Lumbar Spine
Back pain is one of the great human afflictions. Almost anyone born today in Europe or North America has a great chance of suffering a disabling back injury regardless of occupation.1 The lumbar spine supports the upper body and transmits the weight of the upper body to the pelvis and lower limbs. Because of the strategic location of the lumbar spine, this structure should be included in any examination of the spine as a whole (i.e., posture) or in any examination of the hip or sacroiliac joints. Unless there is a definite history of trauma, determining whether an injury originates in the lumbar spine, sacroiliac joints, or hip joints is often difficult; therefore, all three should be examined in a sequential fashion.
Applied Anatomy
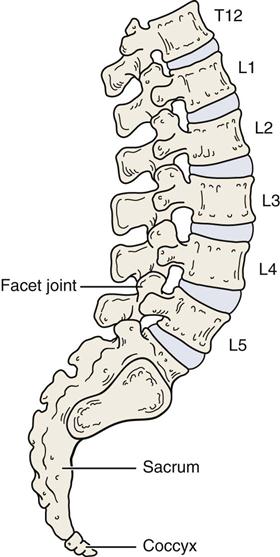
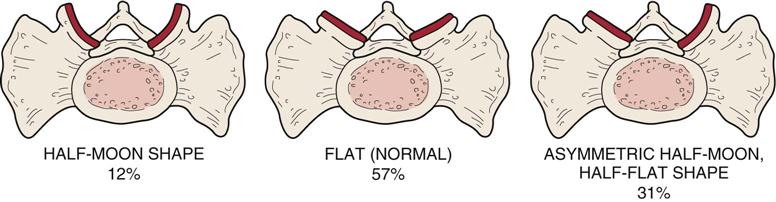
There are ten (five pairs) facet joints (also called apophyseal or zygoapophyseal joints) in the lumbar spine (Figure 9-1).2 These diarthrodial joints consist of superior and inferior facets and a capsule. The facets are located on the vertebral arches. With a normal intact disc, the facet joints carry about 20% to 25% of the axial load, but this may reach 70% with degeneration of the disc. The facet joints also provide 40% of the torsional and shear strength.3 Injury, degeneration, or trauma to the motion segment (the facet joints and disc) may lead to spondylosis4 (degeneration of the intervertebral disc), spondylolysis5 (a defect in the pars interarticularis or the arch of the vertebra), spondylolisthesis5 (a forward displacement of one vertebra over another), or retrolisthesis (backward displacement of one vertebra on another). The superior facets, or articular processes, face medially and backward and, in general, are concave; the inferior facets face laterally and forward and are convex (Figure 9-2). There are, however, abnormalities, or tropisms, that can occur in the shape of the facets, especially at the L5–S1 level (Figures 9-3 and 9-4).6 In the lumbar spine, the transverse processes are virtually at the same level as the spinous processes.
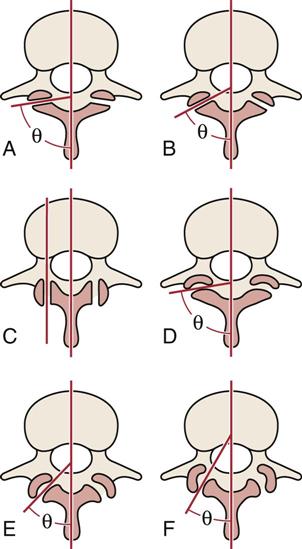
A, Flat joints oriented close to 90° to the sagittal plane. B, Flat joints orientated at 60° to the sagittal plane. C, Flat joints orientated parallel (0°) to the sagittal plane. D, Slightly curved joints with an average orientation close to 90° to the sagittal plane. E, “C”-shaped joints orientated at 45° to the sagittal plane. F, “J”-shaped joints orientated at 30° to the sagittal plane. (Redrawn from Bogduk N, Twomey LT: Clinical anatomy of the lumbar spine, New York, 1987, Churchill Livingstone, p. 26.)
These posterior facet joints direct the movement that occurs in the lumbar spine. Because of the shape of the facets, rotation in the lumbar spine is minimal and is accomplished only by a shearing force. Side flexion, extension, and flexion can occur in the lumbar spine, but the facet joints control the direction of movement. The close packed position of the facet joints in the lumbar spine is extension. Normally, the facet joints carry only a small amount of weight; however, with increased extension, they begin to have a greater weight-bearing function. The resting position is midway between flexion and extension. The capsular pattern is side flexion and rotation equally limited, followed by extension. However, if only one facet joint in the lumbar spine has a capsular restriction, the amount of observable restriction is minimal. The first sacral segment is usually included in discussions of the lumbar spine, and it is at this joint that the fixed segment of the sacrum joins with the mobile segments of the lumbar spine. In some cases, the S1 segment may be mobile. This occurrence is called lumbarization of S1, and it results in a sixth “lumbar” vertebra. At other times, the fifth lumbar segment may be fused to the sacrum or ilium, resulting in a sacralization of that vertebra. Sacralization results in four mobile lumbar vertebrae. These abnormalities are sometimes called transitional vertebra.7
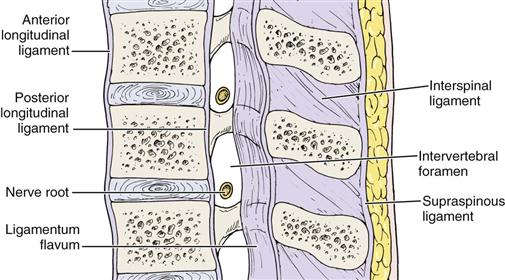
The main ligaments of the lumbar spine are the same as those in the lower cervical and thoracic spine (excluding the ribs). These ligaments include the anterior and posterior longitudinal ligaments, the ligamentum flavum, the supraspinous and interspinous ligaments, and the intertransverse ligaments (Figure 9-5). In addition, there is an important ligament unique to the lumbar spine and pelvis—the iliolumbar ligament (Figure 9-6), which connects the transverse process of L5 to the posterior ilium.8 This ligament helps stabilize L5 with the ilium and helps prevent anterior displacement of L5.9
The intervertebral discs make up approximately 20% to 25% of the total length of the vertebral column. The function of the intervertebral disc is to act as a shock absorber distributing and absorbing some of the load applied to the spine, to hold the vertebrae together and allow movement between the bones, to separate the vertebra as part of a functional segmental unit acting in concert with the facet joints (Figure 9-7), and, by separating the vertebrae, to allow the free passage of the nerve roots out from the spinal cord through the intervertebral foramina. With age, the percentage of spinal length attributable to the discs decreases as a result of disc degeneration and loss of hydrophilic action in the disc.
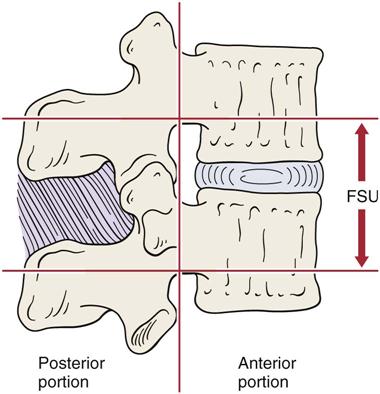
Such a complex may also be seen in the cervical and thoracic spines.
The annulus fibrosus, the outer laminated portion of the disc, consists of three zones: 1) an outer zone made up of fibrocartilage (classified as Sharpey fibers) that attaches to the outer or peripheral aspect of the vertebral body and contains increasing numbers of cartilage cells in the fibrous strands with increasing depth, 2) an intermediate zone made up of another layer of fibrocartilage, and 3) an inner zone primarily made up of fibrocartilage and containing the largest number of cartilage cells.10 The annulus fibrosus contains twenty concentric, collar-like rings of collagenous fibers that crisscross each other to increase their strength and accommodate torsion movements.11
The nucleus pulposus is well developed in both the cervical and the lumbar spines. At birth, it is made up of a hydrophilic mucoid tissue, which is gradually replaced by fibrocartilage. With increasing age, the nucleus pulposus increasingly resembles the annulus fibrosus. The water-binding capacity of the disc decreases with age, and degenerative changes (spondylosis) begin to occur after the second decade of life. Initially, the disc contains approximately 85% to 90% water, but the amount decreases to 65% with age.12 In addition, the disc contains a high proportion of mucopolysaccharides, which cause the disc to act as an incompressible fluid. However, these mucopolysaccharides decrease with age and are replaced with collagen. The nucleus pulposus lies slightly posterior to the center of rotation of the disc in the lumbar spine.
The shape of the disc corresponds to that of the body to which it is attached. The disc adheres to the vertebral body by means of the cartilaginous end plate. The end plates consist of thin layers of cartilage covering the majority of the inferior and superior surfaces of the vertebral body. The cartilaginous end plates are approximately 1 mm thick and allow fluid to move between the disc and the vertebral body. The discs are primarily avascular with only the periphery receiving a blood supply. The remainder of the disc receives nutrition by diffusion, primarily through the cartilaginous end plate. Until the age of 8 years, the intervertebral discs have some vascularity; however, with age this vascularity decreases.
Usually, the intervertebral disc has no nerve supply, although the peripheral posterior aspect of the annulus fibrosus may be innervated by a few nerve fibers from the sinuvertebral nerve.13,14 The lateral aspects of the disc are innervated peripherally by the branches of the anterior rami and gray rami communicants. The pain-sensitive structures around the intervertebral disc are the anterior longitudinal ligament, posterior longitudinal ligament, vertebral body, nerve root, and cartilage of the facet joint.
With the movement of fluid vertically through the cartilaginous end plate, the pressure on the disc decreases as the patient assumes the natural lordotic posture in the lumbar spine. Direct vertical pressure on the disc can cause the disc to push fluid into the vertebral body. If the pressure is great enough, defects may occur in the cartilaginous end plate, resulting in Schmorl nodules, which are herniations of the nucleus pulposus into the vertebral body. These are found in 20% to 30% of individuals.15 Normally, an adult is 1 to 2 cm (0.4 to 0.8 inch) taller in the morning than in the evening (20% diurnal variation).3,16 This change results from fluid movement in and out of the disc during the day through the cartilaginous end plate. This fluid shift acts as a pressure safety valve to protect the disc.
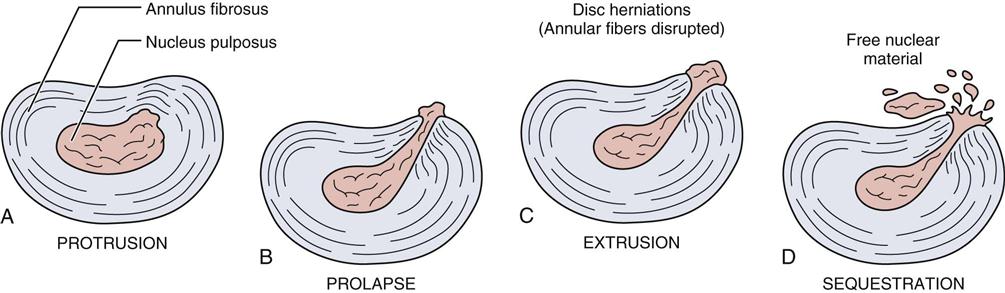
If there is an injury to the disc, four problems can result, all of which can cause symptoms.17 There may be a protrusion of the disc, in which the disc bulges posteriorly without rupture of the annulus fibrosus. In the case of a disc prolapse, only the outermost fibers of the annulus fibrosus contain the nucleus. With a disc extrusion, the annulus fibrosus is perforated, and discal material (part of the nucleus pulposus) moves into the epidural space. The fourth problem is a sequestrated disc, or a formation of discal fragments from the annulus fibrosus and nucleus pulposus outside the disc proper (Figure 9-8).18 These injuries can result in pressure on the spinal cord itself (upper lumbar spine) leading to a myelopathy, pressure on the cauda equina leading to cauda equina syndrome (saddle anesthesia [Figure 9-9], bowel/bladder dysfunction),19 or pressure on the nerve roots (most common). The amount of pressure on the neurological tissues determines the severity of the neurological deficit.20 The pressure may be the result of the disc injury itself or in combination with the inflammatory response of the injury. Saal has outlined favorable, unfavorable, and neutral factors for positive-outcome prognostic factors for nonoperative lumbar disc herniation (Table 9-1).17
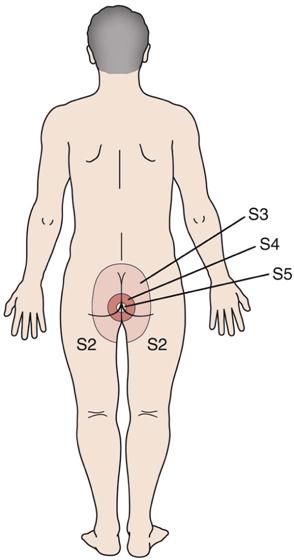
The S3, S4, and S5 nerves provide sensory innervation to the inner thigh, perineum, and rectum.
TABLE 9-1
Prognostic Factors for Positive Outcome with Nonoperative Care for Lumbar Disc Herniation
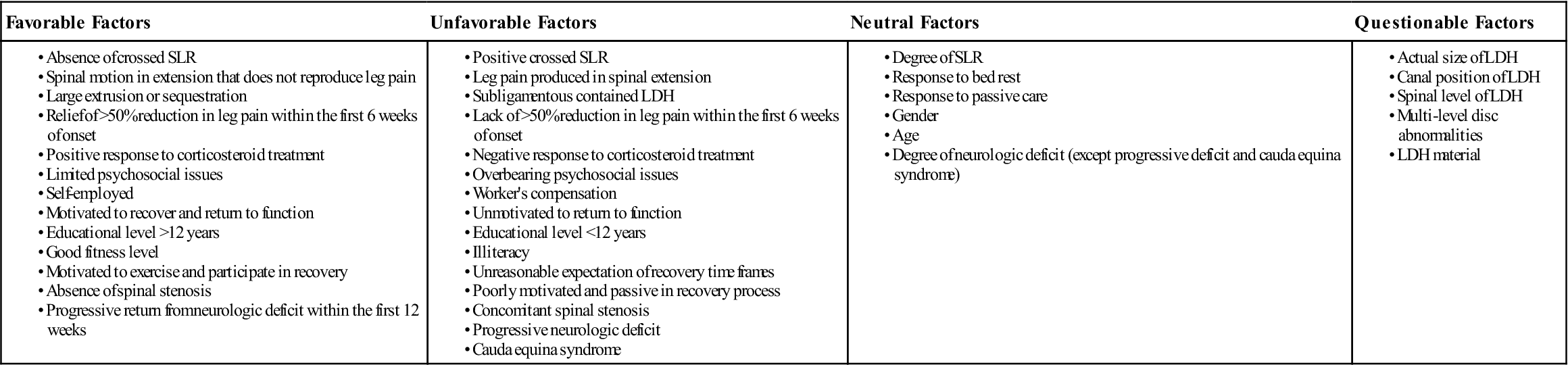
LDH, Lumbar disc herniation; SLR, straight leg raise.
Modified from Saal JA: Natural history and nonoperative treatment of lumbar disc herniation. Spine 21(24S):7S, 1996.
Within the lumbar spine, different postures can increase the pressure on the intervertebral disc (Figure 9-10). This information is based on the work of Nachemson and colleagues,21,22 who performed studies of intradiscal pressure changes in the L3 disc with changes in posture. The pressure in the standing position is classified as the norm, and the values given are increases or decreases above or below this norm that occur with the change in posture.
In the lumbar spine, the nerve roots exit through relatively large intervertebral foramina, and as in the thoracic spine, each one is named for the vertebra above it (in the cervical spine, the nerve roots are named for the vertebra below). For example, the L4 nerve root exits between the L4 and L5 vertebrae. Because of the course of the nerve root as it exits, the L4 disc (between L4 and L5) only rarely compresses the L4 nerve root; it is more likely to compress the L5 nerve root (Figure 9-11).
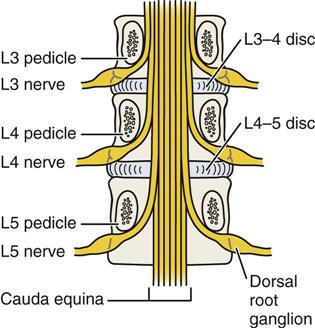
Note that the exiting root takes the name of the vertebral body under which it travels into the neural foramen. Because of the way the nerve roots exit, L4–L5 disc pathology usually affects the L5 root rather than the L4 root. (Redrawn from Borenstein DG, Wiesel SW, Boden SD: Low back pain: medical diagnosis and comprehensive management, Philadelphia, 1995, WB Saunders, p. 5.)
In general, the L5–S1 segment is the most common site of problems in the vertebral column because this level bears more weight than any other vertebral level. The center of gravity passes directly through this vertebra, which is of benefit because it may decrease the shearing stresses to this segment. There is a transition from the mobile segment, L5, to the stable or fixed segment of the sacrum (S1), which can increase the stress on this area. Because the angle between L5 and S1 is greater than those between the other vertebrae, this joint has a greater chance of having stress applied to it. Another factor that increases the amount of stress on this area is the relatively greater amount of movement that occurs at this level compared with other levels of the lumbar spine.
Patient History
Problems of the lumbar spine are difficult to diagnose; in fact, diagnosing pain due to a disc is primarily diagnosis of exclusion.23 Most of the examination commonly revolves around differentiating symptoms of a herniated disc (or space occupying lesion), which refers radicular symptoms into the leg from other conditions (e.g., inflammatory reaction, sprains, strains, facet syndrome) more likely to cause localized pain.24 If there are no radicular symptoms below the knee, it often becomes difficult for the examiner to determine where in the spine the problem is, or for that matter, whether the problem is truly in the lumbar spine or coming from problems in the pelvic joints, primarily the sacroiliac joints, or the hips. Waddell pointed out that in only about 15% of cases can a definitive diagnosis as to the pathology of back pain be made.3 Hall broke low back pain into four categories—two of which are back pain dominant and two of which are leg pain dominant (Table 9-2).25 Pattern 1 suggests disc involvement, whereas pattern 2 suggests facet joint involvement. Pattern 3 suggests nerve root involvement (primarily by a disc or some other space occupying lesion or an injury accompanied by inflammatory swelling), and pattern 4 suggests neurogenic intermittent claudication (pressure on the cauda equina). Thus, only by taking a careful history, followed by a detailed examination, is the examiner able to determine the cause of the problem.26–28 Even then, some doubt may remain.
TABLE 9-2
| Pattern | Where Pain Is Worst | Aggravating Movement |
Relieving Movement |
Onset | Duration | Probable Cause | |
| Back Dominant Pain/Mechanical Cause | 1 | Back/buttocks (>90% back pain) Myotomes seldom affected Dermatomes not affected |
Flexion Stiff in morning |
Extension | Hours to days | Days to months (sudden or slow) | Disc involvement (minor herniation, spondylosis), sprain, strain |
| 2 | Back/buttocks Myotomes seldom affected Dermatomes not affected |
Extension/Rotation | Flexion | Minutes to hours | Days to weeks (sudden) | Facet joint involvement, strain | |
| Leg Pain Dominant/Nonmechanical Cause | 3 | Leg (usually below knee) Myotomes commonly affected (especially in chronic cases) Pain in dermatomes |
Flexion | Extension | Hours to Days | Weeks to months | Nerve root irritation (most likely cause—disc hernation) |
| 4 | Leg (usually below knee) (May be bilateral) Myotomes commonly affected (especially in chronic cases) Pain in dermatomes |
Walking (extension) | Rest (sitting) and/or postural change | With walking | ? | Neurogenic intermittent claudication (stenosis) |
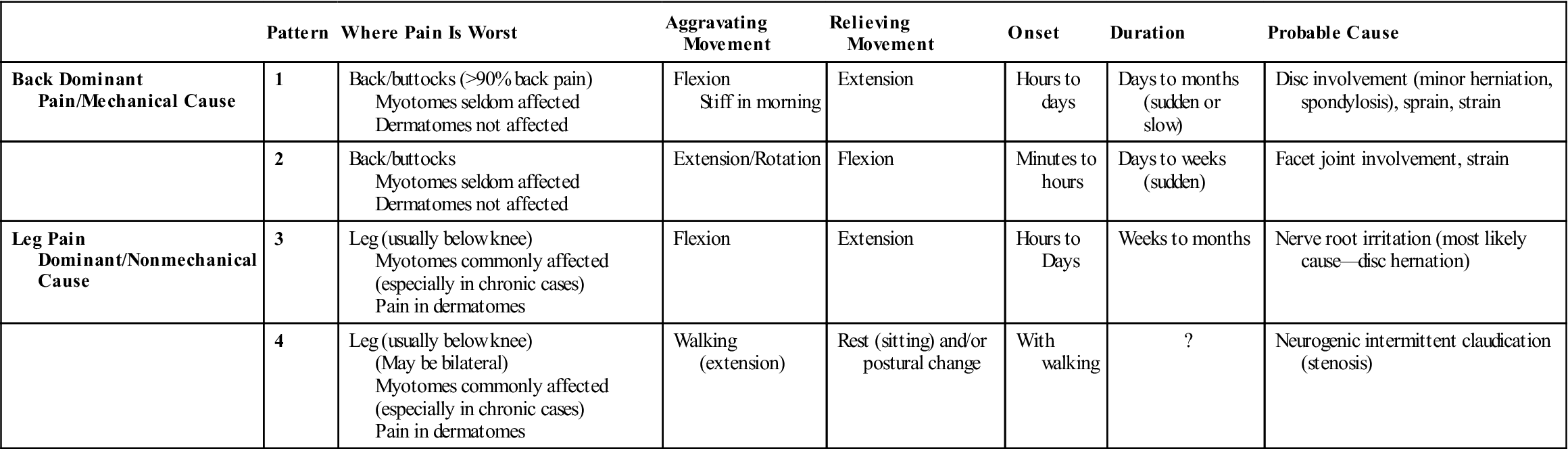
Modified from Hall H: A simple approach to back pain management. Patient Care 15:77–91, 1992.
In addition to the questions listed under the “Patient History” section in Chapter 1, the examiner should obtain the following information from the patient:
1. What is the patient’s age?29 Different conditions affect patients at different ages. For example, disc problems usually occur between the ages of 15 and 40 years, and ankylosing spondylitis is evident between 18 and 45 years. Osteoarthritis and spondylosis are more evident in people older than 45 years of age, and malignancy of the spine is most common in people older than 50 years of age.
2. What is the patient’s occupation?3,30 Back pain tends to be more prevalent in people with strenuous occupations,31 although it has been reported that familial influences have an effect as well as occupation.32,33 For example, truck drivers (vibration) and warehouse workers have a high incidence of back injury.34 Patients who have chronic low back pain develop a deconditioning syndrome, which compounds the problem as it leads to decreased muscle strength, impaired motor control, and decreased coordination and postural control.35 How active is the patient at work (usual job, light duties, full time, frequent days off because of back pain, unemployed because of back, retired)?
4. What was the mechanism of injury? Was major trauma (e.g., car accident) involved? Lifting commonly causes low back pain (Tables 9-3 and 9-4). This is not surprising when one considers the forces exerted on the lumbar spine and disc. For example, a 77-kg (170-lb) man lifting a 91-kg (200-lb) weight approximately 36 cm (14 inches) from the intervertebral disc exerts a force of 940 kg (2072 lbs) on that disc. The force exerted on the disc can be calculated as roughly ten times the weight being lifted. Pressure on the intervertebral discs varies depending on the position of the spine. Nachemson and colleagues showed that pressure on the disc can be decreased by increasing the supported inclination of the back rest (e.g., an angle of 130° decreases the pressure on the disc by 50%).21,22 Using the arms for support can also decrease the pressure on the disc. When one is standing, the disc pressure is approximately 35% of the pressure that occurs in the relaxed sitting position. The examiner should also keep in mind that stress on the lower back tends to be 15% to 20% higher in men than in women because men are taller and their weight is distributed higher in the body.
5. How long has the problem bothered the patient? Acute back pain lasts 3 to 4 weeks. Subacute back pain lasts up to 12 weeks. Chronic pain is anything longer than 3 months. Waddell has outlined predictors (yellow flags) of chronicity with back pain patients.3,36
6. Where are the sites and boundaries of pain? Have the patient point to the location or locations. Note whether the patient indicates a specific joint or whether the pain is more general. The more specific the pain, the easier it is to localize the area of pathology. Unilateral pain with no referral below the knee may be caused by injury to muscles (strain) or ligaments (sprain), the facet joint, or, in some cases, the sacroiliac joints. This is called mechanical low back pain (in older books it is called “lumbago”). With each of these injuries, there is seldom if ever peripheralization of the symptoms. The symptoms tend to stay centralized in the back. If the muscles and ligaments are affected, movement will decrease and pain will increase with repeated movements. If the pain extends to the hip, the hip must be cleared by examination. With facet joint problems, the range of motion (ROM) remains the same (it may be restricted from the beginning), as does the pain with repeated movements. Pain on standing that improves with walking and pain on forward flexion with no substantial muscle tenderness suggests disc involvement.37 The sacroiliac joints will show pain when pain-provoking (stress) tests are used. A minor disc injury (protrusion) may show the same symptoms, but the pain is more likely to be bilateral if it is a central protrusion.38
7. Is there any radiation of pain? Is the pain centralizing or peripheralizing (Figure 9-12)?39,40 Centralization implies the pain is moving toward or is centered in the lumbar spine.41–43 Peripheralization implies the pain is being referred or is moving into the limb. If so, it is helpful for the examiner to remember and correlate this information with dermatome findings when evaluating sensation. The examiner must be careful when looking at the lumbar spine that he or she does not consider every back problem a disc problem. It has been reported that disc problems account for only about 5% of low back pain cases.44 Some authors feel the only definitive clinical diagnosis of a disc problem is neurological pain extending below the knee.25 This means that although there may be pain in the back and in the leg, the leg pain is dominant.3 Pain on the anterolateral aspect of the leg is highly suggestive of L4 disc problems, whereas pain radiating to the posterior aspect of the foot suggests L5 disc problems if the history indicates a disc may be injured.45 Pain radiating into the leg below the knee is highly suggestive of a disc lesion, but isolated back or buttock pain does not rule out the disc. Minor injuries, such as protrusion of the disc, may result only in back or buttock pain.45 Such an injury makes diagnoses more difficult because such pain may also result from muscle or ligament injury or from injury or degeneration to the adjacent facet joints.
Lumbar and sacroiliac pain tend to be referred to the buttock and posterior leg (and sometimes to the lateral aspect of the leg). Hip pain tends to be in the groin and anterior thigh although it may be referred to the knee (usually medial side). The hip can be ruled out later in the examination by the absence of a hip capsular pattern and a negative sign of the buttock.46 The examiner must also determine whether the musculoskeletal system is involved or whether the pain is being referred from another structure or system (e.g., abdominal organs). Abnormal signs and symptoms or red flags (see Table 1-1) would lead the examiner to consider causes other than the musculoskeletal system.
11. Are there any postures or actions that specifically increase or decrease the pain or cause difficulty?39,47 For example, if sitting increases the pain and other symptoms, the examiner may suspect that sustained flexion is causing mechanical deformation of the spine or increasing the intradiscal pressure.48 Classically, disc pathology causes increased pain on sitting, lifting, twisting, and bending.49 It is the most common space-occupying lesion in the lumbar spine and, therefore, is the most common cause of radiating pain below the knee. If standing increases the pain and other symptoms, the examiner may suspect that extension, especially relaxed standing, is the cause. If walking increases the pain and other symptoms, extension is probably causing the mechanical deformation, because walking accentuates extension. If lying (especially prone lying) increases the pain and other symptoms, extension may be the cause. Persistent pain or progressive increases in pain while the patient is in the supine position may lead the examiner to suspect neurogenic or space-occupying lesions, such as an infection, swelling, or tumor. Remember that pain may radiate to the lumbar spine from pathological conditions in other areas as well as from direct mechanical problems. For example, tumors of the pancreas refer pain to the low back. Stiffness or pain after rest may indicate ankylosing spondylitis or Scheuermann disease. Pain from mechanical breakdown tends to increase with activity and decrease with rest. Discogenic pain increases if the patient maintains a single posture (especially flexion) for a long period. Pain arising from the spine almost always is influenced by posture and movement.
The pelvis is the key to proper back posture. Ideally, an individual should be able to stand with the pelvis in neutral. In this position, the anterior superior iliac spines (ASISs) are one to two finger widths lower than the posterior superior iliac spines (PSISs). For the pelvis to “sit” properly on the femora, the abdominal, hip flexor, hip extensor, and back extensor muscles must be strong, supple, and “balanced” (Figure 9-13). Any deviation in the normal alignment should be noted and recorded. For example, shoe heel height can modify the pelvic angle and lumbar curve, altering the stress on the spine.50
13. Which movements hurt? Which movements are stiff? Table 9-5 demonstrates some of the causes of mechanical low back pain and their symptoms. The examiner must help the patient differentiate between true pain and discomfort that is caused by stretching. Postural, or static, muscles (e.g., iliopsoas) tend to respond to pathology with tightness in the form of spasm or adaptive shortening; dynamic, or phasic, muscles (e.g., abdominals) tend to respond with atrophy. Pathology affecting both types of muscles can lead to a pelvic crossed syndrome (discussed later). Does the patient describe a painful arc of movement on forward or side flexion? If so, it may indicate a disc protrusion with a nerve root riding over the bulge or instability in part of the ROM.47 Patients with lumbar instability or lumbar muscle spasm have trouble moving to the seated position, whereas patients with discogenic pain usually have pain in flexion (e.g., sitting) and the pain may increase the longer they are seated.
14. Is paresthesia (a “pins and needles” feeling) or anesthesia present? A patient may experience a sensation or a lack of sensation if there is pressure on a nerve root. Paresthesia occurs if pressure is relieved from a nerve trunk, whereas if the pressure is on the nerve trunk, the patient experiences a numb sensation. Does the patient experience any paresthesia or tingling and numbness in the extremities, perineal (saddle) area, or pelvic area? Abnormal sensations in the perineal area often have associated micturition (urination) problems. These symptoms may indicate a myelopathy and are considered by many to be an emergency surgical situation because of potential long-term bowel and bladder problems if the pressure on the spinal cord is not relieved as soon as possible.51,52 The examiner must remember that the adult spinal cord ends at the bottom of the L1 vertebra and becomes the cauda equina within the spinal column. The nerve roots extend in such a way that it is rare for the disc to pinch on the nerve root of the same level. For example, the L5 nerve root is more likely to be compressed by the L4 intervertebral disc than by the L5 intervertebral disc (Figure 9-14). Seldom is the nerve root compressed by the disc at the same level, except when the protrusion is more lateral.
15. Has the patient noticed any weakness or decrease in strength? Has the patient noticed that his/her legs have become weak while walking or climbing stairs? This may be the result of an injury to the muscles themselves, their nerve supply, or reflex inhibition caused by pain.28,53
17. Which activities aggravate the pain? Is there anything in the patient’s lifestyle that increases the pain? Many common positions assumed by patients are similar to those in some of the provocative special tests. For example, getting into and sitting in a car is similar to the slump test and straight leg raise test. Long sitting in bed is a form of straight leg raise. Reaching up into a cupboard can be similar to an upper limb tension test. A word of caution: There can be a 10° to 20° difference in straight leg raise in lying and sitting because of the change in lordosis and position of the pelvis.3
23. Is the patient able to cope during daily activities? Psychosocial issues often play a role in low back pain, especially if it is chronic.54–57 It is normal for people suffering prolonged pain to exhibit altered psychosocial behaviors that are subject to wide individual differences and the effects of learning.58 Fear avoidance questionnaires, especially Waddell, et al.,59 Fear-Avoidance Beliefs Questionnaire (FABQ) (Figure 9-15) and Linton and Hallden’s Acute Low Back Pain Screening Questionnaire60 (Figure 9-16), are becoming more commonly used in lumbar examination.61–67 The New Zealand Acute Low Back Pain Guide outlines yellow flags indicating psychosocial barriers for recovery with questions related to attitudes and beliefs about back pain, behavior, compensation issues, diagnosis and treatment, emotions, family and work.58 These yellow flags should be seen as factors that can be influenced positively to facilitate recovery and reduce work loss and long term disability.58 Haggman, et al.68 felt that two questions were particularly significant to ask the patient to screen for depressive symptoms:1) “During the past month, have you often been bothered by feeling down, depressed, or hopeless?” and 2) “During the past month, have you been bothered by little interest or pleasure in doing things?”37,69 If the answers to these questions are positive, the patient should be monitored closely and if progress does not occur, then further psychological follow-ups should be considered.70 Does the patient have trouble with work, leisure activities, washing, or dressing? How far can the patient walk before the pain begins?71 What is the patient’s level of disability? Disability implies the effect of the pathology on activity, not pain. Thus, disability testing commonly revolves around activities of daily living (ADLs) and functional activities. Thus, this question may be tied in with the use of the questions in the functional assessment discussed later.
Finally, the examiner must be aware that although in most cases, people who have low back pain have simple mechanical back problems or have nerve root problems involving the disc, there is always the possibility of nonmusculoskeletal causes (e.g., kidney stones, abdominal aortic aneurysm, pancreatic problems) or serious spinal pathology (e.g., tumors).23,37 Waddell outlined signs and symptoms that would lead the examiner to conclude that more serious pathology is present in the lumbar spine (Table 9-6).3
TABLE 9-3
Some Implications of Painful Reactions
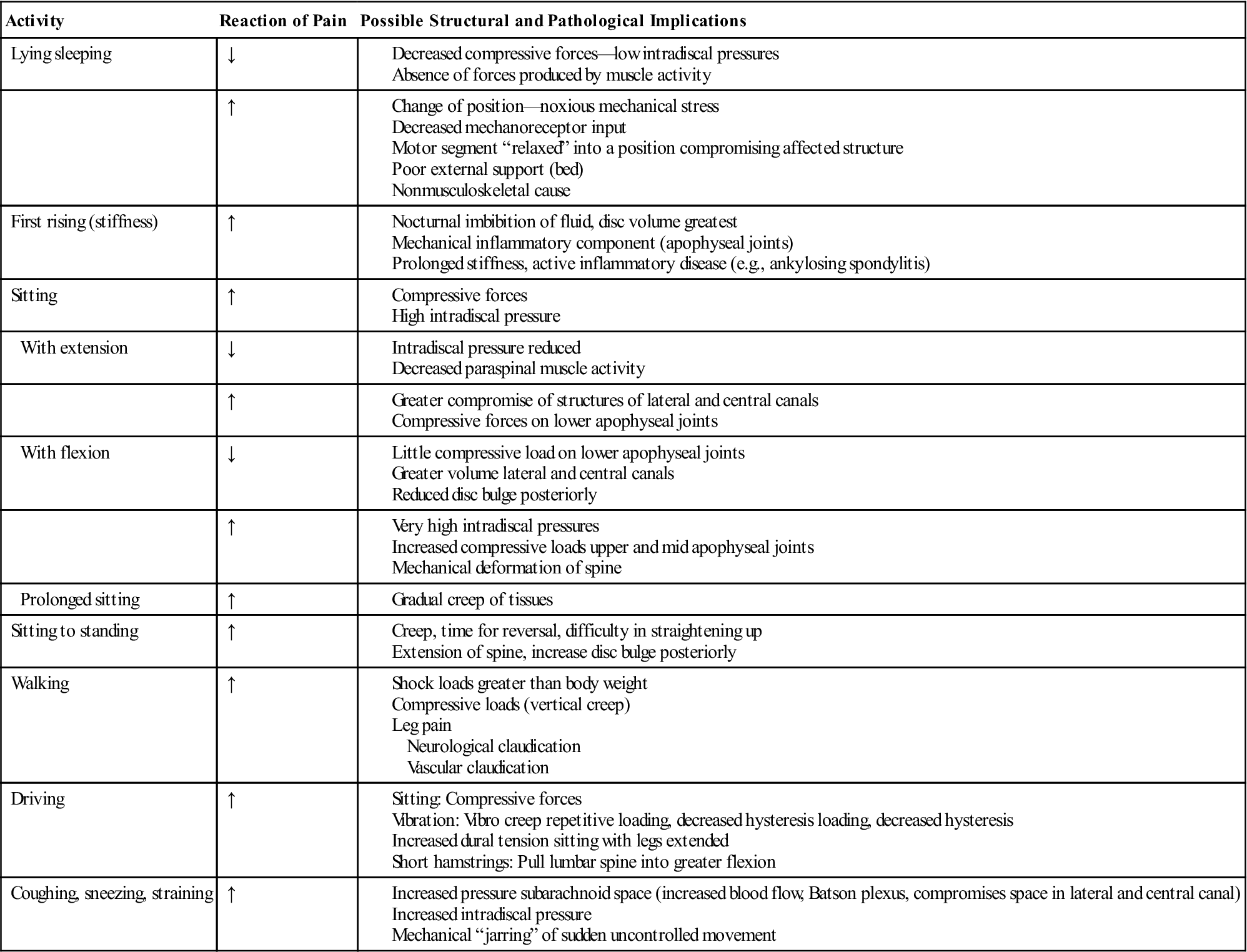
From Jull GA: Examination of the lumbar spine. In Grieve GP, editor: Modern manual therapy of the vertebral column, Edinburgh, 1986, Churchill Livingstone, p. 553.
TABLE 9-4
Some Mechanisms of Musculoskeletal Pain
| Behavior of Pain | Possible Mechanisms |
| Constant ache | |
| Pain on movement | |
| Pain accumulates with activity | |
| Pain increases with sustained postures | |
| Latent nerve root pain |
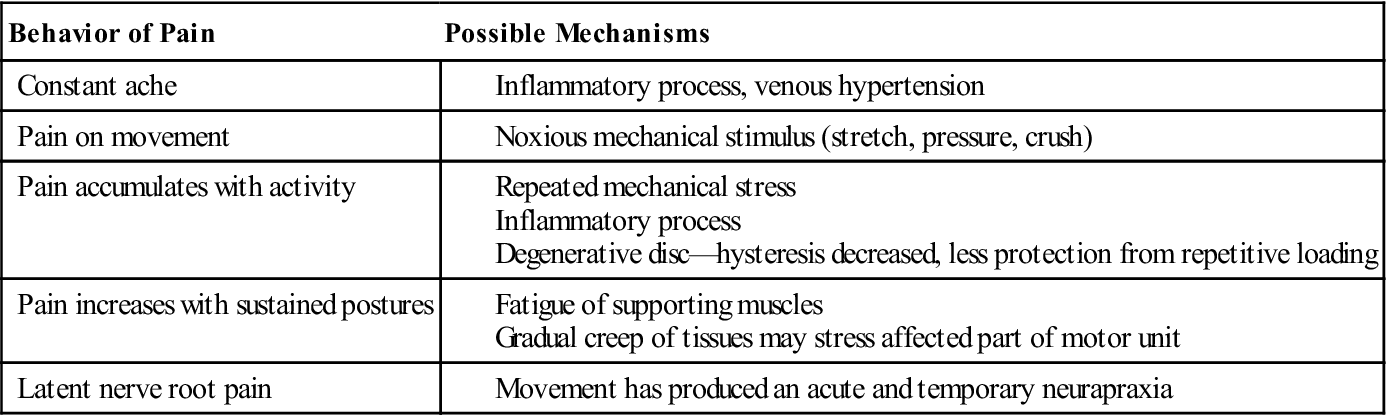
From Jull GA: Examination of the lumbar spine. In Grieve GP, editor: Modern manual therapy of the vertebral column, Edinburgh, 1986, Churchill Livingstone, p. 553.
TABLE 9-5
Differential Diagnosis of Mechanical Low Back Pain
| Muscle Strain | Herniated Nucleus Pulposus | Osteoarthritis | Spinal Stenosis | Spondylolisthesis | Scoliosis | |
| Age (year) | 20 to 40 | 30 to 50 | >50 | >60 | 20 | 30 |
| Pain pattern | ||||||
| Location | Back (unilateral) | Back, leg (unilateral) | Back (unilateral) | Leg (bilateral) | Back | Back |
| Onset | Acute | Acute (prior episodes) | Insidious | Insidious | Insidious | Insidious |
| Standing | ↑ | ↓ | ↑ | ↑ | ↑ | ↑ |
| Sitting | ↓ | ↑ | ↓ | ↓ | ↓ | ↓ |
| Bending | ↑ | ↑ | ↓ | ↓ | ↑ | ↑ |
| Straight leg raise | − | + | − | + (stress) | − | − |
| Plain x-ray | − | − | + | + | + | + |
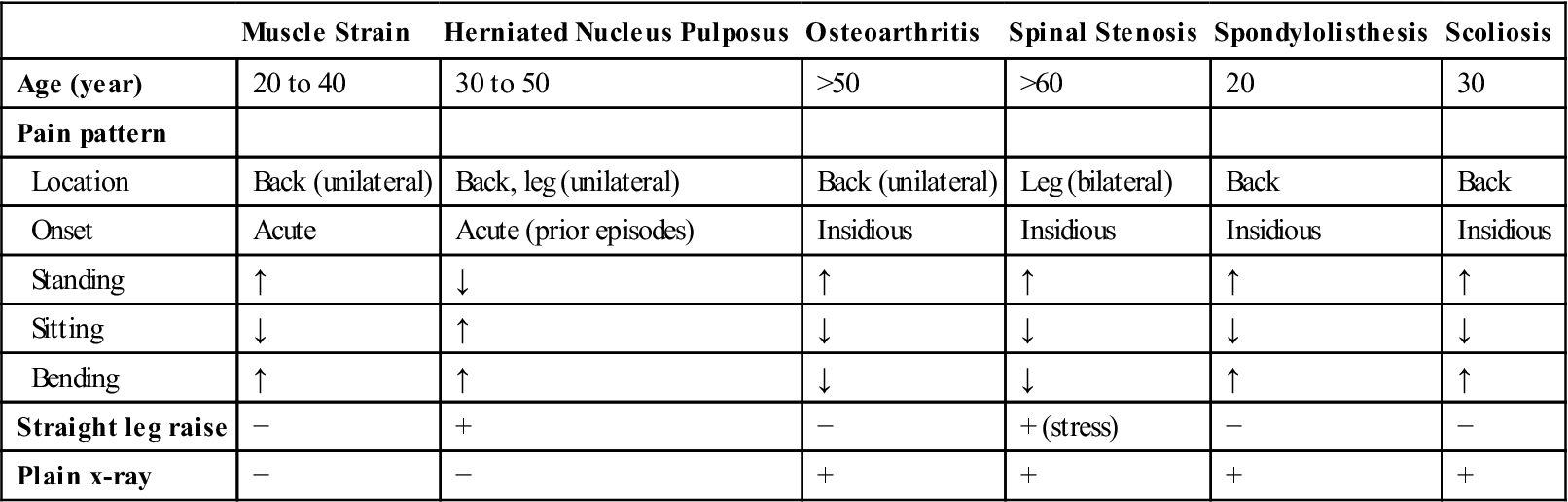
From Borenstein DG, et al: Low back pain: medical diagnosis and comprehensive management, Philadelphia, 1995, WB Saunders, p. 189.
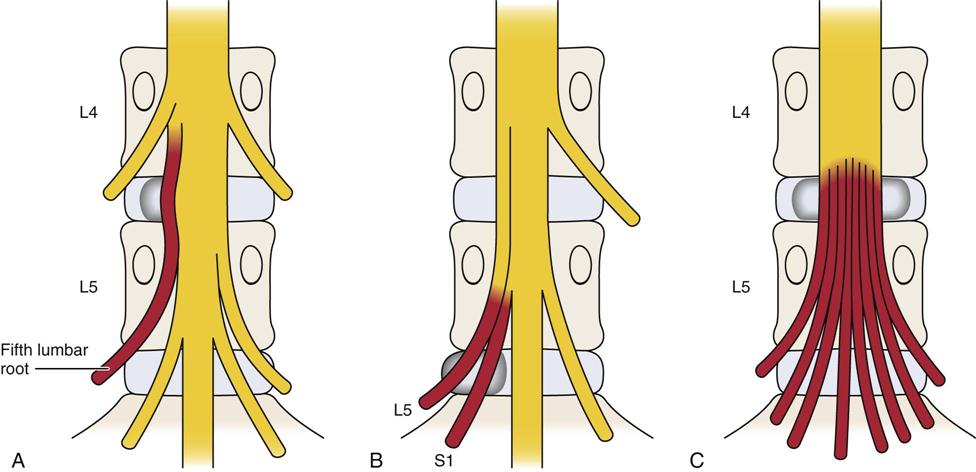
A, Herniation of the disc between L4 and L5 compresses the fifth lumbar root. B, Large herniation of the L5–S1 disc compromises not only the nerve root crossing it (first sacral nerve root) but also the nerve root emerging through the same foramen (fifth lumbar nerve root). C, Massive central sequestration of the disc at the L4–L5 level involves all of the nerve roots in the cauda equina and may result in bowel and bladder paralysis. (Redrawn from MacNab I: Backache, Baltimore, 1977, Williams & Wilkins, pp. 96–97.)
![]() TABLE 9-6
TABLE 9-6
Indications of Serious Spinal Pathology
| Red Flags | Cauda Equina Syndrome/Widespread Neurologic Disorder | Inflammatory Disorders (Ankylosing Spondylitis and Related Disorders) |
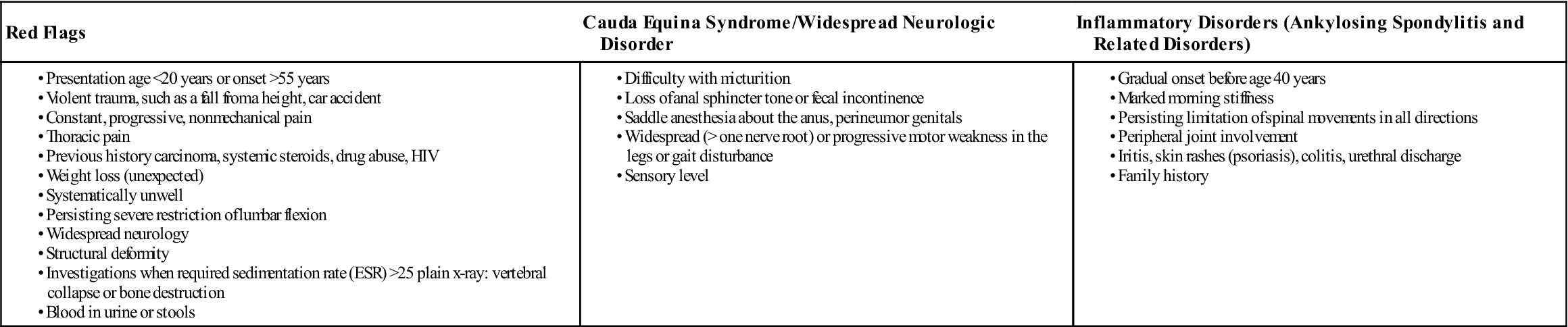
ESR, Erythrocyte sedimentation rate; HIV, human immunodeficiency virus.
From Waddell G: The back pain revolution, New York, 1998, Churchill Livingstone, p. 12.
Observation
The patient must be suitably undressed. Males must wear only shorts, and females must wear only a bra and shorts. When doing the observation, the examiner should note the patient’s willingness to move and the pattern of movement. The patient should be observed for the following traits, first in the standing and then in the sitting position.
Body Type
There are three general body types (see Figure 15-24): ectomorphic—thin body build, characterized by relative prominence of structures developed from the embryonic ectoderm; mesomorphic—muscular or sturdy body build, characterized by relative prominence of structures developed from the embryonic mesoderm; and endomorphic—heavy (fat) body build, characterized by relative prominence of structures developed from the embryonic endoderm.
Gait
Does the gait appear to be normal when the patient walks into the examination area, or is it altered in some way? If it is altered, the examiner must take time to find out whether the problem is in the limb or whether the gait is altered to relieve symptoms elsewhere.
Attitude
What is the patient’s appearance? Is the patient tense, bored, lethargic, healthy looking, emaciated, overweight?
Total Spinal Posture
The patient should be examined in the habitual relaxed posture (see Chapter 15) that he or she would usually adopt. With acute back pain, the patient presents with some degree of antalgic (painful) posturing. Usually, a loss of lumbar lordosis is present, and there may be a lateral shift or scoliosis. This posturing is involuntary and often cannot be reduced because of the muscle spasm.72,73
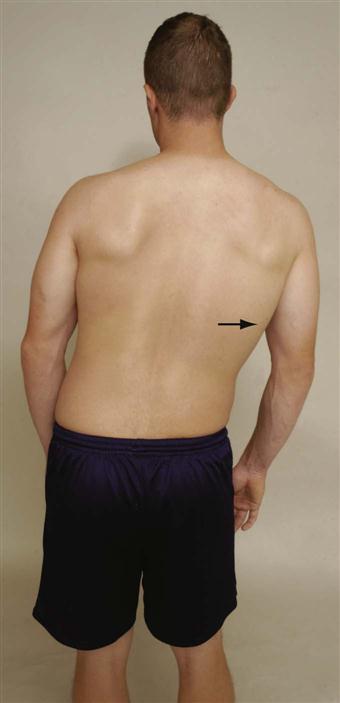
The patient should be observed anteriorly, laterally, and posteriorly (Figure 9-17). During the observation, the examiner should pay particular attention to whether the patient holds the pelvis “in neutral” naturally; if not, is he or she able to achieve the “neutral pelvis” position in standing (normal lordotic curve with the ASISs being slightly lower [one to two finger widths] than the PSISs). Many people with back pain are unable to maintain a neutral pelvis position. Three questions should be considered when looking for a neutral pelvis and whether the pelvis can be stabilized:

A, Anterior view. B, Posterior view. C, Lateral view.
These questions will help the examiner determine if the pelvis (and lumbar spine) can be stabilized during different movements or positions so that other muscles originating from the pelvis can function properly. For example, side lying hip abduction should be able to be performed in the frontal plane with the lower limbs, pelvis, trunk and shoulder aligned in the frontal plane (active hip abduction test ![]() ) (Figure 9-18).74 If the leg wobbles, the pelvis tips, the shoulders or trunk rotate, the hip flexes or the abducted limb medially rotates, it is an indication of lack of movement control and lack of muscle strength and balance.
) (Figure 9-18).74 If the leg wobbles, the pelvis tips, the shoulders or trunk rotate, the hip flexes or the abducted limb medially rotates, it is an indication of lack of movement control and lack of muscle strength and balance.

Note how shoulders, trunk, pelvis, and lower limbs are all in alignment in a negative test.
Anteriorly, the head should be straight on the shoulders, and the nose should be in line with the manubrium, sternum, and xiphisternum or umbilicus. The shoulders and clavicle should be level and equal, although the dominant side may be slightly lower. The waist angles should be equal. Does the patient show a lateral shift or list (Figure 9-19)? Such a shift may be straight lateral movement or it may be a scoliosis (rotation involved). The straight shift is more likely to be caused by mechanical dysfunction and muscle spasm and is likely to disappear on lying down or hanging.3,75 True scoliosis commonly has compensating curves and does not change with hanging or lying down. The arbitrary “high” points on both iliac crests should be the same height. If they are not, the possibility of unequal leg length should be considered. The difference in height would indicate a functional limb length discrepancy. This discrepancy could be caused by altered bone length, altered mechanics (e.g., pronated foot on one side), or joint dysfunction (Table 9-7). The ASISs should be level. The patellae should point straight ahead. The lower limbs should be straight and not in genu varum or genu valgum. The heads of the fibulae should be level. The medial malleoli should be level, as should be the lateral malleoli. The medial longitudinal arches of the feet should be evident, and the feet should angle out equally. The arms should be an equal distance from the trunk and equally medially or laterally rotated. Any protrusion or depression of the sternum, ribs, or costicartilage, as well as any bowing of bones, should be noted. The bony or soft-tissue contours should be equal on both sides.
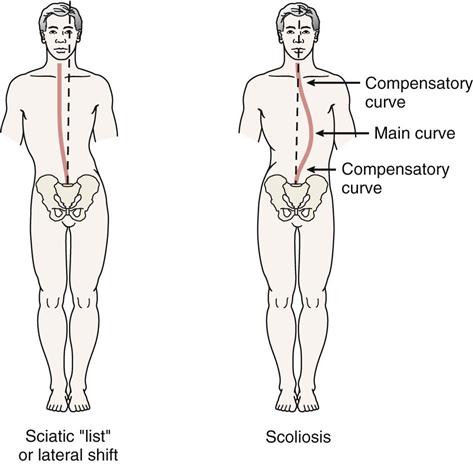
TABLE 9-7
Functional Limb Length Difference
| Joint | Functional Lengthening | Functional Shortening |
| Foot | Supination | Pronation |
| Knee | Extension | Flexion |
| Hip | Lowering | Lifting |
| Extension | Flexion | |
| Lateral rotation | Medial rotation | |
| Sacroiliac | Anterior rotation | Posterior rotation |
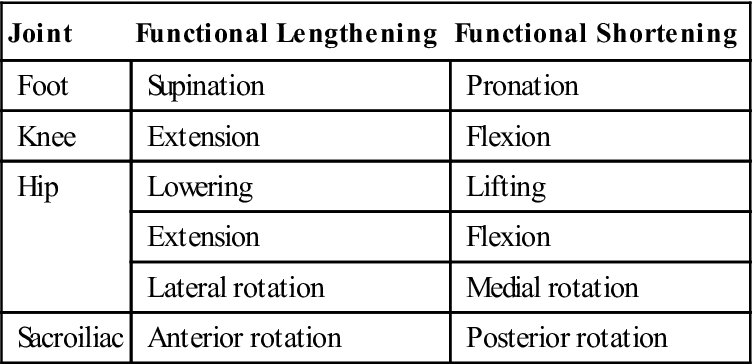
From Wallace LA: Lower quarter pain: mechanical evaluation and treatment. In Grieve GP, editor: Modern manual therapy of the vertebral column, Edinburgh, 1986, Churchill Livingstone, p. 467.
From the side, the examiner should look at the head to ensure that the ear lobe is in line with the tip of the shoulder (acromion process) and the arbitrary highpoint of the iliac crest. Each segment of the spine should have a normal curve. Are any of the curves exaggerated or decreased? Is lordosis present? Kyphosis? Do the shoulders droop forward? Normally with a neutral pelvis, the ASISs are slightly lower than the PSISs. Are the knees straight, flexed, or in recurvatum (hyperextended)?
From behind, the examiner should note the level of the shoulders, spines and inferior angles of the scapula, and any deformities (e.g., a Sprengel deformity). Any lateral spinal curve (scoliosis) should be noted (Figure 9-20). If the scoliotic curve is because of a disc herniation, the herniation usually occurs on the convex side of the curve.76 The waist angles should be equal from the posterior aspect, as they were from the anterior aspect. The PSISs should be level. The examiner should note whether the PSISs are higher or lower than the ASISs and the patient’s ability to maintain a neutral pelvis. The gluteal folds and knee joints should be level. The Achilles tendons and heels should appear to be straight. The examiner should note whether there is any protrusion of the ribs or bowing of bones. Any deviation in the normal spinal postural alignment should be noted and recorded. The various possible sources of pathology related to posture are discussed in Chapter 15.
Janda and Jull described a lumbar or pelvic crossed syndrome (Figure 9-21) to show the effect of muscle imbalance on the ability of a patient to hold and maintain a neutral pelvis.77 With this syndrome, they hypothesized that there was a combination of weak, long muscles and short, strong muscles, which resulted in an imbalance pattern leading to low back pain.78 They felt that only by treating the different groups appropriately could the back pain be relieved. The weak, long inhibited muscles were the abdominals and gluteus maximus, whereas the strong tight (shortened) muscles were the hip flexors (primarily iliopsoas) and the back extensors. The imbalance pattern promotes increased lumbar lordosis because of the forward pelvic tilt and hip flexion contracture and overactivity of the hip flexors compensating for the weak abdominals. The weak gluteals result in increased activity in the hamstrings and erector spinae as compensation to assist hip extension. Interestingly, although the long spinal extensors show increased activity, the short lumbar muscles (e.g., multifidus, rotatores) show weakness. Also, the hamstrings show tightness as they attempt to pull the pelvis backward to compensate for the anterior rotation caused by the tight hip flexors. Weakness of gluteus medius results in increased activity of the quadratus lumborum and tensor fasciae latae on the same side. This syndrome is often seen in conjunction with upper crossed syndrome (see Chapter 3). The two syndromes together are called the layer syndrome.77
Markings
A “faun’s beard” (tuft of hair) may indicate a spina bifida occulta or diastematomyelia (see Figure 9-20).79 Café au lait spots may indicate neurofibromatosis or collagen disease (Figure 9-22). Unusual skin markings or the presence of skin lesions in the midline may lead the examiner to consider the possibility of underlying neural and mesodermal anomalies. Musculoskeletal anomalies tend to form at the same time embryologically. Thus, if the examiner finds one anomaly, he or she must consider the possibility of other anomalies.
Step Deformity
A step deformity in the lumbar spine may indicate a spondylolisthesis. The “step” occurs because the spinous process of one vertebra becomes prominent when either the vertebra above (for example, spondylitic spondylolisthesis) or the affected vertebra (for example, spondylolytic spondylolisthesis) slips forward on the one below (Figure 9-23).
Examination
When assessing the lumbar spine, the examiner must remember that referral of symptoms or the presence of neurological symptoms often makes it necessary to “clear” or rule the lower limb pathology. Many of the symptoms that occur in the lower limb may originate in the lumbar spine. Unless there is a history of definitive trauma to a peripheral joint, a screening or scanning examination must accompany assessment of that joint to rule out problems within the lumbar spine referring symptoms to that joint. It is often helpful at this stage to ask the patient to demonstrate the movements that produce or have produced the pain. When asking the patient to do this, the examiner must allow time for symptoms to disappear before completing the examination.
Active Movements
Active movements are performed with the patient standing (Figure 9-24). The examiner is looking for differences in ROM and the patient’s willingness to do the movement. The ROM taking place during the active movement is normally the summation of the movements of the entire lumbar spine, not just movement at one level, along with hip movement. The most painful movements are done last. If the problem is mechanical, at least one or more of the movements will be painful.27

 Figure 9-24 Active movements of the lumbar spine.
Figure 9-24 Active movements of the lumbar spine.A and B, Measuring forward flexion using tape measure. C, Extension. D, Side flexion (anterior view). E, Side flexion (posterior view). F, Rotation (standing). G, Rotation (sitting).
While the patient is doing the active movements, the examiner looks for limitation of movement and its possible causes, such as pain, spasm, stiffness, or blocking. As the patient reaches the full range of active movement, passive overpressure may be applied, but only if the active movements appear to be full and pain free. The overpressure must be applied with extreme care, because the upper body weight is already being applied to the lumbar joints by virtue of their position and gravity. If the patient reports that a sustained position increases the symptoms, then the examiner should consider having the patient maintain the position (e.g., flexion) at the end of the ROM for 10 to 20 seconds to see whether symptoms increase. Likewise, if repetitive motion or combined movements have been reported in the history as causing symptoms, these movements should be performed as well, but only after the patient has completed the basic movements.
The greatest motion in the lumbar spine occurs between the L4 and L5 vertebrae and between L5 and S1. There is considerable individual variability in the ROM of the lumbar spine (Figure 9-25).80–84 In reality, little obvious movement occurs in the lumbar spine especially in the individual segments because of the shape of the facet joints, tightness of the ligaments, presence of the intervertebral discs, and size of the vertebral bodies.
For flexion (forward bending), the maximum ROM in the lumbar spine is normally 40° to 60°. The examiner must differentiate the movement occurring in the lumbar spine from that occurring in the hips or thoracic spine. Some patients can touch their toes by flexing the hips, even if no movement occurs in the spine. On forward flexion, the lumbar spine should move from its normal lordotic curvature to at least a straight or slightly flexed curve (Figure 9-26).85 If this change in the spine does not occur, there is probably some hypomobility in the lumbar spine resulting from either tight structures or muscle spasm. The degree of injury also has an effect. For example, the more severely a disc is injured (for example, if sequestration has occurred rather than a protrusion), the greater the limitation of movement.86 With disc degeneration, intersegmental motion may increase as disc degeneration increases up to a certain point and follows Kirkaldy-Willis’s description of degenerative changes in the disc.87 He divided the changes into three stages: dysfunctional, unstable, and stable. During the first two phases, intersegmental motion increases in flexion, rotation, and side flexion88 and then decreases in the final stabilization phase. During the unstable phase, it is often possible to see an instability “jog” during one or more movements, especially flexion, returning to neutral from flexion, or side flexion.89,90 An instability jog is a sudden movement shift or “rippling” of the muscles during active movement, indicating an unstable segment.85,91 Similarly, muscle twitching during movement or complaints of something “slipping out” during lumbar spine movement may indicate instability.92 If the patient bends one or both knees on forward flexion, the examiner should watch for nerve root symptoms or tight hamstrings, especially if spinal flexion is decreased when the knees are straight. If tight hamstrings or nerve root symptoms are suspected, the examiner should perform suitable tests (see “Special Tests” section) to determine if the hamstrings or nerve root restriction (see “Knee Flexion Test”) are the cause of the problem. When returning to the upright posture from forward flexion, the patient with no back pain first rotates the hips and pelvis to about 45° of flexion; during the last 45° of extension, the low back resumes its lordosis. In patients with back pain, commonly, most movement occurs in the hips, accompanied by knee flexion, and sometimes with hand support working up the thighs.93 As with the thoracic spine, the examiner may use a tape measure to determine the increase in spacing of the spinous processes on forward flexion. Normally, the measurement should increase 7 to 8 cm (2.8 to 3.1 inches) if it is taken between the T12 spinous process and S1 (see Figures 9-24, A and B). The examiner should note how far forward the patient is able to bend (i.e., to midthigh, knees, midtibia, or floor) and compare this finding with the results of straight leg raising tests (see “Special Tests” section). Straight leg raising, especially if bilateral, is essentially the same movement done passively, except that it is a movement occurring from below upward instead of from above downward.

During the active movements, especially during flexion or extension, the examiner should watch for a painful arc. The pain seen in a lumbar painful arc tends to be neurologically based (i.e., it is lancinating or lightening-like), but it may also be caused by instability. If it does occur on movement in the lumbar spine, it is likely that a space-occupying lesion (most likely a small herniation of the disc) is pinching the nerve root in part of the range as the nerve root moves with the motion.75
Maigne described an active movement flexion maneuver to help confirm lumbar movement and control.72 In this happy round maneuver, the patient bends forward and places the hands on a bed or on the back of a chair. The patient then attempts to arch or hunch the back. Most patients with lumbar pathology are unable to sustain the hunched position.
Extension (backward bending) is normally limited to 20° to 35° in the lumbar spine. While performing the movement, the patient is asked to place the hands in the small of the back to help stabilize the back. Bourdillon and Day have advocated doing this movement in the prone lying position to hyperextend the spine.94 They called the resulting position the sphinx position. The patient hyperextends the spine by resting on the elbows with the hands holding the chin (Figure 9-27) and allows the abdominal wall to relax. The position is held for 10 to 20 seconds to see if symptoms occur or, if present, become worse.

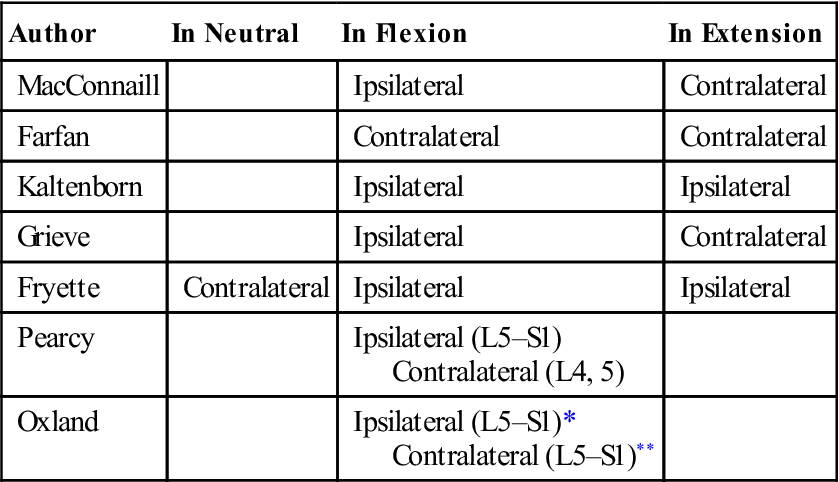
Side (lateral) flexion or side bending is approximately 15° to 20° in the lumbar spine. The patient is asked to run the hand down the side of the leg and not to bend forward or backward while performing the movement. The examiner can then eyeball the movement and compare it with that of the other side. The distance from the fingertips to the floor on both sides may also be measured, noting any difference. In the spine, the movement of side flexion is a coupled movement with rotation. Because of the position of the facet joints, both side flexion and rotation occur together although the amount of movement and direction of movement may not be the same. Table 9-8 shows how different authors interpret the coupled movement in the spine. As the patient side flexes, the examiner should watch the lumbar curve. Normally, the lumbar curve forms a smooth curve on side flexion, and there should be no obvious sharp angulation at only one level. If angulation does occur, it may indicate hypomobility below the level or hypermobility above the level in the lumbar spine (Figure 9-28). Mulvein and Jull advocated having the patient do a lateral shift (Figure 9-29) in addition to side flexion.95 Their viewpoint is that lateral shift in the lumbar spine focuses the movement more in the lower spine (L4–S1) and helps eliminate the compensating movements in the rest of the spine.
TABLE 9-8
| Author | In Neutral | In Flexion | In Extension |
| MacConnaill | Ipsilateral | Contralateral | |
| Farfan | Contralateral | Contralateral | |
| Kaltenborn | Ipsilateral | Ipsilateral | |
| Grieve | Ipsilateral | Contralateral | |
| Fryette | Contralateral | Ipsilateral | Ipsilateral |
| Pearcy | Ipsilateral (L5–S1) Contralateral (L4, 5) |
||
| Oxland | Ipsilateral (L5–S1)* Contralateral (L5–S1)** |
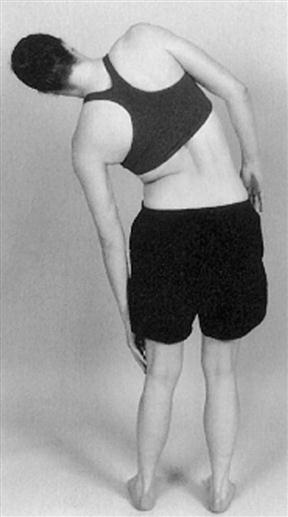
Note that lower lumbar spine stays straight and upper lumbar and lower thoracic spine side flexes. This finding would indicate hypomobility in the lower lumbar spine.
Rotation in the lumbar spine is normally 3° to 18° to the left or right, and it is accomplished by a shearing movement of the lumbar vertebrae on each other. Although the patient is usually in the standing position, rotation may be performed while sitting to eliminate pelvic and hip movement. If the patient stands, the examiner must take care to watch for this accessory movement and try to eliminate it by stabilizing the pelvis.
If a movement such as side flexion toward the painful side increases the symptoms, the lesion is probably intra-articular, because the muscles and ligaments on that side are relaxed. If a disc protrusion is present and lateral to the nerve root, side flexion to the painful side increases the pain and radicular symptoms on that side. If a movement (such as, side flexion away from the painful side) alters the symptoms, the lesion may be articular or muscular in origin, or it may be a disc protrusion medial to the nerve root (Figure 9-30).
McKenzie advocated repeating the active movements, especially flexion and extension, ten times to see whether the movement increases or decreases the symptoms.39 He also advocated, like Mulvein and Jull,95 a side gliding movement in which the head and feet remain in position and the patient shifts the pelvis to the left and to the right.
If the examiner finds that side flexion and rotation have been equally limited and extension has been limited to a lesser extent, a capsular pattern may be suspected. A capsular pattern in one lumbar segment, however, is difficult to detect.
Because back injuries rarely occur during a “pure” movement (such as, flexion, extension, side flexion, or rotation), it has been advocated that combined movements of the spine should be included in the examination.96,97 The examiner may want to test the following more habitual combined movements: lateral flexion in flexion, lateral flexion in extension, flexion and rotation, and extension and rotation. These combined movements (Figure 9-31) may cause signs and symptoms different from those produced by single plane movements and are definitely indicated if the patient has shown that a combined movement is what causes the symptoms. For example, if the patient is suffering from a facet syndrome, combined extension and rotation is the movement most likely to exacerbate symptoms.98 Other symptoms that would indicate facet involvement include absence of radicular signs or neurological deficit, hip and buttock pain, and sometimes leg pain above the knee, no paresthesia, and low back stiffness.99,100

A, Lateral flexion in flexion. B, Lateral flexion in extension. C, Rotation and flexion. D, Rotation and extension.
While the patient is standing, the examiner may perform a quick test of the lower peripheral joints (Figure 9-32), provided the examiner feels the patient has the ability to do the test. The patient squats down as far as possible, bounces two or three times, and returns to the standing position. This action quickly tests the ankles, knees, and hips as well as the sacrum for any pathological condition. If the patient can fully squat and bounce without any signs and symptoms, these joints are probably free of pathology related to the complaint. However, this test should be used only with caution and should not be done with patients suspected of having arthritis or pathology in the lower limb joints, pregnant patients, or older patients who exhibit weakness and hypomobility. If this test is negative, there is no need to test the peripheral joints (peripheral joint scan) with the patient in the lying position.
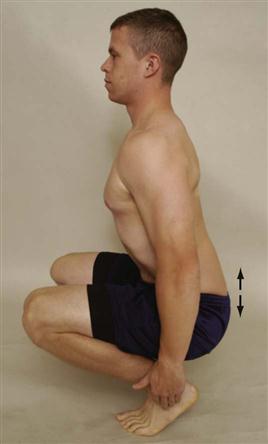
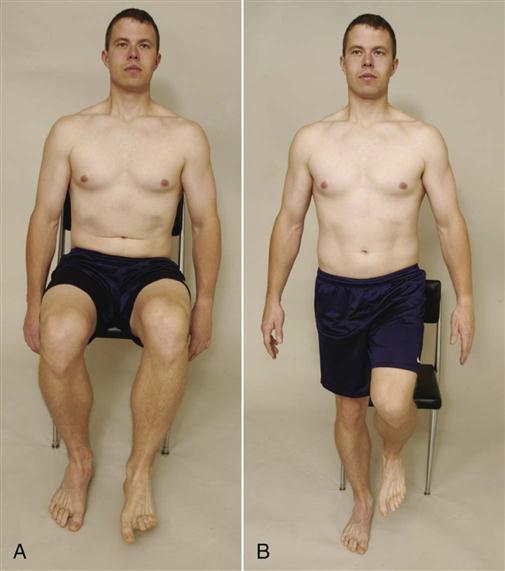
 Figure 9-32 Quick test.
Figure 9-32 Quick test.The patient is then asked to balance on one leg and to go up and down on the toes four or five times. This is, in effect, a modified Trendelenberg test. While the patient does this, the examiner watches for Trendelenburg sign (Figure 9-33). A positive Trendelenburg sign is shown by the nonstance side ilium dropping down instead of elevating as it normally would when standing on the leg. A weak gluteus medius muscle or a coxa vara (abnormal shaft-neck angle of the femur) on the stance leg side may produce a positive sign. If the patient is unable to complete the movement by going up and down on the toes, the examiner should suspect an S1 nerve root lesion. Both legs are tested.

 Figure 9-33 Trendelenburg and S1 nerve root test.
Figure 9-33 Trendelenburg and S1 nerve root test.A, Negative Trendelenburg test (hip hikes) while doing S1 test (up and down on toes). B, Positive Trendelenburg test (hip drops) while doing S1 test. If patient cannot go up on toes, it would indicate a positive S1 test. C, Posterior view. Positive Trendelenburg test for a weak right gluteus medius.
McKenzie advocated doing flexion movements with the patient in the supine lying position as well.39 In the standing position, flexion in the spine takes place from above downward, so pain at the end of the ROM indicates that L5–S1 is affected. When the patient is in the supine lying position with the knees being lifted to the chest, flexion takes place from below upward so that pain at the beginning of movement indicates that L5–S1 is affected. Remember that greater stretch is placed on L5–S1 when the patient is in the lying position.
During the observation stage of the assessment, the examiner will have noted any changes in functional limb length (see Table 9-7). Wallace developed a method for measuring functional leg length.101 The patient is first assessed in a relaxed stance. In this position, the examiner palpates the ASISs and the PSISs, noting any asymmetry. The examiner then places the patient in a symmetric stance, ensuring that the subtalar joint is in the neutral position (see Chapter 13), the toes are straight ahead, and the knees are extended. The ASISs and PSISs are again assessed for asymmetry. If differences are still noted, the examiner should check for structural leg length differences (see Chapters 10 and 11), sacroiliac joint dysfunction, or weak gluteus medius or quadratus lumborum (Figure 9-34). The pelvis may also be leveled with the use of calibrated blocks or cards so that the functional length difference can be recorded.
Passive Movements
In the lumbar spine, passive movements are difficult to perform because of the weight of the body. If active movements are full and pain free, overpressure can be attempted with care. However, it is safer to check the end feel of the individual vertebrae in the lumbar spine during the assessment of joint play movements. The end feel is the same, but the examiner has better control of the patient and is less likely to overstress the joints.
Resisted Isometric Movements
Resisted isometric muscle strength of the lumbar spine is first tested in the neutral position. The patient is seated. The contraction must be resisted and isometric so that no movement occurs (Figure 9-35). Because of the strength of the trunk muscles, the examiner should say, “Don’t let me move you,” so that movement is minimized. The examiner tests flexion, extension, side flexion, and rotation. Figure 9-36 shows the axes of movement of the lumbar spine. The lumbar spine should be in a neutral position, and the painful movements should be done last. The examiner should keep in mind that strong abdominal muscles help to reduce the load on the lumbar spine by approximately 30% and on the thoracic spine by approximately 50%, as a result of the increased intrathoracic and intra-abdominal pressures caused by the contraction of these muscles. Table 9-9 lists the muscles acting on the lumbar vertebrae.
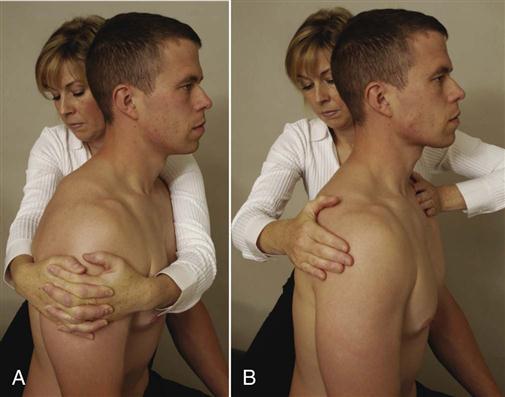
A, Flexion, extension, and side flexion. B, Rotation to right.
TABLE 9-9
Muscles of the Lumbar Spine: Their Actions and Nerve Root Derivations
| Action | Muscles Acting | Nerve Root Derivation |
| Forward flexion | 1. Psoas major | L1–L3 |
| 2. Rectus abdominis | T6–T12 | |
| 3. External abdominal oblique | T7–T12 | |
| 4. Internal abdominal oblique | T7–T12, L1 | |
| 5. Transversus abdominis | T7–T12, L1 | |
| 6. Intertransversarii | L1–L5 | |
| Extension | 1. Latissimus dorsi | Thoracodorsal (C6–C8) |
| 2. Erector spinae | L1–L3 | |
| iliocostalis lumborum | L1–L3 | |
| longissimus thoracis | L1–L5 | |
| 3. Transversospinalis | L1–L5 | |
| 4. Interspinales | L1–L5 | |
| 5. Quadratus lumborum | T12, L1–L4 | |
| 6. Multifidus | L1–L5 | |
| 7. Rotatores | L1–L5 | |
| 8. Gluteus maximus | L1–L5 | |
| Side flexion | 1. Latissimus dorsi | Thoracodorsal (C6–C8) |
| 2. Erector spinae | L1–L3 | |
| iliocostalis lumborum | L1–L3 | |
| longissimus thoracis | L1–L5 | |
| 3. Transversalis | L1–L5 | |
| 4. Intertransversarii | L1–L5 | |
| 5. Quadratus lumborum | T12, L1–L4 | |
| 6. Psoas major | L1–L3 | |
| 7. External abdominal oblique | T7–T12 | |
| Rotation* | 1. Transversalis | L1–L5 |
| 2. Rotatores | L1–L5 | |
| 3. Multifidus | L1–L5 |
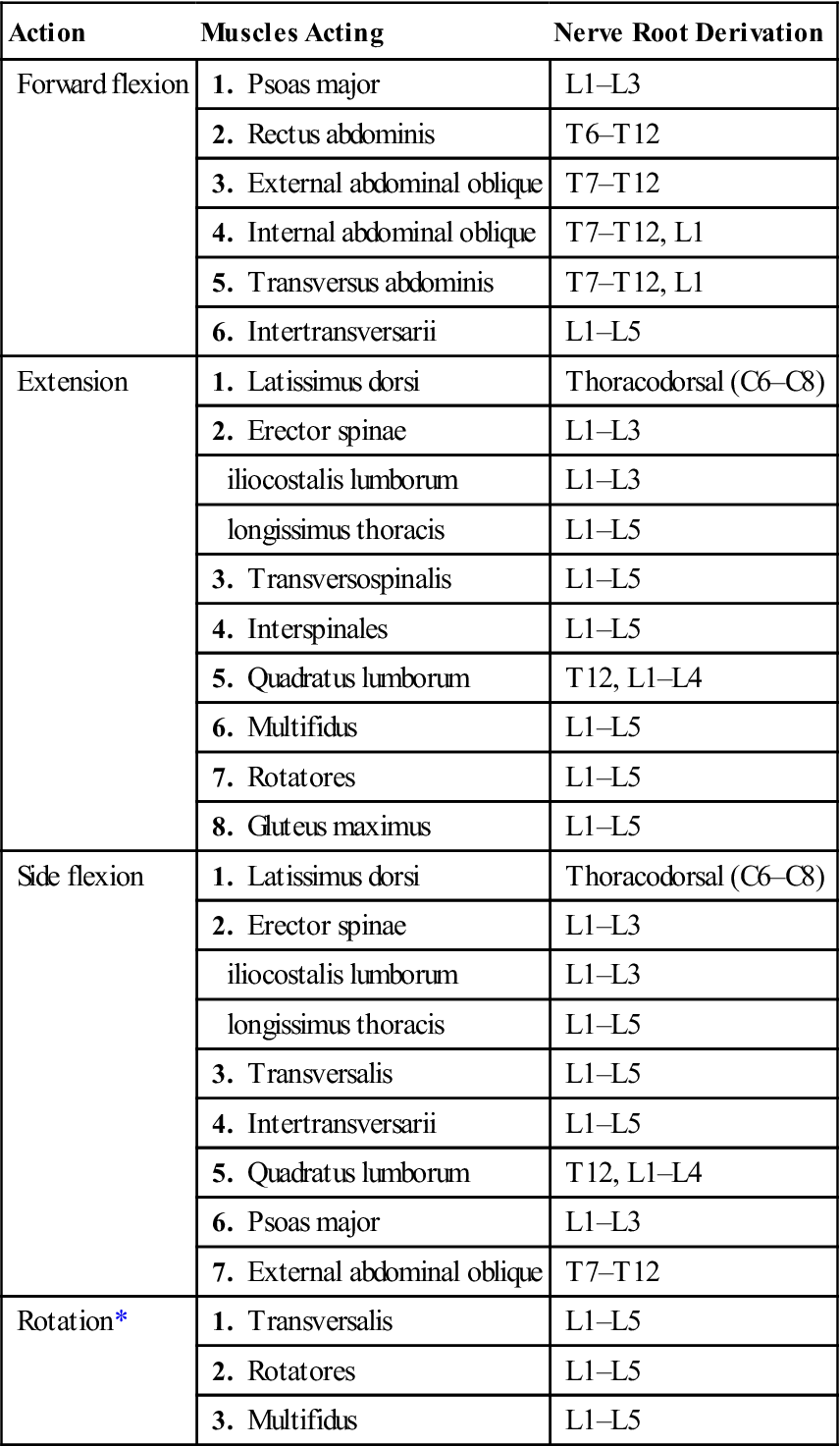
*Very little rotation occurs in the lumbar spine because of the shape of the facet joints. Any rotation would be a result of shearing movement.
Provided neutral isometric testing is normal or only causes a small amount of pain, the examiner can go on to other tests, which will place greater stress on the muscles. These tests are often dynamic and provide both concentric and eccentric work for the muscles supporting the spine. With all of the following tests, the examiner should ensure that the patient can hold a neutral pelvis. If there is excessive movement of the ASIS (supine) or PSIS (prone) when doing the test, the patient should not be allowed to do them. In normal individuals, the ASIS or PSIS should not move when doing the tests. Motivation may also affect the results.102
Dynamic Abdominal Endurance Test.103,104
This test checks the endurance of the abdominals. The patient is in supine with the hips at 45° and knees at 90° and hands at sides. A line is drawn 8 cm (for patients over 40 years of age) or 12 cm (for patients under 40 years of age) distal to the fingers. The patient tucks in the chin and curls the trunk to touch the line with the fingers (Figure 9-37) and repeats as many curls as possible using a cadence of twenty-five repetitions per minute. The number of repetitions possible before cheating (holding breath, altered mechanics) or fatigue occurs is recorded as the score. The test may also be done as an isometric test (Figure 9-38) by assuming the end position and holding it. The grading for this isometric abdominal test would be as follows105–107:
• Normal (5) = Hands behind neck, until scapulae clear table (20 to 30 second hold)
• Good (4) = Arms crossed over chest, until scapulae clear table (15 to 20 second hold)
• Fair (3) = Arms straight, until scapulae clear table (10 to 15 second hold)
• Poor (2) = Arms extended, toward knees, until top of scapulae lift from table (1 to 10 second hold)

 Figure 9-37 Dynamic abdominal endurance test.
Figure 9-37 Dynamic abdominal endurance test.The patient tucks in the chin and curls up the trunk lifting the trunk off the bed. Ideally, the scapula should clear the bed.
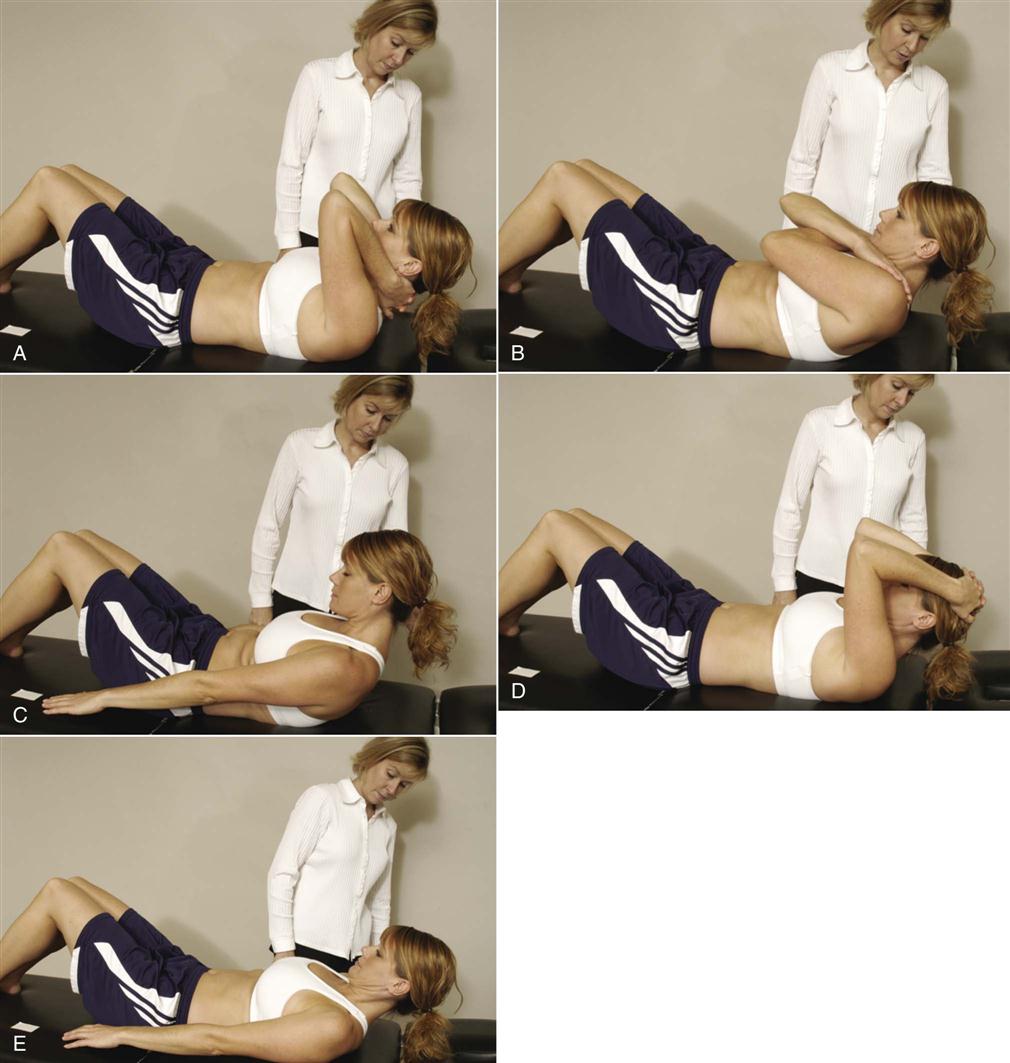
 Figure 9-38 Isometric abdominal test.
Figure 9-38 Isometric abdominal test.A, Hands behind neck. B, Arms crossed over chest, scapulae off table. C, Arms straight, scapulae off table. D, Hands behind head, top of scapulae off table. E, Arms straight, only head off table.
McGill108 advocated doing the isometric test by starting with the patient resting against a back rest angled at 60o from the horizontal with the hips and knees flexed to 90o and the arms folded across the chest and the hands on opposite shoulders (Figure 9-39). The patient’s feet are held securely and the back rest is lowered away from the patient’s back while the patient maintains the 60o position as long as possible.
Dynamic Extensor Endurance Test.103,109,110
This test is designed to test the strength of iliocostalis lumborum (erector spinae) and multifidus. The patient is placed in prone lying with the hips and iliac crests resting on the end of the examining table and the hips and pelvis stabilized with straps (Figure 9-40). Initially, the patient’s hands support the upper body in 30° flexion on a chair or bench (see Figure 9-40, A). Keeping the spine straight, the examiner instructs the patient to extend the trunk to neutral and then lower the head to the start position. During the exercise, the patient’s arms are crossed at the chest. The cadence is twenty-five repetitions per minute. The number of repetitions possible before cheating (holding breath, altered mechanics) or fatigue occurs is recorded as the score. The test may also be done isometrically, and the examiner times how long the patient can hold the contraction without pelvic or spinal movement. This test may also be done with the patient beginning in prone lying and extending the spine if the preceding test is too hard.111,112 In this case, the patient can start with the hands by the side, moving the hands in the small of the back, and finally moving the hands behind the head for increasing difficulty. The test, if done isometrically (isometric extensor test) (Figure 9-41), would be graded as follows105–107:
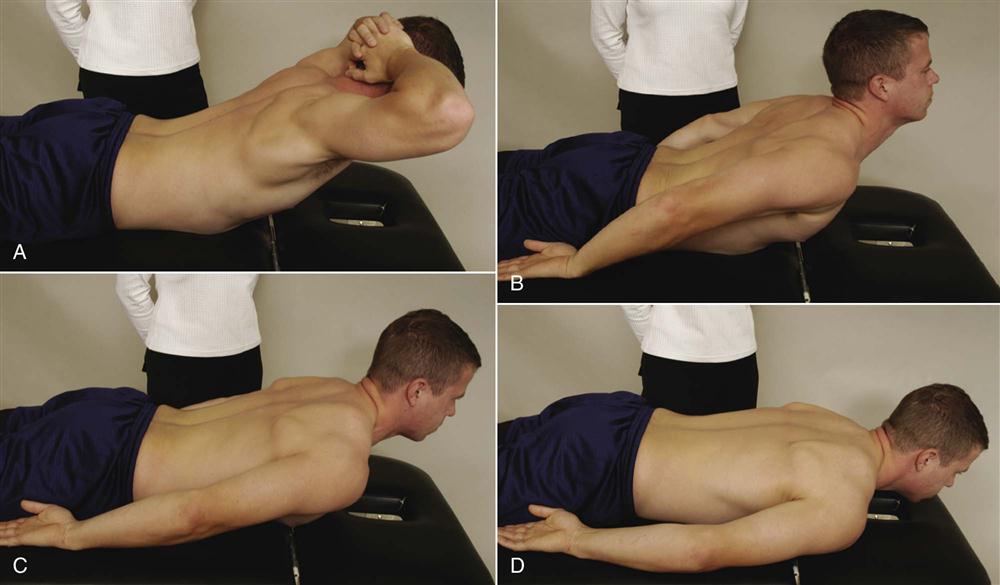
 Figure 9-41 Isometric extensor test.
Figure 9-41 Isometric extensor test.A, Hands behind head, lift head, chest, and ribs off bed. B, Hands at side, lift head, chest, and ribs off bed. C, Hands at side, lift sternum off bed. D, Hands at side, lift head off bed.
Biering and Sorensen described a similar test (Biering-Sorensen fatigue test) in which the subject had arms by the side, and the time the patient was able to hold the straight position before fatigue was recorded (i.e., the patient could not hold the position).113,114 The start position is the same as for the dynamic test.
Double Straight Leg Lowering Test.111,112,115
(Note: This test checks the abdominals. It should only be performed if the patient receives a “normal” grade in the dynamic abdominal endurance test or the abdominal isometric test.) This is an abdominal eccentric test that can place a great deal of stress on the spine so the examiner must ensure the patient is able to hold a neutral pelvis before doing the exercise. It also causes greater abdominal activation than curlups.116 The patient lies supine and flexes the hips to 90° (Figure 9-42, A) and then straightens the knees (Figure 9-42, B). The patient then positions the pelvis in neutral (i.e., the PSISs are slightly superior to the ASISs) by doing a posterior pelvic tilt and holding the spinous processes tightly against the examining table. The straight legs are eccentrically lowered (Figure 9-42, C). As soon as the ASISs start to rotate forward, the test is stopped, the angle measured (plinth to thigh angle), and the knees bent. The test must be done slowly, and the patient must not hold his or her breath. The grading of the test is as follows106:
Internal/External Abdominal Obliques Test.111,112
This test checks the combined action of the internal oblique muscle of one side and the external oblique muscle on the opposite side. The patient is in supine lying with hands by the side. The patient is asked to lift the head and shoulder on one side and reach over and touch the fingernails of the other hand (Figure 9-43, A). The examiner counts the number of repetitions the patient performs. The patient’s feet should not be supported and the patient should breathe normally. The test can be made more difficult by asking the patient to put the hands on the opposite shoulders across the chest (Figure 9-43, B) and do the test by taking the elbow toward where the fingers would have rested beside the body or, more difficult still, by putting the hands behind the head and taking the elbows toward the position where the fingernails would have rested beside the body (Figure 9-43, C). The grading of the test, if done isometrically (isometric internal/external abdominal oblique test), would be as follows106:
• Normal (5) = Flexes and rotates the lumbar spine fully with hands behind head (20 to 30 second hold)
• Good (4) = Flexes and rotates the lumbar spine fully with hands across chest (15 to 20 second hold)
• Poor (2) = Unable to flex and rotate fully
• Trace (1) = Only slight contraction of the muscle with no movement
Dynamic Horizontal Side Support (Side Bridge) Test.117
This movement tests the quadratus lumborum muscle. The patient is in a side lying position resting the upper body on his or her elbow (Figure 9-44, A). To begin, the patient side lies with the knees flexed to 90°. The examiner asks the patient to lift the pelvis off the examining table (Figure 9-44, B) and straighten the spine. The patient should not roll forward or backward when doing the test. The patient repeats the movement as many times as possible in a dynamic test or holds for as long as possible in an isometric test. In younger, more fit patients, the test can be made more difficult by having the legs straight and asking the patient to lift the knees and pelvis off the examining table with the feet as the base so the whole body is straight (Figure 9-44, C). As an isometric test, the test would be graded as follows:
• Normal (5) = Able to lift pelvis off examining table and hold spine straight (10 to 20 second hold)
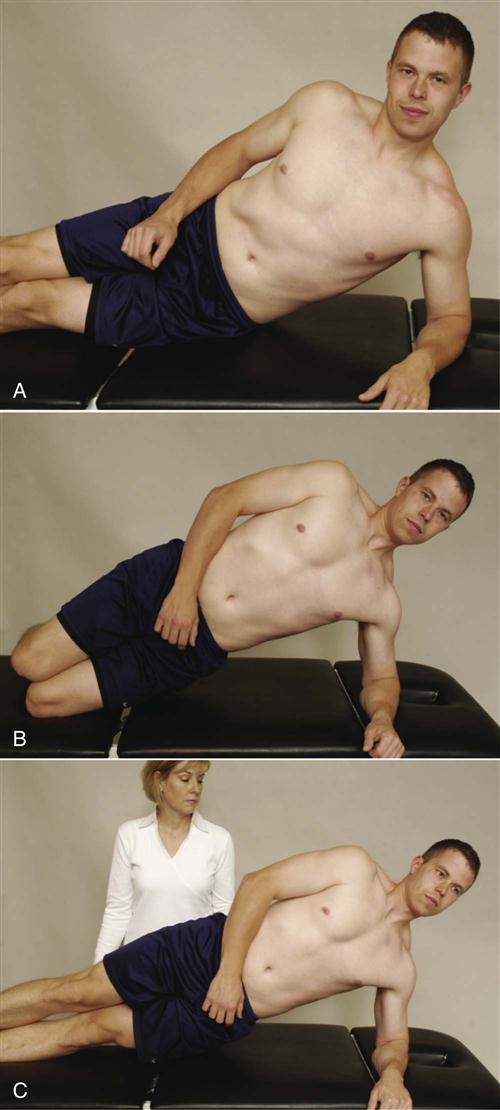
 Figure 9-44 Dynamic horizontal side support.
Figure 9-44 Dynamic horizontal side support.A, Start position. B, Lifting pelvis off bed using knees as support. C, Lifting pelvis off bed using feet and ankles as support.
McGill reported that the side bridge should be able to be held 65% of the extensor time for men and 39% for women and 99% of the flexor time for men and 79% for women.118
Back Rotators/Multifidus Test.
This test checks the ability of the lumbar rotators and multifidus to stabilize the trunk during dynamic extremity movement. The patient assumes the quadriped position (Figure 9-45, A) and is asked to hold the “neutral pelvis” position and breathe normally. The patient is then asked to do the following movements (Figure 9-45, B–D):
1. Single straight arm lift and hold
2. Single straight leg lift and hold
3. Contralateral straight arm and straight leg lift and hold
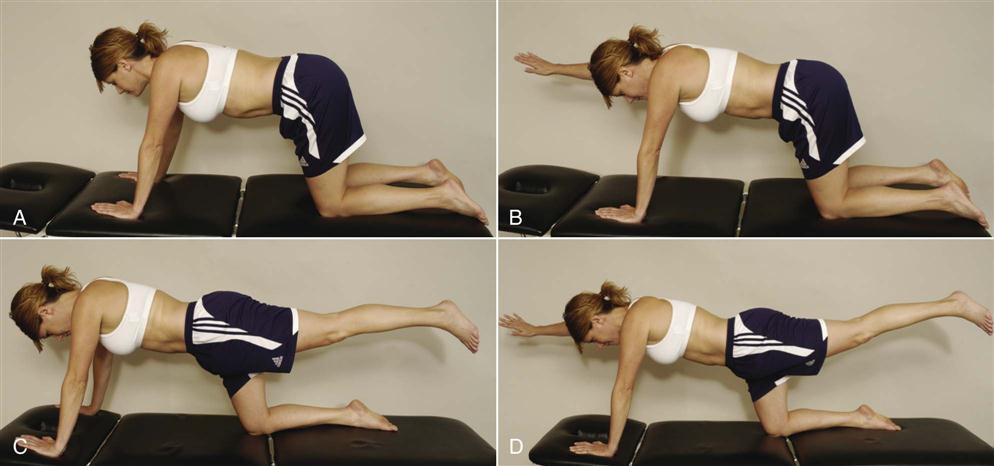
A, Start position. B, Single straight arm lift. C, Single straight leg lift. D, Contralateral straight arm and leg lift.
The scoring for the test would be as follows:
• Fair (3) = Able to do single arm lift and maintain neutral pelvis (20 second hold)
• Poor (2) = Unable to maintain neutral pelvis while doing single arm lift
If tested isokinetically, the back extensors are stronger than the flexors. Men produce a force equal to approximately 65% of body weight in flexion, whereas women produce approximately 65% to 70% of their body weight in flexion. In extension, men produce approximately 90% to 95% of their body weight, and women produce 80% to 95% of their body weight, depending on the speed tested. In rotation, men produce approximately 55% to 65% of their body weight, whereas women produce approximately 40% to 55% of their body weight, depending on the speed tested.119
Peripheral Joint Scanning Examination
After the resisted isometric movements of the lumbar spine have been completed, if the examiner did not use the quick test to test the peripheral joints or is unsure of the findings or whether the peripheral joints are involved, the peripheral joints should be quickly scanned to rule out obvious pathology in the extremities. Any deviation from normal should lead the examiner to do a detailed examination of that joint. The following joints are scanned.120
Sacroiliac Joints
With the patient standing, the examiner palpates the PSIS on one side with one thumb and one of the sacral spines with the other thumb. The patient then fully flexes the hip on that side, and the examiner notes whether the PSIS drops as it normally should or whether it elevates, indicating fixation of the sacroiliac joint on that side (Figure 9-46). The examiner then compares the other side. The examiner next places one thumb on one of the patient’s ischial tuberosities and one thumb on the sacral apex. The patient is then asked to flex the hip on that side again. If the movement is normal, the thumb on the ischial tuberosity moves laterally. If the sacroiliac joint on that side is fixed, the thumb moves up. The other side is then tested for comparison. This test has also been called Gillet’s or the sacral fixation test (see Chapter 10).
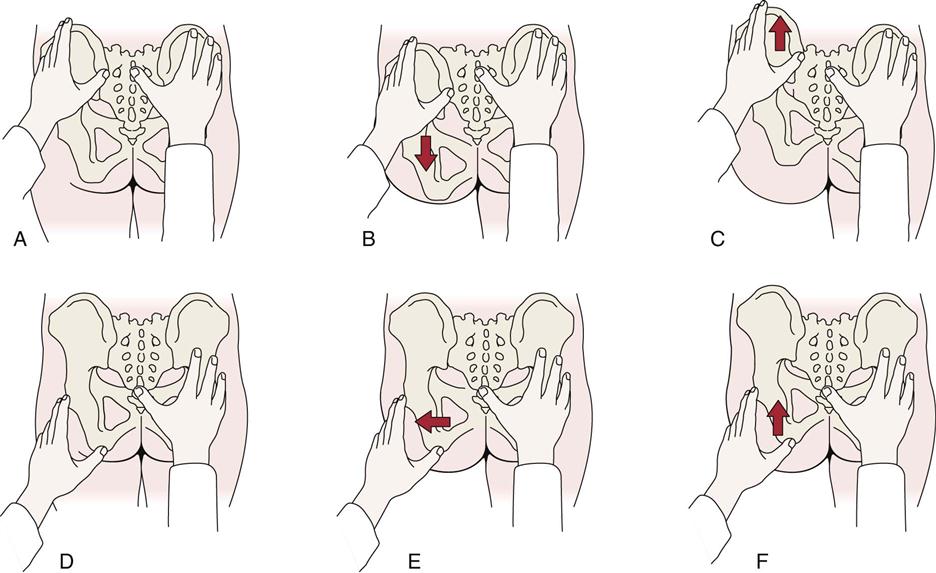
 Figure 9-46 Tests to demonstrate left sacroiliac fixation.
Figure 9-46 Tests to demonstrate left sacroiliac fixation.A, Examiner places the left thumb on the posterior superior iliac spine (PSIS) and the right thumb over one of the sacral spinous processes. B, With normal movement, the examiner’s left thumb moves downward as the patient raises the left leg with full hip flexion. C, If the joint is fixed, the examiner’s left thumb moves upward as the patient raises the left leg. D, The examiner places the left thumb over the ischial tuberosity and the right thumb over the apex of the sacrum. E, With normal movement, the examiner’s left thumb moves laterally as the patient raises the left leg with full hip flexion. F, If the joint is fixed, the examiner’s left thumb moves slightly upward as the patient raises the left leg. (Modified from Kirkaldy-Willis WH: Managing low back pain, New York, 1983, Churchill Livingstone, p. 94.)
Hip Joints
These joints are actively moved through flexion, extension, abduction, adduction, and medial and lateral rotation in as full a ROM as possible. Any pattern of restriction or pain should be noted. As the patient flexes the hip, the examiner may palpate the ilium, sacrum, and lumbar spine to determine when movement begins at the sacroiliac joint on that side and at the lumbar spine during the hip movement. The two sides should be compared.
Knee Joints
The patient actively moves the knee joints through as full a range of flexion and extension as possible. Any restriction of movement or abnormal signs and symptoms should be noted.
Foot and Ankle Joints
Plantar flexion, dorsiflexion, supination, and pronation of the foot and ankle as well as flexion and extension of the toes are actively performed through a full ROM. Again, any alteration in signs and symptoms should be noted.
Myotomes
Having completed the scanning examination of the peripheral joints, the examiner next tests the patient’s muscle power for possible neurological weakness (Table 9-10).120 With the patient lying supine, the myotomes are assessed individually (Figure 9-47). When testing myotomes (Table 9-11), the examiner should place the test joint or joints in a neutral or resting position and then apply a resisted isometric pressure. The contraction should be held for at least 5 seconds to show any weakness. If feasible, the examiner should test the two sides simultaneously to provide a comparison. The simultaneous bilateral comparison is not possible for movements involving the hip and knee joints because of the weight of the limbs and stress to the low back, so both sides must be done individually. The examiner should not apply pressure over the joints, because this action may mask symptoms.
TABLE 9-10
| Root | Dermatome | Muscle Weakness | Reflexes/Special Tests Affected | Paresthesias |
| L1 | Back, over trochanter, groin | None | None | Groin, after holding posture, which causes pain |
| L2 | Back, front of thigh to knee | Psoas, hip adductors | None | Occasionally front of thigh |
| L3 | Back, upper buttock, front of thigh and knee, medial lower leg | Psoas, quadriceps—thigh wasting | Knee jerk sluggish, PKB positive, pain on full SLR | Inner knee, anterior lower leg |
| L4 | Inner buttock, outer thigh, inside of leg, dorsum of foot, big toe | Tibialis anterior, extensor hallucis | SLR limited, neck-flexion pain, weak knee jerk; side flexion limited | Medial aspect of calf and ankle |
| L5 | Buttock, back and side of thigh, lateral aspect of leg, dorsum of foot, inner half of sole and first, second, and third toes | Extensor hallucis, peroneals, gluteus medius, ankle dorsiflexors, hamstrings—calf wasting | SLR limited to one side, neck-flexion pain, ankle jerk decreased, crossed-leg raising—pain | Lateral aspect of leg, medial three toes |
| S1 | Buttock, back of thigh, and lower leg | Calf and hamstrings, wasting of gluteals, peroneals, plantar flexors | SLR limited | Lateral two toes, lateral foot, lateral leg to knee, plantar aspect of foot |
| S2 | Same as S1 | Same as S1 except peroneals | Same as S1 | Lateral leg, knee, heel |
| S3 | Groin, inner thigh to knee | None | None | None |
| S4 | Perineum, genitals, lower sacrum | Bladder, rectum | None | Saddle area, genitals, anus, impotence |
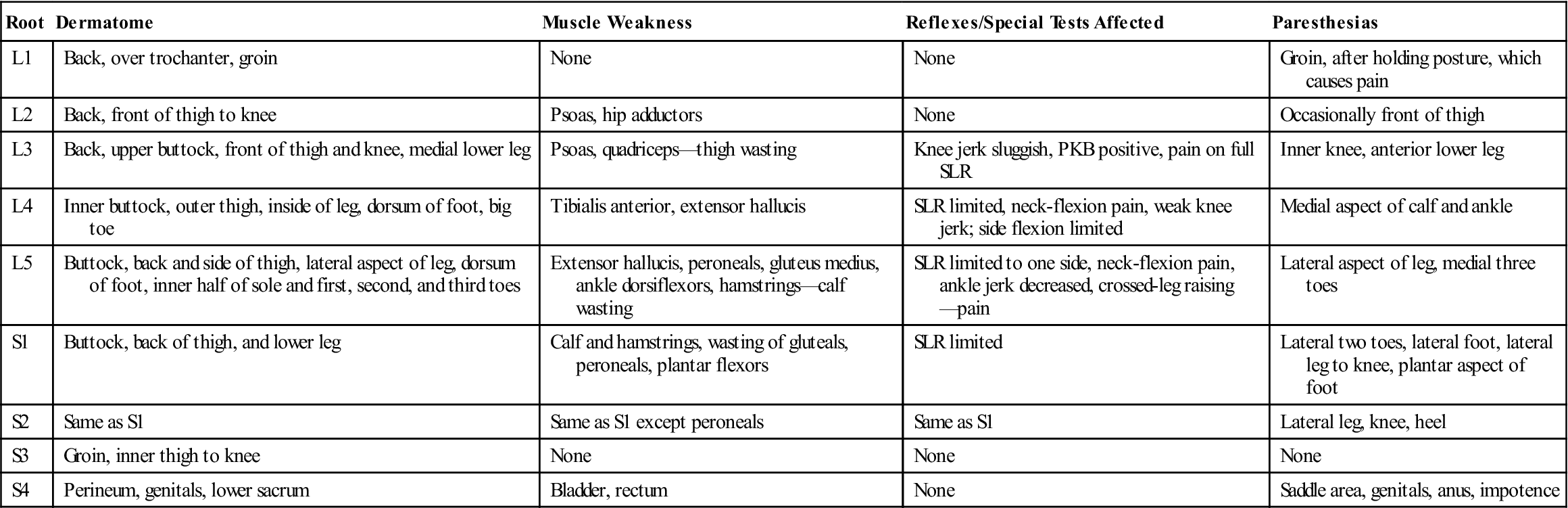
Manipulation and traction are contraindicated if S4 or massive posterior displacement causes bilateral sciatica and S3 pain.
PKB, Prone knee bending; SLR, straight leg raising.
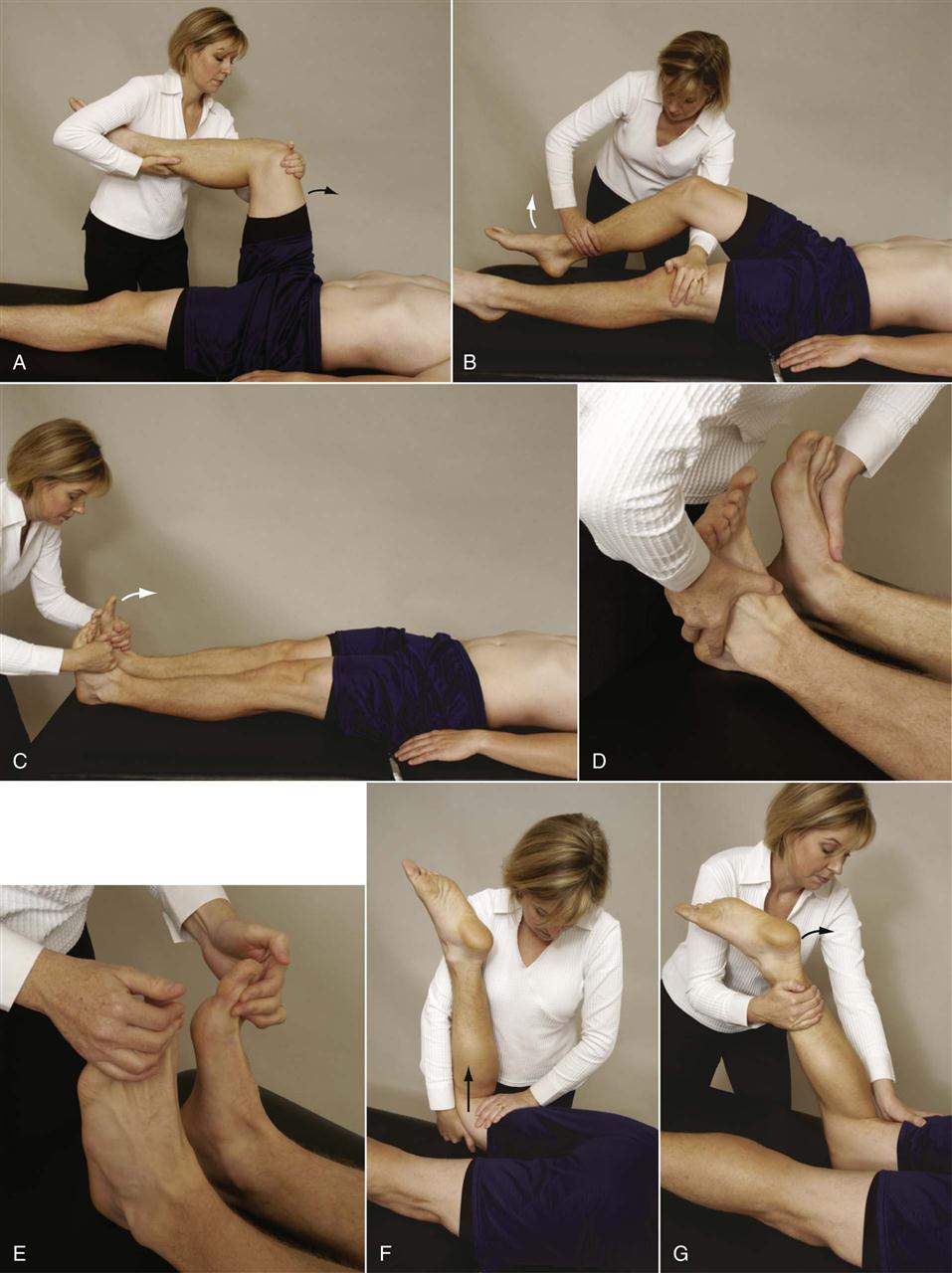
 Figure 9-47 Positioning to test myotomes.
Figure 9-47 Positioning to test myotomes.A, Hip flexion (L2). B, Knee extension (L3). C, Foot dorsiflexion (L4). D, Ankle eversion (S1). E, Extension of the big toe (L5). F, Hip extension (S1). G, Knee flexion (S1–S2).
TABLE 9-11
| Nerve Root | Test Action | Muscles |
| L1–L2 | Hip flexion | Psoas, iliacus, sartorius, gracilis, pectineus, adductor longus, adductor brevis |
| L3 | Knee extension | Quadriceps, adductor longus, magnus, and brevis |
| L4 | Ankle dorsiflexion | Tibialis anterior, quadriceps, tensor fasciae latae, adductor magnus, obturator externus, tibialis posterior |
| L5 | Toe extension | Extensor hallucis longus, extensor digitorum longus, gluteus medius and minimus, obturator internus, semimembranosus, semitendinosus, peroneus tertius, popliteus |
| S1 | Ankle plantar flexion Ankle eversion |
Gastrocnemius, soleus, gluteus maximus, obturator internus, piriformis, biceps femoris, semitendinosus, popliteus, peroneus longus and brevis, extensor digitorum brevis |
| S2 | Hip extension Knee flexion |
Biceps femoris, piriformis, soleus, gastrocnemius, flexor digitorum longus, flexor hallucis longus, intrinsic foot muscles |
| S3 | Knee flexion | Intrinsic foot muscles (except abductor hallucis), flexor hallucis brevis, flexor digitorum brevis, extensor digitorum brevis |
Remember that the examiner has previously tested the S1 myotome with the patient standing and has tested for a positive Trendelenburg sign (modified Trendelenburg test); these movements are repeated here only if the examiner is unsure of the result and wants to test again. The ankle movements should be tested with the knee flexed approximately 30°, especially if the patient complains of sciatic pain, because full dorsiflexion is considered a provocative maneuver for stretching of neurological tissue. Likewise, the extended knee increases the stretch on the sciatic nerve and may result in false signs, such as weakness that results from pain rather than from pressure on the nerve root. Rainville, et al.121 have recommended testing the L3 and L4 nerve roots at the same time by doing a single leg sit-to-stand test to check for unilateral quadriceps weakness (Figure 9-48). Note that the patient can hold the examiner’s hands for balance.
If the patient is in extreme pain, all tests with the patient in the supine position should be completed before the patient is tested in prone. This reduces the amount of movement the patient must do, decreasing the patient’s discomfort. Ideally, all tests in the standing position should be performed first, followed by tests in the sitting, supine, side lying, and prone positions. This procedure is shown in the précis at the end of the chapter.
To test hip flexion (L2 myotome), the examiner flexes the patient’s hip to 30° to 40°. The examiner then applies a resisted force into extension proximal to the knee while ensuring that the heel of the patient’s foot is not resting on the examining table (see Figure 9-47, A). The other side is then tested for comparison. To prevent excessive stress on the lumbar spine, the examiner must ensure that the patient does not increase the lumbar lordosis while doing the test and that only one leg at a time is tested.
To test knee extension or the L3 myotome, the examiner flexes the patient’s knee to 25° to 35° and then applies a resisted flexion force at the midshaft of the tibia ensuring the heel is not resting on the examining table (see Figure 9-47, B). The other side is tested for comparison.
To test ankle dorsiflexion (L4 myotome), the examiner asks the patient to place the feet at 90° relative to the leg (plantigrade position). The examiner applies a resisted force to the dorsum of each foot and compares the two sides (see Figure 9-47, C). Ankle plantar flexion (S1 myotome) is compared in a similar fashion, but the resistance is applied to the sole of the foot. Because of the strength of the plantar flexor muscles, it is better to test this myotome with the patient standing. The patient slowly moves up and down on the toes of each foot (for at least 5 seconds) in turn (modified Trendelenburg test), and the examiner compares the differences as previously described. Ankle eversion (S1 myotome) is tested with the patient in the supine lying position, and the examiner applies a force to move the foot into inversion (see Figure 9-47, D).
Toe extension (L5 myotome) is tested with the patient holding both big toes in a neutral position. The examiner applies resistance to the nails of both toes and compares the two sides (see Figure 9-47, E). It is imperative that the resistance be isometric, so the amount of force in this case is less than that applied during knee extension, for example.
Hip extension (S1 myotome) is tested with the patient lying prone. This test needs to be done only if the patient is unable to do plantar flexion testing in standing or ankle eversion. The knee is flexed to 90°. The examiner then lifts the patient’s thigh slightly off the examining table while stabilizing the leg. A downward force is applied to the patient’s posterior thigh with one hand while the other hand ensures that the patient’s thigh is not resting on the table (see Figure 9-47, F).
Knee flexion (S1–S2 myotomes) is tested in the same position (prone) with the knee flexed to 90°. An extension isometric force is applied just above the ankle (see Figure 9-47, G). Although it is possible to test both knee flexors at the same time, it is not advisable to do this because the stress on the lumbar spine is too great.
Functional Assessment
Injury to the lumbar spine can greatly affect the patient’s ability to function. Activities such as standing, walking, bending, lifting, traveling, socializing, dressing, and sexual intercourse can be affected. Numerical scoring tables may be used to determine the degree of pain caused by lumbar spine pathology or disability. Care must be taken when selecting one of these scales to ensure that it measures the disability from the patient’s perspective.122–125 Examples are the Oswestry Disability Index126–128 (Figure 9-49), the Quebec Back Pain Disability Scale129,130 (Figure 9-50), and the Hendler 10-Minute Screening Test for Chronic Back Pain Patients (Figure 9-51).124,127,131 It has been reported that the Hendler test helps to differentiate organic from functional low back pain.132 The Oswestry Disability Index is a good functional scale because it deals with ADLs and therefore is based on the patient’s response and concerns affecting daily life. It is the most commonly used functional back scale. The disability index is calculated by dividing the total score (each section is worth from 1 to 6 points) by the number of sections answered and multiplying by 100. The Roland-Morris Disability Questionnaire is short and simple, and it is suitable for following up on progress in clinical settings and for combining with other measures of function (e.g., work disability) (Figure 9-52).133,134 Other numerical back pain scales include the Functional Rating Index,135,136 the Dallas Pain Questionnaire,137 the Million Index,138 the Japanese Orthopedic Association Scale,139 the Iowa Low Back Rating Scale,140 the Bournemouth Questionnaire,141,142 the Scoliosis Research Society form (SRS-22 for those with spinal deformity),143–145 the Lumbar Spinal Stenosis Questionnaire,146 and the Aberdeen Back Pain Scale.147 Thomas provide a good review of these and other scales.124 Lehman and colleagues developed a rating scale for lumbar dysfunction (Figure 9-53) that includes assessment criteria, physician criteria, and, perhaps more importantly, patient criteria for determining the degree of dysfunction.140 These criteria can be evaluated during the normal assessment for the patient.
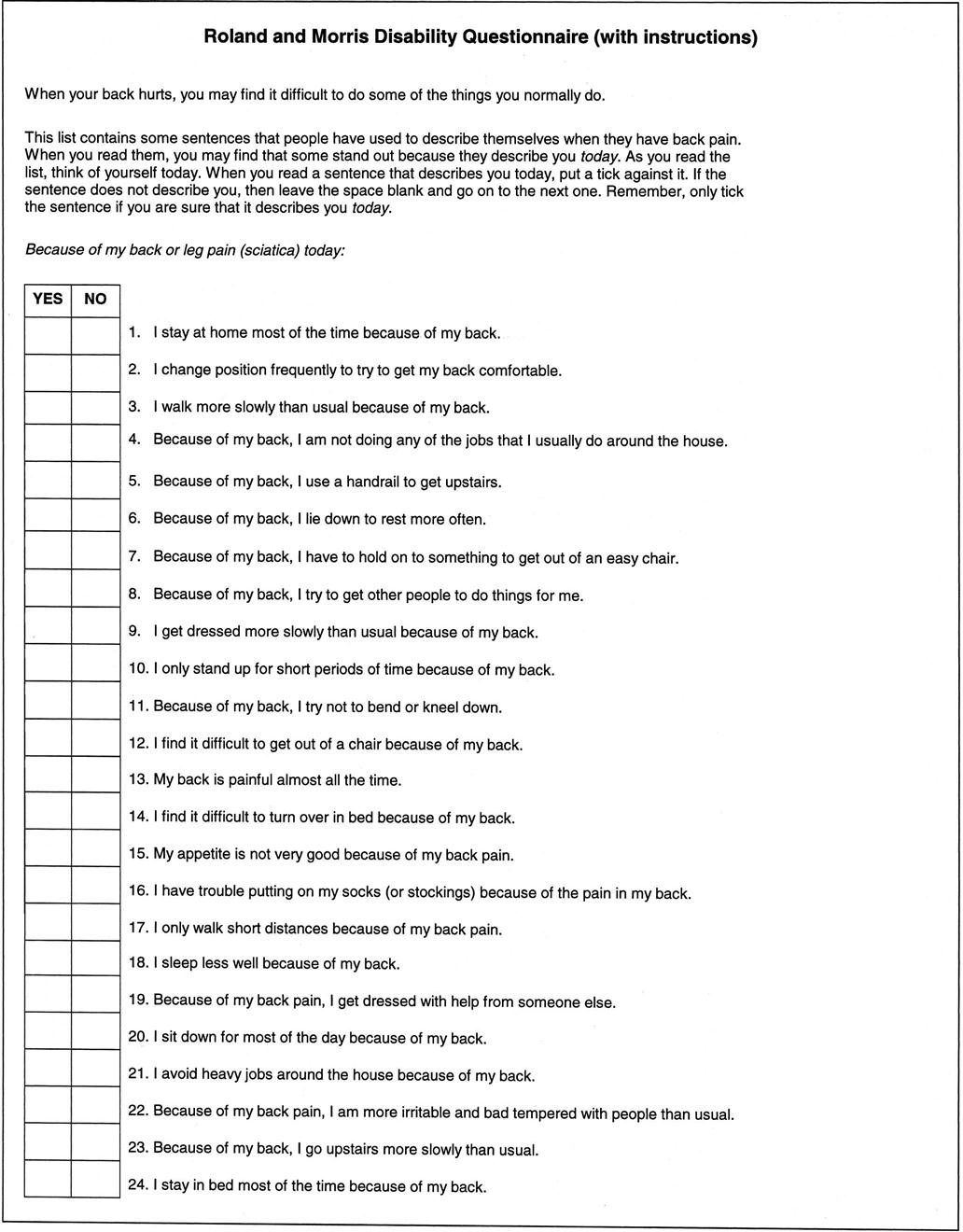
The higher the number of “yes” responses, the greater the disability. (From Roland M, Morris R: A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low back pain. Spine 8:144, 1983.)
Waddell and colleagues developed a series of tests to differentiate between organic and nonorganic back pain.148 Each test counts +1 if positive or 0 if negative:
1. Superficial skin tenderness to light pinch over wide area of lumbar spine
2. Deep tenderness over wide area, often extending to thoracic spine, sacrum, or pelvis
3. Low back pain on axial loading of spine in standing
5. Abnormal neurological (motor or sensory) patterns
6. Overreaction
Positive findings of +3 or more should be investigated for nonorganic cause; these patients may also have social and psychological components to their complaint.3,149,150
Waddell also described a simple clinical functional capacity evaluation (Figure 9-54),3 which examiners may find useful for testing patients.151
Simmonds, et al.152 came up with several functional tests or physical performance measures that they felt would be useful and discriminate between individuals with and without low back pain:
• Repeated Trunk Flexion153: This timed test involves the patient starting in a standing position and then flexing forward as far as possible and returning to the upright posture as fast as tolerable, repeating the motion ten times. The average value of two trials is used as the time.
• Biering-Sorensen Fatigue Test: Described previously under “Resisted Isometric Movements.”
Special Tests
Special tests should always be considered as an integral part of a much larger examination process.154 They should never be used in isolation.155 Many of the special tests in the lumbar spine are purported to have poor diagnostic value.156 Because these are clinical tests and commonly depend on the skill of the examiner, many of them show low reliability and validity or have not been studied at all.157–161 Thus, the icons are graded primarily on clinical experience.
For the reader who would like to review them, the reliability, validity, specificity, sensitivity, and odds ratios of some of the special tests used in the lumbar spine are available on the Evolve website.
APPENDIX 9-1
| BACK PERFORMANCE SCALE | |
| Reliability | Validity |
| CRAMP FINDING | |||
| Sensitivity | Specificity | Responsiveness | Odds Ratio |
| CRANIOSACRAL RHYTHM |
| Reliability |
| DOUBLE STRAIGHT LEG LOWERING TEST |
| Validity |
| DYNAMIC ABDOMINAL ENDURANCE TEST |
| Reliability |
| DYNAMIC EXTENSOR ENDURANCE TEST |
| Reliability |
| EXTENSION (ATTRACTION METHOD FOR MEANS LUMBAR SPINE BACK BEND) |
| Reliability |
| FINGER TO FLOOR | ||
| Reliability | Validity | Responsiveness |
| FUNCTIONAL LEG LENGTH | |
| Reliability | Validity |
| FUNCTIONAL RATING INDEX | ||
| Reliability | Validity | Responsiveness |
| FUNCTIONAL RATING INDEX INTRACLASS | |
| Reliability | Validity |
| GENERAL FUNCTION SCORE | ||
| Reliability | Validity | Responsiveness |
| ISOMETRIC ABDOMINAL TEST |
| Reliability |

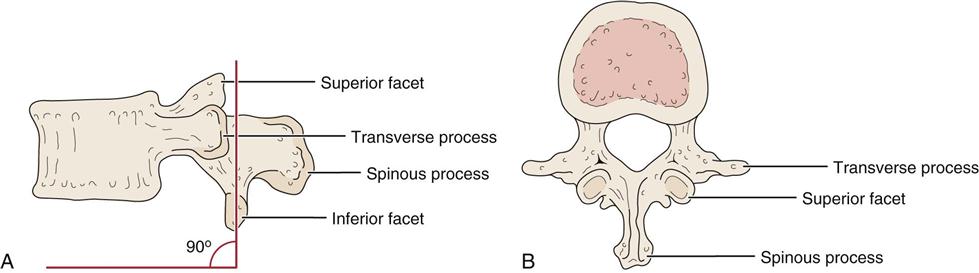
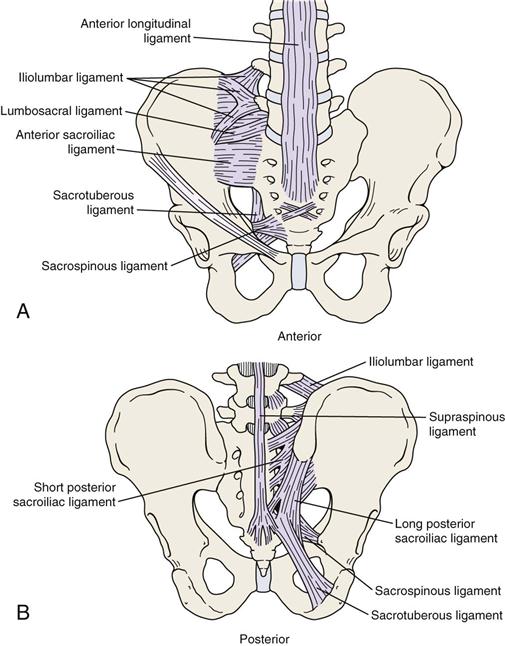
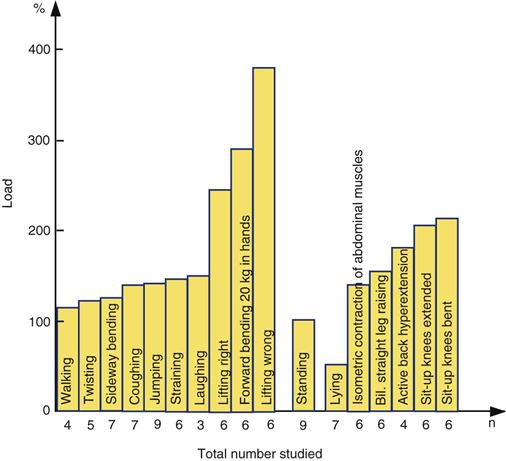
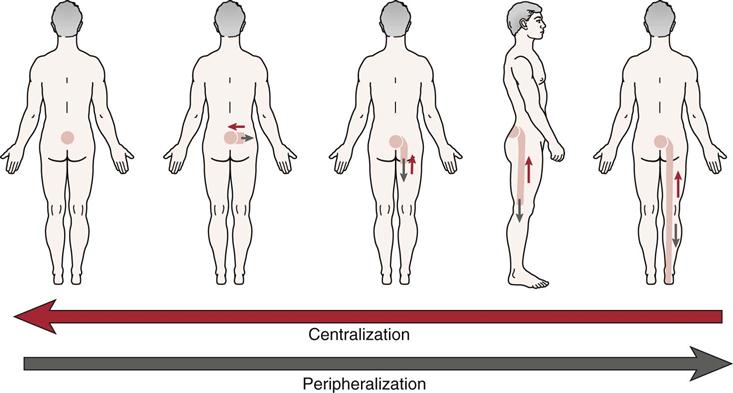
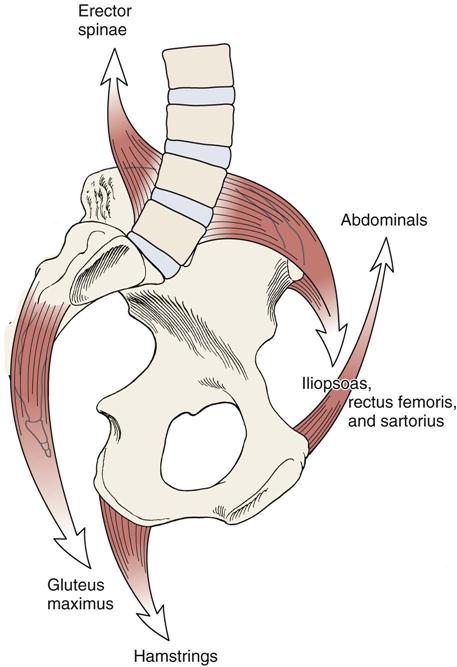
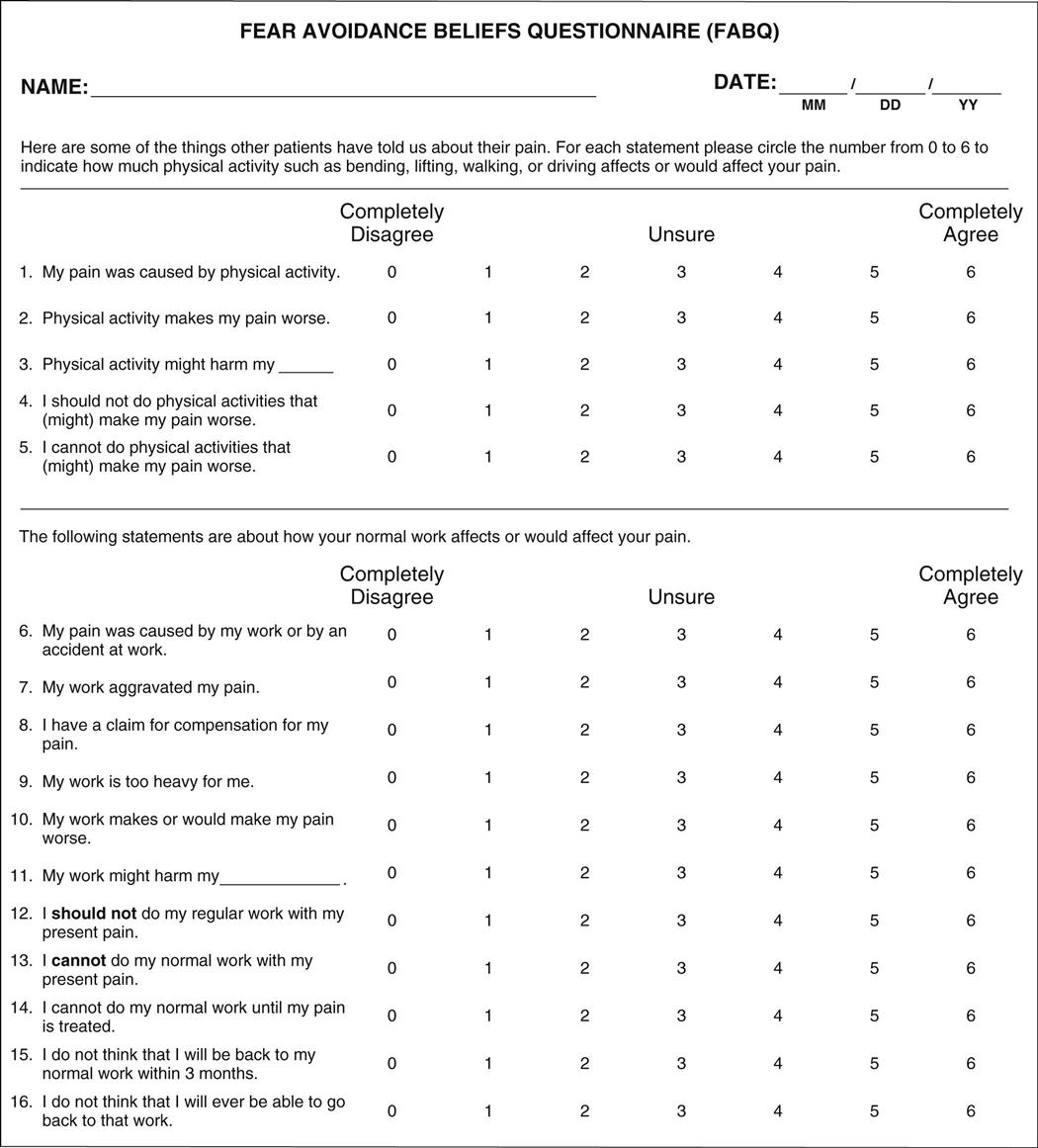
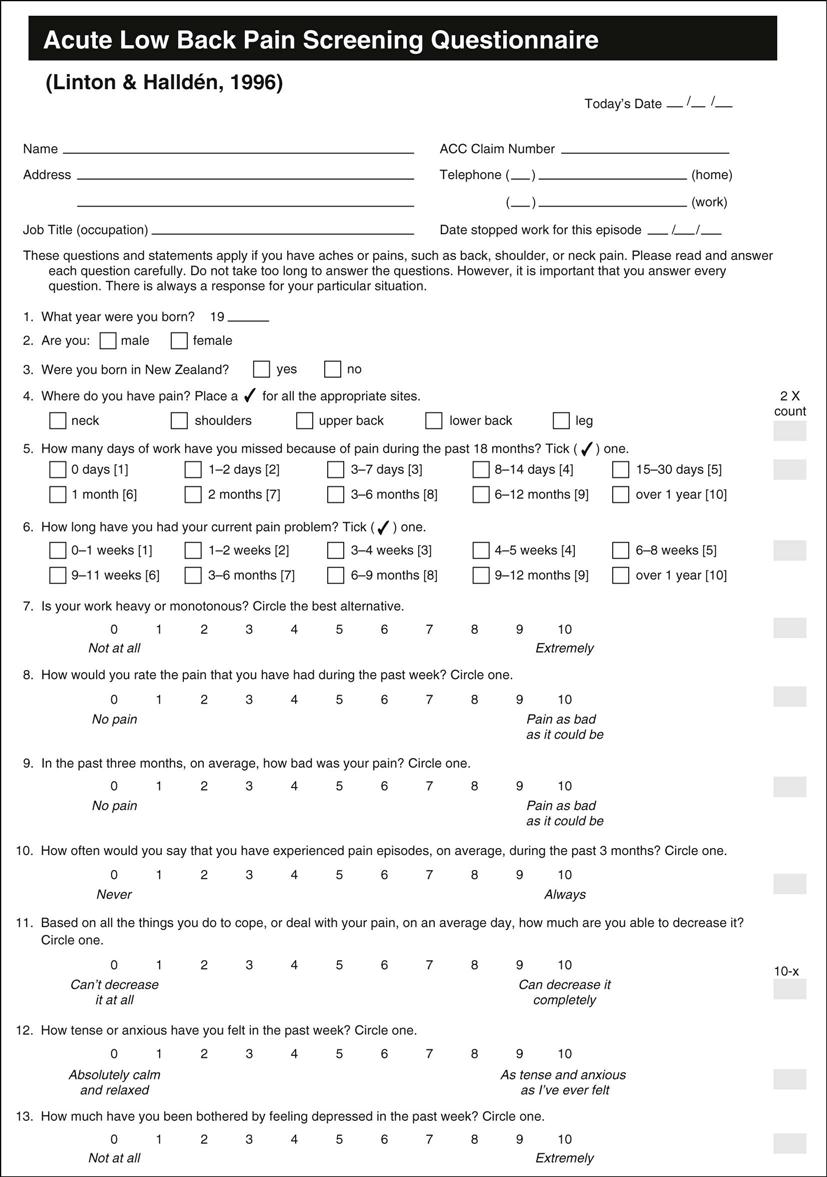
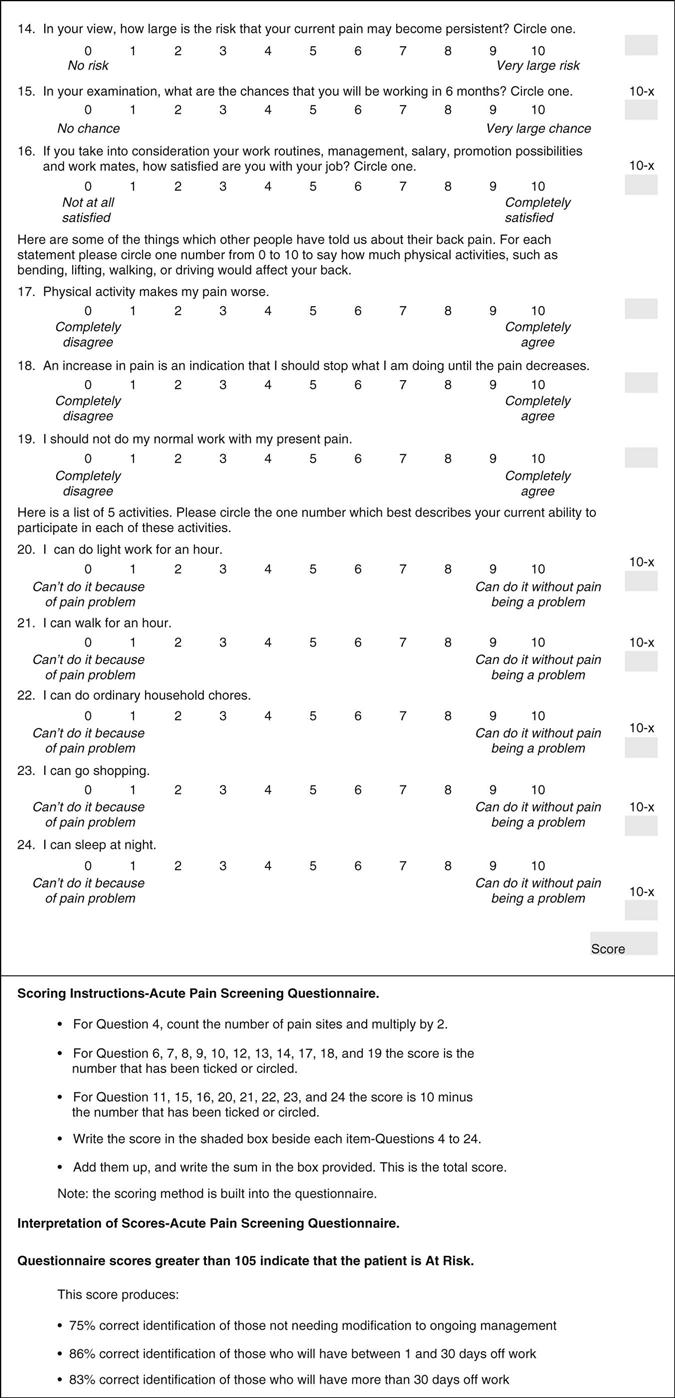

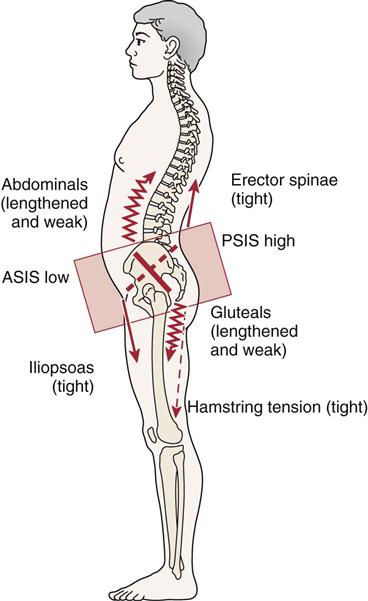
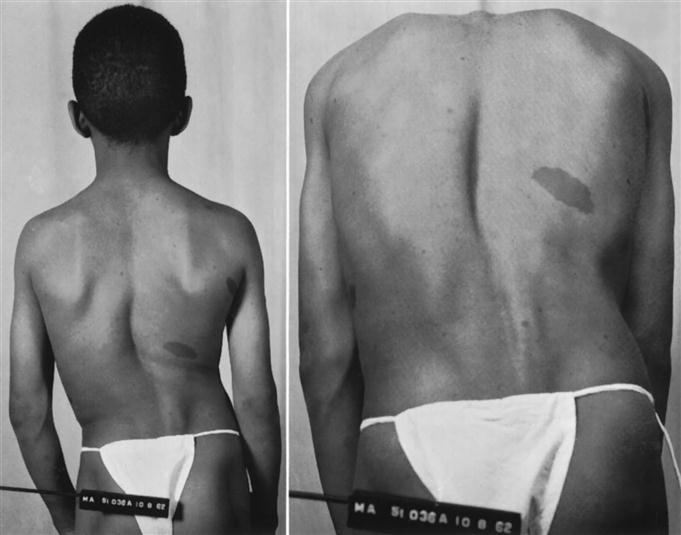
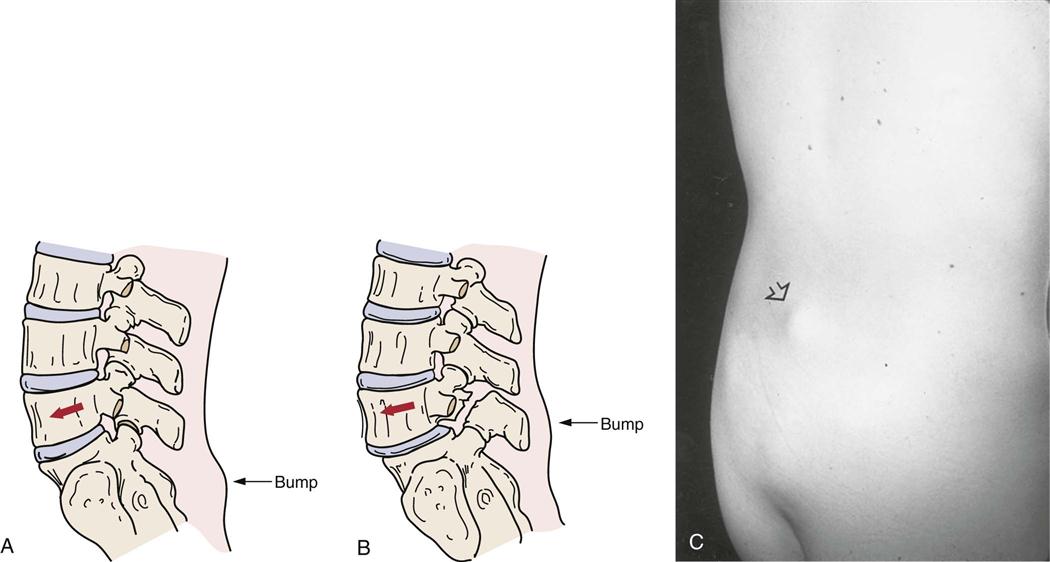
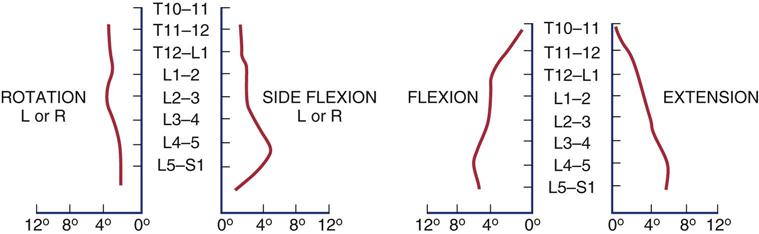
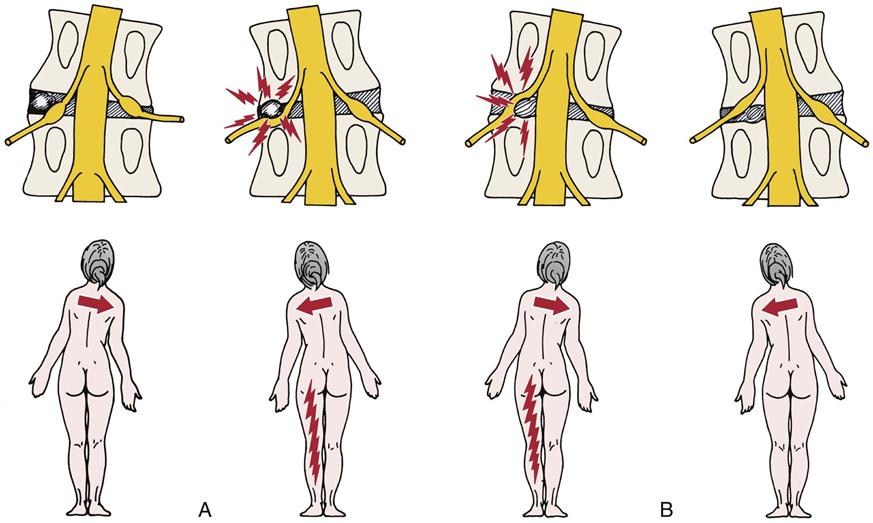
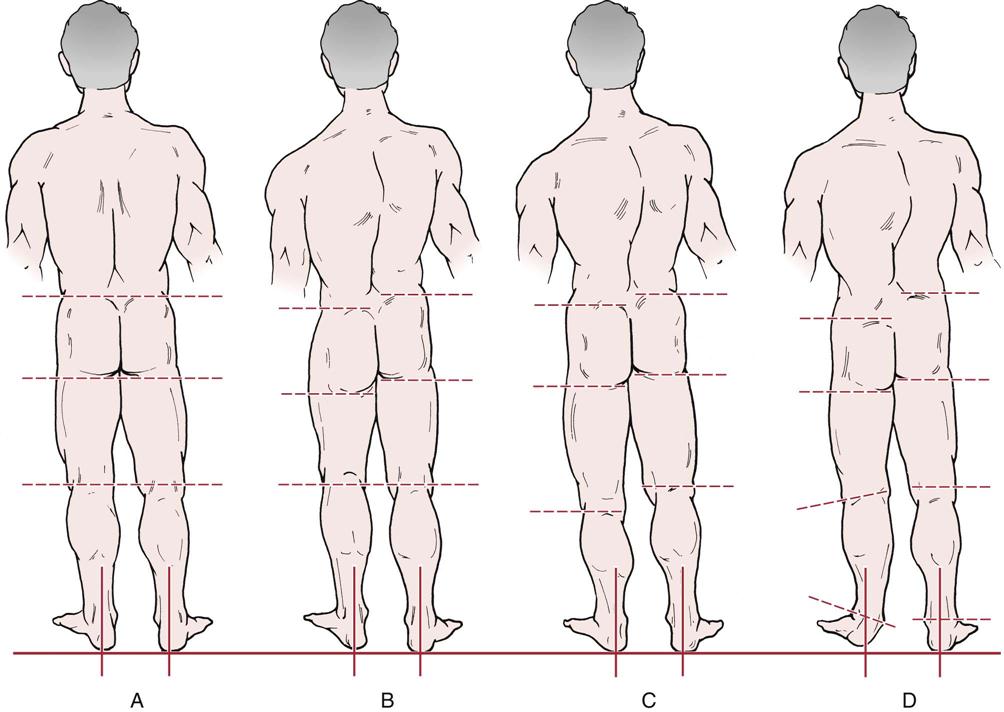
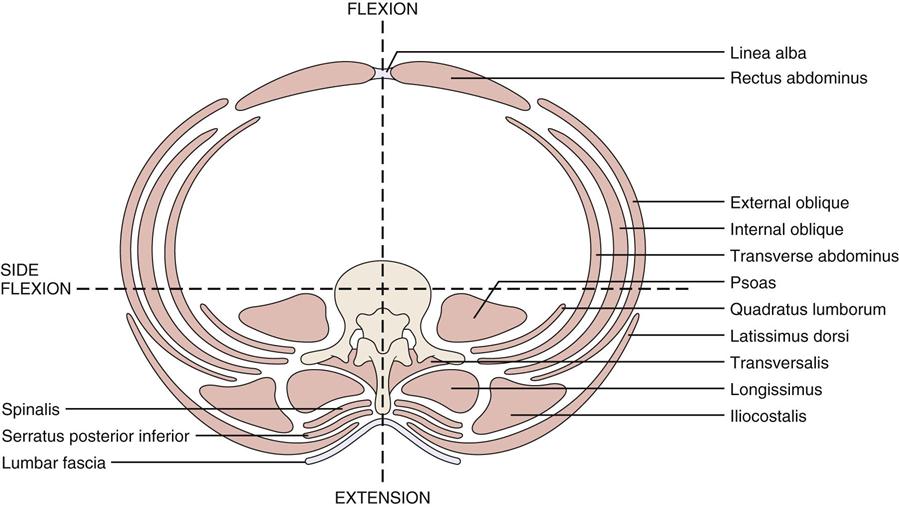
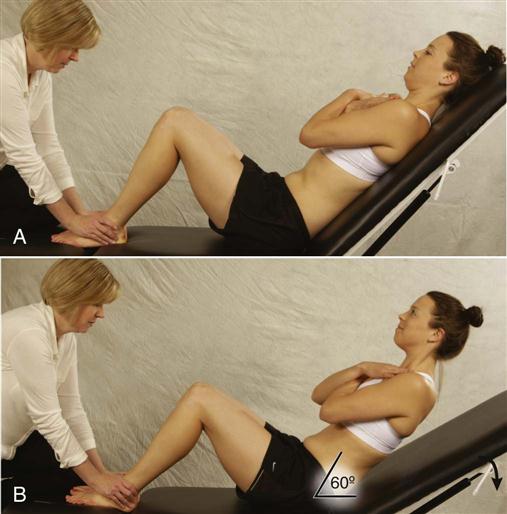
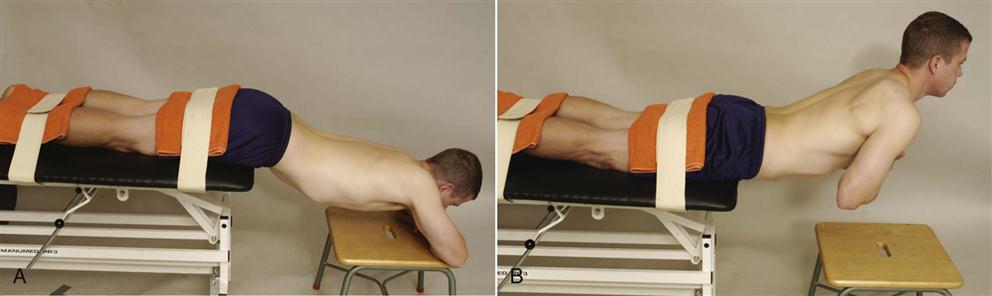
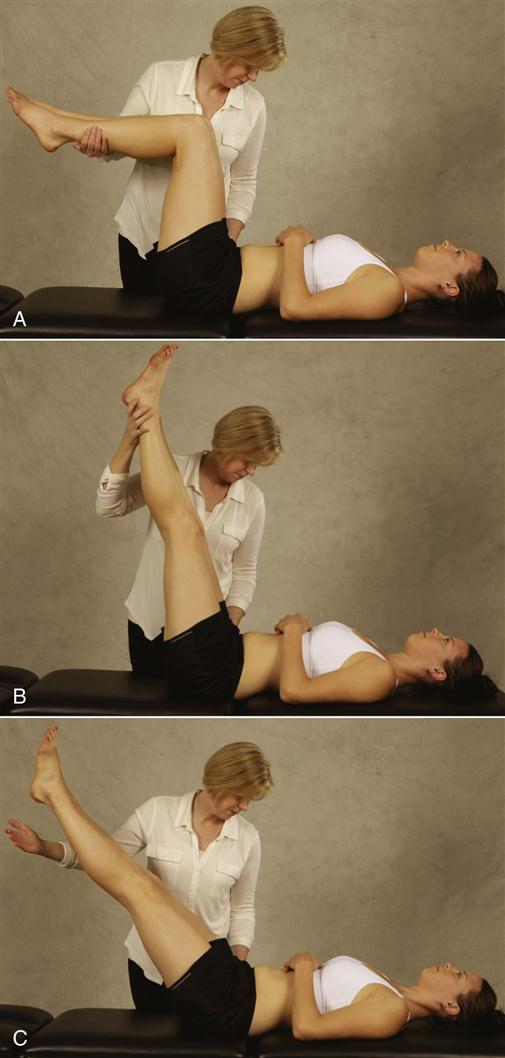
 Figure 9-42
Figure 9-42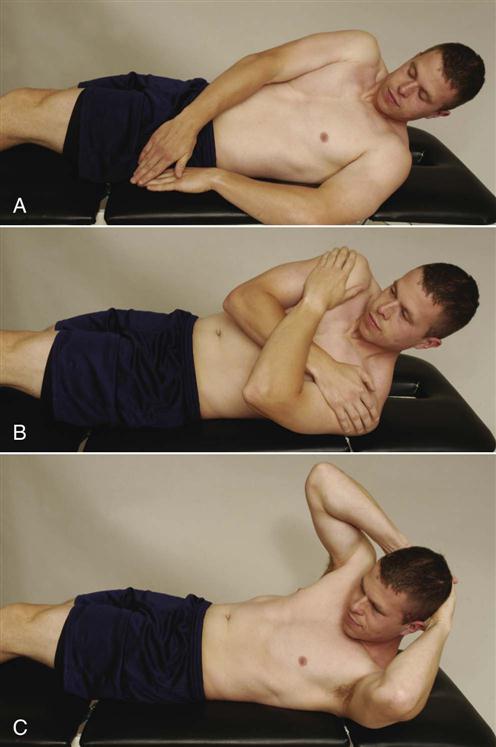
 Figure 9-43
Figure 9-43