Chapter 154 Lumbar Facet Fixation Techniques
The concept of lumbar spine facet fixation has existed since 1948, with King’s description of a novel method of internal fixation in the lumbosacral spine as an alternative to immobilization in plaster.1 This was modified by Boucher in 1959 by using longer screws and slightly altered placement.2 Translaminar placement was introduced in 1984 by Magerl in a paper describing its use as an adjunct to external spinal fixation.3
Anatomy
The capsules of the facet joints are highly innervated. Medial branches from the dorsal rami of the same and often the upper level innervate them, emanating from the neuroforamina. Pain fibers, which are the smallest somatosensory neurons, innervate the capsule. The pain fibers are small myelinated A-delta fibers or unmyelinated C fibers with unencapsulated endings. Studies have demonstrated the presence of pacinian and Ruffini endings, which serve as mechanoreceptors for proprioception and movement sense.4
Biomechanics
In direct axial loading, facet joints bear a relatively small amount of the overall load. However, with extension and hyperextension, they bear a larger portion of the load—approximately 30%, compared with 10% to 20% direct axial loading.5 When flexed, they are reported to handle nearly 50% of the ventral shear load. Because of their motion and distance from the instantaneous axis of rotation, they, along with dorsal ligaments, facilitate the majority of movement in the flexed posture. This opens the joint and stretches the capsule. The capsule is viscoelastic. As such, the elastic zone may diminish over time. Without the ability to return to its neutral state, mobility may increase as the joint capsule is stretched.
Tropism must also be considered. Tropism is manifested by asymmetry in the bilateral facet joints with respect to their angles, with one having a more coronal orientation than the other. The incidence of tropism is increased in degenerative disc disease—perhaps suggesting a contributory factor. The vertebral body rotates toward the more oblique facet with axial loading, possibly leading to increased stress on the anulus fibrosus and accelerated disc degeneration.5
Indications
Adjunct to Noninstrumented Fusions
Pseudarthrosis rates are reported at 10% with bone graft alone during fusion procedures for one level, and possibly greater than 30% with more than two or three levels.6 Internal fixation has been used extensively to assist with fusion procedures in modern spine surgery.7,8 Facet fixation specifically has been shown to decrease pseudarthrosis rates over noninstrumented fusion and to have a low incidence of complications.9
Dorsal fusions were largely supplanted by dorsolateral fusions in the 1980s owing to a decrease in pseudarthrosis rates. Kornblatt et al. also showed that internal fixation, specifically with facet fixation or pelvic rods, improved the rate of fusion (87% vs. 76% without fixation) and time to radiographic fusion (6.2 months vs. 10.5 months) significantly.6 This was also shown by Jacobs et al., using translaminar facet fixation and judging fusion by oblique and flexion-extension films.10 Both studies used patients who had a pseudarthrosis from a prior procedure. They demonstrated that facet fixation can promote fusion after failed procedures—with the caveat that outcomes deteriorate with each successive surgery in most spinal procedures.11
Adjunct to Anterior or Posterior Lumbar Interbody Fusion
One of the uses that has caused a resurgence in facet screw popularity is as an adjunct to anterior lumbar interbody fusion (ALIF), when there is no need for posterior nerve root decompression. Failure of fusion with ALIF alone has been reported in up to 24% of cases.12,13 Cadaveric studies have shown that ALIF alone allows more movement during extension with little preload than does the preoperative spine—a risk for graft displacement and poor fusion. Facet fixation with translaminar screws enhances stability, returning motion to the level allowed preoperatively.14 Kandziora et al. showed the equivalence of ipsilateral facet screws to translaminar screws with regard to range of motion, neutral zone, and elastic zone.15 However, they also demonstrated improved parameters in all test modes with pedicle screws.
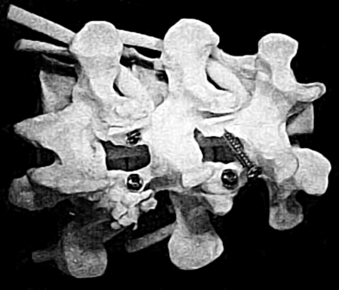
For similar reasons, facet screws are also used as an adjunct to posterior lumbar interbody fusion; this was described as early as 1988, with only 1 complication in 35 patients and fusion apparent in all with the use of postoperative thoracolumbosacral orthosis immobilization.16 This procedure is useful to enhance fusion acquisition and prevent motion that may lead to graft displacement. With posterior lumbar interbody fusion, no further surgical exposure is necessary to place the screws (Fig. 154-1).
Painful Disc Syndromes
The theory behind posterior lumbar fusion for degenerative disc disease is elimination of motion at the affected segment. Outcomes have been shown to be equivalent to interbody procedures in multiple studies.17,18 It is thought that the painful portion of the segment is the disc as a whole or the anulus fibrosus and, therefore, dorsal fusion alone may yield poor outcomes unless the disc material is removed, such as with an interbody procedure (see earlier discussion). However, dorsal fusion alone has significant advantages, such as shorter operative time, less risk for complication, lower cost, preservation of the anterior column, and ease of procedure.
Painful Facet Syndrome
In the healthy spine, the nociceptors in the facet joint capsule fire only under supranormal physiologic conditions. However, it has been shown that with inflammation, chemical mediators can sensitize the pain sensors to fire excessively or spontaneously. One study suggested that 15% of patients with low back pain had pain of facet origin.19 In patients with lumbar facet syndrome, Helbig and Lee demonstrated a positive response to facet block and facet rhizolysis in 50% to 60% of cases.20
The existence of the so-called facet syndrome is still rather controversial. In 1996, Cavanaugh et al. showed in rabbits that algesic chemicals, such as carrageenan or substance P, can sensitize pain receptors or induce persistent firing of these neurons with small movements.4
Results of studies examining the therapeutic potential of facet injections have been contradictory, with some showing significant improvement and others showing equivalent results with the injection of normal saline.21 Once nonsurgical treatment has been exhausted, facet fixation can eliminate motion at the segment, thereby decreasing or eliminating pain.
Translaminar Facet Screws
Technique
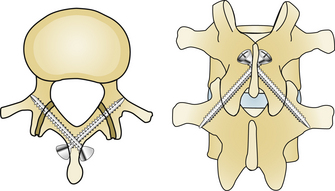
The first description of the translaminar approach was by Magerl in 1984.3 However, the topic of the paper was actually an external fixator and the method of placing facet screws was only vaguely referenced. Diagrams in the article clearly show the path of a translaminar facet screw: entering at the base of the spinous process, traveling the length of the contralateral lamina, crossing the facet joint, and ending at the base of the transverse process (Fig. 154-2). Multiple authors have described percutaneous translaminar screw placement using fluoroscopy.22,23
Comparison with Other Internal Fixation Techniques
However, translaminar placement does require intact dorsal elements. Many surgeons have reported discectomy, lateral recess decompression, and even partial central decompression with preservation of sufficient lamina to perform the translaminar approach, according to Jacobs et al.10 An isthmic spondylolisthesis with a pars defect is therefore an obvious contraindication to this procedure.
Concern also exists regarding the notion that a limited dorsal fusion has the potential for kyphosis over time, as the disc loses height. In addition, although improved pseudarthrosis rates are reported compared with uninstrumented fusion, the rate remains as high as 9% in some reports.10
Comparison with Pedicle Screws
There are some obvious advantages to the facet fixation technique over the more frequently used pedicle screw fixation technique: lower cost, less dissection, more room for bone graft, lower complication rates, and a lower rate of infection. The attraction of the pedicle screw technique is related to the prevailing notion that facet fixation is less stable. Studies have shown equivalence in biomechanics and stability between the two methods in objective tests, although most such studies have been performed in cadaver models.23–25 In a prospective study of patients undergoing translaminar facet fixation versus pedicle fixation, Tuli et al. demonstrated a higher nonunion rate, as confirmed by radiographs, in patients undergoing facet fixation: 17.5% versus 2.7%. This finding correlated with symptoms. However, they also found a non–statistically significant difference in end-fusion degeneration, with pedicle screws having the higher rate (13.5% vs. 5%).26
Pedicle screw fixation requires the insertion of more hardware because of the presence of rods connecting the inserted screws, as well as cross bars. This bulk and higher profile may be one of the reasons that hardware removal is more common after pedicle screw than facet screw insertion. In a comparison with pedicle screws in circumferential interbody fusion, Best and Sasso found that less than 5% of the facet screw group had reoperations due to continued pain, whereas 37.5% of the pedicle screw group returned for another procedure.27 As an aside, one of the facet screw patients who was found to have a pseudarthrosis underwent pedicle screw placement without removal of the facet screws.
Ipsilateral Insertion of Facet Screws
Technique
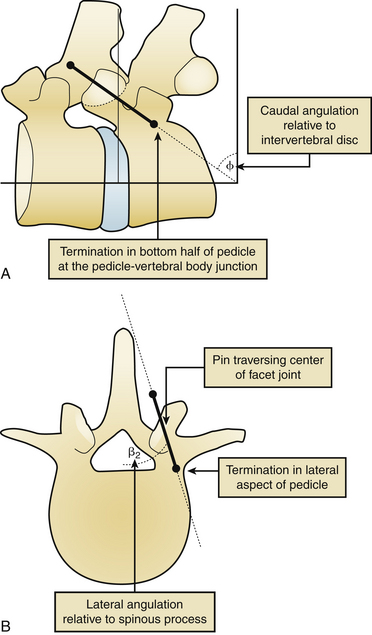
Ipsilateral insertion of facet screws has the advantage of not requiring an intact lamina and spinous process, as does the translaminar approach. In 2009, Su et al. analyzed 80 cadaveric facet joints from 37 spines in an anatomic study of appropriate screw placement.28 The study was designed to determine the radiographic characteristics during percutaneous screw placement that would be expected to traverse the center of the facet joint without complications. They stated that the L2-3 segment could not be instrumented in this fashion because of the vertical orientation of the facet joint. For segments L3 through S1, they observed an appropriate orientation in the mediolateral and craniocaudal planes at each level. Rostrocaudally, the screw trajectory should begin over the caudal end plate of the rostral level. Mediolaterally, the view should show the screw’s starting point to be located over the medial border of the pedicle.
The angle of the screw should be approximately 15 degrees in the axial plane and approximately 30 degrees in the sagittal plane—varying slightly depending on the levels being fused (Fig. 154-3). Another technique orients the screw such that it is parallel to the caudal edge of the lamina.29 The tip of the screw should end up caudally and laterally in the caudal pedicle on the anteroposterior view, and in the caudal half of the pedicle on the lateral view. Su et al. also state that a 35-degree oblique angle on fluoroscopy is optimal for viewing final placement.28
Comparison with Translaminar Screws
The initial impetus for developing ipsilateral screws was to eliminate the long path of translaminar screws and the requirement for intact dorsal elements (spinous process and laminae). Multiple studies have shown equivalence between ipsilaterally placed screws and translaminar screws.15
Comparison with Pedicle Screws
Although facet screws have always been considered inferior to traditional pedicle screw fixation in rigidity and stability, data suggest that ipsilateral facet screw placement may be equivalent biomechanically. In cadaveric models, Ferrara et al. conducted short- and long-term cyclical testing of facet screws and pedicle screws with flexion-compression and torsional loading. Although the two systems were equal in most parameters assessed, they found facet screws provided 30% more stiffness during flexion in short-term cycling. Agarwala et al. performed another cadaver model study showing that the Boucher method of facet screw placement demonstrated a trend toward reduced motion compared to pedicle screws in flexion extension, but not in lateral bending or axial rotation.30 This trend was only shown in primary fusion procedures without ALIF, and did not meet statistical significance. Although performed in vitro, these studies provide support for the theory that facet fixation may be equivalent in stability to pedicle screw fixation and able to maintain its mechanical integrity over long-term cycling.29
Pins
Although no extensive investigation into the use of pins rather than screws to fixate lumbar facets has been performed, Deguchi et al. compared pedicle screw fixation, translaminar screw fixation, and a translaminar technique using bioabsorbable poly-l-lactide pin placement.31 Sheep cadaveric spines were used. Pin placement resulted in restricted motion compared with the intact spine. However, both pedicle screw fixation and translaminar screw fixation provided greater stiffness and rigidity.
Conclusion
The concept of facet fixation is not new. It has been relatively usurped by the technique of pedicle fixation. However, pedicle screws do have serious drawbacks, including higher cost. Also, because of their trajectory and level of skill required for placement, risk of neurologic injury and the need for hardware removal are increased. Pedicle screws require more dissection and, therefore, longer operative times and increased risk for infection. However, although percutaneous pedicle screw insertion has been investigated,32 the placement procedure of open cases is well known. Many spine surgeons are more familiar with this than placement of facet screws.
Overall, the outcomes for facet fixation compare favorably with other methods of fixation. At 10-year follow-up, Aepli et al. reported that 74% of patients stated that their translaminar facet fixation “helped” or “helped a lot”—results comparable with pedicle screw fixation outcomes.33 There are some data showing that disc height significantly less than normal may be a positive predictor for a good outcome.34 There are obvious advantages to this fixation technique and, although not suitable for all situations, it is a valuable technique in the armamentarium of spine surgeons.
Aebi M., Arlet V., Webb J. AO spine manual. Stuttgart: Thieme; 2007.
Kornblatt M.D., Casey M.P., Jacobs R.R. Internal fixation in lumbosacral spine fusion: a biomechanical and clinical study. Clin Orthop Relat Res. 1986;203:141-150.
Prothero S.R., Parkes J.C., Stinchfield F.E. Complications after low-back fusion in 1000 patients: a comparison of two series one decade apart. 1966. Clin Orthop Relat Res. 1994;306:5-11.
1. King D. Internal fixation for lumbosacral fusion. J Bone Joint Surg [Am]. 1948;30:560-565.
2. Boucher H.H. A method of spinal fusion. J Bone Joint Surg [Br]. 1959;41:248-259.
3. Magerl F.P. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984;189:125-141.
4. Cavanaugh J.M., Ozaktay A.C., Yamashita H.T., et al. Lumbar facet pain: biomechanics, neuroanatomy and neurophysiology. J Biomech. 1996;29:1117-1129.
5. Aebi M., Arlet V., Webb J. AO spine manual. Stuttgart: Thieme; 2007.
6. Kornblatt M.D., Casey M.P., Jacobs R.R. Internal fixation in lumbosacral spine fusion: a biomechanical and clinical study. Clin Orthop Relat Res. 1986;203:141-150.
7. Prothero S.R., Parkes J.C., Stinchfield F.E. Complications after low-back fusion in 1000 patients: a comparison of two series one decade apart. 1966. Clin Orthop Relat Res. 1994;306:5-11.
8. Thompson W.A., Ralston E.L. Pseudarthrosis following spine fusion. J Bone Joint Surg [Am]. 1949;31:400-405.
9. Heggeness M.H., Esses S.I. Translaminar facet joint screw fixation for lumbar and lumbosacral fusion: a clinical and biomechanical study. Spine (Phila Pa 1976). 1991;16(Suppl 6):S266-S269.
10. Jacobs R.R., Montesano P.X., Jackson R.P. Enhancement of lumbar spine fusion by use of translaminar facet joint screws. Spine (Phila Pa 1976). 1989;14:12-15.
11. Waddell G. Evaluation of results in lumbar spine surgery: clinical outcome measures—assessment of severity. Acta Orthop Scand Suppl. 1993;251:134-137.
12. Tiusanen H., Hurri H., Seitsalo S., et al. Functional and clinical results after anterior interbody lumbar fusion. Eur Spine J. 1996;5:288-292.
13. Wang X., Chen Y., Chen D., et al. Anterior decompression and interbody fusion with BAK/C for cervical disc degenerative disorders. J Spinal Disord Tech. 2009;22:240-245.
14. Phillips F.M., Cunningham B., Carandang G., et al. Effect of supplemental translaminar facet screw fixation on the stability of stand-alone anterior lumbar interbody fusion cages under physiologic compressive preloads. Spine (Phila Pa 1976). 2004;29:1731-1736.
15. Kandziora F., Schleicher P., Scholz M., et al. Biomechanical testing of the lumbar facet interference screw. Spine (Phila Pa 1976). 2005;30:E34-E39.
16. Stonecipher T., Wright S. Posterior lumbar interbody fusion with facet-screw fixation. Spine (Phila Pa 1976). 1989;14:468-471.
17. Fritzell P., Hagg O., Wessberg P., et al. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976). 2002;27:1131-1141.
18. McCulloch J.A. Uninstrumented posterolateral lumbar fusion for single level isolated disc resorption and/or degenerative disc disease. J Spinal Disord. 1999;12:34-39.
19. Schwarzer A.C., Aprill C.N., Derby R., et al. Clinical features of patients with pain stemming from the lumbar zygapophysial joints: is the lumbar facet syndrome a clinical entity? Spine (Phila Pa 1976). 1994;19:1132-1137.
20. Helbig T., Lee C.K. The lumbar facet syndrome. Spine (Phila Pa 1976). 1988;13:61-64.
21. Lilius G., Laasonen E.M., Myllynen P., et al. Lumbar facet joint syndrome: a randomised clinical trial. J Bone Joint Surg [Br]. 1989;71:681-684.
22. Shim C.S., Sh L.e.e., Jung B., et al. Fluoroscopically assisted percutaneous translaminar facet screw fixation following anterior lumbar interbody fusion: technical report. Spine (Phila Pa 1976). 2005;30:838-843.
23. Jang J.S., Lee S.H. Clinical analysis of percutaneous facet screw fixation after anterior lumbar interbody fusion. J Neurosurg Spine. 2005;3:40-46.
24. Eskander M., Brook D., Ordway N., et al. Analysis of pedicle and translaminar facet fixation in a multisegment interbody fusion model. Spine (Phila Pa 1976). 2007;32:E230-E235.
25. Burton D., McIff T., Fox T., et al. Biomechanical analysis of posterior fixation techniques in a 360 degrees arthrodesis model. Spine (Phila Pa 1976). 2005;30:2765-2771.
26. Tuli J., Tuli S., Eichler M.E., et al. A comparison of long-term outcomes of translaminar facet screw fixation and pedicle screw fixation: a prospective study. J Neurosurg Spine. 2007;7:287-292.
27. Best N.M., Sasso R.C. Efficacy of translaminar facet screw fixation in circumferential interbody fusions as compared to pedicle screw fixation. J Spinal Disord Tech. 2006;19:98-103.
28. Su B.W., Cha T.D., Kim P.D., et al. An anatomic and radiographic study of lumbar facets relevant to percutaneous transfacet fixation. Spine (Phila Pa 1976). 2009;34:E384-E390.
29. Ferrara L.A., Secor J.L., Jin B.H., et al. A biomechanical comparison of facet screw fixation and pedicle screw fixation: effects of short-term and long-term repetitive cycling. Spine (Phila Pa 1976). 2003;28:1226-1234.
30. Agarwala A., Bucklen B., Muzumdar A., et al. Do facet screws provide the required stability in lumbar fixation? A biomechanical comparison of the Boucher technique and pedicular fixation in primary and circumferential fusions. Clin Biomech. 2012;27(1):64-70.
31. Deguchi M., Cheng B.C., Sato K., et al. Biomechanical evaluation of translaminar facet joint fixation: a comparative study of poly-l-lactide pins, screws, and pedicle fixation. Spine (Phila Pa 1976). 1998;23:1307-1312.
32. Foley K.T., Gupta S.K., Justis J.R., et al. Percutaneous pedicle screw fixation of the lumbar spine. Neurosurg Focus. 2001;10(4):E10.
33. Aepli M., Mannion A.F., Grob D. Translaminar screw fixation of the lumbar spine: long-term outcome. Spine (Phila Pa 1976). 2009;34:1492-1498.
34. Hägg O., Fritzell P., Ekselius L., et al. Predictors of outcome in fusion surgery for chronic low back pain: a report from the Swedish Lumbar Spine Study. Eur Spine J. 2003;12(1):22-33.