exhibits a chest point where the lung adheres again to the parietal pleura. This is visualized in a single lung ultrasound scan as the fleeting appearance of a lung pattern (sliding and/or pulse and/or B-lines) replacing a pneumothorax pattern (the “mirror image” of a still lung without B-lines). This sign is known as the “lung point” and is 100% specific for the diagnosis of pneumothorax.12 Although highly specific, the lung point has low sensitivity because it cannot be visualized in totally collapsed lungs.
Lung pulse: In case of absence of lung sliding, B-lines, and lung point, operators should check for the lung pulse. This sign can only be visualized when the two pleural layers adhere.13 Even in case of a pattern highly suggestive of pneumothorax, for instance, absence of sliding and B-lines, visualization of the slightest lung pulse rules out the diagnosis of pneumothorax.
Technical issues and pitfalls
Air in the pleural space is usually mobile and tends to gather in the most dependent chest areas because of gravity. Searching for air in a supine trauma patient starts by scanning the anterior-inferior areas of the chest,9 keeping in mind that patient positioning may be highly variable in prehospital scenarios. Also, lung ultrasound techniques may be variable depending on the patient’s status (e.g., clinically stable or unstable, cardiac arrest). In acute emergency cases, the examination for lung sliding, B-lines, and lung pulse in the most dependent chest areas (bilaterally) is sufficient. In case of absence of these three signs, pneumothorax can be diagnosed, and the patient can be treated accordingly.9 In stable patients, detection of pneumothorax in the most dependent chest areas should be confirmed by checking the lateral chest areas for the lung point sign.6
Sometimes, air cannot move freely inside the pleural cavity because the two pleural layers may adhere or simply because the amount of air is too small to move against gravity inside a virtual cavity.14 The former condition may be observed in trauma patients, because lung contusions may cause pleural adherences.15 Hence small amounts of air may not be located in the most dependent chest areas, and scanning the entire chest surface may be necessary. A condition of loculated pneumothorax produces an image of two simultaneously moving lung points from the two sides of the same ultrasound scan (double lung point sign).9,14
Another possible source of error is subcutaneous emphysema, which is commonly found in trauma patients. Air in the subcutaneous tissue prevents visualization of the pleural line (Figure 21-3). When the pleural line is not visible, no safe diagnostic conclusions can be drawn. However, ultrasonographic and/or physical signs of subcutaneous emphysema in the setting of a chest trauma of an otherwise healthy patient are indicative of pneumothorax and/or rupture of the upper airways.9
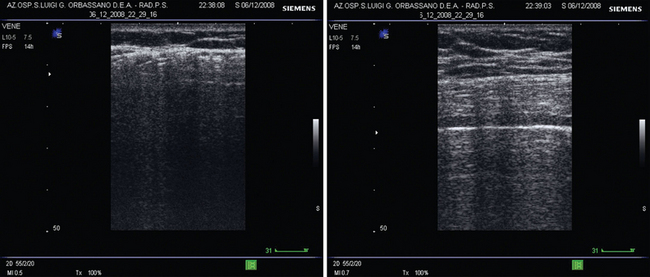
Figure 21-3 Bilateral lung scans in left-sided subcutaneous emphysema resulting from blunt thoracic trauma. The pattern of the left lung (left) does not show the pleural line. Comparison with the pattern of the contralateral lung (right) allows appreciation of a regular pleural line and highlights the difference.
Lung contusion
Lung parenchymal contusion (lung blast) is commonly observed after blunt chest trauma.2,4 Unlike pneumothorax, this condition rarely requires urgent intervention. However, diagnosis of contusion is important because it influences prognosis, while enabling correct diagnostic approaches to respiratory dysfunction. Radiology dramatically underestimates lung contusion in the emergency setting because its classic signs may take several hours to appear. Lung ultrasound detects even the earliest signs of lung blasts.4 Contused lung parenchyma is initially characterized by the presence of a hemorrhagic area resulting from trauma. Over time, progression toward interstitial edema with infiltrates and air loss is common, thus producing regions of increased density within the lung parenchyma. Lung ultrasound detects alterations in regional lung parenchymal density; however, differentiating abnormalities that produce similar sonoanatomic images is not always feasible. Ultrasonographic findings of lung areas in the setting of a blunt chest trauma, with increased density and disappearance of the “mirror effect” resulting from B-lines and consolidations, are highly suggestive of lung contusions. The first step of aeration loss is the interstitial pattern, which is depicted as multiple B-lines, often with some irregularity of the pleural line, whereas increased density and echogenicity may reflect the severity of the condition. The consolidation pattern represents the final step in the loss of aeration. Its ultrasonographic patterns are variable, ranging from the anechoic blurred “fluid alveologram” to the “tissue-like” image with (or without) hyperechoic punctiform or linear elements corresponding to air bronchograms (Figure 21-4). The above patterns represent lung areas with different densities, and they may coexist in the same patient and/or in the same scan (Figure 21-5).

Figure 21-4 Lung scan showing tissue-like evolution of contusion (C) resulting from blunt chest trauma. Echotexture of the consolidation is similar to the liver (L) and shows some air-bronchograms (thin arrow). Between the liver and the consolidated lung, the echoic line represents the diaphragm (D).
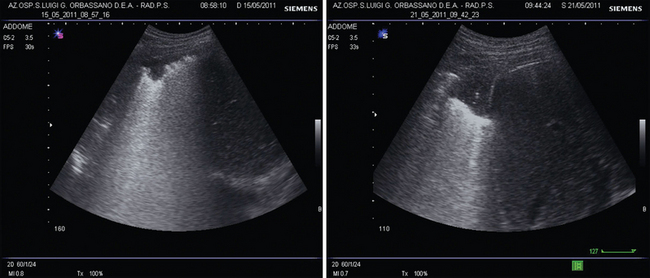
Figure 21-5 A case of blunt chest trauma. Left, Examination upon arrival in the emergency department revealed a basal right lung contusion. The pattern shows an alternation of B-lines with a subpleural anechoic consolidation. Right, The same lung area scanned after 6 days shows evolution of the lung blast to a tissue-like pattern with lentil-sized air bronchograms.
Hemothorax
The use of ultrasonography in the diagnosis of effusion has been routinely applied for many decades and is based on reproduction of a real image of the disorder.16,17 Unlike air, fluids within the pleural space create acoustic windows that permit ultrasound beam penetration. Pleural effusion is a dependent collection usually visualized as an anechoic space between the two pleura layers, with a cyclic variation of the interpleural distance during respiration.2 The ideal technique consists of scanning the most dependent chest areas, which are the lateral-basal lung areas, bilaterally, in a supine patient. The main sonoanatomic landmark is the image of the diaphragm and the abdominal solid organs, liver or spleen, immediately below it. When effusion is absent, the ultrasonographic image of a lung pattern will intermittently overlap and hide, moving like a curtain, the image of the diaphragm and the underlying abdominal organ. Alternatively, a fixed image of a consolidated lung with a tissue-like pattern may be visualized over the diaphragm. In trauma patients, depiction of an anechoic space between the two pleural layers is highly indicative of hemorrhagic effusion.18 Ultrasound may also diagnose the nature of the effusion. In general, while the anechoic pattern cannot be differentiated, visualization of internal echoes (e.g., mobile particles) is highly suggestive of hemothorax (Figure 21-6).16
Pearls and highlights
• Bedside lung ultrasound is superior to conventional radiography in diagnosing common sequelae of blunt chest trauma, such as hemothorax, pneumothorax, and lung blasts.
• Pneumothorax is diagnosed by the combined evaluation of four ultrasonographic signs: lung sliding, B-lines, lung point, and lung pulse. Lung sliding, B-lines, and lung pulse have high negative predictive value, whereas lung point is used to confirm the diagnosis.
• In unstable patients (e.g., cardiac arrest), a “fast-track” technique is applied to diagnose pneumothorax, consisting of checking for B-lines, lung sliding, and lung pulse in the most dependent chest areas (anterior-inferior chest in the supine patient, bilaterally). Absence of these three signs indicates need for immediate drainage. In stable patients, the technique should be extended to the lateral chest by searching for the lung point.
• Subcutaneous emphysema and loculated pneumothorax are possible source of pitfalls when lung ultrasound is used to diagnose pneumothorax.
• Hemorrhagic lung areas, alterations in regional lung parenchymal density, and changes in aeration are common features of lung blasts monitored by ultrasound. Evolution toward interstitial and/or consolidation ultrasonographic patterns is usually observed.
• Hemorrhagic effusion is a dependent collection of blood in the pleural space that can be ultrasonographically detected as an anechoic space between the two pleural layers, with occasional internal echoes, in the most dependent chest areas above the diaphragm.
References
1. Volpicelli, G. Lung sonography. J Ultrasound Med. 2013; 32:165–171.
2. Hyacinthe, AC, Broux, C, Francony, G, et al. Diagnostic accuracy of ultrasonography in the acute assessment of common thoracic lesions after trauma. Chest. 2012; 141:1177–1183.
3. Kirkpatrick, AW, Sirois, M, Laupland, KB, et al, Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Traum. 2004; 57:288–295.
4. Soldati, G, Testa, A, Silva, FR, et al. Chest ultrasonography in lung contusion. Chest. 2006; 130:533–538.
5. Volpicelli, G, Elbarbary, M, Blaivas, M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012; 38:577–591.
6. Lichtenstein, DA. Ultrasound in the management of thoracic disease. Crit Care Med. 2007; 35:S250–S261.
7. Lichtenstein, DA, Mezière, G, Lascols, N, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005; 33:1231–1238.
8. Lichtenstein, DA, Menu, Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest. 1995; 108:1345–1348.
9. Volpicelli, G. Sonographic diagnosis of pneumothorax. Intensive Care Med. 2011; 37:224–232.
10. Lichtenstein, D, Mezière, G, Biderman, P, et al, The comet-tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Me. 1999; 25:383–388.
11. Agricola, E, Bove, T, Oppizzi, M, et al, “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Ches. 2005; 127:1690–1695.
12. Lichtenstein, D, Mezière, G, Biderman, P, et al, The “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Me. 2000; 26:1434–1440.
13. Lichtenstein, DA, Lascols, N, Prin, S. The “lung pulse”: an early ultrasound sign of complete atelectasis. Intensive Care Med. 2003; 29:2187–2192.
14. Volpicelli, G, Audino, B, The double lung point: an unusual sonographic sign of juvenile spontaneous pneumothorax. Am J Emerg Med. 2011;29(355):e1–e2.
15. Soldati, G, Sher, S, Copetti, R. If you see the contusion, there is no pneumothorax. Am J Emerg Med. 2010; 28:106–107. [author reply 7-8].
16. Yang, PC, Luh, KT, Chang, DB, et al, Value of sonography in determining the nature of pleural effusion: analysis of 320 cases. AJR Am J Roentgeno. 1992; 159:29–33.
17. Yu, CJ, Yang, PC, Chang, DB, et al, Diagnostic and therapeutic use of chest sonography: value in critically ill patients. AJR Am J Roentgeno. 1992; 159:695–701.
18. Ma, OJ, Mateer, JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Ann Emerg Med. 1997; 29:312–315.