Chapter 234 Lumbar Fusion versus Total Disc Arthroplasty for Mechanical Low Back Pain
Fusion
Low back pain is so common a condition that most adults are familiar with its symptoms. The majority of patients suffer from the acute or subacute varieties of low back pain and require only minimal intervention. However, about 5% to 10% of patients develop chronic low back pain.1 A substantial body of literature suggests that the outer layers of the lumbar intervertebral disc are the primary tissue involved in mechanical low back pain.2–4 It has been suggested that either abnormal motion or an excessive biomechanical load in the degenerative disc segment results in pain symptoms. Hence, the elimination of these factors by fusion of the affected spinal segment might eliminate pain when nonsurgical treatment has failed to provide sufficient relief.
Fusion Is a Simpler and More Predictable Operation than Total Disc Replacement
If a patient has failed nonsurgical treatment and a diagnostic workup warrants surgery, lumbar fusion has a single goal: to eliminate motion at the affected segment. If the fusion is solid and the patient continues to have pain, the pain is obviously not originating from the fused motion segment. In other words, the surgeon’s rationale for performing the operation was not correct. Recent evidence suggests that motion-sparing procedures are more challenging than fusion.5–10 Implant design, size, precise positioning, status of facet joints, and other variables play significant roles in the outcome of the procedure. In fact, the current literature suggests that the majority of implant-related complications are due to a poor choice of size or position of the implant.11,12 Although current implants are better than their predecessors, they are far from optimal. Mikeal et al. showed that current implants do not fit 98% of the patients. Huang et al. studied the prevalence of contraindications to TDR in a cohort of lumbar surgical patients.13 The authors reviewed 100 consecutive patients who had lumbar surgery carried out by one surgeon in 2002. Contraindications to TDR included central or lateral recess stenosis, facet joint arthrosis, spondylolysis or spondylolisthesis, herniated nucleus pulposus with radiculopathy, scoliosis, osteoporosis, postsurgical pseudarthrosis, or deficiency of the dorsal elements. Patients were divided into fusion or nonfusion groups, and the percentage of patients without contraindications to TDR was calculated. Out of 100 patients, 56 underwent spine fusion and 44 underwent nonfusion surgery. In the fusion group, 56 of 56 (100%) patients had contraindications to TDR. In the nonfusion group, 11% (5 of 44) were considered candidates for TDR. Overall, 5% of patients were considered candidates for TDR. The average number of contraindications to TDR was 2.48 (range, 0–5).
Total Disc Replacement Does Not Provide Greater Improvement of Symptoms and Function
Blumenthal et al. reported the outcomes of the first randomized control trial comparing Charité TDR and ALIF with the BAK cage filled with autograft from iliac crest.14 The study consisted of 304 patients with single-level L4-5 or L5-S1 degenerative disc disease and chronic low back pain. Clinical success was defined as at least 15 points (25%) improvement in Oswestry Disability Index (ODI) scores versus baseline data, no evidence of implant failure, absence of major complications, and maintenance or improvement of neurologic status. There were no differences in operative time, blood loss, or level of surgery between the two treatment groups. Length of hospitalization was significantly shorter in patients with TDR (3.7 vs. 4.2 days, P = .0039). TDR patients also enjoyed statistically greater improvement in visual analogue scale (VAS) and ODI scores at 12 months. However, this difference disappeared at 24 months. The VAS score was 40.6 in the TDR group and 34.1 in the fusion group. The ODI score change at 24 months was 48.5% for the TDR group and 42.4% for the fusion group. Zigler et al. reported the results of a similarly designed randomized clinical trial evaluating Prodisc-L TDR versus ALIF combined with dorsolateral fusion and instrumentation.15 The TDR group experienced statistically significant less intraoperative blood loss, operative time, and length of stay. These results are not surprising, considering that the control group underwent additional dorsal surgery. In contrast to Blumenthal et al.’s study,14 clinical success in Zigler et al.’s study was defined as at least 15% improvement in ODI score. At 24 months, ODI scores were similar in the two treatment groups. The VAS improvements for TDR patients and fusion patients were 39 and 32, respectively. Guyer et al reported on 5-year outcomes of Charité TDR RCT.16 The results showed a 57.8% success rate in the TDR group versus 51.2% in the fusion patients (P = .0359). No statistically significant differences were detected in ODI, VAS pain scores, or 36-Item Short Form Health Survey functional outcomes. However, 65.6% of TDR patients were employed at 5 years after surgery compared to 46.5% of fusion patients (P = .0403). Zindrick et al. performed an extensive review of the TDR literature from 1990 to 2007.17 The majority of studies were excluded, owing to lack of relevant data. The remaining clinical reports (level 3 or 4 evidence) often lacked consistency in outcomes or did not use a control group, precluding any meaningful conclusion. On the basis of available level I and II evidence, TDR does not result in better improvement of symptoms and function even against suboptimal controls.
Total Disc Replacement Maintains or Restores Motion at Affected Segments
McAfee et al. analyzed flexion-extension and translation angles in patients from the Charité IDE study.10 At 24 months, the TDR group demonstrated a 13.6% increase in range of motion compared to baseline. Interestingly, 40% of Charité TDR patients showed 5 degrees of motion less than baseline. These patients were potentially fused at 2 years using Food and Drug Administration criteria (adequate motion = 5 degrees or more; fusion = 5 degrees or less). Zigler et al. reported flexion-extension range of motion of 7.7 ± 4.67 degrees in a Prodisc-L IDE trial.15 Guyer el al. reported no change in range of motion at 5-year follow up.16 Despite these limitations, these results suggest early maintenance of range of motion with TDR.
Total Disc Replacement Maintains or Restores Motion to the Adjacent Segment—Does This Translate to a Decreased Incidence of Adjacent-Level Disease?
Adjacent-level disease is a well-recognized potential consequence of lumbar fusion. Harrop et al. performed a meta-analysis of available literature focusing on adjacent-level disease after fusion and TDR.18 The authors concluded that adjacent-level disease developed in 34% of patients after lumbar fusion and 9% after TDR. Fourteen percent of fusion patients developed clinically significant symptoms related to adjacent-level disease compared to 1% of TDR patients. Using odds ratio analysis, the authors concluded that fusion patients are 4.67 times more likely to develop adjacent-segment disease than TDR patients are. Huang et al. evaluated the relationship between range of motion and adjacent-level disease in patients with TDR. Lateral lumbar radiographs of 42 patients were analyzed.19 The authors defined adjacent-level disease as a loss of motion, disc height narrowing, and osteophyte formation. Ten patients (24%) developed radiographic evidence of adjacent-level disease. These findings correlated with loss of motion at the index TDR level. Putzier et al. reported similar findings in their series.20 These data suggest that the development of adjacent-level disease is greater in patients with lumbar fusion. No level 1 or 2 data are available to address the issue of adjacent-level disease.
Blumenthal S., McAfee P.C., Guyer R.D., et al. A prospective, randomised multi-centre Food & Drug Administration investigational device exemption study of lumbar total disc replacement with the Charité artificial disc versus lumbar fusion. Part I: evaluation of clinical outcomes. Spine (Phila Pa 1976). 2005;30:1565-1575.
Guyer R.D., McAfee P.C., Banco R.J., et al. Prospective, randomized multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: five-year follow up. Spine (Phila Pa 1976). 2009;9:374-386.
Harrop J.S., Youseff J.A., Maltenfort M., et al. Lumbar adjacent segmental degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976). 2008;33:1701-1707.
Huang R.C., Tropiano P., Marnay T., et al. Range of motion and adjacent level degeneration after lumbar total disc replacement. Spine J. 2006;6:242-247.
Zindrick M.R., Tzermiadianos M.N., Voronov L.I., et al. An evidence-based medicine approach in determining factors that may affect outcome in lumbar total disc replacement. Spine (Phila Pa 1976). 2008;33:1262-1269.
1. Thalgott J.S., Albert T.J., Vacaro A.R., et al. A new classification system for degenerative disc disease of the lumbar spine based on MRI, provocative discography, plain radiographs, and anatomic considerations. Spine J. 2004;4(Suppl 6):S167-S172.
2. Aprill C., Bogduk N. High intensity zone: a diagnostic sign of painful lumbar disc on MRI. Br J Radiol. 1992;65(773):361-369.
3. Kuslich S.D., Ulstrom C.L. The tissue origin of low back pain and sciatic: a report of pain response to tissue stimulation during operation on lumbar spine using local anesthesia. Orthop Clin North Am. 1991;22(2):181-187.
4. Weinstein J.W., Claverie W., Gibson S. The pain of discography. Spine (Phila Pa 1976). 1988;13:1344-1348.
5. Buttner-Janz K., Hahn S., Schikora K., et al. Principles for successful application of the Link SB Charité artificial disc. Orthopade. 2002;31:441-453.
6. German J.W., Foley K.T. Disc arthroplasty in the management of the painful lumbar motion segment. Spine (Phila Pa 1976). 2005;30:S60-S67.
7. Huang R.C., Girardi F.P., Cammisa F.P., et al. Correlation between range of motion and outcome after lumbar total disc replacement: 8.6-year follow-up. Spine (Phila Pa 1976). 2005;30:1407-1411.
8. Kurtz S.M., Peloza J., Sisky R., et al. Analysis of a retrieved polyethylene total disc replacement component. Spine (Phila Pa 1976) J. 2005;5:344-350.
9. Lui J., Ebraheim N.A., Haman S.P., et al. Effect of the increase in the height of lumbar disc space on facet joint articulation area in sagittal plane. Spine (Phila Pa 1976). 2006;31:E198-E202.
10. McAfee P.C., Cunningham B., Holsapple G., et al. A prospective, randomized, multi-center food and drug administration investigational device exemption study of total lumbar disc replacement with the Charité artificial disc versus lumbar fusion. Part II: evaluation of radiographic outcomes and correlation of surgical technique accuracy with clinical outcomes. Spine (Phila Pa 1976). 2005;30:1576-1583.
11. Steiber J.R., Donald G.D. Early failure of lumbar disc replacement: case report and review of the literature. J Spinal Disord Tech. 2006;19(1):55-60.
12. Van Ooij A., Oner F.C., Verbout A.J. Complications of artificial disc replacement; a report of 27 patients with the SB Charité disc. J Spinal Disord Tech. 2003;16:369-383.
13. Huang R.C., Lim M.R., Girardi F.P., et al. The prevalence of contraindications to total disc replacement in a cohort of lumbar surgical patients. Spine (Phila Pa 1976). 2004;29:2538-2541.
14. Blumenthal S., McAfee P.C., Guyer R.D., et al. A prospective, randomised multi-centre Food & Drug Administration investigational device exemption study of lumbar total disc replacement with the Charité artificial disc versus lumbar fusion. Part I: evaluation of clinical outcomes. Spine (Phila Pa 1976). 2005;30:1565-1575.
15. Zigler J., Delamarter R., Spivak J.M., et al. Results of prospective randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine (Phila Pa 1976). 2007;32:1155-1163.
16. Guyer R.D., McAfee P.C., Banco R.J., et al. Prospective, randomized multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: five-year follow up. Spine (Phila Pa 1976). 2009;9:374-386.
17. Zindrick M.R., Tzermiadianos M.N., Voronov L.I., et al. An evidence-based medicine approach in determining factors that may affect outcome in lumbar total disc replacement. Spine (Phila Pa 1976). 2008;33:1262-1269.
18. Harrop J.S., Youseff J.A., Maltenfort M., et al. Lumbar adjacent segmental degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976). 2008;33:1701-1707.
19. Huang R.C., Tropiano P., Marnay T., et al. Range of motion and adjacent level degeneration after lumbar total disc replacement. Spine J. 2006;6:242-247.
20. Putzier M., Funk J.F., Schneider S.V., et al. Charité total disc replacement—clinical and radiographic results after an average follow up of 17 years. Eur Spine J. 2006;15:183-195.
Total Disc Arthroplasty
Lumbar Artificial Disc
It has been opined that the fusion of a spine motion segment leads to increased adjacent-segment degenerative changes. The incidence of such changes has been reported to range from 10% to 30%,1–10 which has led to the development and evolution of other treatment modalities for mechanical LBP, including artificial disc replacement. Lumbar artificial disc replacement facilitates the relief of pain by eliminating presumed pain generators (including the annulus fibrosus and nucleus pulposus) while preserving motion, thereby allegedly minimizing the development of adjacent-segment disease.
Lumbar artificial discs can be divided into total disc replacement and partial disc replacement, which is also known as nucleus replacement. The recent explosion in the number of lumbar artificial disc devices was spurred by the development of the first-generation Charité artificial disc by Butner-Janz and Schellnack and the Prodisc-L by Marnay. Lumbar artificial disc devices are categorized in several ways. These devices can be categorized on the basis of their biomechanical properties or on the basis of design of composite materials. Alternatively, they may be categorized on the basis of the number of components that make up the fully assembled device. In general, they are broadly classified as either metal-on-metal or metal-on-polymer (based on composite materials) or as unconstrained, semiconstrained, or constrained (based on biomechanics). An example of an unconstrained device is the Charité. Examples of the unconstrained devices with a fixed center of rotation include the ProDisc, Maverick, and FlexiCore discs. Thus far, the Food and Drug Administration (FDA) has approved several lumbar artificial discs for implantation in the United States. These include the Charité artificial disc (2004), Prodisc-L (2006), and the next generation Charité artificial disc (2007). Other devices are in various stages of development or have received an investigational device exemption from the FDA.
Lumbar Fusion: Advantages and Disadvantages
Prior to the development of lumbar artificial discs, the surgical treatment for mechanical LBP due to degenerative disc disease consisted of arthrodesis of the painful motion segment. Fusion is intended to eliminate painful, nonphysiologic motion across the dysfunctional motion segment. Spine fusion alters the biomechanics of the spine and results in the transmission forces to adjacent vertebral levels, which may lead to accelerated disc degeneration, facet arthropathy, and osteophyte formation. Recurrent back pain and symptomatic spinal stenosis at levels adjacent to the fusion site may result.11–14
Advantages of Lumbar Artificial Disc
Lumbar artificial disc technology, to one degree or another, restores the normal disc space height and preserves physiologic motion rather than eliminating it as fusion does.15–18 A degenerated disc leads to an abnormal joint that is unable to completely support the weight of the body, thereby causing pain with motion. Fusion of the joint eliminates the abnormal motion, thereby theoretically relieving the pain. Artificial lumbar discs preserve motion, restore disc height and lumbar lordosis, and attempt to replicate the normal instantaneous axis of rotation without exerting undue stress on the adjacent segments. Artificial joints are not a new concept in orthopedics as demonstrated by the various widely available artificial hip and knee joints. As technology continually improves, similar success may be encountered in lumbar artificial discs.19
Indications and Contraindications for Lumbar Artificial Discs
• Degenerative disc disease with loss of disc height and dehydration
• Extensive degenerative disc interspace changes
• Intensive annular pathology including high-intensity zones and annular disruption
• Degenerative disc disease with annular pathology, including disc fragment extrusion or containment within the annulus
• Degenerative disc disease or acute disc space collapse after previous microdiscectomy using facet-saving techniques.
The other indications for the implantation of the disc include the following:
• Back pain of discogenic origin with degeneration of a single disc (L5-S1)
• Axial back pain greater than leg/radicular pain
• Radiographic evidence of decreased disc height by 2 mm compared with adjacent (cranial) disc height or (1) translational instability (≥3 mm translation) or (2) angular instability (≥5 degrees).
• A preoperative visual analog scale score for back pain of at least 40/100
• A preoperative Oswestry score of at least 40/100
• Failed conservative treatment for back pain for a minimum of 6 months
Absolute contraindications for implanting a lumbar artificial disc include the following:
• Symptomatic degenerative disc disease at more than one level
• Previous lumbar fusion or bilateral open decompressive procedures
• Compromised vertebral body structure
• Degenerative spondylolisthesis/retrolisthesis >25%
• Spondylolysis with or without spondylolisthesis
• Lumbar scoliosis >15 degrees
• Facet joint disease or degeneration
• Obesity, pregnancy, or allergy to implant materials
• Infection, hepatitis, rheumatoid arthritis, autoimmune diseases, or malignancy.
Relative contraindications to lumbar artificial disc implantation include the following:
• Multilevel pathology with indeterminate source of pain
• Lumbar scoliosis with apical degenerative disc disease
• Translational instability syndromes, including spondylolisthesis and spondylolysis
• Presence of stenosis and subarticular disease and severe facet joint pathology
Lumbar Artificial Disc Design
Lumbar artificial discs are designed to withstand a significant amount of wear and tear. The materials that are used are designed to be biocompatible and not cause an inflammatory reaction when implanted. The artificial disc is designed to replicate the biomechanics of the normal disc and should be able to withstand normal motion, which includes translation and rotation in the x-, y-, and z-axes.
Biomechanics of Lumbar Artificial Discs
Lumbar Artificial Disc Center of Rotation
The center of rotation (COR) of the lumbar spinal motion segment does not move about a single fixed axis of rotation. It moves about an elliptical locus termed the instantaneous axis of rotation.20,21 The instantaneous axis of rotation is generally located within the dorsal half of the disc space in the normal intact spine. In the spine with early degenerative disc disease, the path of the COR lengthens, and as the disc degeneration worsens, the COR migrates caudally. In an in vitro human cadaveric model, the flexibility of the COR of a lumbar artificial disc (SB Charité) was compared to that of conventional threaded fusion cages (e.g., BAK cages) and BAK cages augmented with pedicle screw fixation across a single spinal level.22 The SB Charité prosthesis displayed an increase in axial rotation by 44% compared to the intact lumbar spine. The BAK-only construct and BAK-pedicle-screw construct displayed a 29% and 80% decreased range of motion, respectively. Flexion-extension range of motion was slightly increased for the SB Charité (3%) versus the intact state, while it was decreased with the BAK-only construct and BAK-pedicle-screw construct. According to flexion-extension radiographs, the COR of the Charité device was located in the dorsal one third of the disc space, which was comparable to the intact spine, thereby allowing investigators to theorize that the artificial disc preserved the kinematic properties of the normal intact spine.
Stability of the Implant-Bone Interface
A variety of strategies are employed for anchoring lumbar artificial discs to the vertebral end plates and adjacent vertebral bodies. The initial SB Charité was suboptimally anchored. This might have played a role in early device failure. The device was later modified and reengineered with a porous titanium and an electrochemically bonded calcium hydroxyapatite coating. This facilitated bony in-growth into the end plate. After 6 months follow-up, the range of motion of the SB Charité and intact nonoperative controls under compression, flexion, extension, and lateral bending showed no statistical difference.22 Plain radiographs showed no lucencies or loosening of any component of the prosthesis. Finally, histochemical analysis did not reveal any local or systemic accumulation of particulate wear debris.
Wear Testing
Lumbar artificial discs are relatively new devices, and as such, when compared to artificial hips and knees, little is known about in vivo degradation or the contribution of wear to implant failure. Retrieval studies have shown that clinically relevant wear and polyethylene degradation (metal-polyethylene implants) occur. Chronic inflammatory reactions and wear debris have also been observed in tissue surrounding failed artificial discs. The wear potential of the ProDisc L was determined by using an adaptive finite element technique.23 The testing scheme was validated by using a model of a total hip replacement and was then used to model the ProDisc L. The degree of flexion-extension, lateral bending, axial twist, and axial loading were applied through 10 million simulation cycles. The polyethylene wear rate of the ProDisc L was 9.8 mg/million cycles. The comparable rate for a total hip replacement is 16.1 mg/million cycles.23 Metal-on-metal wear for the Maverick artificial disc has been tested extensively, and there is essentially no metal wear at 31.5 years equivalent of simulated loading.
Surgical Implantation
The majority of the lumbar artificial discs are implanted through a ventral approach, with the notable exception of the Prosthetic Disc Nucleus (RayMedica, Bloomington, MN). Most are implanted via an approach similar to that utilized in performing anterior lumbar interbody fusions (ALIF).24,25 Obviously, there are obligatory device-specific nuances. The implantation technique for the SB Charité III artificial disc (Depuy Spine, Johnson and Johnson, Raynham, MA) is as follows24,25: The lumbar spine is approached via a retroperitoneal approach, usually on the right side. A standard anterior discectomy is performed, with care taken to avoid violating the end plates. The disc space is then distracted with a lamina spreader, followed by end-plate sizing and the actual implantation of the end plate of the prosthesis. It is crucial for the implant to be placed centrally in the disc space. This can be confirmed with anteroposterior fluoroscopy. Next, the polyethylene core is trialed and then implanted. The distracting device is released, and a final confirmatory radiograph is obtained.
ProDisc-L
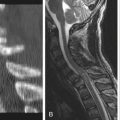
ProDisc-L (Synthes, Paoli, PA; Fig. 234-1) is an artificial disc that has three implant components. It has two cobalt-chrome and molybdenum alloy end plates that are plasma sprayed with titanium. Each has a vertical keel for acute fixation to the vertebral bodies. The rostral component is composed of a solid one-piece design available in two lordotic angles: 6 and 11 degrees. There are two implant sizes, a medium and a large. The medium size is 27 mm in the anteroposterior dimension and 34.5 mm in the lateral-lateral dimension. The large size is 30 mm in the anteroposterior dimension and 39 mm in the medial-lateral dimension. The disc also has a high-molecular-weight polyethylene inlay. The inlay is available in 10-, 12-, and 14-mm sizes. The inlay locks into the caudal end plate. In terms of anatomic sizing, the anteroposterior dimension of each end plate must be at least 28 mm, and the lateral-lateral dimension of the end plate must be at least 35 mm to permit implantation of the ProDisc-L. This can be determined on preoperative axial CT scans.
Charité III Disc
The SB Charité III disc (Fig. 234-2) consists of two cobalt chromium end plates with an intervening ultra-high-molecular-weight polyethylene sliding core. This free-floating core facilitates spacer dynamic shifting within the disc space during normal spinal motion. It moves dorsally in flexion and ventrally in extension. The end plates have anchoring teeth and a titanium/hydroxyapatite coating to enhance fixation to the vertebral body. The dynamic stabilizer of the Charité artificial disc comes in a variety sizes. During implantation, the largest size that the disc space will accommodate is typically inserted. There are various end-plate angles to match the distracted disc space anatomy. The polyethylene core is inserted between the two end plates and comes in a variety of heights. The appropriate size and angles of the end plates are determined intraoperatively, as is the height of the polyethylene core. The Charité lumbar artificial disc is implanted with the metal end plates on the rostral and caudal end plates, with the ultra-high-molecular-weight polyethylene core placed between the two metal end plates. The fact that the core is free floating facilitates replication of normal and natural translation. The concept behind the mobile sliding core of the Charité disc is similar to the mobile knee bearing in many of today’s artificial knee joints.
Maverick Disc
The Maverick (Medtronic Sofamor-Danek, Memphis, TN) total disc replacement is associated with a relatively dorsal center of rotation that mimics that of the normal lumbar motion segment. It has a metal-on-metal cobalt chrome molybdenum design that allows for 16 degrees of motion in all planes. It has a semiconstrained design. This device simulates the intact functional spinal unit in flexion-extension and lateral bending and is stiffer than the intact spinal unit in compression, bending, and rotation. The implant has a keel and has a hydroxyapatite coating on both components that promotes bone growth on the implant. It is designed as a two-piece ball-and-socket joint replacement, with three overall sizes for end plate coverage: 25-, 27-, and 30-mm anteroposterior diameter coverage and 32-, 35-, and 39-mm lateral end-plate coverage. It comes in three dorsal disc heights: 10, 12, and 14 mm. There are three lordosis configurations: 6, 9, and 12 degrees (Fig. 234-3).
FlexiCore Intervertebral Disc
The FlexiCore intervertebral disc (Stryker Spine, Allendale, NJ) is an all-metal total disc replacement device that consists of superior and inferior baseplates that articulate about a centrally located stationary center of rotation. Each baseplate has a central dome that is shaped to approximate the concavity of an adjacent vertebral body end plate. The domes have spikes that facilitate fixation. They are coated with a titanium plasma spray to aid fixation. The baseplates are joined by a central ball-and-socket joint that is set during the manufacturing process to prevent the device from separating under tension loads. The ball-and-socket joint provides ±15 degrees of flexion-extension and lateral bending. This exceeds the natural range of motion without allowing the baseplates to slide. The bearing surfaces of the ball-and-socket components are highly polished cobalt chromium, which allows for a metal-on-metal surface contact that virtually eliminates the creep that is observed with metal-on-polyethylene devices (Fig. 234-4). Sasso et al.26 recently published their experience with the FlexiCore disc.
Kineflex Artificial Disc
The Kineflex artificial disc (SpinalMotion, Inc., Mountain View, CA) has a metal-on-metal design with a semiconstrained core. It is made of cobalt chrome, and the mobile core is seated within a retention ring. The rostral and caudal end plates have multiple serrations in addition to a central fin that allows for keel fixation and initial stability (Fig. 234-5).
Complications of Lumbar Artificial Disc Implants
As one might imagine, the complications associated with artificial discs are similar to those that occur with anterior lumbar interbody fusions. These include facet joint degeneration, unexplained radiculopathy and back pain, extrusion of the implant, facet fracture, and acquired spondylolysis.27,28 Some of these complications have been ascribed to suboptimal device placement, sizing errors, surgical approach errors, inappropriate indications, and problems with patient compliance.29,30 Implant extrusion may be encountered as a result of absence of the anterior longitudinal ligament, which is incised in order to place the implant. Under normal circumstances, this ligament serves to limit excessive extension in the disc space, and when it is excised, excessive lumbar extension may occur. This may increase the risk of implant extrusion.
Revision Strategies for Lumbar Artificial Disc Surgery
McAfee et al.31 report an 8.8% revision rate in a group of 688 patients. As one can imagine, the risks of the anterior surgical approach to the spine are higher in revision surgery. These include visceral injuries and vascular injuries that may occur as a result of increased fragility of the blood vessels due to adhesions. The natural anatomic planes are also ill defined and may lead to difficulty identifying normal anatomy. Most of the visceral injuries may be repaired by primarily suturing the damaged organs. The great vessels lie anterior to the discs above the L5-S1 level, and the bifurcation of the aorta and vena cava lie superior to the L5-S1 disc space, so vascular complications could be devastating and life threatening.32–34 McAfee et al.31 report a 3.6% incidence of vessel injury in primary lumbar artificial disc placement and 16.7% in anterior revision surgery.
Other complications that may be associated with both primary and revision surgery include ureteral injuries and injury to the sympathetic chain, which could lead to both retrograde ejaculation and impotence.35 It is advisable that a vascular surgeon assist in the reoperation approach with the spine surgeon because of the increased risk of complications associated with the exposure. Angiography and venography may also be helpful in identifying any areas of compression of the great vessels. Catheterization of the iliac vessels with inflatable balloon catheters provides the option for intraoperative tamponade of vessels to help prevent significant blood loss. Some surgeons have advocated a transperitoneal or contralateral approach for revision surgery, as it may help to avoid adhesions that result from the initial operation. There has been a lot of recent interest in adhesion prevention and a number of commercially available barriers have been developed to help limit or eliminate adhesions. Some of these materials are nonresorbable; others are resorbable. The nonresorbale barriers function as a permanent mechanical barrier between tissue and are placed at the time of the initial surgery. They can serve as a marker if reoperation is required. An example of this is Gore Preclude (W.L. Gore and Associates, Inc., Flagstaff, AZ). Resorbable barriers may be solid or liquid and can function as both physical and biologic barriers to adhesion formation.36 Examples of the solid resorbable barriers include Interceed R (Ethicon, Somerville, NJ) and Seprafilm (Genzyme, Cambridge, MA). The liquid-based resorbable barriers offer increased ease of application and include Sepracoat (Genzyme), Adcon gels (Wright Medical, Arlington TN), and Intergel (Lifecore Biomedical Inc., Chaska, MN).
Eck J.C., Humphreys S.C., Hodges S.D. Adjacent-segment degeneration after lumbar fusion: a review of clinical, biomechanical, and radiology studies. Am J Orthop. 1999;28:336-340.
Geisler F.H., Blumenthal S.L., Guyer R.D., et al. Neurological complications of lumbar artificial disc replacement and comparison of clinical results with those related to lumbar arthrodesis in the literature: results of a multicenter, prospective, randomized investigational device exemption study of Charité intervertebral disc. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:143-154.
Mummaneni P.V., Haid R.W., Rodts G.E. Lumbar interbody fusion: state of the art technical advances. Neurosurg Spine. 2004;1:24-30.
Rodts G.E., Mummaneni P.V. Discogenic back pain: the case for surgery. Clin Neurosurg. 2004;51:277-280.
Sasso R.C., Foulk D.M., Hahn M. Prospective randomized trial of metal-on-metal artificial lumbar disc replacement: initial results for discogenic pain. Spine (Phila Pa 1976). 2008;33(2):123-131.
Sohn M.J., Kayanja M.M., Kilincer C., et al. Biomechanical evaluation of the ventral and lateral surface shear strain distributions in central compared with dorsolateral placement of cages for lumbar interbody fusion. J Neurosurg Spine. 2006;4:219-224.
Wang J., Mummaneni P.V., Haid R.W. Current treatment strategies for the painful lumbar motion segment: posterolateral fusion versus interbody fusion. Spine (Phila Pa 1976). 2005;30:S33-S43.
1. Eck J.C., Humphreys S.C., Hodges S.D. Adjacent-segment degeneration after lumbar fusion: a review of clinical, biomechanical, and radiology studies. Am J Orthop. 1999;28:336-340.
2. Huang R.C., Tropiano P., Marna T., et al. Range of motion and adjacent level degeneration after lumbar total disc replacement. Spine J. 2006;6:242-247.
3. Lee C.K. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976). 1988;13:375-377.
4. Lehman T.R., Spratt K.F., Tozzi J.E., et al. Long-term follow up of lower lumbar fusion patients. Spine (Phila Pa 1976). 1987;12:97-104.
5. Mummaneni P.V., Haid R.W., Rodts G.E. Lumbar interbody fusion: state of the art technical advances. Neurosurg Spine. 2004;1:24-30.
6. Ozgur B.M., Aryan H.E., Pimenta L., Taylor W.R. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006;6:435-443.
7. Rodts G.E., Mummaneni P.V. Discogenic back pain: the case for surgery. Clin Neurosurg. 2004;51:277-280.
8. Schlegel J.D., Smith J.A., Schleusener R.L. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar and lumbosacral fusions. Spine (Phila Pa 1976). 1996;21:970-981.
9. Sohn M.J., Kayanja M.M., Kilincer C., et al. Biomechanical evaluation of the ventral and lateral surface shear strain distributions in central compared with dorsolateral placement of cages for lumbar interbody fusion. J Neurosurg Spine. 2006;4:219-224.
10. Wang J., Mummaneni P.V., Haid R.W. Current treatment strategies for the painful lumbar motion segment: posterolateral fusion versus interbody fusion. Spine (Phila Pa 1976). 2005;30:S33-S43.
11. Rahm M.D., Hall B.B. Adjacent segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord. 1996;9:392-400.
12. Frymoyer J.W., Durrett C.L. The economics of spinal disorders. In: Frymoyer J.W., editor. The adult and pediatric spine: principles and practice. Philadelphia: Lippincott-Raven; 1997:143-150.
13. Lee C.K., Langrana N.A. A review of spinal fusion for degenerative disc disease: need for alternative treatment approach of disc arthroplasty? Spine J. 2004;4:S173-S176.
14. Lee C.K., Goel V.K. Artificial disc prosthesis: Design concepts and criteria. Spine J. 2004;4:S209-S218.
15. Bao Q.B., McCullen G.M., Higham P.A., et al. The artificial disc: theory, design and materials. Biomaterials. 1996;17:1157-1167.
16. Dooris A.P., Goel V.K., Grosland N.M., et al. Load sharing between anterior and posterior elements in a lumbar motion segment implanted with an artificial disc. Spine (Phila Pa 1976). 2001;26:E122-E129.
17. Eijkelkamp M.F., van Donkelaar C.C., Veldhuizen A.G., et al. Requirements for an artificial intervertebral disc. Int J Artif Organs. 2001;24:311-321.
18. Hedman T.P., Kostuik J.P., Fernie G.R., et al. Design of an intervertebral disc prosthesis. Spine (Phila Pa 1976). 1991;16:S256-S260.
19. Arnold P.M., Kirschman D.L., Meredith C. Prosthetic vertebral disc replacement. In: Vaccaro A.R., Betz R.R., Zeidman Z., editors. Principles and practice of spine surgery. Philadelphia: Mosby; 2003:379-384.
20. Seligman J.V., Gertzbein S.D., Tile M., Kapasouri A. Computer analysis of spinal segment motion in degenerative disc disease with and without axial loading. Spine (Phila Pa 1976). 1984;9(6):566-573.
21. Gertzbein S.D., Seligman J., Holtby R., et al. Centrode patterns and segmental instability in degenerative disc disease. Spine (Phila Pa 1976). 1985;10(3):257-261.
22. Cunningham B.W., Gordon J.D., Dmitriev A.E., et al. Biomechanical evaluation of total disc replacement arthroplasty: an in-vitro human cadaveric model. Spine (Phila Pa 1976). 2003;28(20):S110-S117.
23. Rawlinson J.J., Punga K.P., Gunsallus K.L., et al. Wear simulation of the ProDisc-L disc replacement using adaptive finite element analysis. J Neurosurg Spine. 2007;7(2):165-173.
24. Hochschuler S.H., Ohnmeiss D.D., Guyer R.D., Blumenthal S.L. Artificial disc: preliminary results of a prospective study in the United States. Eur Spine J. 2002;11(Suppl 2):S106-S110.
25. Buttner-Janz K. Optimal minimally traumatic approach for the SB-Charite Artificial Disc. Eur Spine J. 2002;11(Suppl 2):S111-S114.
26. Sasso R.C., Foulk D.M., Hahn M. Prospective randomized trial of metal-on-metal artificial lumbar disc replacement: initial results for discogenic pain. Spine (Phila Pa 1976). 2008;33(2):123-131.
27. Putzier M., Funk J.F., Schneider S.V., et al. Charite total disc replacement: clinical and radiographical results after an average follow-up of 17 years. Eur Spine J. 2006;15:183-195.
28. Van Ooij A., Oner F.C., Verbout A.J. Complications of artificial disc replacement: a report of 27 patients with the SB Charite disc. J Spinal Disord Tech. 2003;16:369-383.
29. Geisler F.H., Blumenthal S.L., Guyer R.D., et al. Neurological complications of lumbar artificial disc replacement and comparison of clinical results with those related to lumbar arthrodesis in the literature: results of a multicenter, prospective, randomized investigational device exemption study of Charite intervertebral disc. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1:143-154.
30. Leary S.P., Regan J.J., Lanman T.H., Wagner W.H. Revision and explantation strategies involving the Charite lumbar artificial disc replacement. Spine (Phila Pa 1976). 2007;32:1001-1011.
31. McAfee P.C., Geisler F.H., Saiedy S.S., et al. Revisability of the CHARITE artificial disc replacement: analysis of 688 patients enrolled in the US IDE study of the CHARITE artificial disc. Spine (Phila Pa 1976). 2006;31:1217-1226.
32. Kulkarini S.S., Lowery G.L., Ross R.E., et al. Arterial complications following anterior lumbar interbody fusion: report of eight cases. Eur Spine J. 2003;12:48-54.
33. Marsicano J., Mirovsky Y., Remer S., et al. Thrombotic occlusion of the left common iliac artery after an anterior retroperitoneal approach to the lumbar spine. Spine (Phila Pa 1976). 1994;19:357-359.
34. Khazim R., Boos N., Webb J.K. Progressive thrombotic occlusion of the left common iliac artery after anterior lumbar interbody fusion. Eur Spine J. 1998;7:239-241.
35. Gayer G., Caspi I., Garniek A., et al. Perirectal urinoma from ureteral injury incurred during spinal surgery mimicking rectal perforation on computed tomography scan. Spine (Phila Pa 1976). 2002;27:E451-E453.
36. Habara T., Nakatsuka M., Konishi H., et al. The biological effects of anti-adhesion agents on activated RAW264.7 macrophages. J Biomed Mater Res. 2002;61:628-633.