The big picture203
13.2 Hip joint, gluteal region and upper thigh205
13.3 Knee joint, movements, muscles, posterior thigh, popliteal fossa213
13.4 Ankle joint and movements: posterior, anterior and lateral compartments of leg217
13.5 Foot222
13.6 Venous drainage of the lower limb225
13.7 Innervation, nerve testing, surface anatomy226
13.1. The big picture
First, some words of caution.
Parts of this chapter assume that you have already studied the upper limb. When comparing the lower limb with the upper, there are some potentially confusing issues that you need to keep in mind:
• Thigh, leg. ‘Thigh’ means lower limb from groin to knee. ‘Leg’ means knee to ankle, not the entire lower limb.
• Lateral, medial, tibial, fibular. In the lower limb, unlike the upper limb, lateral and medial are unambiguous. Nevertheless, in the leg, the terms tibial (medial) and fibular or peroneal (lateral) are also used.
• Anterior, posterior, flexors, extensors. During development, the lower limb rotates medially so that muscles and skin supplied by anterior divisions of ventral rami become medial (above the knee) or posterior (below the knee), and muscles and skin supplied by posterior divisions come round to be lateral and in front. So, extensors are at the front, flexors at the back, the knee points forwards (not backwards like the elbow) and the dorsum of the foot is at the front, not the back.
• Peroneal (from Greek) and fibular (from Latin) are synonymous. Peroneus and peroneal are used by many older books but are increasingly being replaced by fibularis and fibular. If you use peroneal, spell it correctly: perineal means something else altogether.
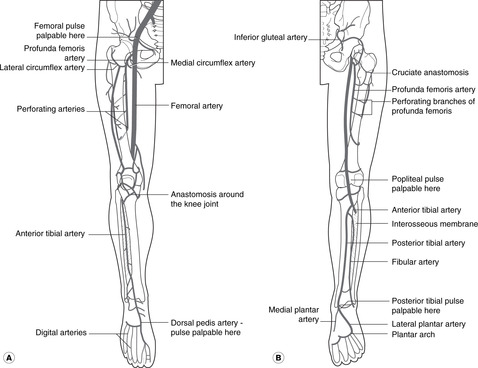
Arteries (see Fig. 7.1, p. 44; Fig. 13.1)
Arterial blood to the lower limb comes from the femoral artery and its branches, with the gluteal arteries (from the internal iliac) supplying the gluteal region.
• Femoral. This is the principal artery to the lower limb. It enters the thigh behind the midpoint of the inguinal ligament and descends into the popliteal fossa where it becomes the popliteal.
• Profunda femoris. The profunda femoris is an early branch of the femoral. It supplies the thigh and gives a series of branches which encircle the femur and contribute to the supply of the hip joint.
• Popliteal. At the lower border of the popliteal fossa the popliteal artery divides into anterior and posterior tibial arteries.
• Anterior tibial. This descends in the anterior (extensor) compartment becoming the:
• Dorsalis pedis artery of the foot.
• Posterior tibial. This descends in the posterior (flexor) compartment, entering the foot posteromedial to the ankle and dividing into:
• Medial and lateral plantar arteries. The lateral plantar anastomoses with the continuation of the dorsalis pedis that passes into the sole between the first (big toe) and second metatarsals.
Palpable pulses. These are the femoral, popliteal, dorsalis pedis, and posterior tibial.
Veins, deep fascia, fascia lata (see Fig. 7.2, p. 45)
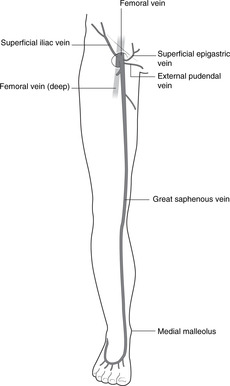
Venous blood drains to the femoral vein, thence to the external iliac and inferior vena cava. As in the upper limb there are deep and superficial systems.
• Superficial veins are immediately subcutaneous, superficial to the deep fascia. Although the pattern of superficial veins is variable, one is particularly important: the great (or long) saphenous vein (saphenous: from Greek, meaning visible), which empties into the femoral vein by passing through a defect in the deep fascia at the top of the thigh, the saphenous opening. Note that the deep fascia of the thigh is called the fascia lata.
• Deep veins accompanying the arteries (venae comitantes) converge to form the popliteal vein, which in turn becomes the femoral. They receive blood from superficial veins through connections which, since they penetrate the deep fascia, are known as perforating veins, or simply perforators.
Since we stand on our feet, venous return from the lower limb is often against gravity. Venous disease of the lower limb is common and the mechanism of venous return is important. It is dealt with in section 13.6 (p. 225).
Lymph (see Fig. 7.4, p. 46; Fig. 13.2)
All lymph drains to inguinal nodes.
• From the medial side, lymph drains directly to inguinal nodes.
• From the lateral side, lymph drains to the popliteal nodes behind the knee, thence to inguinal nodes.
• From inguinal nodes, lymph passes to external iliac nodes, thence to para-aortic nodes, the cisterna chyli and thoracic duct to the venous system at the origin of the left brachiocephalic vein.
Nerves
• From the lumbar plexus (L1–5): to the anterior and medial thigh – hip flexion and adduction and knee extension. Revise the lumbar plexus (Fig. 11.26, p. 134).
• Dermatomes and myotomes. As in the upper limb, the muscles and skin supplied by one segmental nerve are not adjacent as in the trunk. The dermatomes (sensory) are shown in Figure 6.6 (p. 36).
13.2. Hip joint, gluteal region and upper thigh
The head of the femur articulates with the acetabulum of the hip bone. The hip joint is surrounded by large muscles, bones, joint and ligaments reflecting the forces imposed as a result of our bipedal gait. The blood supply of the joint and the head of the femur is an important consideration in patients with fractured femoral necks. Hip flexion and medial rotation are performed by muscles in and around the femoral region; extension and lateral rotation by posterior muscles (gluteal and hamstrings). The principal nerves in this region are the femoral anteriorly, vulnerable to injury in the femoral triangle, and the sciatic posteriorly, at risk in ill-judged injections and posterior dislocations of the hip.
You should:
• describe the structure of the hip joint and how it may be injured
• describe the blood supply of the joint and head of the femur
• list the principal muscle groups acting on the joint, and their innervation
• describe the structures in the femoral triangle, and the anatomy of femoral hernia
• describe the surface markings of the sciatic and femoral nerves, and the femoral artery in the femoral triangle
• explain the effects of damage to the femoral and sciatic nerves.
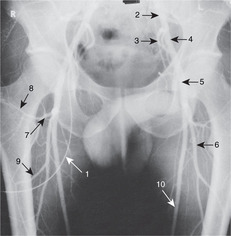
Bones
Sacrum (see Fig. 11.29, p. 137)
• Posterior surface: provides attachment for gluteus maximus, and foramina for dorsal rami of sacral nerves are evident (not important).
• Anterior surface: provides attachment for piriformis, and foramina for ventral rami of sacral nerves are evident.
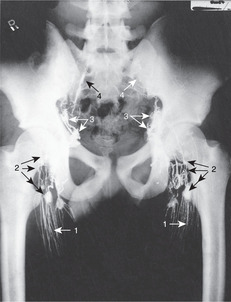
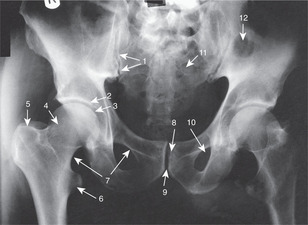
Hip bone (see Fig. 11.29, p. 137; Fig. 13.3)
• Anterior surface of ilium: provides attachment for iliacus which, with psoas from the vertebral column, forms the main hip flexor, iliopsoas.
• Posterior (gluteal) surface of ilium: provides attachment for gluteus medius and gluteus minimus.
• Ischial tuberosity: provides attachment for posterior muscles of the thigh (hamstrings); these extend the hip and flex the knee.
• Pubic symphysis: a midline secondary cartilaginous joint.
• Pubic crest and pecten: provide attachment for pectineus (not important).
• Obturator foramen: this is a large defect closed by membrane in which is a small hole allowing the obturator neurovascular bundle to pass between pelvis and medial thigh.
• Ischiopubic ramus (lower border of obturator foramen formed by ramus of ischium and inferior ramus of pubis): provides attachment for adductor muscles.
• Acetabulum: articular surface for the head of the femur. The acetabular notch allows a branch of the obturator artery to enter the round ligament (ligamentum teres) of the head of the femur, which attaches the femur to the hip bone. The components of the hip bone, the ilium, ischium and pubis, meet in the centre of the acetabulum, the three parts fusing at about 16 years of age.
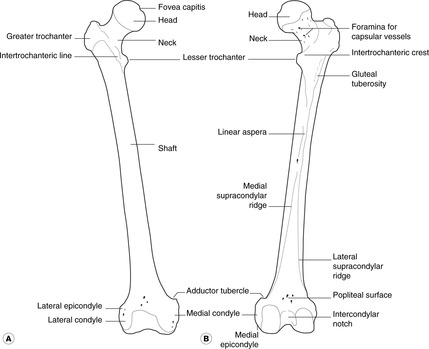
Femur (Fig. 13.4)
• Head: this articulates with the acetabulum. A small pit, the fovea capitis, marks the attachment of the round ligament.
• Neck: note the many small foramina which allow blood vessels to enter the bone.
• Lesser trochanter: for the distal attachment of iliopsoas.
• Greater trochanter: provides attachment for gluteus medius and gluteus minimus.
• Trochanteric line, the ridge on the anterior surface of the femur connecting the two trochanters: the iliofemoral ligament of the hip joint capsule is attached here.
• Trochanteric fossa, between the greater trochanter and the femoral neck: provides attachment for piriformis, obturator externus and obturator internus.
• Gluteal tuberosity, on the posterior aspect of femur: provides attachment for part of gluteus maximus.
• Linea aspera: provides attachment for adductors, vastus muscles and the short head of biceps femoris.
• Adductor tubercle: provides attachment for adductor and vastus muscles.
• Shaft: this is smooth, except for the linea aspera posteriorly.
Hip joint (Fig. 13.5, Fig. 13.6 and Fig. 13.7)
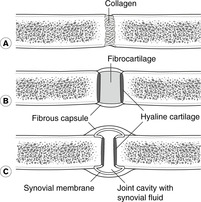
This is a ball and socket synovial joint. The acetabulum is deepened by the acetabular labrum, a rim of hyaline cartilage which, with the transverse acetabular ligament, closes the acetabular notch.
 |
| Fig. 13.6 |
 |
| Fig. 13.7 |
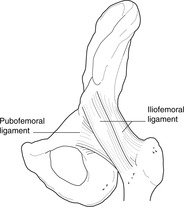
Joint capsule: iliofemoral, pubofemoral and ischiofemoral ligaments (Figs 13.6, 13.7)
The fibrous capsule is attached proximally to the acetabular margin and distally to the intertrochanteric line on the anterior surface of the femur and about halfway up the femoral neck above and behind. Inferiorly, it extends some way down the medial border of the femur to provide sufficient slack capsule which can be taken up on abduction. The fibres of the capsule form three strong ligaments:
• Iliofemoral ligament. Attachments: anterior inferior iliac spine and acetabular margin (proximally)–intertrochanteric line (distally). This strengthens the front of the joint capsule.
Blood supply of head of femur and hip joint: cruciate and trochanteric anastomoses
• Capsular (retinacular) vessels arise from the cruciate and trochanteric anastomoses posterior to the hip joint and neck of the femur. These receive blood from the gluteal and obturator arteries (from the internal iliac), and from circumflex femoral branches of the profunda femoris artery.
• Terminal branches of the nutrient artery from the shaft. In children these do not reach the femoral head, since vessels never cross the epiphyseal plate of developing bone.
• Artery of the round ligament (from the obturator). This is never sufficient to keep the femoral head viable if the other sources of blood are compromised (e.g. in fractures of the femoral neck).
Avascular necrosis of the femoral head may occur after a fracture of the femoral neck. It may also occur in children for reasons that are not entirely clear: this is Perthes’ disease.
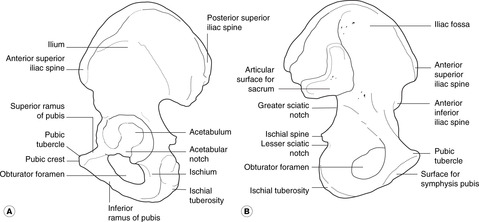
Shenton’s line
On a radiograph, the lower margin of the femoral neck appears to be continuous with the iliopubic ramus (upper margin of the obturator foramen) of the hip. This is Shenton’s line (Fig. 13.5). If it appears to be discontinuous, it is likely that the femoral neck is fractured.
Nerve supply: hip pain and the knee
Branches of femoral, obturator, sciatic and gluteal nerves. Some of these nerves also give branches to the knee joint and pain from the hip may be referred to the knee. So, if you have a patient with pain in the knee, you must exclude disease of the hip.
Flexion and adduction at the hip, femoral triangle, adductor compartment
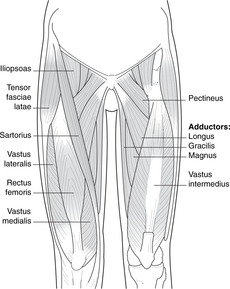
Flexion (Fig. 13.8)
Nerve supply: femoral nerve (L2–4) and direct branches from the lumbar plexus.
• Iliopsoas. Attachments: anterior surface of iliac crest (iliacus) and lumbar vertebral column and discs (psoas)–lesser trochanter. It is the principal flexor supplied directly from the lumbar plexus. It passes deep to the inguinal ligament.
• Sartorius. Attachments: anterior superior iliac spine–medial side of upper end of tibia.
• Pectineus. Attachments: superior border (pecten) of pubis–lesser trochanter with iliopsoas. It also has an adductor role and receives fibres from the obturator nerve as well as the femoral.
 |
| Fig. 13.8 |
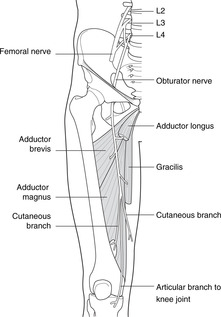
Adduction (Fig. 13.8)
Nerve supply: obturator nerve, L2, 3, 4.
• Adductor longus. Attachments: below pubic tubercle–linea aspera of femur.
• Gracilis (strictly speaking, adductor gracilis). Attachments: inferior ramus of pubis–medial side of tibia.
• Adductor brevis. Attachments: inferior ramus of pubis–linea aspera of femur.
• Adductor magnus. Attachments: ischiopubic ramus–linea aspera and adductor tubercle of femur. Just above the attachment to the adductor tubercle the muscle fibres part to allow the femoral artery and vein to pass between the anterior and posterior compartments: the femoral/popliteal boundary.
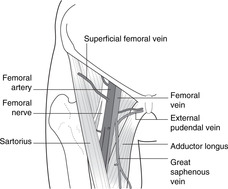
Femoral region (Fig. 13.9)
• At the midpoint of the inguinal ligament, the femoral artery passes from abdomen to thigh. Lateral to it is the femoral nerve and medial the femoral vein. Medial to the vein is:
• The femoral canal – a short extension of the abdominal cavity beneath the inguinal ligament into the thigh. It contains nothing in particular other than a few lymph nodes. Medial to it is:
• The lacunar ligament, an extension of the inguinal ligament which passes on to the superior pubic ramus.
• The femoral ring is the opening of the femoral canal to the abdominal cavity.
• The femoral sheath encloses the canal, the vein and the artery, but not the nerve.
Femoral triangle and vessels (Figs 13.9, 13.10)
• The base of the triangle is the inguinal ligament, the medial border of sartorius laterally, and the medial border of adductor longus medially. Its floor is formed by (from above down) iliopsoas, pectineus and adductor longus.
• The femoral artery passes to the apex of the femoral triangle and then runs for a short distance under sartorius to the gap in adductor magnus where it enters the popliteal fossa. The subsartorial ‘canal’ is also called the adductor or Hunter’s canal.
• The profunda femoris artery arises in the upper part of the femoral triangle and is large, its size reflecting the importance of the thigh muscles and hip joint. It provides a series of arteries that encircle the femur, the uppermost of which, the circumflex femorals, contribute to the cruciate and trochanteric anastomoses supplying the hip joint. The lower branches perforate the fascia between the anterior and posterior thigh muscles and are known as perforating arteries (not to be confused with perforating veins joining the deep and superficial venous systems).
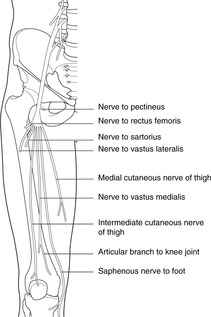
Femoral and obturator nerves (Figs 13.11, 13.12)
• The femoral nerve enters the thigh immediately lateral to the femoral pulse at the inguinal ligament. It divides into numerous branches:
– to knee extensors
– medial and intermediate cutaneous nerves of the thigh (the lateral cutaneous is a separate nerve, see Fig. 11.26, p. 134)
– saphenous nerve (sensory), which continues through the subsartorial canal and then becomes superficial, running down the medial side of the lower thigh and leg with the great saphenous vein to the foot. It supplies a strip of medial skin over and around it and thus a branch of the femoral nerve carries L4 fibres all the way to the foot.
• The obturator nerve enters the thigh through the obturator foramen and supplies:
– hip adductor muscles
– skin of the upper medial thigh
– sensory fibres to the knee joint.
• Both femoral and obturator nerves are formed from ventral rami of L2, 3, 4, the obturator from anterior divisions, and the femoral from posterior divisions. Posterior divisions at the front? Yes: remember the embryonic medial rotation: see the beginning of this chapter.
Femoral hernia
Abdominal contents (e.g. fat, gut) may find their way into this and form a femoral hernia. It would be deep to the deep fascia of the thigh – the fascia lata – and may not be evident upon physical examination until it is large enough to protrude through the saphenous opening in the fascia lata which transmits the termination of the great saphenous vein. The hernia would present as a swelling in the thigh below and lateral to the pubic tubercle (an inguinal hernia would be above the pubic tubercle). Surgical procedures to reduce a femoral hernia may involve cutting the lacunar ligament to allow more room for manoeuvre: beware an accessory obturator artery passing from the external iliac artery to the obturator foramen.
Stab wounds in the femoral triangle
The femoral vessels and nerve are at risk and the potential for serious injury is great: paralysis of knee extension with resultant difficulties in locomotion, and potentially fatal haemorrhage. Apart from criminal attacks, those who wield long knives professionally (e.g. butchers) may injure themselves here: chain mail protection is available.
 |
| Fig. 13.11 |
 |
| Fig. 13.12 |
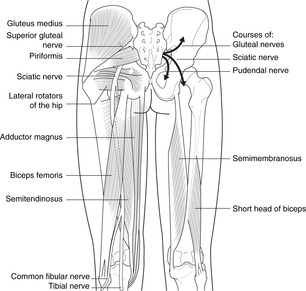
Hip abduction, rotation, extension; gluteal region
Abduction and medial rotation (Fig. 13.13)
These muscles are hip abductors: if you contract them whilst seated, this is what they do. But if you are standing with, say, your right foot on the ground and you contract them on the right, they will raise the opposite side of the pelvis, allowing you to lift your left foot. This is their principal function: the hip abductors contract on the weightbearing side during locomotion to allow body weight to be supported on the ipsilateral lower limb. If they are weakened or paralysed (e.g. poliomyelitis affecting L4, 5, S1), the pelvis will dip to the non-weightbearing side resulting in a waddling gait, the Trendelenburg gait (not to be confused with the waddling gait that workers in the fashion industry, and others, try hard to acquire).
• Tensor fasciae latae. Attachments: lateral iliac crest–lateral longitudinal thickening of fascia lata, the iliotibial tract, which passes between the ilium and the lateral condyle of the tibia. Many authorities regard this muscle as an extensor, but my eyes and hands tell me it is an abductor, and it is supplied by the superior gluteal nerve.
Extension (Fig. 13.13)
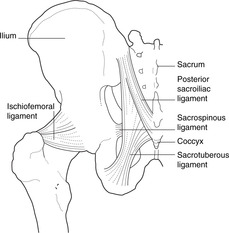
• Gluteus maximus. Attachments: posterior surface of iliac crest, sacrum, coccyx, sacrotuberous ligament–femur and tibia via iliotibial tract (see below).
Nerve supply: inferior gluteal nerve, L5 S1, 2.
Gluteus maximus is the big superficial muscle of the backside. Less than one-quarter of its fibres are attached to the femur, to the gluteal tuberosity just below the greater trochanter. Most fibres pass to the iliotibial tract of the fascia lata (see above). Gluteus maximus is a powerful extensor of the hip, used particularly for antigravity movements such as rising from the kneeling or sitting position, or climbing stairs.
• Hamstrings (semitendinosus, semimembranosus, biceps femoris). Attachments: ischial tuberosity–femur, tibia and fibula.
Nerve supply: tibial and common fibular nerves, L5, S1, 2, 3.
These hip extensors are also important knee flexors and are considered in detail in that section.
Lateral rotation: direct branches of L4–S2 (Fig. 13.13)
None of these muscles is particularly important.
• Piriformis. Attachments: anterior aspect of sacrum–greater trochanter (through greater sciatic foramen).
• Obturator externus. Attachments: outer margins of obturator foramen and membrane–trochanteric fossa.
• Obturator internus. Attachments: inner margins of obturator foramen and membrane–trochanteric fossa. This muscle turns a right angle through the lesser sciatic foramen. As it emerges it is joined above and below by fibres attached to the margins of the foramen, the superior gemellus and inferior gemellus (definitely not important).
• Quadratus femoris: ischial tuberosity–greater trochanter.
Other features of gluteal region and the hip
Greater and lesser sciatic foramina
The greater sciatic foramen transmits:
• the superior gluteal nerve and vessels above piriformis
• the inferior gluteal nerve and vessels, the pudendal nerve and vessels, and (usually) the sciatic nerve below piriformis. The pudendal nerve immediately then dives into the lesser sciatic foramen to pass in the ischioanal fossa of the perineum.
Sciatic nerve (Fig. 13.13)
• The nerve roots of L4–S3 form two large nerves, the tibial (anterior divisions supplying flexors) and the common fibular or fibular (posterior divisions supplying extensors). These nerves, although separate entities, are usually bound together as the sciatic nerve, the two components separating in the popliteal fossa.
However, they may be separate throughout their length, with the common fibular nerve passing above or through piriformis and the tibial through or below piriformis.
• The sciatic nerve in the gluteal region is immediately posterior to the hip joint capsule and may be damaged by posterior hip dislocations.
Sciatic nerve surface markings: injections
Surface markings of sciatic nerve:
• halfway between posterior superior iliac spine and ischial tuberosity, to
• halfway between ischial tuberosity and greater trochanter.
To be sure to avoid the nerve, intramuscular injections must be given in the upper outer quadrant of the backside.
13.3. Knee joint, movements, muscles, posterior thigh, popliteal fossa
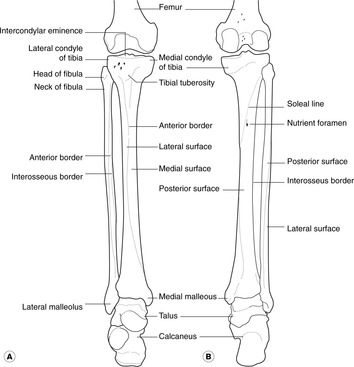
Bones
Distal femur (Fig. 13.14)
• Articular condyles: articulate with the tibia, the medial is bigger than the lateral. The patella articulates anteriorly.
• Linea aspera: this provides attachment for vastus muscles and the short head of biceps femoris. The linea aspera widens to form the:
• Popliteal surface, immediately related to the popliteal artery.
• Intercondylar notch: provides attachment for cruciate ligaments.
Proximal tibia (Fig. 13.14)
• Articular surfaces: receive the femoral condyles, the medial is bigger than the lateral.
• Intercondylar eminence: provides attachments for cruciate ligaments and menisci.
• Tibial tuberosity: provides attachment for the patellar ligament.
• Facet for articulation of fibula (superior tibiofibular joint).
Proximal fibula (Fig. 13.14)
• Head: this articulates with the tibia.
• Neck: this is related to the common fibular nerve.
Patella
This is a sesamoid bone in the tendon of quadriceps femoris.
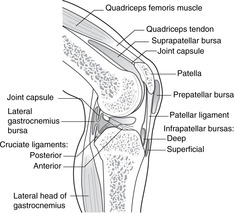
Knee joint
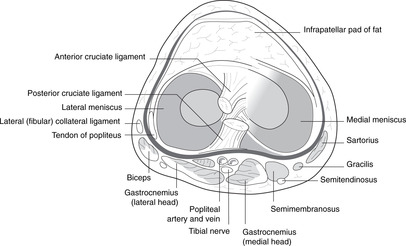
Synovial cavity
The synovial cavity has medial and lateral compartments that communicate anteriorly behind an infrapatellar fat pad. It extends superiorly for about a handsbreadth above the upper margin of the patella – the suprapatellar bursa (see below). There are two articulations between the tibia and femur, right and left, and one between the anterior femur and the patella.
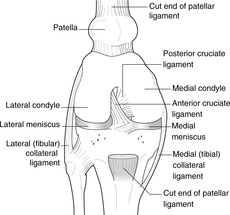
Menisci (semilunar cartilages) and collateral ligaments (Figs 13.15, 13.16)
• Medial and lateral menisci form partial cushions between tibia and femur and are attached to the intercondylar eminence of the tibia.
• The medial collateral ligament, a broad and flat band, is a thickening of the knee joint capsule and is attached to the medial meniscus. It is taut in knee extension and prevents knee abduction.
• The lateral collateral ligament is a cord-like structure, attached neither to the lateral meniscus nor the knee joint capsule. It is taut in knee extension and prevents knee adduction.
• The medial meniscus is more commonly injured in twisting (‘cartilage’) injuries than the lateral, partly because it is less mobile than the lateral and can not move out of the way.
Cruciate ligaments (Figs 13.16, 13.17)
• The anterior cruciate ligament is attached to the anterior intercondylar area of the tibia and passes upwards, backwards and laterally to the lateral side of the intercondylar notch of the femur. It limits anterior movement of the tibia on the femur (or posterior movement of the femur on the tibia). We can manage without it if it is torn.
• The posterior cruciate ligament is attached to the posterior intercondylar area of the tibia and the lateral meniscus. It passes upwards, forwards and medially (the two ligaments thus making a cross – hence the name) to the medial side of the intercondylar notch of the femur. It limits posterior movement of the tibia on the femur (or anterior movement of the femur on the tibia). It takes the weight of the body when we are standing with our knees bent, or when we descend stairs or a slope. We can not easily manage without it.
Testing the ligaments
• Collateral ligaments. Take the leg in your hands and, keeping the knee straight, try (gently!) to abduct and adduct the knee. There should be little if any movement.
• Cruciates. Ask the patient to sit with the knees flexed to about a right angle. Sit on the foot of the side you are testing. Grasp the upper tibia in your hands and try to pull it forwards. If it comes forwards more than it should, the anterior cruciate is torn. Now push backwards. If the tibia goes back more than it should, the posterior cruciate is torn. Since someone (who?) imagined this to be similar to pulling and pushing a drawer open and closed, it is called the drawer test.
 |
| Fig. 13.17 |
Movements and muscles
Extension (Figs 13.8, 13.17)
Note: the tendon between the muscle and the patella is the quadriceps tendon; that from patella to tibia is the patellar ligament or tendon.
Knee jerk (patellar tendon reflex). Tapping the patellar tendon to elicit the knee jerk tests the femoral nerve and spinal segments L3, 4. It is an important part of a general neurological examination.
Flexion (Fig. 13.13)
Nerve supply: tibial nerve, L5–S3.
The hamstrings are attached to the ischial tuberosity above.
• Biceps femoris. This passes laterally to the head of the fibula. Its tendon is easily palpated as it approaches the fibula. Its long head comes from the ischial tuberosity, and its short head (supplied by the common fibular nerve) from the lower part of the linea aspera.
• Semitendinosus. This passes medially and ends in a long tendon attached to the medial side of the upper tibia, in company with sartorius and gracilis.
• Semimembranosus. This passes medially ending in a wide membrane-like aponeurosis, deep to semitendinosus, attached to the medial side of the upper tibia and knee joint capsule.
• Both semi-muscles are palpable.
Locking, unlocking: tibial nerve, L4, 5, S1
Imagine you are sitting with your knee flexed. Now extend it. The lateral articular surfaces (smaller) reach the end of available movement before the medial, and the tibia rotates to allow more extension on the medial side. This is locking, and the rotation is passive. This happens when you stand from a sitting position, and the locking mechanism means that the knee is reasonably stable in extension without muscular activity maintaining it in this position.
At the beginning of flexion, unlocking must occur. This is not passive: popliteus muscle exists for this purpose. It arises from the posterior surface of the tibia and passes upwards and laterally to the lateral joint capsule and, by a part that penetrates the joint capsule, to the lateral meniscus and lateral condyle of the femur. It is having to cope with this unlocking mechanism that makes good artificial knees tricky to develop.
Bursitis
There are many bursas associated with the knee joint. Some of them are shown in Figure 13.17.
• Suprapatellar: an extension of the cavity of the knee joint. If the patella bounces when tapped, there is probably a knee joint effusion. An enlarged suprapatellar bursa may be palpable.
• Prepatellar. In the days when housemaids scrubbed floors, the superficial prepatellar bursa often became inflamed: housemaid’s knee.
• Infrapatellar, superficial and deep, on either side of the patellar tendon: separate from the joint. In the days when clergymen knelt on hard wooden surfaces to pray, this bursa often became inflamed: clergyman’s knee.
• Semimembranosus: between membrane and joint, may communicate with the joint.
• Popliteus: between popliteus tendon and the back of the joint, communicating with the joint and the lateral gastrocnemius bursa.
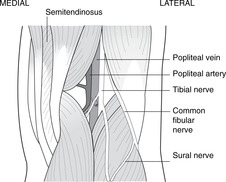
Popliteal fossa, neck of fibula, superior tibiofibular joint
This is a diamond-shaped area behind the knee. It is bounded above by the diverging hamstrings (biceps laterally, semi-muscles medially) and below by the lateral and medial heads of gastrocnemius. It contains the popliteal vessels and the two divisions of the sciatic nerve.
The popliteal artery and pulse (Fig. 13.18)
The artery is deep (= anterior) in the fossa, immediately adjacent to the posterior surface of the femur. It is vulnerable here: in a supracondylar femoral fracture, the distal portion of the femur may be pulled posteriorly by the gastrocnemius with the sharp edge of the fracture severing the artery.
 |
| Fig. 13.18 |
The popliteal pulse is palpated by pressing from behind against the back of the femur. The leg muscles must be relaxed, so ask the patient to sit with feet and backside on the same surface.
The popliteal artery divides at the lower margin in the popliteal fossa to give:
• the posterior tibial artery, which descends in the posterior compartment of the leg
• the anterior tibial artery, which descends in the anterior compartment of the leg.
The fibular artery, running close to the fibula in the posterior compartment, is usually a branch of the posterior tibial, but the pattern varies.
Nerves
• The tibial and common fibular nerves diverge in the upper part of the popliteal fossa, the tibial continuing more or less vertically and the common fibular passing laterally to the neck of the fibula. Both nerves are vulnerable to trauma in the fossa. Both nerves give branches to form the sural nerve supplying skin over the posterior calf.
• The common fibular is also vulnerable at the neck of the fibula, at just the right height to take the maximum impact from a car bumper (fender) injury. This nerve here is equivalent to the radial nerve at the radial neck: damage to the one may cause wrist drop; to the other foot drop.
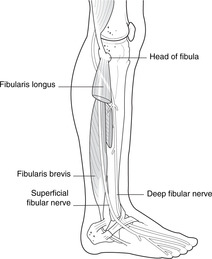
• At the neck of the fibula, the common fibular nerve divides into:
– deep fibular: supplies muscles that extend (dorsiflex) the ankle
– superficial fibular: supplies muscles that evert the ankle.
Again, compare the common fibular nerve with the radial in the upper limb.
Superior tibiofibular joint
It is synovial, separate from the knee joint, and unimportant.
13.4. Ankle joint and movements: posterior, anterior and lateral compartments of leg
The ankle joint is formed by the talus, tibia and fibula. Dorsiflexion is performed by muscles supplied by the deep fibular nerve, and plantarflexion by muscles supplied by the tibial nerve. Stability is provided by muscles and ligaments, the lateral ligament being frequently injured. Palpable pulses around the ankle include the posterior tibial and anterior tibial. Tendons passing from the leg to the foot are surrounded in the ankle region by synovial sheaths and restrained by retinacula.
Bones
Distal tibia (Fig. 13.14)
• Medial aspect. This is directly subcutaneous: feel your own. Because of this it is painful when it is kicked. The lack of muscular attachments also means it has a relatively poor blood supply, and fractures are sometimes slow to heal.
• Soleal line. An obvious ridge running upwards and laterally on the posterior of the bone. It is caused by the attachments of soleus (below) and popliteus (above).
• Interosseous border: to which is attached the interosseous membrane.
• Medial malleolus: the large bony prominence palpable medially at the ankle.
Distal fibula (Fig. 13.14)
• Interosseous border: to which is attached the interosseous membrane.
• Lateral malleolus: the large bony prominence palpable laterally at the ankle.
• Articular surface: the internal aspect of the lateral malleolus forms about one-third of the proximal articular surface of the ankle joint.
• There is nothing else below the neck of the fibula that is important.
Talus (Figs 13.14, 13.19)
• Body (proximal). This articulates with the tibia and fibula, the lateral articular surface being larger than the medial (tibial). There is a separate articular surface for the posterior part of the calcaneus: this is considered in section 13.5 (p. 222).
• Neck. Like the scaphoid, to which it is equivalent, the talus has a narrow central section which may be fractured. It is liable to avascular necrosis, since in twisting it may tear its blood supply.
• Head (distal). This is palpable. It articulates with the anterior part of the calcaneus and navicular and is considered in section 13.5.
Calcaneus (calcaneum) (Figs 13.19, 13.20)
This is considered in more detail in section 13.5, but at this stage note the sustentaculum tali (Latin: support of the talus), which extends medially from the bone and is palpable inferior to the head of the talus.
Other foot bones (Figs 13.19, 13.20)
These are not directly relevant to the ankle joint although some of them provide attachments for muscles that act on the ankle. They are considered in section 13.5.
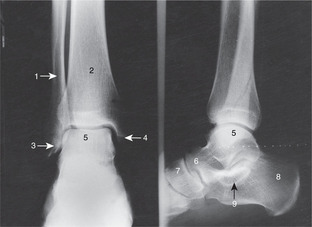
Ankle joint (Fig. 13.20)
• The distal ends of the tibia and fibula are united by fibrous tissue (inferior tibiofibular joint) and form a mortise into which the body of the talus fits.
• The dorsum of the foot is at the front (see p. 203).
• Moving the distal foot down is plantarflexion, the equivalent of flexion at the wrist.
• Moving the distal foot up is dorsiflexion, the equivalent of extension at the wrist.
• Turning the sole of the foot medially (inwards) is inversion.
• Turning the sole of the foot laterally (outwards) is eversion.
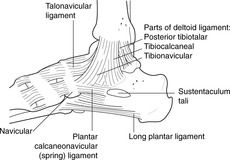
Inferior tibiofibular joint and ankle ligaments (Fig. 13.21)
• Inferior tibiofibular ligaments: the fibres are oblique rather than horizontal, so there is some ‘give’ at this joint, but otherwise there is no significant movement of the tibia and fibula.
• Lateral ligaments: calcaneofibular, anterior talofibular and posterior talofibular. The anterior talofibular ligament is most often the site of an ankle ‘sprain’. Tenderness just below and in front of the lateral malleolus is indicative of a torn anterior talofibular ligament.
• Deltoid (medial) ligament. From the medial malleolus, the medial ligament spreads out as a triangle (hence the name). There are two parts:
– superficial: down and back to the sustentaculum tali of the calcaneus
– deep: backwards and downwards to the entire length of the sustentaculum tali, down to the spring ligament (see section 13.5) and down and forwards to the navicular. It is a very strong ligament – so strong that the sustentaculum may be fractured rather than the ligament torn.
 |
| Fig. 13.21 |
Stability
The articular surface of the talus is wider in front than behind so that when the ankle is dorsiflexed, the wider part of the articular surface of the talus is in the mortise formed by the tibia and fibula and the joint is stable. In plantarflexion, though, the narrower part of the talus is in the mortise and the joint is therefore somewhat unstable. Fortunately, we do not walk with the ankle in plantarflexion, but ballet dancers need to be very careful.
Movements and muscles
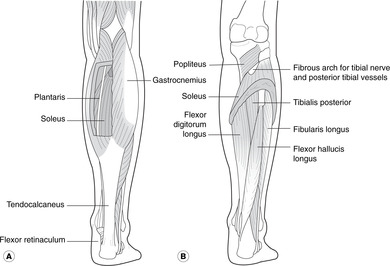
Plantarflexion, toe flexion, inversion (Fig. 13.22)
Muscles which plantarflex the ankle and invert the foot occupy the posterior compartment of the leg.
Nerve supply: tibial nerve, L4, 5, S1, 2.
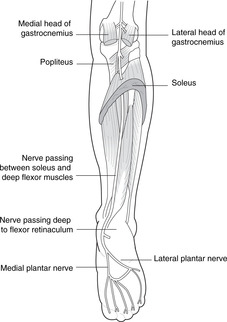
Superficial flexors. Attached to the calcaneus by the Achilles tendon (tendo calcaneus): gastrocnemius (from femur) and soleus (from tibia, fibula):
• Gastrocnemius: medial and lateral heads attached to medial and lateral condyles of the femur. They form obvious bulges at the back of the leg and unite on the Achilles tendon (tendo calcaneus), which is attached to the lower part of the posterior surface of the calcaneus.
• Soleus. This is attached to the soleal line on the posterior surface of the tibia and the upper third of the back of the fibula. Between these two bones is a fibrous arch, deep to which pass the tibial nerve and the posterior tibial artery and veins. It is a very bulky muscle and contains the soleal venous plexus, so important in the soleal muscle pump (see p. 225). It is attached by the Achilles tendon to the calcaneus.
• Plantaris. This very small muscle from the lateral condyle of the femur has a very long tendon that joins the Achilles tendon. It is very unimportant, so everyone remembers it.
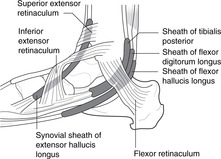
Deep flexors. Attached to the bones of the sole of the foot: tibialis posterior, flexor digitorum longus, flexor hallucis longus:
• Tibialis posterior. Attachments: posterior tibia, fibula, interosseous membrane–navicular, inferior surface. Its tendon grooves the posterior surface of the medial malleolus and is palpable at the ankle. The tendon sends slips to every tarsal and metatarsal bone except the talus and first metatarsal.
• Flexor digitorum longus. Attachments: posterior tibia–distal phalanges of digits 2–5. Its tendon grooves the medial malleolus and is palpable at the ankle.
• Flexor hallucis longus. Attachments: posterior fibula–distal phalanx of first (big) toe (with part of flexor digitorum longus). Its tendon grooves the back of the tibia and passes immediately deep to the sustentaculum tali of the calcaneus. Its tendon is not easily palpable, being deeply situated. Note that in the leg the long flexor of the big toe is lateral to that of the other toes, whereas in the foot the big toe is medial. The tendons cross in the foot.
Ankle jerk. Tapping the Achilles tendon to elicit the ankle jerk tests the tibial nerve and spinal segments S1, 2. It is an important part of a general neurological examination.
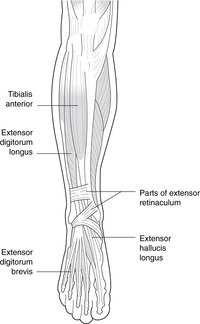
Dorsiflexion, eversion (Fig. 13.23)
Nerve supply: common fibular nerve, L4, 5, S1.
 |
| Fig. 13.23 |
Ankle dorsiflexion and toe extension: deep fibular nerve. These muscles occupy the anterior compartment of the leg:
• Tibialis anterior. Attachments: tibia, interosseous membrane–medial cuneiform and first metatarsal. This fleshy muscle and its tendon anterior to the medial side of the ankle are palpable.
• Extensor digitorum longus. Attachments: fibula, interosseous membrane–extensor expansion of digits 2–5. These tendons are palpable. On the dorsum of the foot they are joined by tendons of extensor digitorum brevis. The tendon passing to the fifth toe may be reinforced by a slip from the fibula – fibularis tertius. Forget about it.
• Extensor hallucis longus. Attachments: fibula, interosseous membrane–base of distal phalanx of first (big) toe. The tendon is palpable.
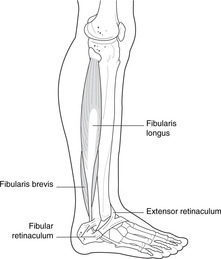
Ankle eversion: superficial fibular nerve (see Fig. 13.28). Muscles that evert the foot occupy the lateral compartment of the leg:
• Fibularis longus. Attachments: fibula–inferior surface of medial cuneiform and first metatarsal. The tendon enters the foot laterally but then crosses under the bones to the medial side, grooving the under surface of the cuboid. Both muscle and tendon are palpable.
• Fibularis brevis. Attachments: fibula–base of fifth metatarsal.
 |
| Fig. 13.28 |
Arrangements to help tendons turn corners
• Flexor retinaculum (Fig. 13.24). The tendons of tibialis posterior (superficial), flexor digitorum longus and flexor hallucis longus (deep) enter the foot behind the medial malleolus deep to the flexor retinaculum. Other structures which accompany them are the tibial nerve, the posterior tibial artery and its venae comitantes.
 |
| Fig. 13.24 |
• Extensor retinaculum (Figs 13.23, 13.24). Extensor tendons (extensor hallucis, extensor digitorum, fibularis tertius) pass from leg to foot behind the extensor retinaculum, which is in two parts: an upper transverse band, and a lower Y-shaped band. Other structures that accompany them are the deep fibular nerve, the anterior tibial artery and its venae comitantes.
• Fibular retinaculum (Fig. 13.25). The tendons of fibularis longus and brevis pass between ankle and foot deep to the superior and inferior fibular retinacula.
 |
| Fig. 13.25 |
• Synovial sheaths. As the tendons pass deep to the retinacula at the ankle, they are enclosed in synovial sheaths. As at the wrist, it is more important that you know that they exist rather than details of them. Athletes (jumpers, gymnasts, basketball players, etc.) and others may suffer from tenosynovitis of these tendons and sheaths – a condition which can be painful and disabling. Pain fibres are conveyed in the nearest local cutaneous nerve.
Pulses at the ankle (Fig. 13.1)
Posterior tibial
The posterior tibial pulse is easily palpable just behind the medial malleolus, deep to the flexor retinaculum. Feel your own.
Anterior tibial and dorsalis pedis
The anterior tibial pulse is easily palpable between the tendons of extensor hallucis longus and digitorum longus. At the level of the malleoli, the anterior tibial artery becomes the dorsalis pedis artery, another important palpable pulse. Feel your own.
13.5. Foot
Because the foot is less often injured than the hand, you do not require such detailed knowledge of it. Revise the hand before proceeding. The small muscles of the foot are equivalent to those of the hand, and, together with foot bones and ligaments, constitute a dynamic structure that adapts to posture, stance and terrain. Inversion and eversion take place at several joints in the foot, inversion being supplied by the tibial nerve and eversion by the superficial fibular. The dorsalis pedis pulse is usually palpable on the dorsum of the foot.
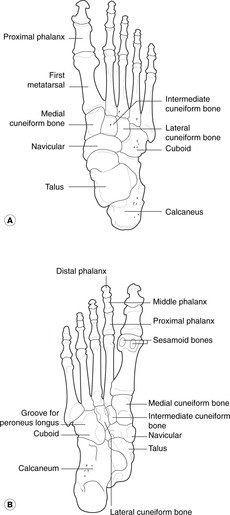
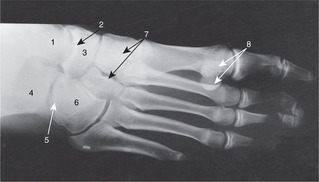
Bones (Figs 13.19, 13.26)
• Tarsal bones: learn the names, be able to recognise the bones on radiographs, and point out the following surface features:
– head of the talus
– sustentaculum tali of the calcaneus
– tuberosity of the navicular
– cuboid.
• Metatarsals 1–5, and phalanges, as in the hand.
Joints
Talus–calcaneus–cuboid–navicular
There are two separate talocalcaneal articulations and one also includes the navicular. There is disagreement concerning the nomenclature of these joints and the version that follows is as good as any.
• Subtalar joint. This is directly underneath the talus, in line with the tibia.
• Talocalcaneonavicular joint. This is anterior to the head of the talus and involves the sustentaculum tali, the head of the talus, the spring ligament and the navicular.
• Calcaneocuboid joint. This is a separate joint cavity, but is a functional unit with the talocalcaneonavicular joint, the two together being called by some the midtarsal joint. However, this term is used differently by different authorities.
Other joints, foot movements
There is no need to bother with the details of other tarsal joints.
Inversion and eversion are composite movements that involve several joints. Disease of any one synovial cavity will result in limitation of foot function. This involves all the small movements that must take place during locomotion, not only the obvious ones concerned with taking a step, but also the small adjustments concerned with adapting foot position to an uneven or sloping surface. You do not need to learn details, but try to appreciate that joint diseases in the foot will affect our stance and our ability to get about.
Ligaments
There are numerous tarsal ligaments: some are worth reading about.
• Medially in the sole: spring (plantar calcaneonavicular) ligament: sustentaculum tali of calcaneus–navicular. This forms part of the articular surface for the talocalcaneonavicular joint: its upper surface is covered by articular cartilage. It is continuous with the deltoid ligament (see section 13.4, p. 217). Note that the bones to which the spring ligament is attached are palpable.
• Laterally in the sole: long and short plantar (calcaneocuboid) ligaments. The long plantar also sends slips to the middle three metatarsals. The short plantar is deep (superior) to the long plantar and the tendon of fibularis longus runs between them on its way from the lateral side of the foot to the medial cuneiform.
• On the dorsum: bifurcate ligament: calcaneus–cuboid, navicular.
Muscles and arches of the foot
Muscles of the sole
Nerve supply: medial and lateral plantar nerves, L5–S3.
Muscles of the sole are equivalent to the thenar, hypothenar, lumbricals and interosseous muscles of the hand except that:
• hallucis replaces pollicis
• there are no opponens muscles.
As in the hand, the first toe has no lumbrical. There is no need to learn details of actions or attachments: for most practitioners these are superfluous. The muscles are innervated as in the hand: regard the medial plantar nerve as the equivalent of the median nerve and the lateral plantar as the equivalent of the ulnar, except that the medial plantar (median equivalent) supplies only one lumbrical, that of the second toe.
Muscle actions
Although we can train our toes to wield paintbrushes, etc., it is sufficient to regard the small muscles of the foot as dynamic ligaments, constantly contracting and relaxing in response to subtle changes in posture, activity and orientation of the supporting surface.
Long flexor tendons
• Flexor hallucis longus, flexor digitorum longus:
– After passing behind the medial malleolus, these tendons cross.
– An additional muscle, flexor accessorius (quadratus plantae) connects the tendon of flexor digitorum longus to the lower surface of the calcaneus and converts the oblique pull of the long tendon to one in line with the axis of the foot itself.
– Sesamoid bones are found in these tendons –we walk on them.
• Fibularis longus, from the lateral side; tibialis posterior, from the medial side (see above).
Plantar fascia
This is tougher than the palmar fascia in the hand. The skin is so tightly attached to it that infiltration of local anaesthetics, for instance in order to deal with something as simple as a plantar wart, may be difficult and painful.
Dorsum of the foot
• Extensor digitorum brevis: deep fibular nerve. It is unimportant except that its fleshy belly may be mistaken for a tumour.
• The superficial dorsal venous arch gives rise medially to the great saphenous vein, and laterally to the small saphenous vein.
Arteries of the foot (Fig. 13.1)
• Branches of the posterior tibial artery (see above): medial and lateral plantar arteries. The lateral plantar curves medially under the metatarsals to anastomose with a branch of the dorsalis pedis artery that has passed between the first and second metatarsals.
• Dorsalis pedis artery, a continuation of the anterior tibial artery. See above.
Nerves of the foot
• Branches of the tibial nerve (Fig. 13.27):
– medial plantar: fewer muscles, more skin (like the median in the hand): plantar skin of the medial three and a half digits
– lateral plantar: more muscles, less skin (like the ulnar in the hand): plantar skin of the lateral one and a half digits.
 |
| Fig. 13.27 |
• Branches of the common fibular nerve (Fig. 13.28):
– deep fibular: only a tiny area of skin at the base of the first and second toes
– superficial fibular: most of the skin of the dorsum.
13.6. Venous drainage of the lower limb (Figs 13.9, 13.29)
 |
| Fig. 13.29 |
Mechanism of venous return
• Superficial veins:
– Great saphenous vein. This is formed medially from the dorsal venous arch of the foot and ascends in front of the medial malleolus and behind the knee, continuing up the thigh to penetrate the fascia lata below and lateral to the pubic tubercle at the saphenous opening. It drains into the femoral vein. Below the knee it is accompanied by the saphenous nerve.
– Small saphenous vein. This is formed laterally from the dorsal venous arch of the foot and ascends on the back of the calf accompanied by the sural nerve. It penetrates the deep fascia in the popliteal fossa, and joins the popliteal vein.
There are several tributaries in the calf and thigh (details not necessary).
• Deep veins: venae comitantes of the deep arteries unite to form the popliteal vein, which becomes the femoral.
• Perforators, permitting blood to flow from superficial to deep.
The effective venous return from the lower limb depends upon a pumping mechanism within the deep fascia.
• The deep fascia, in the thigh called fascia lata, is a tough fibrous layer, in no way elastic. The valves in the deep veins permit blood to flow only towards the heart so when muscles within the deep fascial sleeve contract, deep veins are compressed and blood flows upwards (because of the valves). When the muscles relax, blood is sucked into the deep veins through the perforators from the superficial system, the perforators also containing valves allowing blood to flow only in this direction.
• Below the knee, one of the largest muscles surrounding the deep veins is the soleus, and this mechanism is known as the soleal muscle pump.
• The chances of a blood cell passing from foot to femoral vein through the length of the great saphenous vein are very small – it is likely to be sucked into the deep system through a perforator.
Disorders of the venous system
• Lack of muscular contraction encourages venous stasis and blood clotting with the risk of potentially dangerous emboli formation. This is why lying lazily in bed is dangerous, and sitting for long periods in aircraft is dangerous. It is even worse in economy class because the chances are that the front of the seat digs into the back of your soleus, restricting blood flow even more – yet another peril of poverty.
• After a deep vein thrombosis affecting the perforators, they recanalise without valves. This means that the muscle pump will force blood back from deep to superficial systems – one cause of venous disease in the lower limb.
• Varicosities of the great saphenous vein may result from incompetence of the valve at the top of the vein. A test for this is Trendelenburg’s test. With the patient lying, elevate the leg to empty the great saphenous vein. Then apply pressure to the saphenous opening. Now place the leg in a dependent position and release the pressure. If the valve is competent, the vein should not fill from above; if it is incompetent it will do so.
• At the termination of the great saphenous vein, just before it passes deep through the saphenous opening in the fascia lata, it is joined by tributaries including those from the genitalia (external pudendal) and skin of the thigh (superficial femoral) (Fig. 13.9). If the great saphenous is to be removed or ligated in this region in order to treat symptoms of varicose veins, the way must be left clear for blood from these tributaries to reach the femoral vein, so the great saphenous must be ligated distal to its union of these veins.
13.7. Innervation, nerve testing, surface anatomy
Nerves: a revision of some important points
Dermatomes (see Fig. 6.6, p. 36)
Remember these:
• L3 at the knee (over the patella)
• S2 over the popliteal fossa
• L5 under the first toe
• S1 under the fifth toe.
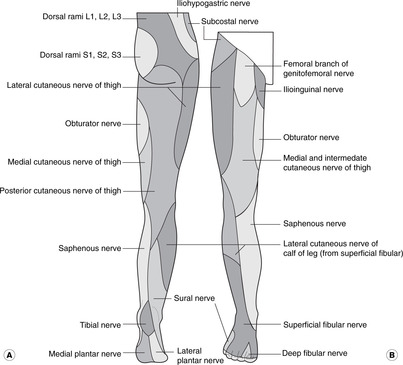
Sensory nerves (Fig. 13.30)
• Gluteal region:
– posterior cutaneous branches of sacral plexus.
• Anterior thigh:
– branches of genitofemoral and ilioinguinal
– lateral cutaneous nerve of the thigh
– intermediate and medial cutaneous nerves of the thigh (branches of the femoral).
• Posterior thigh and popliteal fossa: sacral plexus:
– posterior cutaneous nerve of the thigh (sacral plexus).
• Leg:
– saphenous nerve (from femoral): medial skin; since it accompanies the great saphenous vein it may be damaged by surgical procedures on the vein.
– sural nerve (from tibial and common fibular in the popliteal fossa): posterolateral skin
– superficial fibular nerve: lower anterior skin; it may be affected by trauma at the fibular neck.
– lateral cutaneous nerve (from common fibular nerve); it may be affected by trauma at the fibular neck.
• Foot:
– superficial fibular nerve: dorsum
– saphenous nerve: medial skin
– sural nerve: lateral skin
– medial and lateral plantar nerves (branches of tibial nerve).
Segmental values for movements and reflexes
| Hip | |
| Flexion, adduction, medial rotation | L2, 3 |
| Extension, abduction, lateral rotation | L4, 5, S1 |
| Knee | |
| Extension | L3, 4 |
| Flexion | L5, S1 |
| Ankle | |
| Dorsiflexion | L4, 5 |
| Plantarflexion | S1, 2 |
| Foot | |
| Inversion | L4 |
| Eversion | L5, S1 |
Revise dermatomes: see Figure 6.6 (p. 36)
Surface anatomy: a revision of some important points
Thigh
• Femoral pulse: midpoint of inguinal ligament.
• Femoral vein: medial to femoral pulse.
• Femoral nerve: lateral to femoral pulse.
• Saphenous opening in fascia lata, femoral hernia: about 2 cm below and lateral to pubic tubercle.
Knee
• Popliteal pulse: press deep in popliteal fossa against popliteal surface of femur.
• Suprapatellar bursa: extends about one handsbreadth above upper margin of patella.
• Prepatellar bursa: directly over patella.
• Head of fibula: tendon of biceps femoris.
• Common fibular nerve: neck of fibula.
Ankle region and foot
• Posterior tibial pulse: immediately posterior to medial malleolus.
• Dorsalis pedis pulse: between tendons of extensors hallucis and digitorum longus.
• Great saphenous vein: anterior to medial malleolus.
• Lateral ligaments of ankle: below and in front of lateral malleolus.
• Sustentaculum tali of calcaneus: attachment of deltoid ligament.
Single best answer questions
For each numbered question, only ONE of the options lettered a–d is correct.
21. Synovium is found:
a. in epiphyseal plates.
b. in symphyses.
c. lining all nonarticular surfaces in synovial joints.
d. on adjacent articular surfaces of bones in synovial joints.
22. In the lower limb:
a. a femoral hernia would be lateral to the femoral pulse at the inguinal region.
b. damage to L5 nerve would cause weakness of knee extension.
c. hip adductor muscles are attached to the tibia.
d. the superior gluteal nerve supplies hip abductors.
23. The sciatic nerve:
a. gives off the obturator nerve.
b. is the same as the tibial nerve.
c. is vulnerable in anterior hip dislocations.
d. is vulnerable in posterior hip dislocations.
24. At the knee joint:
a. skin over the posterior aspect of the joint is supplied by L3.
b. the anterior cruciate ligament is taut when the joint is fully flexed.
c. the lateral meniscus is more fixed than the medial.
d. the patella is more likely to dislocate laterally than medially.
25. Which bursa is most likely to be injured by repeated pressure over the patella?
a. infrapatellar.
b. popliteus.
c. prepatellar.
d. semimembranosus.
26. In the foot and at the ankle:
a. dorsiflexor tendons pass deep to the flexor retinaculum.
b. medial skin of the foot is supplied by a branch of the femoral nerve.
c. plantarflexion would be lost after section of the common fibular (common peroneal) nerve.
d. the Achilles tendon is attached to the talus.
27. At the ankle region:
a. eversion mainly takes place at the ankle joint.
b. the Achilles tendon is attached to the talus.
c. the great saphenous vein is posterior to the medial malleolus.
d. tibialis posterior tendon passes deep to the flexor retinaculum.
28. Damage at the neck of the fibula may cause:
a. anaesthesia over gastrocnemius.
b. anaesthesia over the medial foot.
c. foot drop.
d. plantar anaesthesia.
29. In the vertebral column:
a. a herniated nucleus pulposus between L4 and L5 may compress the spinal cord.
b. ligamenta flava are attached to adjacent pedicles.
c. lumbar spinal nerves pass through the superior part of the intervertebral foramina.
30. A midline herniation of a lower lumbar intervertebral disc is most likely to damage nerves that:
a. supply anterior thigh sensation.
b. supply bladder and anal sphincters.
c. supply hip adduction.
d. supply knee extension.
Matching item questions
Questions 31–35: nerves
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. femoral nerve
b. tibial nerve
c. nerve related to the neck of the fibula
d. obturator nerve
e. genitofemoral nerve
31. supplies knee extensors.
32. damage to this nerve may result in foot drop.
33. is related to the ovarian fossa in the pelvis.
34. a branch of this supplies skin on the medial side of the foot.
35. cutaneous sensation of the medial thigh.
Questions 36–41: vessels and nerves
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. profunda femoris artery
b. popliteal artery
c. L3, 4
d. S1, 2
e. anterior superior iliac spine
36. blood supply to the hip joint.
37. branch of artery palpable deep to the inguinal ligament.
38. may be damaged by supracondylar femoral fracture.
39. contributes to obturator nerve.
40. patellar tendon reflex.
41. Achilles tendon reflex.
Questions 42–47: nerve lesions
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. common fibular (common peroneal) nerve lesion
b. femoral nerve lesion
c. L3 lesion
d. S1, 2 lesion
e. S3, 4 lesion
42. anaesthesia over anterior thigh.
43. anaesthesia of posterior leg and popliteal skin.
44. hyporeflexia of the patellar tendon reflex.
45. foot drop.
46. weakness of hip adduction.
47. hyporeflexia of ankle jerk.
Questions requiring short answers
48. A patient is stabbed in the thigh just below the middle of the inguinal ligament. What structures are in danger? What will be the effect of section of the major nerve here?
49. Describe or draw the main arterial tree of the lower limb. Name three sites where peripheral pulses may be palpated. Where are these vessels liable to injury?
50. Describe the venous drainage of the lower limb, indicating the normal direction of blood flow between the superficial and deep veins.
51. Describe the blood supply of the head of the femur in the adult. How is this relevant to femoral neck fractures?
52. Describe the knee joint cartilages and ligaments. How would you test the ligaments? List the muscle groups that perform flexion and extension and the segmental innervation of these muscle groups. Names of individual muscles are not required.
53. What is foot drop? How may it be caused?
54. A 20-year-old student twists his ankle playing basketball. There is marked tenderness anterior to the lateral malleolus. Name the bones constituting the ankle joint and state the injury that has occurred. List the muscle groups acting on the joint and give their nerve supply and segmental innervation.
55. List the structures attached to and/or related to the sustentaculum tali of the calcaneus.
Self-assessment on Chapter 13: answers
True/false answers
1.
b. False. It is very important.
c. True. Posterior dislocations of the hip joint may damage the nerve.
d. True. The important capsular (retinacular) vessels may be damaged.
e. True. Sensory information from both joints passes in the same nerves, so referred pain from hip to knee is not unusual.
2.
a. True.
b. True.
c. True.
d. True.
e. False. Posterior.
3.
a. False. This is the most unsafe area.
b. False. They flex the knee and extend the hip.
c. True.
d. True.
e. True.
4.
a. False. It is attached to the anterior superior iliac spine.
b. True. Ovarian pain may be referred to the territory of the obturator nerve. Revise the pelvis.
c. True.
d. False. The vein is medial to the artery at the inguinal ligament.
e. False. Biceps is lateral.
5.
a. False. It is attached to the intertrochanteric line anteriorly, but posteriorly it is well up the neck.
b. True.
c. False. It limits extension.
d. True.
e. True.
6.
a. False. The sartorius muscle is inserted on the medial side of the tibia.
b. False. Sartorius is superficial to quadriceps femoris.
c. True.
d. False. It forms the lateral boundary of the femoral triangle.
e. False. It flexes the hip joint (but only weakly).
7.
a. True.
b. True.
c. True.
d. False.
e. False.
8.
a. False. Pull the tibia anteriorly on the femur.
b. False. It is not attached (unlike the medial).
c. True.
d. True. (Why does this matter?)
e. False. It is part of the joint.
9.
a. False. The femoral nerve supplies these.
b. True.
c. False. Anterior femoral skin is supplied by the femoral nerve and its branches.
d. True. Plantar branches of the tibial nerve supply skin on the sole of the foot.
e. True.
10.
a. False. It is a branch of the popliteal artery.
b. True.
c. True.
d. False. Dorsiflexors are supplied by the anterior tibial artery.
e. False. It is nowhere near the sural nerve.
11.
a. False. It is a branch of the tibial and common fibular nerves (the saphenous nerve is a branch of the femoral).
b. True.
c. False. It is a cutaneous nerve.
e. False. It supplies skin over the posterior aspect of the leg.
12.
a. False. It is a branch of the popliteal.
b. False. The posterior tibial is so related.
c. False. The posterior tibial does so.
d. True.
e. False. In the foot, by definition, it is called the dorsalis pedis artery. (Sorry! I agree that this is a nit-picking question, but it does illustrate that names can make all the difference.)
13.
a. True.
b. False. Dorsiflexors and evertors.
c. False.
d. True.
e. False. To the tibia, as you might expect from the name.
14.
a. True. Even though it comes round to the ‘front’.
b. True.
c. True.
d. True.
e. False. On the dorsum.
15.
a. False. It is anterior. Anyone who gets this wrong is foolish: they have only to look down at their ankles.
b. True.
c. False. Eversion and inversion take place at joints in the foot.
d. False. It is attached to the calcaneus
e. True.
16.
a. True. Compare it with the scaphoid in the upper limb.
b. True. It has an articulation posteriorly at the subtalar joint, and another anteriorly at the talocalcaneonavicular joint.
c. True.
d. True. Saphenous nerve function would be lost if the laceration severed the femoral nerve.
e. True.
17.
a. False. Tibia, navicular and calcaneus.
b. True.
c. True.
d. True.
e. True.
18. All true!
19.
a. False. It is medial to the pulse. The nerve is lateral.
b. False. Top of thigh, almost level with pubic tubercle.
c. False. Other direction.
d. False. The artery is there, and vulnerable in supracondylar femoral fractures.
e. True.
20. The sciatic nerve:
a. True.
b. True.
c. True.
d. True.
e. False. They are supplied by the gluteal nerves.
Single best answers
21. c.
22. d.
23. d.
24. d.
25. c.
26. b.
27. d.
28. c.
29. c.
30. b. Cauda equina syndrome.
Matching item answers
31. a. Quadriceps femoris, the extensor of the knee, is supplied by the femoral nerve.
32. c. The common fibular nerve may be damaged at the neck of the fibula, causing foot drop.
33. d.
35. e.
36. a.
37. a. Profunda femoris is a branch of the femoral artery, whose pulse is palpable at the inguinal ligament.
38. b.
39. c.
40. c.
41. d.
42. c.
43. d.
44. c. The reflex is generally held to test L3, 4, so it would be affected.
45. a.
46. c. Adductors are supplied by obturator nerve (L2, 3, 4), so there would be weakness.
47. d.
Short answers
48. The femoral nerve, artery, and vein, with branches and tributaries, may be damaged. Section of the femoral nerve will cause functional loss of knee extensors (quadriceps), reduced or absent knee jerk, and loss of skin sensation over the anterior thigh.
49. Figure 13.1 shows the main arteries of the lower limb and the sites of palpable pulses. The femoral artery is liable to injury in the anterior thigh; the popliteal artery is vulnerable in supracondylar femoral fracture. See page 216.
50. The main points are as follows. There are superficial (name the long and short saphenous veins) and deep systems; perforators have valves to allow blood to go from superficial to deep; the soleal pump draws blood into the deep system; if the valves in the perforators are destroyed, blood will go from deep to superficial and cause venous disease of the saphenous veins.
51. The most important vessels supplying the head of the femur are the capsular (retinacular) vessels. Next in importance are branches of the nutrient artery (not in the child because these do not cross the epiphyseal plates) and least important is the artery of the round ligament of the head. Femoral neck fractures will damage the capsular vessels and/or the branches of the nutrient artery. (You could give information about the trochanteric and cruciate anastomoses if you like.)
52. See section 13.3, page 213. The important ligaments you should mention are the menisci, the cruciates and the collaterals. Test the cruciates by the drawer test, and the collaterals by passive abduction/adduction: there should be very little. Flexion: hamstrings, L5, S1. Extension: quadriceps femoris, L3, 4.
53. Foot drop is paralysis or weakness of dorsiflexion and eversion. It is caused by damage to the common fibular (peroneal) nerve at the neck of the fibula, often as a result of direct trauma from, for example, a road traffic accident.
54. The ankle joint consists of the tibia, fibula and talus. The lateral collateral ligaments have been torn. Ankle dorsiflexion is performed by the muscle groups of the anterior compartment, supplied by the deep fibular nerve, L4, 5. Ankle plantarflexion is performed by the muscle groups of the posterior compartment, supplied by the tibial nerve, S1, 2.
55. The following structures are attached to the sustentaculum tali of the calcaneus: deltoid ligament, spring ligament. Related structures are:
• superficial: tendons of flexor digitorum longus, tibialis posterior
• inferior (a smooth groove is visible on the bone): tendon of flexor hallucis longus.