6
Lower Limb
Deep fascia and the saphenous opening
Tarsal tunnel, retinacula, and arrangement of major structures at the ankle
ADDITIONAL LEARNING RESOURCES FOR CHAPTER 6, LOWER LIMB, ON STUDENT CONSULT (www.studentconsult.com):
 Image Library — illustrations of lower limb anatomy, Chapter 6
Image Library — illustrations of lower limb anatomy, Chapter 6
 Self-Assessment (scored) — National Board style multiple-choice questions, Chapter 6
Self-Assessment (scored) — National Board style multiple-choice questions, Chapter 6
 Short Questions (not scored) — National Board style multiple-choice questions, Chapter 6
Short Questions (not scored) — National Board style multiple-choice questions, Chapter 6
 Interactive Surface Anatomy — interactive surface animations, Chapter 6
Interactive Surface Anatomy — interactive surface animations, Chapter 6
Achilles tendinitis and tendinosis
Regional anatomy
The lower limb is divided into the gluteal region, thigh, leg, and foot on the basis of major joints, component bones, and superficial landmarks (Figs. 6.1, 6.2):
 The leg is between the knee and ankle joints. The bones of the leg are the tibia and fibula.
The leg is between the knee and ankle joints. The bones of the leg are the tibia and fibula.
Fig. 6.1 Regions of the lower limb.
Fig. 6.2 Bones and joints of the lower limb.
The major functions of the lower limb are:
 to support the weight of the body when standing, and
to support the weight of the body when standing, and
 to move the body through space.
to move the body through space.
When standing erect, the line of the center of gravity is slightly posterior to the hip joints, anterior to the knee and ankle joints, and directly over the almost circular support base formed by the feet on the ground. The organization of ligaments at the hip and knee joints, together with the shape of the articular surfaces, particularly at the knee, facilitates “locking” of these joints into position, thereby reducing the muscular energy required to maintain a standing position.
When walking, integration of movements at all joints in the lower limb positions the foot on the ground and moves the body smoothly over the foot with minimal changes in the position of the body’s center of gravity.
The lower limb is directly anchored to the axial skeleton by a sacroiliac joint and by strong ligaments, which link the pelvic bone to the sacrum. This design serves to transmit the weight of the body above to the lower limb below.
Movements at the hip joint are flexion, extension, abduction, adduction, medial and lateral rotation, and circumduction (Fig. 6.3).
Fig. 6.3 Movements of the hip joint. A. Flexion and extension. B. Abduction and adduction. C. External and internal rotation. D. Circumduction.
The knee and ankle joints are primarily hinge joints. Movements at the knee are mainly flexion and extension (Fig. 6.4A). Movements at the ankle are dorsiflexion (movement of the dorsal side of foot toward the leg) and plantarflexion (Fig. 6.4B).
THE HIP
Bony pelvis
The external surfaces of the pelvic bones, sacrum, and coccyx are predominantly the regions of the pelvis associated with the lower limb, although some muscles do originate from the deep or internal surfaces of these bones and from the deep surfaces of the lumbar vertebrae, above.
Each pelvic bone is formed by three bones (ilium, ischium, and pubis), which fuse during childhood. The ilium is superior and the pubis and ischium are anteroinferior and posteroinferior, respectively (Fig. 6.5).
Fig. 6.5 External surface of the bony pelvis. Lateral view.
Ilium
The upper fan-shaped part of the ilium is associated on its inner side with the abdomen and on its outer side with the lower limb. The top of this region is the iliac crest, which ends anteriorly as the anterior superior iliac spine and posteriorly as the posterior superior iliac spine (Fig. 6.5). A prominent lateral expansion of the crest just posterior to the anterior superior iliac spine is the tuberculum of iliac crest.
The anterior inferior iliac spine is on the anterior margin of the ilium, and below this, where the ilium fuses with the pubis, is a raised area of bone (the iliopubic eminence [Fig. 6.5]).
The gluteal surface of the ilium faces posterolaterally, lies below the iliac crest, and provides attachment for the gluteal muscles. It is marked by three curved lines (inferior, anterior, and posterior gluteal lines (Fig. 6.5):
Ischial tuberosity
The ischial tuberosity is posteroinferior to the acetabulum and is associated mainly with the hamstring muscles of the posterior thigh (Fig. 6.6). It is divided into upper and lower areas by a transverse line.
Fig. 6.6 Ischial tuberosity. Posterolateral view.
The upper area of the ischial tuberosity is oriented vertically and is further subdivided into two parts by an oblique line, which descends, from medial to lateral, across the surface.
The lower area of the ischial tuberosity is oriented horizontally and is divided into medial and lateral regions by a ridge of bone.
When sitting, this medial part supports the body weight.
The sacrotuberous ligament is attached to a sharp ridge on the medial margin of the ischial tuberosity.
Ischiopubic ramus and pubic bone
The external surfaces of the ischiopubic ramus anterior to the ischial tuberosity and the body of the pubis provide attachment for muscles of the medial compartment of the thigh (Fig. 6.6).
Acetabulum
The large cup-shaped acetabulum for articulation with the head of the femur is on the lateral surface of the pelvic bone in the region where the ilium, pubis, and ischium fuse (Fig. 6.7).
Fig. 6.7 Acetabulum.
The margin of the acetabulum is marked inferiorly by a prominent notch (acetabular notch).
The wall of the acetabulum consists of nonarticular and articular parts:
 The nonarticular part is rough and forms a shallow circular depression (the acetabular fossa) in central and inferior parts of the acetabular floor; the acetabular notch is continuous with the acetabular fossa (Fig. 6.7).
The nonarticular part is rough and forms a shallow circular depression (the acetabular fossa) in central and inferior parts of the acetabular floor; the acetabular notch is continuous with the acetabular fossa (Fig. 6.7).
 The articular (lunate) surface is broad and surrounds the anterior, superior, and posterior margins of the acetabular fossa (Fig. 6.7).
The articular (lunate) surface is broad and surrounds the anterior, superior, and posterior margins of the acetabular fossa (Fig. 6.7).
The smooth crescent-shaped articular surface (the lunate surface) is broadest superiorly where most of the body’s weight is transmitted through the pelvis to the femur. The lunate surface is deficient inferiorly at the acetabular notch (Fig. 6.7).
The acetabular fossa provides attachment for the ligament of the head of the femur, whereas blood vessels and nerves pass through the acetabular notch.
Clinical app
Pelvic fractures
There are many ways of classifying pelvic fractures, which enable a surgeon to determine the appropriate treatment and the patient’s prognosis. The pelvic bones, sacrum, and associated joints form a bony ring surrounding the pelvic cavity.
Pelvic fractures are generally of four types.
 Type 4 injuries occur at and around the acetabulum.
Type 4 injuries occur at and around the acetabulum.
Other types of pelvic ring injuries include disruption of the sacroiliac joint with or without dislocation. This may involve significant visceral pelvic trauma and hemorrhage.
Other general pelvic injuries include stress fractures and insufficiency fractures, as seen in athletes and in elderly patients with osteoporosis, respectively.
Proximal femur
The femur is the bone of the thigh and the longest bone in the body. Its proximal end is characterized by a head and neck, and two large projections (the greater and lesser trochanters) on the upper part of the shaft (Fig. 6.8).
The head of the femur is spherical and articulates with the acetabulum of the pelvic bone. It is characterized by a nonarticular pit (fovea) on its medial surface for the attachment of the ligament of the head.
The neck of the femur is a cylindrical strut of bone that connects the head to the shaft of the femur. It projects superomedially from the shaft at an angle of approximately 125°, and projects slightly forward. The orientation of the neck relative to the shaft increases the range of movement of the hip joint.
The upper part of the shaft of the femur bears a greater and lesser trochanter, which are attachment sites for muscles that move the hip joint.
Greater and lesser trochanters
The greater trochanter extends superiorly from the shaft of the femur just lateral to the region where the shaft joins the neck of the femur (Fig. 6.8). It continues posteriorly where its medial surface is deeply grooved to form the trochanteric fossa. The lateral wall of this fossa bears a distinct oval depression for attachment of the obturator externus muscle.
The greater trochanter has an elongate ridge on its anterolateral surface for attachment of the gluteus minimus and a similar ridge more posteriorly on its lateral surface for attachment of the gluteus medius. Between these two points, the greater trochanter is palpable.
On the medial side of the superior aspect of the greater trochanter and just above the trochanteric fossa is a small impression for attachment of the obturator internus and its associated gemelli muscles, and immediately above and behind this feature is an impression on the margin of the trochanter for attachment of the piriformis muscle.
The lesser trochanter is smaller than the greater trochanter and has a blunt conical shape. It projects posteromedially from the shaft of femur just inferior to the junction with the neck (Fig. 6.8). It is the attachment site for the combined tendons of psoas major and iliacus muscles.
Extending between the two trochanters and separating the shaft from the neck of the femur are the intertrochanteric line and intertrochanteric crest.
Intertrochanteric line
The intertrochanteric line is a ridge of bone on the anterior surface of the upper margin of the shaft that descends medially from a tubercle on the anterior surface of the base of the greater trochanter to a position just anterior to the base of the lesser trochanter (Fig. 6.8). It is continuous with the pectineal line (spiral line), which curves medially under the lesser trochanter and around the shaft of the femur to merge with the medial margin of the linea aspera on the posterior aspect of the femur.
Intertrochanteric crest
The intertrochanteric crest is on the posterior surface of the femur and descends medially across the bone from the posterior margin of the greater trochanter to the base of the lesser trochanter (Fig. 6.8). It is a broad smooth ridge of bone with a prominent tubercle (the quadrate tubercle) on its upper half, which provides attachment for the quadratus femoris muscle.
Shaft of the femur
The shaft of the femur descends from lateral to medial in the coronal plane at an angle of 7° from the vertical axis (Fig. 6.9). The distal end of the femur is therefore closer to the midline than the upper end of the shaft.
Fig. 6.9 Shaft of the femur. On the right is a posterior view of proximal shaft of right femur.
The middle third of the shaft of the femur is triangular in shape with smooth lateral and medial margins between anterior, lateral (posterolateral), and medial (posteromedial) surfaces. The posterior margin is broad and forms a prominent raised crest (the linea aspera) (Fig. 6.9).
The linea aspera is a major site of muscle attachment in the thigh. In the proximal third of the femur, the medial and lateral margins of the linea aspera diverge and continue superiorly as the pectineal line and gluteal tuberosity, respectively (Fig. 6.9):
The gluteus maximus muscle is attached to the gluteal tuberosity.
The triangular area enclosed by the pectineal line, the gluteal tuberosity, and the intertrochanteric crest is the posterior surface of the proximal end of the femur (Fig. 6.9).
Clinical app
Femoral neck fractures
Femoral neck fractures (Fig. 6.10) can interrupt blood supply to the femoral head. Blood supply to the head and neck is primarily from an arterial ring formed around the base of the femoral neck. From here, vessels course along the neck, penetrate the capsule, and supply the femoral head. Blood supply to the femoral head and femoral neck is further enhanced by the artery of the ligamentum teres, which is generally small and variable. Femoral neck fractures may disrupt associated vessels and lead to necrosis of the femoral head.
Clinical app
Intertrochanteric fractures
In these fractures, the break usually runs from the greater trochanter through to the lesser trochanter and does not involve the femoral neck. Intertrochanteric fractures preserve the femoral neck blood supply and do not render the femoral head ischemic.
Clinical app
Femoral shaft fractures
An appreciable amount of energy is needed to fracture the femoral shaft. This type of injury is therefore accompanied by damage to the surrounding soft tissues, which include the muscle compartments and the structures they contain.
Hip joint
The hip joint is a synovial articulation between the head of the femur and the acetabulum of the pelvic bone (Fig. 6.11A; also see Fig. 6.16). The joint is a multiaxial ball and socket joint designed for stability and weightbearing at the expense of mobility.
When considering the effects of muscle action on the hip joint, the long neck of the femur and the angulation of the neck on the shaft of the femur must be kept in mind. For example, medial and lateral rotation of the femur involves muscles that move the greater trochanter forward and backward, respectively, relative to the acetabulum (Fig. 6.11B).
The articular surfaces of the hip joint are:
 the spherical head of the femur, and
the spherical head of the femur, and
 the lunate surface of the acetabulum of the pelvic bone (Fig. 6.12A).
the lunate surface of the acetabulum of the pelvic bone (Fig. 6.12A).
The acetabulum almost entirely encompasses the hemispherical head of the femur and contributes substantially to joint stability. The nonarticular acetabular fossa contains loose connective tissue. The lunate surface is covered by hyaline cartilage and is broadest superiorly (Fig. 6.12).
Except for the fovea, the head of the femur is also covered by hyaline cartilage.
The rim of the acetabulum is raised slightly by a fibrocartilaginous collar (the acetabular labrum). Inferiorly, the labrum bridges across the acetabular notch as the transverse acetabular ligament and converts the notch into a foramen (Fig. 6.12A).
The ligament of head of femur is a flat band of delicate connective tissue that attaches at one end to the fovea on the head of the femur and at the other end to the acetabular fossa, transverse acetabular ligament, and margins of the acetabular notch (Fig. 6.12B). It carries a small branch of the obturator artery, which contributes to the blood supply of the head of the femur.
The synovial membrane attaches to the margins of the articular surfaces of the femur and acetabulum, forms a tubular covering around the ligament of head of femur, and lines the fibrous membrane of the joint (Figs. 6.12B, 6.13). From its attachment to the margin of the head of the femur, the synovial membrane covers the neck of the femur before reflecting onto the fibrous membrane (Fig. 6.13).
Fig. 6.13 Synovial membrane of the hip joint.
The fibrous membrane that encloses the hip joint is strong and generally thick. Medially, it is attached to the margin of the acetabulum, the transverse acetabular ligament, and the adjacent margin of the obturator foramen (Fig. 6.14A). Laterally, it is attached to the intertrochanteric line on the anterior aspect of the femur and to the neck of the femur just proximal to the intertrochanteric crest on the posterior surface.
Ligaments
Three ligaments reinforce the external surface of the fibrous membrane and stabilize the joint: the iliofemoral, pubofemoral, and ischiofemoral ligaments.
 The iliofemoral ligament is anterior to the hip joint and is triangular-shaped (Fig. 6.14B). Its apex is attached to the ilium between the anterior inferior iliac spine and the margin of the acetabulum and its base is attached along the intertrochanteric line of the femur. Parts of the ligament attached above and below the intertrochanteric line are thicker than those attached to the central part of the line. This results in the ligament having a Y appearance.
The iliofemoral ligament is anterior to the hip joint and is triangular-shaped (Fig. 6.14B). Its apex is attached to the ilium between the anterior inferior iliac spine and the margin of the acetabulum and its base is attached along the intertrochanteric line of the femur. Parts of the ligament attached above and below the intertrochanteric line are thicker than those attached to the central part of the line. This results in the ligament having a Y appearance.
 The pubofemoral ligament is anteroinferior to the hip joint (Fig. 6.14B). It is also triangular in shape, with its base attached medially to the iliopubic eminence, adjacent bone, and obturator membrane. Laterally, it blends with the fibrous membrane and with the deep surface of the iliofemoral ligament.
The pubofemoral ligament is anteroinferior to the hip joint (Fig. 6.14B). It is also triangular in shape, with its base attached medially to the iliopubic eminence, adjacent bone, and obturator membrane. Laterally, it blends with the fibrous membrane and with the deep surface of the iliofemoral ligament.
 The ischiofemoral ligament reinforces the posterior aspect of the fibrous membrane (Fig. 6.14C). It is attached medially to the ischium, just posteroinferior to the acetabulum, and laterally to the greater trochanter deep to the iliofemoral ligament.
The ischiofemoral ligament reinforces the posterior aspect of the fibrous membrane (Fig. 6.14C). It is attached medially to the ischium, just posteroinferior to the acetabulum, and laterally to the greater trochanter deep to the iliofemoral ligament.
The fibers of all three ligaments are oriented in a spiral fashion around the hip joint so that they become taut when the joint is extended. This stabilizes the joint and reduces the amount of muscle energy required to maintain a standing position.
Blood supply and innervation
Vascular supply to the hip joint is predominantly through branches of the obturator artery, medial and lateral circumflex femoral arteries, superior and inferior gluteal arteries, and the first perforating branch of the deep artery of the thigh. The articular branches of these vessels form a network around the joint (Fig. 6.15).
Fig. 6.15 Blood supply of the hip joint.
The hip joint is innervated by articular branches from the femoral, obturator, and superior gluteal nerves, and the nerve to the quadratus femoris.
Imaging app
Visualizing the hip joint
Fig. 6.16 Hip joint. A. Normal hip joint. Radiograph, AP view. B. Hip joints. CT image in coronal plane.
Gateways to the lower limb
There are four major routes by which structures pass from the abdomen and pelvis into and out of the lower limb (Fig. 6.17):
 Greater sciatic foramen — formed on the posterolateral pelvic wall and is the major route for structures to pass between the pelvis and the gluteal region of the lower limb (Fig. 6.17). The piriformis muscle passes out of the pelvis into the gluteal region through the greater sciatic foramen and separates the foramen into two parts, a part above the muscle and a part below.
Greater sciatic foramen — formed on the posterolateral pelvic wall and is the major route for structures to pass between the pelvis and the gluteal region of the lower limb (Fig. 6.17). The piriformis muscle passes out of the pelvis into the gluteal region through the greater sciatic foramen and separates the foramen into two parts, a part above the muscle and a part below.
 Lesser sciatic foramen — inferior to the greater sciatic foramen on the posterolateral pelvic wall (Fig. 6.17). It is also inferior to the lateral attachment of the pelvic floor (levator ani and coccygeus muscles) to the pelvic wall and therefore connects the gluteal region with the perineum.
Lesser sciatic foramen — inferior to the greater sciatic foramen on the posterolateral pelvic wall (Fig. 6.17). It is also inferior to the lateral attachment of the pelvic floor (levator ani and coccygeus muscles) to the pelvic wall and therefore connects the gluteal region with the perineum.
 Gap between the inguinal ligament and pelvic bone — a large crescent-shaped gap between the inguinal ligament above and the anterosuperior margin of the pelvic bone below is the major route of communication between the abdomen and the anteromedial aspect of the thigh (Fig. 6.17).
Gap between the inguinal ligament and pelvic bone — a large crescent-shaped gap between the inguinal ligament above and the anterosuperior margin of the pelvic bone below is the major route of communication between the abdomen and the anteromedial aspect of the thigh (Fig. 6.17).
Fig. 6.17 Gateways to the lower limb.
Nerves
Nerves that enter the lower limb from the abdomen and pelvis are terminal branches of the lumbosacral plexus on the posterior wall of the abdomen and the posterolateral walls of the pelvis (Fig. 6.18).
Fig. 6.18 Branches of the lumbosacral plexus.
The lumbar plexus is formed by the anterior rami of spinal nerves L1 to L3 and part of L4. The rest of the anterior ramus of L4 and the anterior ramus of L5 combine to form the lumbosacral trunk, which enters the pelvic cavity and joins with the anterior rami of S1 to S3 and part of S4 to form the sacral plexus.
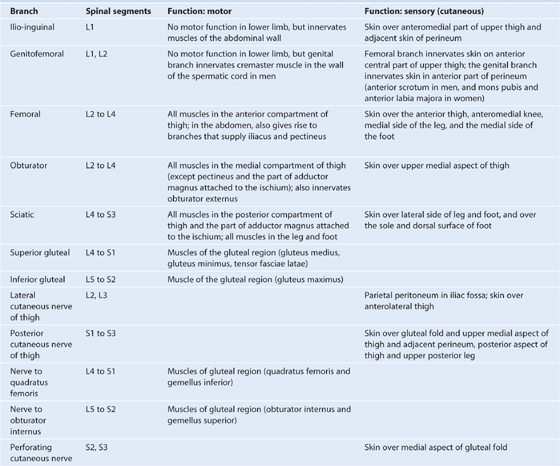
Nerves that originate from the lumbosacral plexus and that leave the abdomen and pelvis to enter the lower limb are indicated in Fig. 6.18 and described in Table 6.1, p. 278.
Table 6.1 Branches of the lumbosacral plexus associated with the lower limb
Arteries
Femoral artery
The major artery supplying the lower limb is the femoral artery (Fig. 6.19), which is the continuation of the external iliac artery in the abdomen. The external iliac artery becomes the femoral artery as the vessel passes under the inguinal ligament to enter the femoral triangle in the anterior aspect of the thigh. Branches supply most of the thigh and all of the leg and foot.
Fig. 6.19 Arteries of the lower limb.
Superior and inferior gluteal arteries and the obturator artery
The superior and inferior gluteal arteries originate in the pelvic cavity as branches of the internal iliac artery (Fig. 6.19, see pp. 240-241) and supply the gluteal region. The superior gluteal artery leaves the pelvis through the greater sciatic foramen above the piriformis muscle and the inferior gluteal artery leaves through the same foramen, but below the piriformis muscle.
The obturator artery is also a branch of the internal iliac artery in the pelvic cavity (p. 241) and passes through the obturator canal to enter and supply the medial compartment of the thigh (Fig. 6.19).
Branches of the femoral, inferior gluteal, superior gluteal, and obturator arteries, together with branches from the internal pudendal artery of the perineum, interconnect to form an anastomotic network in the upper thigh and gluteal region. The presence of these anastomotic channels may provide collateral circulation when one of the vessels is interrupted.
Veins
Veins draining the lower limb form superficial and deep groups (Fig. 6.20).
Fig. 6.20 Veins of the lower limb.
The deep veins generally follow the arteries (femoral, superior gluteal, inferior gluteal, and obturator). The major deep vein draining the limb is the femoral vein (Fig. 6.20). It becomes the external iliac vein when it passes under the inguinal ligament to enter the abdomen.
The superficial veins are in the subcutaneous connective tissue and are interconnected with and ultimately drain into the deep veins. The superficial veins form two major channels—the great saphenous vein and the small saphenous vein. Both veins originate from a dorsal venous arch in the foot (Fig. 6.20):
 The great saphenous vein originates from the medial side of the dorsal venous arch, and then ascends up the medial side of the leg, knee, and thigh to connect with the femoral vein just inferior to the inguinal ligament.
The great saphenous vein originates from the medial side of the dorsal venous arch, and then ascends up the medial side of the leg, knee, and thigh to connect with the femoral vein just inferior to the inguinal ligament.
Clinical app
Varicose veins
The normal flow of blood in the venous system depends on the presence of competent valves, which prevent reflux. Venous return is supplemented with contraction of the muscles in the lower limb, which pump the blood toward the heart. When venous valves become incompetent they tend to place extra pressure on more distal valves, which may also become incompetent. This condition produces dilated tortuous superficial veins (varicose veins) in the distribution of the great (long) and small (short) saphenous venous systems.
Clinical app
Deep vein thrombosis
Thrombosis resulting from venous stasis, injury to the vessel wall, or hypercoagulable states may occur in the deep veins of the lower limb and within the pelvic veins.
In some patients a deep vein thrombosis (DVT) in the veins of the leg may propagate into the femoral veins. This clot may break off and pass through the heart to enter the pulmonary circulation, resulting in occlusion of the pulmonary artery (pulmonary embolism), cardiopulmonary arrest, and death.
Clinical app
Harvesting veins for grafts
Vein grafts have long been used for vascular conduits. Superficial veins of the arms and legs are harvested and used to bypass areas of arterial occlusion and stenoses. Typically vein bypass grafts are used for coronary artery bypass surgery and to bypass areas of vascular occlusion in the lower limb.
The commonest vein used for bypass grafting is the great saphenous vein. A long incision is required to obtain access to the vein and after tributaries of the vein are ligated, the vein is removed.
It is important to remember that veins contain valves and in order to use the vein as an appropriate conduit, it must either be reversed or, using special surgical techniques, the valves can be obliterated.
In coronary artery bypass grafting the vein is anastomosed to the ascending arch of the aorta and then anastomosed distal to the regions of occlusion on the coronary vessels. Similarly, in lower limb ischemic disease the vein can be used to bypass the regions of stenosis and occlusion within the femoral artery and the distal branches.
Lymphatics
Most lymphatic vessels in the lower limb drain into superficial and deep inguinal nodes located in the fascia just inferior to the inguinal ligament (Fig. 6.21).
Fig. 6.21 Lymphatic drainage of the lower limb.
Superficial inguinal nodes
The superficial inguinal nodes, approximately 10 in number, are in the superficial fascia and parallel the course of the inguinal ligament in the upper thigh (Fig. 6.21). Medially, they extend inferiorly along the terminal part of the great saphenous vein.
Superficial inguinal nodes receive lymph from the gluteal region, lower abdominal wall, perineum, and superficial regions of the lower limb. They drain, via vessels that accompany the femoral vessels, into external iliac nodes associated with the external iliac artery in the abdomen.
Deep inguinal nodes
The deep inguinal nodes, up to three in number, are medial to the femoral vein (Fig. 6.21).
Popliteal nodes
In addition to the inguinal nodes, there is a small collection of deep nodes posterior to the knee close to the popliteal vessels (Fig. 6.21). These popliteal nodes receive lymph from superficial vessels, which accompany the small saphenous vein, and from deep areas of the leg and foot. They ultimately drain into the deep and superficial inguinal nodes.
Deep fascia and the saphenous opening
Fascia lata
The outer layer of deep fascia in the lower limb forms a thick “stocking-like” membrane, which covers the limb and lies beneath the superficial fascia (Fig. 6.22A). This deep fascia is particularly thick in the thigh and gluteal region and is termed the fascia lata.
Fig. 6.22 Fascia lata. A. Right limb. Anterior view. B. Left limb. Lateral view.
The fascia lata is anchored superiorly to bone and soft tissues along a line of attachment that defines the upper margin of the lower limb.
Inferiorly, the fascia lata is continuous with the deep fascia of the leg.
Iliotibial tract
The fascia lata is thickened laterally into a longitudinal band (the iliotibial tract), which descends along the lateral margin of the limb from the tuberculum of iliac crest to a bony attachment just below the knee (Fig. 6.22B).
The superior aspect of the fascia lata in the gluteal region splits anteriorly to enclose the tensor fasciae latae muscle and posteriorly to enclose the gluteus maximus muscle:
 Most of the gluteus maximus muscle inserts into the posterior aspect of the iliotibial tract.
Most of the gluteus maximus muscle inserts into the posterior aspect of the iliotibial tract.
The tensor fasciae latae and gluteus maximus muscles, working through their attachments to the iliotibial tract, hold the leg in extension once other muscles have extended the leg at the knee joint. The iliotibial tract and its two associated muscles also stabilize the hip joint by preventing lateral displacement of the proximal end of the femur away from the acetabulum.
Saphenous opening
The fascia lata has one prominent aperture on the anterior aspect of the thigh just inferior to the medial end of the inguinal ligament (the saphenous opening), which allows the great saphenous vein to pass from superficial fascia through the deep fascia to connect with the femoral vein (Fig. 6.23).
Fig. 6.23 Saphenous opening. Anterior view.
Femoral triangle
The femoral triangle is a wedge-shaped depression formed by muscles in the upper thigh at the junction between the anterior abdominal wall and the lower limb (Fig. 6.24):
 The base of the triangle is the inguinal ligament.
The base of the triangle is the inguinal ligament.
Fig. 6.24 Boundaries of the femoral triangle.
The femoral nerve, artery, and vein, and lymphatics pass between the abdomen and lower limb under the inguinal ligament and in the femoral triangle (Fig. 6.25). The femoral artery and vein pass inferiorly through the adductor canal and become the popliteal vessels behind the knee where they meet and are distributed with branches of the sciatic nerve, which descends through the posterior thigh from the gluteal region.
Fig. 6.25 Contents of the femoral triangle.
From lateral to medial, major structures in the femoral triangle are the femoral nerve, the femoral artery, the femoral vein, and lymphatic vessels (Fig. 6.25).
Femoral sheath
In the femoral triangle, the femoral artery and vein and the associated lymphatic vessels are surrounded by a funnel-shaped sleeve of fascia (the femoral sheath) (Fig. 6.25). The sheath is continuous superiorly with the transversalis fascia and iliacus fascia of the abdomen and merges inferiorly with connective tissue associated with the vessels. Each of the three structures surrounded by the sheath is contained within a separate fascial compartment within the sheath. The most medial compartment (the femoral canal) contains the lymphatic vessels and is conical in shape. The opening of this canal superiorly is potentially a weak point in the lower abdomen and is the site for femoral hernias. The femoral nerve is lateral to and not contained within the femoral sheath.
Surface anatomy
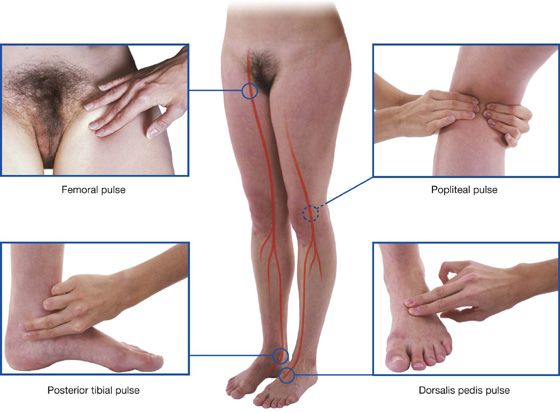
Finding the femoral artery in the femoral triangle
The femoral artery descends into the thigh from the abdomen by passing under the inguinal ligament and into the femoral triangle (Fig. 6.26). In the femoral triangle, its pulse is easily felt just inferior to the inguinal ligament midway between the pubic symphysis and the anterior superior iliac spine. Medial to the artery is the femoral vein and medial to the vein is the femoral canal, which contains lymphatics and lies immediately lateral to the pubic tubercle. The femoral nerve lies lateral to the femoral artery.
Fig. 6.26 Position of the femoral artery in the femoral triangle.
Clinical app
Vascular access in the lower limb
The femoral artery and vein are easily accessible in the femoral triangle.
Many radiological procedures involve catheterization of the femoral artery or the femoral vein to obtain access to the contralateral lower limb, the ipsilateral lower limb, the vessels of the thorax and abdomen, and even the cerebral vessels.
Cardiologists also can use the femoral artery to place catheters in vessels around the arch of the aorta and into the coronary arteries to perform coronary angiography and angioplasty.
GLUTEAL REGION
The gluteal region lies posterolateral to the bony pelvis and the proximal end of the femur (Fig. 6.27). Muscles in the region mainly abduct, extend, and laterally rotate the femur relative to the pelvic bone.
Fig. 6.27 Gluteal region. Posterior view.
The gluteal region communicates anteromedially with the pelvic cavity and perineum through the greater and lesser sciatic foramina, respectively (Fig. 6.27). Inferiorly, it is continuous with the posterior thigh.
Muscles
Muscles of the gluteal region (Table 6.2, Fig. 6.28) compose mainly two groups:
Table 6.2 Muscles of the gluteal region (spinal segments in bold are the major segments innervating the muscle)
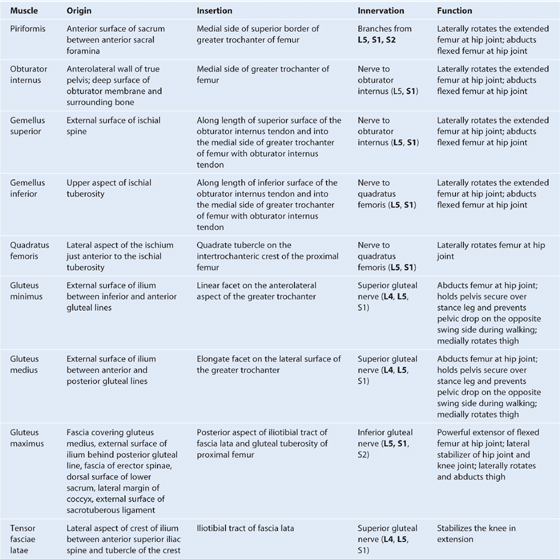
Fig. 6.28 Deep muscles in the gluteal region. A. Posterior view. B. Function.
The piriformis muscle is the most superior of the deep group of muscles (Fig. 6.28A) and is a muscle of the pelvic wall and of the gluteal region. It originates from between the anterior sacral foramina on the anterolateral surface of the sacrum and passes laterally and inferiorly through the greater sciatic foramen. Piriformis is an important landmark because it divides the greater sciatic foramen into two regions, one above and one below the piriformis.
The obturator internus muscle, like the piriformis muscle, is a muscle of the pelvic wall and of the gluteal region (Fig. 6.28A). The muscle fibers of the obturator internus converge to form a tendon, which bends 90° around the ischium between the ischial spine and ischial tuberosity, and passes through the lesser sciatic foramen to enter the gluteal region. Gemellus superior and inferior (gemelli is Latin for “twins”) are a pair of triangular muscles associated with the upper and lower margins of the obturator internus tendon (Fig. 6.28A).
The gluteus medius and minimus muscles abduct the pelvis over the stance limb at the hip joint and reduce pelvic drop over the opposite swing limb during walking (Fig. 6.28B).
Clinical app
Trendelenburg’s sign
Trendelenburg’s sign occurs in people with weak or paralyzed abductor muscles (gluteus medius and gluteus minimus) of the hip. The sign is demonstrated by asking the patient to stand on one limb. When standing on the affected limb, the pelvis severely drops over the swing limb.
Positive findings are typically found in patients with damage to the superior gluteal nerve. Damage to this nerve may occur with associated pelvic fractures, space occupying lesions within the pelvis extending into the greater sciatic foramen and in some cases relating to hip surgery where there has been atrophy and disruption of the insertion of the gluteus medius and gluteus minimus tendons on the greater trochanter.
In patients with a positive Trendelenburg’s sign, gait also is abnormal. Typically during the stance phase of the affected limb, the weakened abductor muscles allow the pelvis to tilt inferiorly over the swing limb. The patient compensates for the pelvic drop by lurching the trunk to the affected side in order to maintain the level of the pelvis throughout the gait cycle.
Gluteus maximus is the largest muscle in the gluteal region and overlies most of the other gluteal muscles (Fig. 6.29). It is quadrangular in shape and has a broad origin from the bony pelvis and associated ligaments and fascia. It is often described as being enclosed within two layers of the fascia lata, which covers the thigh and gluteal region. Laterally, the upper and superficial lower parts of the gluteus maximus insert into the iliotibial tract, which passes over the lateral surface of the greater trochanter and descends down the thigh and into the upper leg. Deep distal parts of the muscle attach to the elongate gluteal tuberosity of the proximal femur.
Fig. 6.29 Gluteus maximus muscle. Posterior view.
Nerves
Superior gluteal nerve
Of all the nerves that pass through the greater sciatic foramen, the superior gluteal nerve is the only one that passes above the piriformis muscle (Fig. 6.30A). After entering the gluteal region, the nerve loops up over the inferior margin of gluteus minimus and travels anteriorly and laterally in the plane between the gluteus minimus and medius muscles.
Fig. 6.30 Nerves of the gluteal region.
The superior gluteal nerve supplies branches to the gluteus minimus and medius muscles and terminates by innervating the tensor fasciae latae muscle.
Sciatic nerve
The sciatic nerve enters the gluteal region through the greater sciatic foramen inferior to the piriformis muscle (Fig. 6.30A). It descends in the plane between the superficial and deep group of gluteal region muscles, crossing the posterior surfaces of first the obturator internus and associated gemellus muscles and then the quadratus femoris muscle. It lies just deep to the gluteus maximus at the midpoint between the ischial tuberosity and the greater trochanter. At the lower margin of the quadratus femoris muscle, the sciatic nerve enters the posterior thigh.
The sciatic nerve is the largest nerve in the body and innervates all muscles in the posterior compartment of the thigh that flex the knee and all muscles that work the ankle and foot. It also innervates a large area of skin in the lower limb.
Nerve to quadratus femoris
The nerve to the quadratus femoris enters the gluteal region through the greater sciatic foramen inferior to the piriformis muscle and deep to the sciatic nerve (Fig. 6.30). Unlike other nerves in the gluteal region, the nerve to the quadratus femoris lies anterior to the plane of the deep muscles.
The nerve to the quadratus femoris descends along the ischium deep to the tendon of the obturator internus muscle and associated gemellus muscles to penetrate and innervate the quadratus femoris. It supplies a small branch to the gemellus inferior.
Nerve to obturator internus
The nerve to the obturator internus enters the gluteal region through the greater sciatic foramen inferior to the piriformis muscle and between the posterior cutaneous nerve of the thigh and the pudendal nerve (Fig. 6.30). It supplies a small branch to the gemellus superior and then passes over the ischial spine and through the lesser sciatic foramen to innervate the obturator internus muscle from the medial surface of the muscle in the perineum.
Posterior cutaneous nerve of the thigh
The posterior cutaneous nerve of the thigh enters the gluteal region through the greater sciatic foramen inferior to the piriformis muscle and immediately medial to the sciatic nerve (Fig. 6.30). It descends through the gluteal region just deep to the gluteus maximus and enters the posterior thigh.
The posterior cutaneous nerve of the thigh has a number of gluteal branches, which loop around the lower margin of the gluteus maximus muscle to innervate skin over the gluteal fold. A small perineal branch passes medially to contribute to the innervation of skin of the scrotum or labia majora in the perineum. The main trunk of the posterior cutaneous nerve of the thigh passes inferiorly, giving rise to branches that innervate skin on the posterior thigh and leg.
Pudendal nerve
The pudendal nerve enters the gluteal region through the greater sciatic foramen inferior to the piriformis muscle and medial to the sciatic nerve (Fig. 6.30). It passes over the sacrospinous ligament and immediately passes through the lesser sciatic foramen to enter the perineum. The course of the pudendal nerve in the gluteal region is short and the nerve is often hidden by the overlying upper margin of the sacrotuberous ligament.
The pudendal nerve is the major somatic nerve of the perineum and has no branches in the gluteal region.
Inferior gluteal nerve
The inferior gluteal nerve enters the gluteal region through the greater sciatic foramen inferior to the piriformis muscle and along the posterior surface of the sciatic nerve (Fig. 6.30). It penetrates and supplies the gluteus maximus muscle.
Perforating cutaneous nerve
The perforating cutaneous nerve is the only nerve in the gluteal region that does not enter the area through the greater sciatic foramen. It is a small nerve that leaves the sacral plexus in the pelvic cavity by piercing the sacrotuberous ligament. It then loops around the lower border of the gluteus maximus to supply skin over the medial aspect of the gluteus maximus (Fig. 6.30).
Clinical app
Intramuscular injection in the gluteal region: avoiding the sciatic nerve
From time to time it is necessary to administer drugs intramuscularly; that is, by direct injection into muscles. This procedure must be carried out without injuring neurovascular structures. A typical site for an intramuscular injection is the gluteal region. The sciatic nerve passes through this region and needs to be avoided. The safest place to inject is the upper outer quadrant of either gluteal region.
The gluteal region can be divided into quadrants by two imaginary lines positioned using palpable bony landmarks (Fig. 6.31).
Fig. 6.31 Site for intramuscular injections.
One line descends vertically from the highest point of the iliac crest.
The other line passes horizontally through the first line midway between the highest point of the iliac crest and the horizontal plane through the ischial tuberosity.
It is important to remember that the gluteal region extends as far forward as the anterior superior iliac spine. The sciatic nerve curves through the upper lateral corner of the lower medial quadrant and descends along the medial margin of the lower lateral quadrant.
Occasionally, the sciatic nerve bifurcates into its tibial and common fibular branches in the pelvis, in which case the common fibular nerve passes into the gluteal region through, or even above, the piriformis muscle.
The anterior corner of the upper lateral quadrant is normally used for injections to avoid injuring any part of the sciatic nerve or other nerves and vessels in the gluteal region. A needle placed in this region enters the gluteus medius anterosuperior to the margin of the gluteus maximus.
Arteries
Inferior gluteal artery
The inferior gluteal artery originates from the anterior trunk of the internal iliac artery in the pelvic cavity. It leaves the pelvic cavity through the greater sciatic foramen inferior to the piriformis muscle (Fig. 6.32).
Fig. 6.32 Arteries of the gluteal region.
The inferior gluteal artery supplies adjacent muscles and descends through the gluteal region and into the posterior thigh where it supplies adjacent structures and anastomoses with perforating branches of the femoral artery. It also supplies a branch to the sciatic nerve.
Superior gluteal artery
The superior gluteal artery originates from the posterior trunk of the internal iliac artery in the pelvic cavity. It leaves the pelvic cavity through the greater sciatic foramen above the piriformis muscle (Fig. 6.32). In the gluteal region, it divides into a superficial branch and a deep branch:
 The superficial branch passes onto the deep surface of the gluteus maximus muscle.
The superficial branch passes onto the deep surface of the gluteus maximus muscle.
 The deep branch passes between the gluteus medius and minimus muscles.
The deep branch passes between the gluteus medius and minimus muscles.
In addition to adjacent muscles, the superior gluteal artery contributes to the supply of the hip joint. Branches of the artery also anastomose with the lateral and medial femoral circumflex arteries from the deep femoral artery in the thigh, and with the inferior gluteal artery (Fig. 6.33).
Veins
Inferior and superior gluteal veins follow the inferior and superior gluteal arteries into the pelvis where they join the pelvic plexus of veins. Peripherally, the veins anastomose with superficial gluteal veins, which ultimately drain anteriorly into the femoral vein.
Lymphatics
Deep lymphatic vessels of the gluteal region accompany the blood vessels into the pelvic cavity and connect with internal iliac nodes.
Superficial lymphatics drain into the superficial inguinal nodes on the anterior aspect of the thigh.
THIGH
The thigh is the region of the lower limb that is approximately between the hip and knee joints (Fig. 6.34):
 Anteriorly, it is separated from the abdominal wall by the inguinal ligament.
Anteriorly, it is separated from the abdominal wall by the inguinal ligament.
Fig. 6.34 Thigh. A. Posterior view. B. Anterior view. C. Cross-section through the midthigh.
Structures enter and leave the top of the thigh by three routes:
 Posteriorly, the thigh is continuous with the gluteal region and the major structure passing between the two regions is the sciatic nerve (Fig. 6.34A).
Posteriorly, the thigh is continuous with the gluteal region and the major structure passing between the two regions is the sciatic nerve (Fig. 6.34A).
 Anteriorly, the thigh communicates with the abdominal cavity through the aperture between the inguinal ligament and pelvic bone (Fig. 6.34B), and major structures passing through this aperture are the iliopsoas and pectineus muscles, the femoral nerve, artery and vein, and lymphatic vessels.
Anteriorly, the thigh communicates with the abdominal cavity through the aperture between the inguinal ligament and pelvic bone (Fig. 6.34B), and major structures passing through this aperture are the iliopsoas and pectineus muscles, the femoral nerve, artery and vein, and lymphatic vessels.
 Medially, structures (including the obturator nerve and associated vessels) pass between the thigh and pelvic cavity through the obturator canal (Fig. 6.34B).
Medially, structures (including the obturator nerve and associated vessels) pass between the thigh and pelvic cavity through the obturator canal (Fig. 6.34B).
The thigh is divided into three compartments (anterior, medial, and posterior) by intermuscular septa between the posterior aspect of the femur and the fascia lata (the thick layer of deep fascia that completely surrounds or invests the thigh; Fig. 6.34C).
Bones
The skeletal support for the thigh is the femur (Fig. 6.35). Most of the large muscles in the thigh insert into the proximal ends of the two bones of the leg (tibia and fibula), and flex and extend the leg at the knee joint. The distal end of the femur provides origin for the gastrocnemius muscles, which are predominantly in the posterior compartment of the leg and plantarflex the foot.
Shaft and distal end of femur
The shaft of femur is bowed forward and has an oblique course from the neck of the femur to the distal end (Fig. 6.35A, B). As a consequence of this oblique orientation, the knee is close to the midline under the body’s center of gravity.
The middle part of the shaft of femur is triangular in cross-section (Fig. 6.35D). In the middle part of the shaft, the femur has smooth medial (posteromedial), lateral (posterolateral), and anterior surfaces and medial, lateral, and posterior borders. The medial and lateral borders are rounded, whereas the posterior border forms a broad roughened crest—the linea aspera (Fig. 6.35C).
In proximal and distal regions of the femur, the linea aspera widens to form an additional posterior surface. At the distal end of the femur, this posterior surface forms the floor of the popliteal fossa and its margins, which are continuous with the linea aspera above, form the medial and lateral supracondylar lines. The medial supracondylar line terminates at a prominent tubercle (the adductor tubercle) on the superior aspect of the medial condyle of the distal end. Just lateral to the lower end of the medial supracondylar line is an elongate roughened area of bone for the proximal attachment of the medial head of the gastrocnemius muscle (Fig. 6.35).
The distal end of femur is characterized by two large condyles, which articulate with the proximal head of the tibia (Fig. 6.35). The condyles are separated posteriorly by an intercondylar fossa and are joined anteriorly where they articulate with the patella.
The surfaces of the condyles that articulate with the tibia are rounded posteriorly and become flatter inferiorly. On each condyle, a shallow oblique groove separates the surface that articulates with the tibia from the more anterior surface that articulates with the patella. The surfaces of the medial and lateral condyles that articulate with the patella form a V-shaped trench, which faces anteriorly. The lateral surface of the trench is larger and steeper than the medial surface.
The walls of the intercondylar fossa bear two facets for the superior attachment of the cruciate ligaments, which stabilize the knee joint (Fig. 6.35C).
Epicondyles, for the attachment of collateral ligaments of the knee joint, are bony elevations on the nonarticular outer surfaces of the condyles (Fig. 6.35).
Additionally, just posterosuperior to the medial epicondyle is the adductor tubercle and just posterior to the lateral epicondyle are facets for the attachment of the lateral head of the gastrocnemius and the popliteus muscles (Fig. 6.35C).
Patella
The patella (knee cap) is the largest sesamoid bone (a bone formed within the tendon of a muscle) in the body and is formed within the tendon of the quadriceps femoris muscle as it crosses anterior to the knee joint to insert on the tibia.
The patella is triangular (Fig. 6.36):
 Its base is broad and thick for the attachment of the quadriceps femoris muscle from above.
Its base is broad and thick for the attachment of the quadriceps femoris muscle from above.
 Its posterior surface articulates with the femur and has medial and lateral facets (Fig. 6.36B), which slope away from a raised smooth ridge—the lateral facet is larger than the medial facet for articulation with the larger corresponding surface on the lateral condyle of the femur.
Its posterior surface articulates with the femur and has medial and lateral facets (Fig. 6.36B), which slope away from a raised smooth ridge—the lateral facet is larger than the medial facet for articulation with the larger corresponding surface on the lateral condyle of the femur.
Fig. 6.36 Patella. A. Anterior view. B. Posterior view. C. Superior view.
Proximal end of tibia
The tibia is the medial and larger of the two bones in the leg, and is the only one that articulates with the femur at the knee joint.
The proximal end of the tibia is expanded in the transverse plane for weight bearing and consists of a medial condyle and a lateral condyle, which are both flattened in the horizontal plane and overhang the shaft (Fig. 6.37).
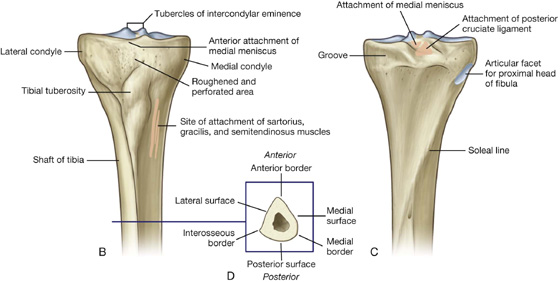
The superior surfaces of the medial and lateral condyles are articular and separated by an intercondylar region, which contains sites of attachment for the cruciate ligaments and interarticular cartilages (menisci) of the knee joint (Fig. 6.37A).
The articular surfaces of the medial and lateral condyles and the intercondylar region together form a “tibial plateau,” which articulates with and is anchored to the distal end of the femur. Inferior to the condyles on the proximal part of the shaft is a large tibial tuberosity and the roughening for muscle and ligament attachments.
Tibial condyles and intercondylar areas
The tibial condyles are thick horizontal discs of bone attached to the top of the tibial shaft (Fig. 6.37).
The medial condyle is larger than the lateral condyle and is better supported over the shaft of the tibia. Its superior surface is oval for articulation with the medial condyle of the femur (Fig. 6.37A). The articular surface extends laterally onto the side of the raised medial intercondylar tubercle.
The superior surface of the lateral condyle is circular and articulates above with the lateral condyle of the femur (Fig. 6.37A). The medial edge of this surface extends onto the side of the lateral intercondylar tubercle.
The superior articular surfaces of both the lateral and medial condyles are concave, particularly centrally. The outer margins of the surfaces are flatter and are the regions in contact with the interarticular discs (menisci) of fibrocartilage in the knee joint.
The nonarticular posterior surface of the medial condyle bears a distinct horizontal groove for part of the attachment of the semimembranosus muscle, and the undersurface of the lateral condyle bears a distinct circular facet for articulation with the proximal head of the fibula.
The intercondylar region of the tibial plateau lies between the articular surfaces of the medial and lateral condyles (Fig. 6.37). It is narrow centrally where it is raised to form the intercondylar eminence, the sides of which are elevated further to form medial and lateral intercondylar tubercles.
The intercondylar region bears six distinct facets (Fig. 6.37A) for the attachment of menisci and cruciate ligaments. In addition to these facets, a large anterolateral region of the anterior intercondylar area is roughened and perforated by numerous small nutrient foramina for blood vessels. This region is continuous with a similar surface on the front of the tibia above the tuberosity and lies against infrapatellar connective tissue.
Tibial tuberosity
The tibial tuberosity is a palpable inverted triangular area on the anterior aspect of the tibia below the site of junction between the two condyles (Fig. 6.37A, B). It is the site of attachment for the patellar ligament, which is a continuation of the quadriceps femoris tendon below the patella.
Shaft of tibia
The shaft of the tibia is triangular in cross-section and has three surfaces (posterior, medial, and lateral) and three borders (anterior, interosseous, and medial) (Fig. 6.37D):
The large medial surface of the shaft of the tibia, between the anterior and medial borders, is smooth and subcutaneous, and is palpable along almost its entire extent. Medial and somewhat inferior to the tibial tuberosity, this medial surface bears a subtle, slightly roughened elongate elevation. This elevation is the site of the combined attachment of three muscles (sartorius, gracilis, and semitendinosus), which descend from the thigh (Fig. 6.37B).
The posterior surface of the shaft of the tibia, between the interosseous and medial borders, is widest superiorly where it is crossed by a roughened oblique line (the soleal line) (Fig. 6.37C).
The lateral surface, between the anterior and interosseous borders, is smooth and unremarkable.
Proximal end of fibula
The fibula is the lateral bone of the leg and does not take part in formation of the knee joint or in weight bearing. It is much smaller than the tibia and has a small proximal head, a narrow neck, and a delicate shaft, which ends as the lateral malleolus at the ankle.
The head of the fibula is a globe-shaped expansion at the proximal end of the fibula (Fig. 6.38). A circular facet on the superomedial surface is for articulation above with a similar facet on the inferior aspect of the lateral condyle of the tibia. Just posterolateral to this facet, the bone projects superiorly as a blunt apex (styloid process).
Fig. 6.38 Proximal end of the fibula. A. Anterior view. B. Cross-section through the shaft of fibula.
The neck of the fibula separates the expanded head from the shaft. The common fibular nerve lies against the posterolateral aspect of the neck.
Like the tibia, the shaft of the fibula has three borders (anterior, posterior, and interosseous) and three surfaces (lateral, posterior, and medial), which lie between the borders (Fig. 6.38B):
 The anterior border is sharp midshaft and begins superiorly from the anterior aspect of the head.
The anterior border is sharp midshaft and begins superiorly from the anterior aspect of the head.
 The posterior border is rounded and descends from the region of the styloid process of the head.
The posterior border is rounded and descends from the region of the styloid process of the head.
 The interosseous border is medial in position.
The interosseous border is medial in position.
The three surfaces of the fibula are associated with the three muscular compartments (lateral, posterior, and anterior) of the leg.
Muscles
Muscles of the thigh are arranged in three compartments (anterior, medial, and posterior) separated by intermuscular septa (Fig. 6.39).
Fig. 6.39 Transverse section through the midthigh.
Anterior compartment (Table 6.3, Fig. 6.40)
Table 6.3 Muscles of the anterior compartment of thigh (spinal segments in bold are the major segments innervating the muscle)
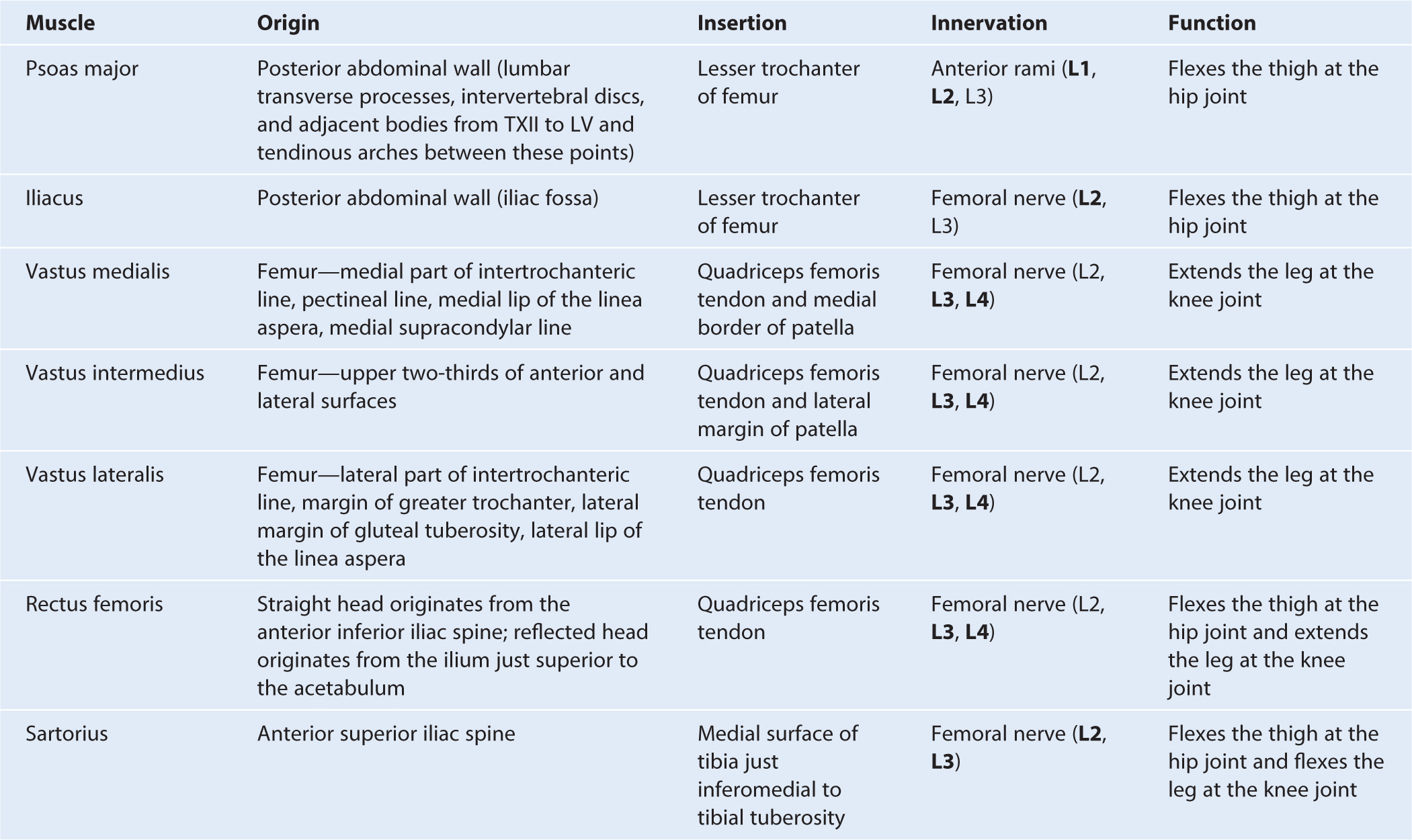
Fig. 6.40 Muscles of the anterior compartment of thigh.
The anterior compartment of thigh contains the sartorius and the four large quadriceps femoris muscles (rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius). All are innervated by the femoral nerve. A tiny muscle (articularis genus), which is often part of the vastus intermedius muscle, originates from the femur just inferior to the origin of the vastus intermedius and inserts into the suprapatellar bursa associated with the knee joint. This articular muscle pulls the bursa away from the knee joint during extension. In addition to these muscles, the terminal ends of the psoas major and iliacus muscles pass into the upper part of the anterior compartment from sites of origin on the posterior abdominal wall (Fig. 6.41). These muscles are innervated by branches directly from the anterior rami of L1 to L3 (psoas major) or from the femoral nerve (iliacus) as it passes down the abdominal wall.
Fig. 6.41 Psoas major and iliacus muscles.
The sartorius muscle together with gracilis, and semitendinosus muscles from the medial and posterior compartments, respectively, attach to the tibia as part of a three-pronged pattern on the tibia. These combined tendons of insertion are often termed the pes anserinus (Latin for “goose foot”) (Fig. 6.40).
Muscles in the anterior compartment act on the hip and knee joints:
 Psoas major and iliacus act on the hip joint.
Psoas major and iliacus act on the hip joint.
 Sartorius and rectus femoris act on both the hip and knee joints.
Sartorius and rectus femoris act on both the hip and knee joints.
 The vastus muscles act on the knee joint.
The vastus muscles act on the knee joint.
Clinical app
Quadriceps injury
Quadriceps muscle injuries include avulsion of the straight and reflected head of the rectus femoris muscles, proximal musculotendinous muscle tears and quadriceps tendon disruption. Proximal injuries of the straight and reflected heads of the rectus femoris are uncommon. However, in adolescents it is possible to avulse these origins with a small fragment of bone. This can cause considerable pain and may result in the growth of a prominent bony tubercle.
Proximal injuries of the rectus femoris muscle occur very frequently in professional athletes and are the second most common thigh injury.
Quadriceps tendon disruption is a devastating injury. A typical history is “miss-kicking” a ball and hitting the ground, producing an abrupt deceleration and resulting in tearing the quadriceps tendon. Examination demonstrates that the patient is unable to extend the knee against resistance and in most cases a gap in the tendon can be palpated. In most instances, surgery is required to reattach the tendon to the patella.
Patellar ligament
The patellar ligament is functionally the continuation of the quadriceps femoris tendon below the patella and is attached above to the apex and margins of the patella and below to the tibial tuberosity (Fig. 6.40). The more superficial fibers of the quadriceps femoris tendon and the patellar ligament are continuous over the anterior surface of the patella, and lateral and medial fibers are continuous with the ligament beside the margins of the patella.
Medial compartment (Table 6.4, Fig. 6.42)
Table 6.4 Muscles of the medial compartment of thigh (spinal segments in bold are the major segments innervating the muscle)
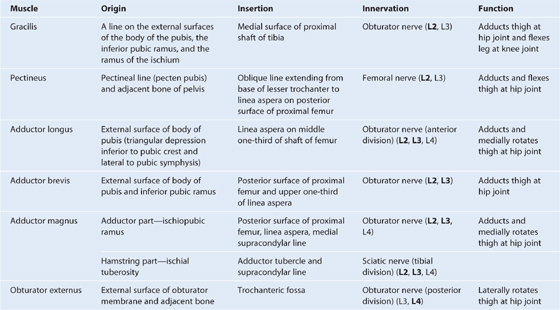
Fig. 6.42 Muscles of the medial compartment of thigh. Anterior view.
The medial compartment of thigh contains six muscles (gracilis, pectineus, adductor longus, adductor brevis, adductor magnus, and obturator externus). All except the pectineus, which is innervated by the femoral nerve, and part of the adductor magnus, which is innervated by the sciatic nerve, are innervated by the obturator nerve. Collectively, all these muscles except the obturator externus mainly adduct the thigh at the hip joint; the adductor longus and magnus may also medially rotate the thigh. Obturator externus is a lateral rotator of the thigh at the hip joint and the gracilis also flexes the leg at the knee joint.
The adductor magnus is the largest and deepest of the muscles in the medial compartment of thigh (Fig. 6.43). The muscle forms the distal posterior wall of the adductor canal. It is a triangular or fan-shaped muscle anchored by its apex to the pelvis and attached by its expanded base to the femur. The medial part of the adductor magnus, often called the “hamstring part,” originates from the ischial tuberosity of the pelvic bone and descends almost vertically along the thigh to insert via a rounded tendon into the adductor tubercle on the medial condyle of the distal head of the femur. The lateral or adductor part of the muscle inserts via an aponeurosis up onto the medial supracondylar line. A large circular gap inferiorly between the hamstring and adductor parts of the muscle is the adductor hiatus (Fig. 6.43), which allows the femoral artery and associated veins to pass between the adductor canal on the anteromedial aspect of the thigh and the popliteal fossa posterior to the knee. The adductor part of the muscle is innervated by the obturator nerve and the hamstring part is innervated by the tibial division of the sciatic nerve.
Fig. 6.43 Adductor magnus and obturator externus muscles. Anterior view.
Posterior compartment (Table 6.5, Fig. 6.44)
Table 6.5 Muscles of the posterior compartment of thigh (spinal segments in bold are the major segments innervating the muscle)
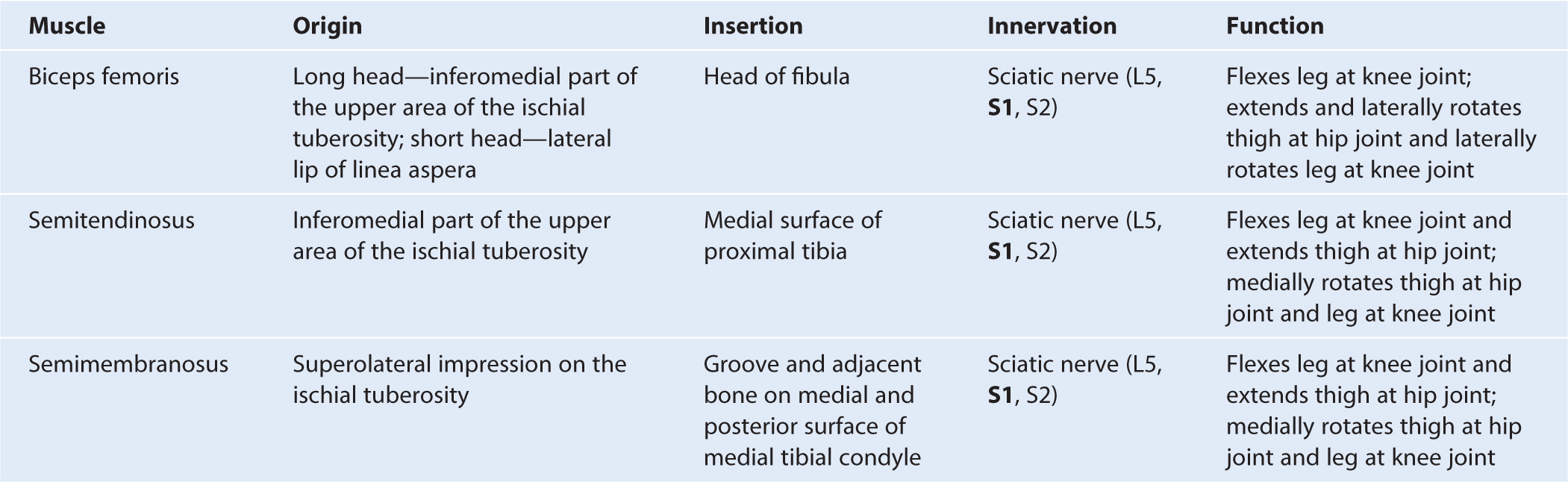
Fig. 6.44 Muscles of the posterior compartment of thigh. Posterior view.
There are three long muscles in the posterior compartment of thigh: biceps femoris, semitendinosus, and semimembranosus—and they are collectively known as the hamstrings. All except the short head of biceps femoris cross both the hip and knee joints. As a group, the hamstrings flex the leg at the knee joint and extend the thigh at the hip joint. They are also rotators at both joints. All are innervated by the sciatic nerve.
Clinical app
Hamstring injuries
Hamstring injuries include tendon avulsion at the ischial tuberosity, and intermuscular, musculotendinous, and myofascial disruptions within the muscle bellies. Among the common causes of these injuries are water skiing (hamstring tendon avulsion), track and field events, football and soccer injuries and rapid sprint injuries (muscle belly injuries). Occasionally, hamstring origin avulsions may require surgical reattachment.
Clinical app
Compartment syndrome
Compartment syndrome occurs when there is swelling within a fascial enclosed muscle compartment in the limbs. Typical causes may include limb trauma, intracompartment hemorrhage, and limb compression. As pressure within the compartment elevates, capillary blood flow and tissue perfusion is compromised, which can ultimately lead to neuromuscular damage if not treated.
Arteries
Three arteries enter the thigh: the femoral artery, the obturator artery, and the inferior gluteal artery. Of these, the femoral artery is the largest and supplies most of the lower limb. The three arteries contribute to an anastomotic network of vessels around the hip joint.
Femoral artery
The femoral artery (Fig. 6.45) is the continuation of the external iliac artery and begins as the external iliac artery passes under the inguinal ligament to enter the femoral triangle on the anterior aspect of the upper thigh (Fig. 6.45).
Fig. 6.45 Femoral artery.
The femoral artery passes vertically through the femoral triangle and then continues down the thigh in the adductor canal. It leaves the canal by passing through the adductor hiatus in the adductor magnus muscle and becomes the popliteal artery behind the knee (Fig. 6.45).
A cluster of four small branches—superficial epigastric artery, superficial circumflex iliac artery, superficial external pudendal artery, and deep external pudendal artery—originate from the femoral artery in the femoral triangle and supply cutaneous regions of the upper thigh, lower abdomen, and perineum (Fig. 6.45).
Deep artery of thigh
The largest branch of the femoral artery in the thigh is the deep artery of thigh (profunda femoris artery), which originates from the lateral side of the femoral artery in the femoral triangle and is the major source of blood supply to the thigh (Fig. 6.46). The deep artery of thigh immediately passes:
Fig. 6.46 Deep artery of thigh. A. Anterior view. B. Posterior view.
The deep artery of thigh has lateral and medial circumflex femoral branches and three perforating branches.
Lateral circumflex femoral artery
The lateral circumflex femoral artery normally originates proximally from the lateral side of the deep artery of thigh, but may arise directly from the femoral artery (Fig. 6.46). It passes deep to the sartorius and rectus femoris and divides into three terminal branches:
 One vessel (transverse branch) passes laterally to pierce the vastus lateralis and then circles around the proximal shaft of femur to anastomose with branches from the medial femoral circumflex artery, the inferior gluteal artery, and the first perforating artery to form the cruciate anastomosis around the hip (Fig. 6.46).
One vessel (transverse branch) passes laterally to pierce the vastus lateralis and then circles around the proximal shaft of femur to anastomose with branches from the medial femoral circumflex artery, the inferior gluteal artery, and the first perforating artery to form the cruciate anastomosis around the hip (Fig. 6.46).
Medial circumflex femoral artery
The medial circumflex femoral artery normally originates proximally from the posteromedial aspect of the deep artery of thigh, but may originate from the femoral artery (Fig. 6.46). It passes medially around the shaft of femur, first between the pectineus and iliopsoas and then between the obturator externus and adductor brevis muscles. Near the margin of the adductor brevis, the vessel gives off a small branch, which enters the hip joint through the acetabular notch and anastomoses with the acetabular branch of the obturator artery.
The main trunk of the medial circumflex femoral artery passes over the superior margin of the adductor magnus and divides into two major branches deep to the quadratus femoris muscle:
The three perforating arteries branch from the deep artery of thigh (Fig. 6.46) as it descends anterior to the adductor brevis muscle—the first originates above the muscle, the second originates anterior to the muscle, and the third originates below the muscle. All three penetrate through the adductor magnus near its attachment to the linea aspera to enter and supply the posterior compartment of thigh. Here, the vessels have ascending and descending branches, which interconnect to form a longitudinal channel, which participates above in forming an anastomotic network of vessels around the hip and inferiorly anastomoses with branches of the popliteal artery behind the knee.
Obturator artery
The obturator artery originates as a branch of the internal iliac artery in the pelvic cavity and enters the medial compartment of thigh through the obturator canal (Fig. 6.47). As it passes through the canal, it bifurcates into an anterior branch and a posterior branch, which together form a channel that circles the margin of the obturator membrane and lies within the attachment of the obturator externus muscle.
Fig. 6.47 Obturator artery.
Vessels arising from the anterior and posterior branches supply adjacent muscles and anastomose with the inferior gluteal and medial circumflex femoral arteries. In addition, an acetabular vessel originates from the posterior branch, enters the hip joint through the acetabular notch, and contributes to the supply of the head of the femur.
Clinical app
Peripheral vascular disease
Peripheral vascular disease is often characterized by reduced blood flow to the legs. This disorder may be due to stenoses (narrowing) and/or occlusions (blockages) in the lower aorta, iliac, femoral, tibial, and fibular vessels. Patients typically have chronic leg ischemia and “acute on chronic” leg ischemia.
Chronic leg ischemia is a disorder in which vessels have undergone atheromatous change and often there is significant luminal narrowing (usually over 50%). Most patients with peripheral arterial disease have widespread arterial disease (including cardiovascular and cerebrovascular disease), which may be clinically asymptomatic. Some of these patients develop such severe ischemia that the viability of the limb is threatened (critical limb ischemia).
The commonest symptom of chronic leg ischemia is intermittent claudication. Patients typically have a history of pain that develops in the calf muscles (usually associated with occlusions or narrowing in the femoral artery) or the buttocks (usually associated with occlusion or narrowing in the aorto-iliac segments). The pain experienced in these muscles is often cramplike and occurs with walking. The patient rests and is able to continue walking up to the same distance until the pain recurs and stops walking as before.
In some patients with chronic limb ischemia, an acute event blocks the vessels or reduces the blood supply to such a degree that the viability of the limb is threatened.
Occasionally a leg may become acutely ischemic with no evidence of underlying atheromatous disease. In these instances a blood clot is likely to have embolized from the heart. Patients with mitral valve disease and atrial fibrillation are prone to embolic disease.
Critical limb ischemia occurs when the blood supply to the limb is so poor that the viability of the limb is severely threatened, and in this case many patients develop gangrene, ulceration, and severe rest pain in the foot. These patients require urgent treatment, which may be in the form of surgical reconstruction, radiological angioplasty, or even amputation.
Veins
Veins in the thigh consist of superficial and deep veins. Deep veins generally follow the arteries and have similar names. Superficial veins are in the superficial fascia, interconnect with deep veins, and do not generally accompany arteries. The largest of the superficial veins in the thigh is the great saphenous vein.
Great saphenous vein
The great saphenous vein originates from a venous arch on the dorsal aspect of the foot and ascends along the medial side of the lower limb to the proximal thigh (see Fig. 6.20). Here it passes through the saphenous opening in the deep fascia covering the anterior thigh to connect with the femoral vein in the femoral triangle (see Fig. 6.23).
Nerves
There are three major nerves in the thigh, each associated with one of the three compartments. The femoral nerve is associated with the anterior compartment of thigh, the obturator nerve is associated with the medial compartment of thigh, and the sciatic nerve is associated with the posterior compartment of thigh.
Femoral nerve
The femoral nerve originates from the lumbar plexus (spinal cord segments L2-L4) on the posterior abdominal wall and enters the femoral triangle of the thigh by passing under the inguinal ligament (Fig. 6.48). In the femoral triangle, the femoral nerve lies on the lateral side of the femoral artery and is outside the femoral sheath, which surrounds the vessels.
Fig. 6.48 Femoral nerve.
Before entering the thigh, the femoral nerve supplies branches to the iliacus and pectineus muscles.
Immediately after passing under the inguinal ligament, the femoral nerve divides into anterior and posterior branches, which supply muscles of the anterior compartment of thigh and skin on the anterior and medial aspects of the thigh and on the medial sides of the leg and foot.
Branches of the femoral nerve (Fig. 6.48) include:
The saphenous nerve accompanies the femoral artery through the adductor canal, but does not pass through the adductor hiatus with the femoral artery (Fig. 6.48). Rather, the saphenous nerve penetrates directly through connective tissues near the end of the canal to appear between the sartorius and gracilis muscles on the medial side of the knee. Here the saphenous nerve penetrates deep fascia and continues down the medial side of the leg to the foot, and supplies skin on the medial side of the knee, leg, and foot.
Obturator nerve
The obturator nerve is a branch of the lumbar plexus (spinal cord segments L2-L4) on the posterior abdominal wall. It descends in the psoas muscle, and then passes out of the medial margin of the psoas muscle to enter the pelvis (Fig. 6.49). The obturator nerve continues along the lateral pelvic wall and then enters the medial compartment of thigh by passing through the obturator canal. It supplies most of the adductor muscles and skin on the medial aspect of the thigh. As the obturator nerve enters the thigh, it divides into two branches, an anterior branch and a posterior branch, which are separated by the adductor brevis muscle:
Fig. 6.49 Obturator nerve.
Sciatic nerve
The sciatic nerve is a branch of the lumbosacral plexus (spinal cord segments L4-S3) and descends into the posterior compartment of thigh from the gluteal region (Fig. 6.50). It innervates all muscles in the posterior compartment of thigh and then its branches continue into the leg and foot.
Fig. 6.50 Sciatic nerve.
In the posterior compartment of thigh, the sciatic nerve lies on the adductor magnus muscle and is crossed by the long head of biceps femoris muscle.
Proximal to the knee, and sometimes within the pelvis, the sciatic nerve divides into its two terminal branches: the tibial nerve and the common fibular nerve (Fig. 6.50). These nerves travel vertically down the thigh and enter the popliteal fossa posterior to the knee. Here, they meet the popliteal artery and vein.
The tibial nerve supplies branches to all muscles in the posterior compartment of thigh (long head of biceps femoris, semimembranosus, semitendinosus) except the short head of biceps femoris, which is innervated by the common fibular part (Fig. 6.50).
The tibial nerve descends through the popliteal fossa, enters the posterior compartment of leg, and continues into the sole of the foot.
The tibial nerve innervates:
 all muscles in the posterior compartment of leg,
all muscles in the posterior compartment of leg,
The common fibular nerve supplies the short head of biceps femoris in the posterior compartment of thigh and then continues into the lateral and anterior compartments of leg and onto the foot (Fig. 6.50).
The common fibular nerve innervates:
 all muscles in the anterior and lateral compartments of leg,
all muscles in the anterior and lateral compartments of leg,
 one muscle (extensor digitorum brevis) on the dorsal aspect of the foot,
one muscle (extensor digitorum brevis) on the dorsal aspect of the foot,
 the first two dorsal interossei muscles in the sole of the foot, and
the first two dorsal interossei muscles in the sole of the foot, and
 skin over the lateral aspect of the leg, and ankle, and over the dorsal aspect of the foot and toes.
skin over the lateral aspect of the leg, and ankle, and over the dorsal aspect of the foot and toes.
Knee joint
The knee joint is the largest synovial joint in the body (Fig. 6.51; also see Fig. 6.59). The detailed movements of the knee joint are complex, but basically the joint is a hinge joint that allows mainly flexion and extension. The joint consists of:
 the articulation between the femur and tibia, which is weight bearing, and
the articulation between the femur and tibia, which is weight bearing, and
Fig. 6.51 Knee joint. Joint capsule is not shown.
Articular surfaces
The articular surfaces of the bones that contribute to the knee joint are covered by hyaline cartilage. The major surfaces involved include:
 the adjacent surfaces of the superior aspect of the tibial condyles.
the adjacent surfaces of the superior aspect of the tibial condyles.
The surfaces of the femoral condyles that articulate with the tibia in flexion of the knee are curved or round, whereas the surfaces that articulate in full extension are flat (Fig. 6.52A,B).
Fig. 6.52 Articular surfaces of the knee joint. A. Extended. B. Flexed. C. Anterior view (flexed).
The articular surfaces between the femur and patella are the V-shaped trench on the anterior surface of the distal end of the femur where the two condyles join and the adjacent surfaces on the posterior aspect of the patella. The joint surfaces are all enclosed within a single articular cavity, as are the intra-articular menisci between the femoral and tibial condyles (Fig. 6.52C).
Menisci
There are two menisci, which are fibrocartilaginous C-shaped cartilages, in the knee joint, one medial (medial meniscus) and the other lateral (lateral meniscus) (Fig. 6.53). Both are attached at each end to facets in the intercondylar region of the tibial plateau.
Fig. 6.53 Menisci of the knee joint. Superior view.
The medial meniscus is attached around its margin to the capsule of the joint and to the tibial collateral ligament, whereas the lateral meniscus is unattached to the capsule. Therefore, the lateral meniscus is more mobile than the medial meniscus.
The menisci are interconnected anteriorly by a transverse ligament of the knee (Fig. 6.53). The lateral meniscus is also connected to the tendon of the popliteus muscle, which passes superolaterally between this meniscus and the capsule to insert on the femur (Fig. 6.53).
The menisci improve congruency between the femoral and tibial condyles during joint movements where the surfaces of the femoral condyles articulating with the tibial plateau change from small curved surfaces in flexion to large flat surfaces in extension (Fig. 6.52).
Synovial membrane
The synovial membrane of the knee joint attaches to the margins of the articular surfaces and to the superior and inferior outer margins of the menisci (Fig. 6.54A). The two cruciate ligaments, which attach in the intercondylar region of the tibia below and the intercondylar fossa of the femur above, are outside the articular cavity, but enclosed within the fibrous membrane of the knee joint.
Anteriorly, the synovial membrane is separated from the patellar ligament by an infrapatellar fat pad (Fig. 6.54). On each side of the pad, the synovial membrane forms a fringed margin (an alar fold), which projects into the articular cavity. In addition, the synovial membrane covering the lower part of the infrapatellar fat pad is raised into a sharp midline fold directed posteriorly (the infrapatellar synovial fold), which attaches to the margin of the intercondylar fossa of the femur.
The synovial membrane of the knee joint forms pouches in two locations to provide low friction surfaces for the movement of tendons associated with the joint:
 the small subpopliteal recess (Fig. 6.54A), which extends between the lateral meniscus and the tendon of the popliteus muscle, and
the small subpopliteal recess (Fig. 6.54A), which extends between the lateral meniscus and the tendon of the popliteus muscle, and
 the large suprapatellar bursa (Fig. 6.54B) is a continuation of the articular cavity superiorly between the distal end of the shaft of femur and the quadriceps femoris muscle and tendon. The apex of this bursa is attached to the small articularis genus muscle, which pulls the bursa away from the joint during extension of the knee.
the large suprapatellar bursa (Fig. 6.54B) is a continuation of the articular cavity superiorly between the distal end of the shaft of femur and the quadriceps femoris muscle and tendon. The apex of this bursa is attached to the small articularis genus muscle, which pulls the bursa away from the joint during extension of the knee.
Other bursae associated with the knee, but not normally communicating with the articular cavity include the subcutaneous prepatellar bursa, deep and subcutaneous infrapatellar bursae, and numerous other bursae associated with tendons and ligaments around the joint (Fig. 6.54B).
The prepatellar bursa is subcutaneous and anterior to the patella. The deep and subcutaneous infrapatellar bursae are on the deep and subcutaneous sides of the patellar ligament, respectively.
Fibrous membrane
The fibrous membrane of the knee joint is extensive and is partly formed and reinforced by extensions from tendons of the surrounding muscles (Fig. 6.55). In general, the fibrous membrane encloses the articular cavity and the intercondylar region (Fig. 6.55):
Fig. 6.55 Fibrous membrane of the knee joint capsule. A. Anterior view. B. Posterior view.
The fibrous membrane is reinforced anterolaterally by a fibrous extension from the iliotibial tract and posteromedially by an extension from the tendon of semimembranosus (the oblique popliteal ligament), which reflects superiorly across the back of the fibrous membrane from medial to lateral (Fig. 6.55B).
The upper end of the popliteus muscle passes through an aperture in the posterolateral aspect of the fibrous membrane of the knee and is enclosed by the fibrous membrane as its tendon travels around the joint to insert into the lateral aspect of the lateral femoral condyle (Fig. 6.55B).
Ligaments
The major ligaments associated with the knee joint are the patellar ligament, the tibial (medial) and fibular (lateral) collateral ligaments, and the anterior and posterior cruciate ligaments.
Patellar ligament
The patellar ligament is basically the continuation of the quadriceps femoris tendon inferior to the patella (Fig. 6.55A). It is attached above to the margins and apex of the patella and below to the tibial tuberosity.
Collateral ligaments
The collateral ligaments, one on each side of the joint, stabilize the hingelike motion of the knee (Fig. 6.56).
Fig. 6.56 Collateral ligaments of the knee joint. A. Lateral view. B. Medial view.
The cordlike fibular collateral ligament is attached superiorly to the lateral femoral epicondyle just above the groove for the popliteus tendon (Fig. 6.56A). Inferiorly, it is attached to a depression on the lateral surface of the fibular head. It is separated from the fibrous membrane by a bursa.
The broad and flat tibial collateral ligament (Fig. 6.56B), is attached by much of its deep surface to the underlying fibrous membrane. It is anchored superiorly to the medial femoral epicondyle just inferior to the adductor tubercle and descends anteriorly to attach to the medial margin and medial surface of the tibia above and behind the attachment of sartorius, gracilis, and semitendinosus tendons (Fig. 6.56B).
Cruciate ligaments
The two cruciate ligaments are in the intercondylar region of the knee and interconnect the femur and tibia (Fig. 6.57). They are termed “cruciate” (Latin for “shaped like a cross”) because they cross each other in the sagittal plane between their femoral and tibial attachments:
 The anterior cruciate ligament attaches to a facet on the anterior part of the intercondylar area of the tibia and ascends posteriorly to attach to a facet at the back of the lateral wall of the intercondylar fossa of the femur (Fig. 6.57).
The anterior cruciate ligament attaches to a facet on the anterior part of the intercondylar area of the tibia and ascends posteriorly to attach to a facet at the back of the lateral wall of the intercondylar fossa of the femur (Fig. 6.57).
 The posterior cruciate ligament attaches to the posterior aspect of the intercondylar area of the tibia and ascends anteriorly to attach to the medial wall of the intercondylar fossa of the femur (Fig. 6.57).
The posterior cruciate ligament attaches to the posterior aspect of the intercondylar area of the tibia and ascends anteriorly to attach to the medial wall of the intercondylar fossa of the femur (Fig. 6.57).
Fig. 6.57 Cruciate ligaments of the knee joint. Superolateral view.
The anterior cruciate ligament crosses lateral to the posterior cruciate ligament as they pass through the intercondylar region.
The anterior cruciate ligament prevents anterior displacement of the tibia relative to the femur and the posterior cruciate ligament restricts posterior displacement (Fig. 6.57).
Locking mechanism
When standing, the knee joint is locked into position, thereby reducing the amount of muscle work needed to maintain the standing position (Fig. 6.58).
Fig. 6.58 Knee “locking” mechanism.
One component of the locking mechanism is a change in the shape and size of the femoral surfaces that articulate with the tibia (see Fig. 6.52A,B):
Consequently the joint surfaces become larger and more stable in extension.
Another component of the locking mechanism is medial rotation of the femur on the tibia during extension. Medial rotation and full extension tightens all the associated ligaments.
Another feature that keeps the knee extended when standing is that the body’s center of gravity is positioned along a vertical line that passes anterior to the knee joint.
The popliteus muscle unlocks the knee by initiating lateral rotation of the femur on the tibia.
Imaging app
Visualizing the knee joint
Fig. 6.59 Normal knee joint. A. Normal knee joint showing the tibial collateral ligament, the medial and lateral menisci, and the anterior and posterior cruciate ligaments. T1-weighted magnetic resonance image in the coronal plane. B. Radiograph, AP view. C. Radiograph, lateral view.
Vascular supply and innervation
Vascular supply to the knee joint is predominantly through descending and genicular branches from the femoral, popliteal, and lateral circumflex femoral arteries in the thigh and the circumflex fibular artery and recurrent branches from the anterior tibial artery in the leg. These vessels form an anastomotic network around the joint (Fig. 6.60).
Fig. 6.60 Anastomoses of arteries around the knee. Anterior view.
The knee joint is innervated by branches from the obturator, femoral, tibial, and common fibular nerves.
Clinical app
Soft tissue injuries to the knee
Soft tissue injuries are common at and around the knee joint.
The typical injuries include tears of the anterior and posterior cruciate ligaments, meniscal tears, and trauma to the collateral ligaments. Isolated soft tissue injuries may occur, but it is not uncommon for certain types of injuries to occur together, for example, anterior cruciate ligament disruption, tibial collateral ligament disruption, and tears of the medial or lateral menisci.
Clinical app
Clinical tests for tears in the cruciate ligaments:
 Anterior drawer test—a positive anterior drawer test is when the proximal head of a supine patient’s tibia can be pulled anteriorly on the femur. The knee is flexed to 90° and the heel and sole of the foot are placed on the couch. If the tibia moves forward, the anterior cruciate ligament is torn.
Anterior drawer test—a positive anterior drawer test is when the proximal head of a supine patient’s tibia can be pulled anteriorly on the femur. The knee is flexed to 90° and the heel and sole of the foot are placed on the couch. If the tibia moves forward, the anterior cruciate ligament is torn.
Clinical app
Arthroscopy
An arthroscope is a small camera that is placed into the knee joint through the anterolateral or anteromedial aspect of the knee joint. The joint is filled with a saline solution and the camera is manipulated around the knee joint to assess the cruciate ligaments, menisci, and cartilaginous surfaces. Any damage observed can be repaired or trimmed.
Tibiofibular joint
The small proximal tibiofibular joint is synovial in type and allows very little movement (Fig. 6.61). The opposing joint surfaces, on the undersurface of the lateral condyle of the tibia and on the superomedial surface of the head of the fibula, are flat and circular. The capsule is reinforced by anterior and posterior ligaments.
Fig. 6.61 Tibiofibular joint.
Popliteal fossa
The popliteal fossa is an important area of transition between the thigh and leg and is the major route by which structures pass from one region to the other.
The popliteal fossa is a diamond-shaped space behind the knee joint formed between muscles in the posterior compartments of thigh and leg (Fig. 6.62A):
Fig. 6.62 Popliteal fossa. A. Boundaries. B. Nerves and vessels. C. Superficial structures.
Contents
The major contents of the popliteal fossa are the popliteal artery, the popliteal vein, and the tibial and common fibular nerves (Fig. 6.62B).
The tibial and common fibular nerves originate proximal to the popliteal fossa as the two major branches of the sciatic nerve (Fig. 6.62B). They are the most superficial of the neurovascular structures in the popliteal fossa and enter the region directly from above under the margin of the biceps femoris muscle (Fig. 6.62B):
The popliteal artery is the continuation of the femoral artery in the anterior compartment of thigh, and begins as the femoral artery passes posteriorly through the adductor hiatus in the adductor magnus muscle (Fig. 6.62B).
The popliteal artery appears deep in the popliteal fossa on the upper medial side under the margin of the semimembranosus muscle. It descends obliquely through the fossa with the tibial nerve and enters the posterior compartment of leg where it ends just lateral to the midline of the leg by dividing into the anterior and posterior tibial arteries.
In the popliteal fossa, the popliteal artery gives rise to branches, which supply adjacent muscles, and to a series of geniculate arteries, which contribute to vascular anastomoses around the knee.
The popliteal vein is superficial to and travels with the popliteal artery (Fig. 6.62B). It exits the popliteal fossa superiorly to become the femoral vein by passing through the adductor hiatus.
Roof of popliteal fossa
The roof of the popliteal fossa is covered by superficial fascia and skin (Fig. 6.62C). The most important structure in the superficial fascia is the small saphenous vein. This vessel ascends vertically in the superficial fascia on the back of the leg from the lateral side of the dorsal venous arch in the foot. It ascends to the back of the knee where it penetrates deep fascia, which forms the roof of the popliteal fossa and joins with the popliteal vein.
One other structure that passes through the roof of the fossa is the posterior cutaneous nerve of thigh, which descends through the thigh superficial to the hamstring muscles, passes through the roof of the popliteal fossa, and then continues inferiorly with the small saphenous vein to innervate skin on the upper half of the back of the leg.
Surface anatomy
Visualizing the contents of the popliteal fossa
The popliteal fossa is a diamond-shaped depression formed between the hamstrings and gastrocnemius muscle posterior to the knee. The tendons of the biceps femoris muscle and the semitendinosus muscle are palpable and often visible.
The head of the fibula is palpable on the lateral side of the knee and can be used as a landmark for identifying the biceps femoris tendon and the common fibular nerve, which curves laterally out of the popliteal fossa and crosses the neck of the fibula just inferior to the head.
The popliteal fossa contains the popliteal artery, the popliteal vein, the tibial nerve, and the common fibular nerve (Fig. 6.63). The popliteal artery is the deepest of the structures in the fossa and descends through the region from the upper medial side. As a consequence of its position, the popliteal artery pulse is difficult to find, but usually can be detected on deep palpation just medial to the midline of the fossa.
Fig. 6.63 Visualizing the contents of the popliteal fossa. Posterior view of the left knee.
The small saphenous vein penetrates deep fascia in the upper part of the posterior leg and joins the popliteal vein.
LEG
The leg is that part of the lower limb between the knee joint and ankle joint (Fig. 6.64).
Fig. 6.64 Posterior view of leg; cross-section through the left leg (inset).
The bones of the leg are the lateral fibula and the medial tibia. The tibia is the weight-bearing bone of the leg and is therefore much larger than the fibula.
The leg is divided into anterior (extensor), posterior (flexor), and lateral (fibular) compartments (Fig. 6.64) by:
 two intermuscular septa, which pass between the fibula and deep fascia surrounding the limb.
two intermuscular septa, which pass between the fibula and deep fascia surrounding the limb.
Bones
Shaft and distal end of tibia
The shaft of tibia (Fig. 6.65A,B) is triangular in cross-section and has anterior, interosseous, and medial borders and medial, lateral, and posterior surfaces (Fig. 6.65C):
 The anterior and medial borders, and the entire medial surface are subcutaneous and easily palpable.
The anterior and medial borders, and the entire medial surface are subcutaneous and easily palpable.
 The posterior surface is marked by an oblique line (the soleal line).
The posterior surface is marked by an oblique line (the soleal line).
The soleal line descends across the bone from the lateral side to the medial side where it merges with the medial border. In addition, a vertical line descends down the upper part of the posterior surface from the midpoint of the soleal line. It disappears in the lower one third of the tibia.
The shaft of the tibia expands at both the upper and lower ends to support the body’s weight at the knee and ankle joints.
The distal end of the tibia is shaped like a rectangular box with a bony protuberance on the medial side (the medial malleolus; Fig. 6.65). The upper part of the box is continuous with the shaft of the tibia, whereas the lower surface and the medial malleolus articulate with one of the tarsal bones (talus) to form a large part of the ankle joint.
The posterior surface of the boxlike distal end of the tibia is marked by a vertical groove, which continues inferiorly and medially onto the posterior surface of the medial malleolus. The groove is for the tendon of the tibialis posterior muscle.
The lateral surface of the distal end of the tibia is occupied by a deep triangular notch (the fibular notch) (Fig. 6.65D), to which the distal head of the fibula is anchored by a thickened part of the interosseous membrane.
Shaft and distal end of fibula
The fibula is not involved in weight bearing. The fibular shaft is therefore much narrower than the shaft of the tibia (Fig. 6.65A,B). Also, and except for the ends, the fibula is enclosed by muscles.
Like the tibia, the shaft of the fibula is triangular in cross-section and has three borders and three surfaces for the attachment of muscles, intermuscular septa, and ligaments (Fig. 6.65C). The interosseous border of the fibula faces and is attached to the interosseous border of the tibia by the interosseous membrane. Intermuscular septa attach to the anterior and posterior borders. Muscles attach to the three surfaces.
The narrow medial surface faces the anterior compartment of leg, the lateral surface faces the lateral compartment of leg, and the posterior surface faces the posterior compartment of leg.
The posterior surface is marked by a vertical crest (medial crest), which divides the posterior surface into two parts each attached to a different deep flexor muscle.
The distal end of the fibula expands to form the spade-shaped lateral malleolus (Fig. 6.65).
The medial surface of the lateral malleolus bears a facet for articulation with the lateral surface of talus, thereby forming the lateral part of the ankle joint. Just superior to this articular facet is a triangular area, which fits into the fibular notch on the distal end of the tibia (Fig. 6.65D). Here the tibia and fibula are joined together by the distal end of the interosseous membrane. Posteroinferior to the facet for articulation with the talus is a pit or fossa (the malleolar fossa) for the attachment of the posterior talofibular ligament associated with the ankle joint.
The posterior surface of the lateral malleolus is marked by a shallow groove for the tendons of the fibularis longus and fibularis brevis muscles.
Joints
Interosseous membrane of leg
The interosseous membrane of leg is a tough fibrous sheet of connective tissue that spans the distance between facing interosseous borders of the tibial and fibular shafts (Fig. 6.66A).
Fig. 6.66 Interosseous membrane. A. Anterior view. B. Posteromedial view.
There are two apertures in the interosseous membrane, one at the top and the other at the bottom, for vessels to pass between the anterior and posterior compartments of leg (Fig. 6.66A).
The interosseous membrane not only links the tibia and fibula together, but also provides an increased surface area for muscle attachment.
The distal ends of the fibula and tibia are held together by the inferior aspect of the interosseous membrane, which spans the narrow space between the fibular notch on the lateral surface of the distal end of the tibia and the corresponding surface on the distal end of the fibula (Fig. 6.66A,B). This expanded end of the interosseous membrane is reinforced by anterior and posterior tibiofibular ligaments. This firm linking together of the distal ends of the tibia and fibula is essential to produce the skeletal framework for articulation with the foot at the ankle joint.
Posterior compartment of leg
Muscles
Muscles in the posterior (flexor) compartment of leg are organized into two groups, superficial and deep, separated by a layer of deep fascia. Generally, the muscles mainly plantarflex and invert the foot and flex the toes. All are innervated by the tibial nerve.
Superficial group
The superficial group of muscles in the posterior compartment of leg comprises three muscles—the gastrocnemius, plantaris, and soleus (Table 6.6, Fig. 6.67)—all of which insert onto the heel (calcaneus) of the foot and plantarflex the foot at the ankle joint (Fig. 6.67). As a unit, these muscles are large and powerful because they propel the body forward off the planted foot during walking and can elevate the body upward onto the toes when standing. Two of the muscles (gastrocnemius and plantaris) originate on the distal end of the femur and can also flex the knee.
Table 6.6 Superficial group of muscles in the posterior compartment of leg (spinal segments in bold are the major segments innervating the muscle)
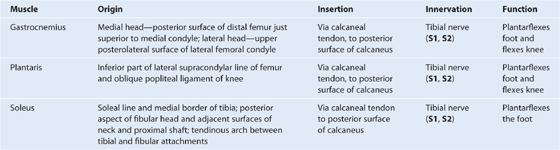
Deep group
There are four muscles in the deep posterior compartment of leg (Table 6.7, Fig. 6.68)—the popliteus, flexor hallucis longus, flexor digitorum longus, and tibialis posterior. The popliteus muscle acts on the knee, whereas the other three muscles act mainly on the foot.
Table 6.7 Deep group of muscles in the posterior compartment of the leg (spinal segments in bold are the major segments innervating the muscle)
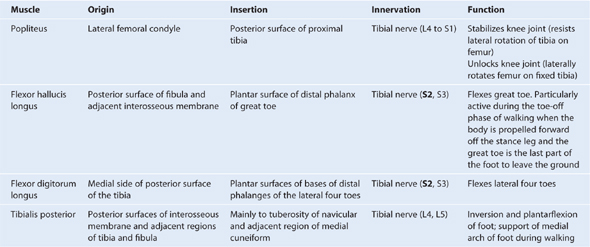
Fig. 6.68 Deep group of muscles in the posterior compartment of leg.
Arteries
Popliteal artery
The popliteal artery is the major blood supply to the leg and foot and enters the posterior compartment of leg from the popliteal fossa behind the knee (Fig. 6.69).
Fig. 6.69 Arteries in the posterior compartment of leg.
The popliteal artery passes into the posterior compartment of leg between the gastrocnemius and popliteus muscles. As it continues inferiorly it passes under the tendinous arch formed between the fibular and tibial heads of the soleus muscle and enters the deep region of the posterior compartment of leg where it immediately divides into an anterior tibial artery and a posterior tibial artery.
There are two large sural arteries, one on each side, that branch from the popliteal artery to supply the gastrocnemius, soleus, and plantaris muscles (Fig. 6.69). In addition, the popliteal artery gives rise to branches that contribute to a collateral network of vessels around the knee joint (see Fig. 6.60).
The anterior tibial artery passes forward through the aperture in the upper part of the interosseous membrane and enters and supplies the anterior compartment of the leg (Fig. 6.69). It continues inferiorly onto the dorsal aspect of the foot.
The posterior tibial artery supplies the posterior and lateral compartments of the leg and continues into the sole of the foot (Fig. 6.69).
The posterior tibial artery descends through the deep region of the posterior compartment of the leg on the superficial surfaces of the tibialis posterior and flexor digitorum longus muscles. It passes through the tarsal tunnel behind the medial malleolus and into the sole of the foot.
In the leg, the posterior tibial artery supplies adjacent muscles and bone and has two major branches, the circumflex fibular artery and the fibular artery:
 The circumflex fibular artery passes laterally through the soleus muscle and around the neck of the fibula to connect with the anastomotic network of vessels surrounding the knee (Fig. 6.69; see also Fig. 6.60).
The circumflex fibular artery passes laterally through the soleus muscle and around the neck of the fibula to connect with the anastomotic network of vessels surrounding the knee (Fig. 6.69; see also Fig. 6.60).
 The fibular artery parallels the course of the tibial artery, but descends along the lateral side of the posterior compartment adjacent to the medial crest on the posterior surface of the fibula, which separates the attachments of the tibialis posterior and flexor hallucis longus muscles (Fig. 6.69).
The fibular artery parallels the course of the tibial artery, but descends along the lateral side of the posterior compartment adjacent to the medial crest on the posterior surface of the fibula, which separates the attachments of the tibialis posterior and flexor hallucis longus muscles (Fig. 6.69).
The fibular artery supplies adjacent muscles and bone in the posterior compartment of the leg and also has branches that pass laterally through the intermuscular septum to supply the fibularis muscles in the lateral compartment of the leg.
A perforating branch that originates from the fibular artery distally in the leg passes anteriorly through the inferior aperture in the interosseous membrane to anastomose with a branch of the anterior tibial artery.
The fibular artery passes behind the attachment between the distal ends of the tibia and fibula and terminates in a network of vessels over the lateral surface of the calcaneus.
Veins
Deep veins in the posterior compartment generally follow the arteries.
Nerves
Tibial nerve
The nerve associated with the posterior compartment of leg is the tibial nerve (Fig. 6.70A), a major branch of the sciatic nerve that descends into the posterior compartment from the popliteal fossa.
Fig. 6.70 Tibial nerve. A. Posterior view. B. Sural nerve.
The tibial nerve passes under the tendinous arch formed between the fibular and tibial heads of the soleus muscle and passes vertically through the deep region of the posterior compartment of leg on the surface of the tibialis posterior muscle with the posterior tibial vessels.
The tibial nerve leaves the posterior compartment of the leg at the ankle by passing through the tarsal tunnel behind the medial malleolus. It enters the foot to supply most intrinsic muscles and skin.
In the leg, the tibial nerve gives rise to:
 branches that supply all the muscles in the posterior compartment of the leg, and
branches that supply all the muscles in the posterior compartment of the leg, and
 two cutaneous branches, the sural nerve and medial calcaneal nerve (Fig. 6.70A,B).
two cutaneous branches, the sural nerve and medial calcaneal nerve (Fig. 6.70A,B).
Branches of the tibial nerve that innervate the superficial group of muscles of the posterior compartment and popliteus muscle of the deep group originate high in the leg between the two heads of the gastrocnemius muscle in the distal region of the popliteal fossa. Branches innervate the gastrocnemius, plantaris, and soleus muscles, and pass more deeply into the popliteus muscle.
Branches to the deep muscles of the posterior compartment originate from the tibial nerve deep to the soleus muscle in the upper half of the leg and innervate the tibialis posterior, flexor hallucis longus, and flexor digitorum longus muscles.
The sural nerve originates high in the leg between the two heads of the gastrocnemius muscle (Fig. 6.70B). It descends superficial to the belly of the gastrocnemius muscle and penetrates through the deep fascia approximately in the middle of the leg where it is joined by a sural communicating branch from the common fibular nerve. It passes down the leg, around the lateral malleolus, and into the foot.
The sural nerve supplies skin on the lower posterolateral surface of the leg and the lateral side of the foot and little toe.
The medial calcaneal nerve is often multiple and originates from the tibial nerve low in the leg near the ankle and descends onto the medial side of the heel.
The medial calcaneal nerve innervates skin on the medial surface and sole of the heel (Fig. 6.70A).
Lateral compartment of leg
Muscles
There are two muscles in the lateral compartment of leg—the fibularis longus and fibularis brevis (Table 6.8, Fig. 6.71). Both evert the foot (turn the sole outward) and are innervated by the superficial fibular nerve, which is a branch of the common fibular nerve.
Table 6.8 Muscles of the lateral compartment of leg (spinal segments in bold are the major segments innervating the muscle)
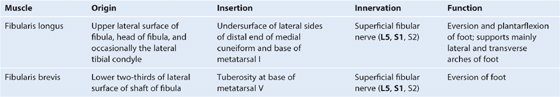
Arteries
No major artery passes vertically through the lateral compartment of leg. It is supplied by branches (mainly from the fibular artery in the posterior compartment of leg) that penetrate into the lateral compartment (Fig. 6.72).
Veins
Deep veins generally follow the arteries.
Nerves
Superficial fibular nerve
The nerve associated with the lateral compartment of the leg is the superficial fibular nerve. This nerve originates as one of the two major branches of the common fibular nerve, which enters the lateral compartment of the leg from the popliteal fossa (Fig. 6.72B).
The common fibular nerve courses around the neck of the fibula (Fig. 6.72A) and enters the lateral compartment by passing between the attachments of the fibularis longus muscle to the head and shaft of fibula. Here the common fibular nerve divides into its two terminal branches (Fig. 6.72B):
 the superficial fibular nerve, and
the superficial fibular nerve, and
The superficial fibular nerve descends in the lateral compartment deep to the fibularis longus and innervates the fibularis longus and fibularis brevis (Fig. 6.72B). It then penetrates deep fascia in the lower leg and enters the foot where it divides into medial and lateral branches, which supply dorsal areas of the foot and toes except for:
 the web space between the great and second toes, which is supplied by the deep fibular nerve, and
the web space between the great and second toes, which is supplied by the deep fibular nerve, and
 the lateral side of the little toe, which is supplied by the sural branch of the tibial nerve.
the lateral side of the little toe, which is supplied by the sural branch of the tibial nerve.
The deep fibular nerve passes anteromedially through the intermuscular septum into the anterior compartment of the leg, which it supplies.
Anterior compartment of the leg
Muscles
There are four muscles in the anterior compartment of the leg—the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius (Table 6.9, Fig. 6.73). Collectively they dorsiflex the foot at the ankle joint, extend the toes, and invert the foot. All are innervated by the deep fibular nerve, which is a branch of the common fibular nerve.
Table 6.9 Muscles of the anterior compartment of leg (spinal segments in bold are the major segments innervating the muscle)
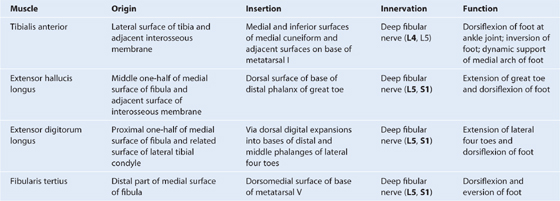
Fig. 6.73 Muscles of the anterior compartment of leg. A. Muscles. B. Proximal attachments.
Arteries
The artery associated with the anterior compartment of leg is the anterior tibial artery, which originates from the popliteal artery in the posterior compartment of the leg and passes forward into the anterior compartment of the leg through an aperture in the interosseous membrane.
The anterior tibial artery descends through the anterior compartment on the interosseous membrane (Fig. 6.74). In the distal leg, it lies between the tendons of the tibialis anterior and extensor hallucis longus muscles. It leaves the leg by passing anterior to the distal end of the tibia and ankle joint, and continues onto the dorsal aspect of the foot as the dorsalis pedis artery.
Fig. 6.74 Anterior tibial artery and deep fibular nerve.
In the proximal leg, the anterior tibial artery has a recurrent branch, which connects with the anastomotic network of vessels around the knee joint (see Fig. 6.60).
Along its course, the anterior tibial artery supplies numerous branches to adjacent muscles and is joined by the perforating branch of the fibular artery, which passes forward through the lower aspect of the interosseous membrane from the posterior compartment of the leg.
Distally, the anterior tibial artery gives rise to an anterior medial malleolar artery and an anterior lateral malleolar artery, which pass posteriorly around the distal ends of the tibia and fibula, respectively, and connect with vessels from the posterior tibial and fibular arteries to form an anastomotic network around the ankle.
Veins
Deep veins follow the arteries and have similar names.
Nerves
Deep fibular nerve
The nerve associated with the anterior compartment of the leg is the deep fibular nerve (Fig. 6.74). This nerve originates in the lateral compartment of the leg as one of the two divisions of the common fibular nerve.
The deep fibular nerve passes through the intermuscular septum that separates the lateral from the anterior compartments of the leg and then passes deep to the extensor digitorum longus. It reaches the anterior interosseous membrane where it meets and descends with the anterior tibial artery.
The deep fibular nerve:
 innervates all muscles in the anterior compartment;
innervates all muscles in the anterior compartment;
Clinical app
Foot drop
Foot drop is an inability to dorsiflex the foot. Patients with foot drop have a characteristic “steppage” gait. As the patient walks, the knee of the affected limb is elevated to an abnormal height during the swing phase to prevent the foot from dragging. At the end of the swing phase, the foot “slaps” the ground. Also, the unaffected limb often acquires a characteristic tiptoe pattern of gait during the stance phase. A typical cause of foot drop is damage to the common fibular nerve. Other causes include disc protrusion compressing the L5 nerve root, disorders of the sciatic nerve and the lumbosacral plexus, and pathologies of the spinal cord and brain.
FOOT
The foot is the region of the lower limb distal to the ankle joint. It is subdivided into the ankle, the metatarsus, and the digits.
There are five digits consisting of the medially positioned great toe (digit I) and four more laterally placed digits, ending laterally with the little toe (digit V) (Fig. 6.75).
The foot has a superior surface (dorsum of foot) and an inferior surface (sole; Fig. 6.75).
Abduction and adduction of the toes are defined with respect to the long axis of the second digit. Unlike in the hand where the thumb is oriented 90° to the other fingers, the great toe is oriented in the same position as the other toes. The foot is the body’s point of contact with the ground and provides a stable platform for upright stance. It also levers the body forward during walking.
Bones
There are three groups of bones in the foot (Fig. 6.76):
 the seven tarsal bones, which form the skeletal framework for the ankle,
the seven tarsal bones, which form the skeletal framework for the ankle,
 metatarsals (I to V), which are the bones of the metatarsus, and
metatarsals (I to V), which are the bones of the metatarsus, and
Fig. 6.76 Bones of the foot. A. Dorsal view, right foot. B. Lateral view, right foot.
Tarsal bones
The tarsal bones are arranged in a proximal group and a distal group with an intermediate bone between the two groups on the medial side of the foot (Fig. 6.76A).
Proximal group
The proximal group consists of two large bones, the talus (Latin for “ankle”) and the calcaneus (Latin for “heel”):
 The talus is the most superior bone of the foot and sits on top of and is supported by the calcaneus (Fig. 6.76B)—it articulates above with the tibia and fibula to form the ankle joint and also projects forward to articulate with the intermediate tarsal bone (navicular) on the medial side of the foot.
The talus is the most superior bone of the foot and sits on top of and is supported by the calcaneus (Fig. 6.76B)—it articulates above with the tibia and fibula to form the ankle joint and also projects forward to articulate with the intermediate tarsal bone (navicular) on the medial side of the foot.
 The calcaneus is the largest of the tarsal bones (Fig. 6.76A,B)—posteriorly it forms the bony framework of the heel and anteriorly projects forward to articulate with one of the distal group of tarsal bones (cuboid) on the lateral side of the foot.
The calcaneus is the largest of the tarsal bones (Fig. 6.76A,B)—posteriorly it forms the bony framework of the heel and anteriorly projects forward to articulate with one of the distal group of tarsal bones (cuboid) on the lateral side of the foot.
The talus, when viewed from the medial or lateral sides, is snail shaped (Fig. 6.77A). It has a rounded head, which is projected forward and medially at the end of a short broad neck, which is connected posteriorly to an expanded body.
Fig. 6.77 Talus. A. Medial view. B. Inferior view.
Anteriorly, the head of the talus is domed for articulation with a corresponding circular depression on the posterior surface of the navicular bone. Inferiorly, this domed articular surface is continuous with an additional three articular facets separated by smooth ridges (Fig. 6.76B):
 The anterior and middle facets articulate with adjacent surfaces on the calcaneus bone.
The anterior and middle facets articulate with adjacent surfaces on the calcaneus bone.
The neck of the talus is marked inferiorly by a deep groove (the sulcus tali), which passes obliquely forward across the inferior surface from medial to lateral, and expands dramatically on the lateral side. Posterior to the sulcus tali is a large facet (posterior calcaneal articular facet) for articulation with the calcaneus.
The superior aspect of the body of the talus is elevated to fit into the socket formed by the distal ends of the tibia and fibula to form the ankle joint:
 The medial surface articulates with the medial malleolus of the tibia.
The medial surface articulates with the medial malleolus of the tibia.
 The lateral surface articulates with the lateral malleolus of the fibula.
The lateral surface articulates with the lateral malleolus of the fibula.
Because the lateral malleolus is larger and projects more inferiorly than the medial malleolus at the ankle joint, the corresponding lateral articular surface on the talus is larger and projects more inferiorly than the medial surface.
The lower part of the lateral surface of the body of the talus, which supports the lower part of the facet for articulation with the fibula, forms a bony projection (the lateral process) (Fig. 6.76A).
The inferior surface of the body of the talus has a large oval concave facet (the posterior calcaneal articular facet) for articulation with the calcaneus (Fig. 6.77B).
The posterior aspect of the body of the talus consists of a backward and medially facing projection (the posterior process). The posterior process is marked on its surface by a lateral tubercle and a medial tubercle, which bracket between them the groove for tendon of the flexor hallucis longus as it passes from the leg into the foot.
The calcaneus sits under and supports the talus. It is an elongate, irregular, box-shaped bone with its long axis generally oriented along the midline of the foot, but deviating lateral to the midline anteriorly (Fig. 6.78).
Fig. 6.78 Calcaneus. A. Superior view. B. Inferior view. C. Lateral view.
The calcaneus projects behind the ankle joint to form the skeletal framework of the heel. The posterior surface of this heel region is circular and divided into upper, middle, and lower parts. The calcaneal tendon (Achilles tendon) attaches to the middle part:
 The upper part is separated from the calcaneal tendon by a bursa.
The upper part is separated from the calcaneal tendon by a bursa.
The calcaneal tuberosity projects forward on the plantar surface as a large medial process and a small lateral process separated from each other by a V-shaped notch (Fig. 6.78B). At the anterior end of the plantar surface is a tubercle (the calcaneal tubercle) for the posterior attachment of the short plantar ligament of the sole of the foot.
The lateral surface of the calcaneus has a smooth contour except for two slightly raised regions (Fig. 6.78C). One of these raised areas—the fibular trochlea (peroneal tubercle)—is anterior to the middle of the surface and often has two shallow grooves, which pass, one above the other, obliquely across its surface. The tendons of the fibularis brevis and longus muscles are bound to the trochlea as they pass over the lateral side of the calcaneus.
The medial surface of the calcaneus is concave and has one prominent feature associated with its upper margin (the sustentaculum tali; Fig. 6.78A), which is a shelf of bone projecting medially and supporting the more posterior part of the head of the talus.
The underside of the sustentaculum tali has a distinct groove running from posterior to anterior and along which the tendon of the flexor hallucis longus muscle travels into the sole of the foot (Fig. 6.78B).
The superior surface of the sustentaculum tali has a facet (middle talar articular surface) for articulation with the corresponding middle facet on the head of the talus (Fig. 6.78A,C).
Anterior and posterior talar articular surfaces are on the superior surface of the calcaneus itself (Fig. 6.78A):
Between the posterior talar articular surface, which articulates with the body of the talus and the other two articular surfaces, which articulate with the head of the talus, is a deep groove (the calcaneal sulcus; Fig. 6.78A,C).
The calcaneal sulcus on the superior surface of the calcaneus and the sulcus tali on the inferior surface of the talus together form the tarsal sinus, which is a large gap between the anterior ends of the calcaneus and talus that is visible when the skeleton of the foot is viewed from its lateral aspect (Fig. 6.79).
Fig. 6.79 Tarsal sinus. Lateral view, right foot.
Clinical app
Achilles tendon rupture
Rupture of the Achilles tendon is often related to sudden or direct trauma. This type of injury frequently occurs in a normal healthy tendon. In addition, there are certain conditions that may predispose the tendon to rupture. Among these conditions are tendinopathy (due to overuse, or to age-related degenerative changes) and previous Achilles tendon interventions such as injections of pharmaceuticals and the use of certain antibiotics (quinolone group). The diagnosis of Achilles tendon rupture is relatively straightforward. The patient typically complains of ‘being kicked’ or ‘shot’ behind the ankle, and clinical examination often reveals a gap in the tendon.
Intermediate tarsal bone
The intermediate tarsal bone on the medial side of the foot is the navicular (boat shaped) (see Fig. 6.76). This bone articulates behind with the talus and articulates in front and on the lateral side with the distal group of tarsal bones.
One distinctive feature of the navicular is a prominent rounded tuberosity for the attachment of the tibialis posterior tendon, which projects inferiorly on the medial side of the plantar surface of the bone.
Distal group
From lateral to medial, the distal group of tarsal bones consists of (see Fig. 6.76):
 The cuboid (Greek for “cube”), which articulates posteriorly with the calcaneus, medially with the lateral cuneiform, and anteriorly with the bases of the lateral two metatarsals—the tendon of the fibularis longus muscle lies in a prominent groove on the anterior plantar surface, which passes obliquely forward across the bone from lateral to medial.
The cuboid (Greek for “cube”), which articulates posteriorly with the calcaneus, medially with the lateral cuneiform, and anteriorly with the bases of the lateral two metatarsals—the tendon of the fibularis longus muscle lies in a prominent groove on the anterior plantar surface, which passes obliquely forward across the bone from lateral to medial.
 Three cuneiforms (Latin for “wedge”)—the lateral, intermediate, and medial cuneiform bones, in addition to articulating with each other, articulate posteriorly with the navicular bone and anteriorly with the bases of the medial three metatarsals (see Fig. 6.76).
Three cuneiforms (Latin for “wedge”)—the lateral, intermediate, and medial cuneiform bones, in addition to articulating with each other, articulate posteriorly with the navicular bone and anteriorly with the bases of the medial three metatarsals (see Fig. 6.76).
Metatarsals
There are five metatarsals in the foot, numbered I to V from medial to lateral (Fig. 6.80; also see Fig. 6.81). Metatarsal I, associated with the great toe, is shortest and thickest. The second is the longest.
Fig. 6.80 Metatarsals and phalanges. Dorsal view.
Each metatarsal has a head at the distal end, an elongate shaft in the middle, and a proximal base.
The head of each metatarsal articulates with the proximal phalanx of a toe and the base articulates with one or more of the distal group of tarsal bones. The plantar surface of the head of metatarsal I also articulates with two sesamoid bones.
The sides of the bases of metatarsals II to V also articulate with each other. The lateral side of the base of metatarsal V has a prominent tuberosity, which projects posteriorly and is the attachment site for the tendon of the fibularis brevis muscle (Fig. 6.80).
Phalanges
The phalanges are the bones of the toes (Figs. 6.80 and 6.81). Each toe has three phalanges (proximal, middle, and distal), except for the great toe, which has only two (proximal and distal).
Each phalanx consists of a base, a shaft, and a distal head:
 The base of each proximal phalanx articulates with the head of the related metatarsal.
The base of each proximal phalanx articulates with the head of the related metatarsal.
In each toe, the total length of the phalanges combined is much shorter than the length of the associated metatarsal.
Joints
Ankle joint
The ankle joint is synovial in type and involves the talus of the foot and the tibia and fibula of the leg (Fig. 6.82; also see Fig. 6.86).
The ankle joint mainly allows hingelike dorsiflexion and plantarflexion of the foot on the leg.
The distal end of the fibula is firmly anchored to the larger distal end of the tibia by strong ligaments. Together, the fibula and tibia create a deep bracket-shaped socket for the upper expanded part of the body of the talus:
 The roof of the socket is formed by the inferior surface of the distal end of the tibia.
The roof of the socket is formed by the inferior surface of the distal end of the tibia.
 The medial side of the socket is formed by the medial malleolus of the tibia.
The medial side of the socket is formed by the medial malleolus of the tibia.
 The longer lateral side of the socket is formed by the lateral malleolus of the fibula.
The longer lateral side of the socket is formed by the lateral malleolus of the fibula.
The articular surfaces are covered by hyaline cartilage.
The articular part of the talus is shaped like a short half cylinder tipped onto its flat side with one end facing lateral and the other end facing medial. The curved upper surface of the half cylinder and the two ends are covered by hyaline cartilage and fit into the bracket-shaped socket formed by the distal ends of the tibia and fibula (Fig. 6.82C).
When viewed from above, the articular surface of the talus is much wider anteriorly than it is posteriorly. As a result, the bone fits tighter into its socket when the foot is dorsiflexed and the wider surface of the talus moves into the ankle joint than when the foot is plantarflexed and the narrower part of the talus is in the joint. The joint is therefore most stable when the foot is dorsiflexed.
The articular cavity is enclosed by a synovial membrane, which attaches around the margins of the articular surfaces, and by a fibrous membrane, which covers the synovial membrane and is also attached to the adjacent bones.
The ankle joint is stabilized by medial (deltoid) and lateral ligaments (Figs. 6.83 and 6.84).
Fig. 6.83 Medial ligament of the ankle joint.
Fig. 6.84 Lateral ligament of the ankle joint. A. Lateral view. B. Posterior view.
Medial ligament (deltoid ligament)
The medial (deltoid) ligament is large, strong (Fig. 6.83), and triangular in shape. Its apex is attached above to the medial malleolus and its broad base is attached below to a line that extends from the tuberosity of the navicular bone in front to the medial tubercle of the talus behind.
The medial ligament is subdivided into four parts based on the inferior points of attachment (Fig. 6.83):
 The posterior tibiotalar part attaches to the medial side and medial tubercle of the talus.
The posterior tibiotalar part attaches to the medial side and medial tubercle of the talus.
Lateral ligament
The lateral ligament of the ankle is composed of three separate ligaments, the anterior talofibular ligament, the posterior talofibular ligament, and the calcaneofibular ligament (Fig. 6.84):
Fig. 6.85 Intertarsal joints.
Imaging app
Visualizing the ankle joint
Fig. 6.86 Normal ankle joint. A. Radiograph, lateral view. B. Radiograph, AP view. C. Coronal view of the ankle joint showing the medial ligament (deltoid ligament). T2-weighted MR image in coronal plane. D. Coronal view of ankle joint showing posterior talofibular and calcaneofibular ligaments. T2-weighted MR image in coronal plane.
Intertarsal joints
The numerous synovial joints between the individual tarsal bones mainly invert, evert, supinate, and pronate the foot (Fig. 6.85):
 Inversion and eversion is turning the whole sole of the foot inward and outward, respectively.
Inversion and eversion is turning the whole sole of the foot inward and outward, respectively.
Pronation and supination allow the foot to maintain normal contact with the ground when in different stances or when standing on irregular surfaces.
The major joints at which movements occur include the subtalar, talocalcaneonavicular, and calcaneocuboid joints (Fig. 6.85). The talocalcaneonavicular and calcaneocuboid joints together form what is often referred to as the transverse tarsal joint.
Intertarsal joints between the cuneiforms and between the cuneiforms and the navicular allow only limited movement.
The joint between the cuboid and navicular is normally fibrous.
Clinical app
Ankle injuries
The anatomy of the ankle joint is complex. However, from a clinical perspective it may be regarded as a fibro-osseous ring oriented in the coronal plane.
The upper part of the ring is formed by the distal ends of the fibula and tibia, the distal joint between the tibia and fibula, the tibiofibular ligaments, and the ankle joint itself.
The sides of the ring are formed by the ligaments that connect the medial malleolus and lateral malleolus to the adjacent tarsal bones. The medial (deltoid) ligament consists of the anterior tibiotalar, posterior tibiotalar, tibiocalcaneal, and tibionavicular parts. The lateral ligament consists of the anterior talofibular ligament, calcaneofibular ligament, and the posterior talofibular ligament.
The bottom of the ring is not part of the ankle joint but consists of the subtalar joint and the associated ligaments.
Injuries may occur as fractures or ligament disruptions. Typically, two parts of this fibro-osseous ring are disrupted. Inversion injuries of the ankle joint are common. In this injury, the anterior talofibular and calcaneofibular parts of the lateral ligament are disrupted. These structures, once disrupted, allow the ankle to invert often producing a fracture of the medial malleolus or a partial tear to the medial (deltoid) ligament.
Subtalar joint
The subtalar joint is between (Fig. 6.87):
 the large posterior calcaneal facet on the inferior surface of the talus, and
the large posterior calcaneal facet on the inferior surface of the talus, and
 the corresponding posterior talar facet on the superior surface of the calcaneus.
the corresponding posterior talar facet on the superior surface of the calcaneus.
Fig. 6.87 Interosseous talocalcaneal ligament. Lateral view.
The articular cavity is enclosed by synovial membrane, which is covered by a fibrous membrane.
The subtalar joint allows gliding and rotation, which are involved in inversion and eversion of the foot. Lateral, medial, posterior, and interosseous talocalcaneal ligaments stabilize the joint. The interosseous talocalcaneal ligament lies in the tarsal sinus (Fig. 6.87).
Talocalcaneonavicular joint
The talocalcaneonavicular joint (Fig. 6.88) is a complex joint in which the head of the talus articulates with the calcaneus and plantar calcaneonavicular ligament (spring ligament) below and the navicular in front (Fig. 6.88A).
The talocalcaneonavicular joint allows gliding and rotation movements, which together with similar movements of the subtalar joint are involved with inversion and eversion of the foot. It also participates in pronation and supination.
The parts of the talocalcaneonavicular joint between the talus and calcaneus are:
 the anterior and middle calcaneal facets on the inferior surface of the talar head, and
the anterior and middle calcaneal facets on the inferior surface of the talar head, and
 the corresponding anterior and middle talar facets on the superior surface and sustentaculum tali, respectively, of the calcaneus (Fig. 6.88B).
the corresponding anterior and middle talar facets on the superior surface and sustentaculum tali, respectively, of the calcaneus (Fig. 6.88B).
The part of the joint between the talus and the plantar calcaneonavicular ligament (spring ligament) is between the ligament and a facet on the inferior surface of the talar head.
The joint between the navicular and talus is the largest part of the talocalcaneonavicular joint and is between the ovoid anterior end of the talar head and the corresponding concave posterior surface of the navicular.
The capsule of the talocalcaneonavicular joint, which is a synovial joint, is reinforced (Fig. 6.88A,B,C):
 posteriorly by the interosseous talocalcaneal ligament,
posteriorly by the interosseous talocalcaneal ligament,
 inferiorly by the plantar calcaneonavicular ligament (spring ligament).
inferiorly by the plantar calcaneonavicular ligament (spring ligament).
The lateral part of the talocalcaneonavicular joint is reinforced by the calcaneonavicular part of the bifurcate ligament, which is a Y-shaped ligament superior to the joint (Fig. 6.88D). The base of the bifurcate ligament is attached to the anterior aspect of the superior surface of the calcaneus and its arms are attached to:
 the dorsomedial surface of the cuboid (calcaneocuboid ligament), and
the dorsomedial surface of the cuboid (calcaneocuboid ligament), and
 the dorsolateral part of the navicular (calcaneonavicular ligament).
the dorsolateral part of the navicular (calcaneonavicular ligament).
The plantar calcaneonavicular ligament (spring ligament) is a broad thick ligament that spans the space between the sustentaculum tali behind and the navicular bone in front (Fig. 6.88B,C). It supports the head of the talus, takes part in the talocalcaneonavicular joint, and resists depression of the medial arch of the foot.
Calcaneocuboid joint
The calcaneocuboid joint is a synovial joint between:
 the facet on the anterior surface of the calcaneus, and
the facet on the anterior surface of the calcaneus, and
 the corresponding facet on the posterior surface of the cuboid.
the corresponding facet on the posterior surface of the cuboid.
The calcaneocuboid joint allows sliding and rotating movements involved with inversion and eversion of the foot, and also contributes to pronation and supination of the forefoot on the hindfoot.
The calcaneocuboid joint is reinforced by the bifurcate ligament (see previous discussion) and by the long plantar ligament and the plantar calcaneocuboid ligament (short plantar ligament) (Fig. 6.89).
The plantar calcaneocuboid ligament (short plantar ligament) is short, wide, and very strong, and connects the calcaneal tubercle to the inferior surface of the cuboid (Fig. 6.89A). It not only supports the calcaneocuboid joint, but also assists the long plantar ligament in resisting depression of the lateral arch of the foot.
The long plantar ligament is the longest ligament in the sole of the foot and lies inferior to the plantar calcaneocuboid ligament (Fig. 6.89B):
More superficial fibers of the long plantar ligament extend to the bases of the metatarsal bones.
Tarsometatarsal joints
The tarsometatarsal joints between the metatarsal bones and adjacent tarsal bones are plane joints and allow limited sliding movements (Fig. 6.90).
The range of movement of the tarsometatarsal joint between the metatarsal of the great toe and the medial cuneiform is greater than that of the other tarsometatarsal joints and allows flexion, extension, and rotation. The tarsometatarsal joints, with the transverse tarsal joint, take part in pronation and supination of the foot.
Metatarsophalangeal joints
The metatarsophalangeal joints are ellipsoid synovial joints between the sphere-shaped heads of the metatarsals and the corresponding bases of the proximal phalanges of the digits.
The metatarsophalangeal joints allow extension and flexion, and limited abduction, adduction, rotation, and circumduction.
The joint capsules are reinforced by medial and lateral collateral ligaments, and by plantar ligaments, which have grooves on their plantar surfaces for the long tendons of the digits (Fig. 6.90).
Clinical app
Bunions
Clinically, a bunion is a significant protuberance of bone that may include soft tissue around the medial aspect of the first metatarsophalangeal joint. This area is an extremely important region of the foot because it is crossed by tendons and ligaments, which transmit and distribute the body’s weight during movement. It is postulated that abnormal stresses in this region of the joint may actually produce the bunion deformity. As the bunion progresses, the great toe appears to move toward the smaller toes, producing crowding of the digits. Typically the patient’s symptoms are pain, swelling, and inflammation.
Deep transverse metatarsal ligaments
Four deep transverse metatarsal ligaments link the heads of the metatarsals together and enable the metatarsals to act as a single unified structure (Fig. 6.90). The ligaments blend with the plantar ligaments of the adjacent metatarsophalangeal joints.
The metatarsal of the great toe is oriented in the same plane as the metatarsals of the other toes and is linked to the metatarsal of the second toe by a deep transverse metatarsal ligament. In addition, the joint between the metatarsal of the great toe and medial cuneiform has a limited range of motion. The great toe therefore has a very restricted independent function.
Interphalangeal joints
The interphalangeal joints are hinge joints that allow mainly flexion and extension. They are reinforced by medial and lateral collateral ligaments and by plantar ligaments (Fig. 6.90).
Tarsal tunnel, retinacula, and arrangement of major structures at the ankle
The tarsal tunnel is formed on the posteromedial side of the ankle by (Fig. 6.91):
 an overlying flexor retinaculum.
an overlying flexor retinaculum.
Flexor retinaculum
The flexor retinaculum is a straplike layer of connective tissue that spans the bony depression formed by the medial malleolus, the medial and posterior surfaces of the talus, the medial surface of calcaneus, and the inferior surface of the sustentaculum tali (Fig. 6.91). It attaches above to the medial malleolus and below and behind to the inferomedial margin of the calcaneus.
The retinaculum is continuous above with the deep fascia of the leg and below with deep fascia (plantar aponeurosis) of the foot.
Septa from the flexor retinaculum convert grooves on the bones into tubular connective tissue channels for the tendons of the flexor muscles as they pass into the sole of the foot from the posterior compartment of the leg (Fig. 6.91). Free movement of the tendons in the channels is facilitated by synovial sheaths, which surround the tendons.
Two compartments on the posterior surface of the medial malleolus are for the tendons of the tibialis posterior and flexor digitorum longus muscles. The tendon of the tibialis posterior is medial to the tendon of the flexor digitorum longus.
Immediately lateral to the tendons of the tibialis posterior and flexor digitorum longus, the posterior tibial artery with its associated veins and the tibial nerve pass through the tarsal tunnel into the sole of the foot.
Lateral to the tibial nerve is the compartment on the posterior surface of the talus and the undersurface of the sustentaculum tali for the tendon of the flexor hallucis longus muscle.
Surface anatomy
Finding the tarsal tunnel—the gateway to the foot
The tarsal tunnel (Fig. 6.92) is formed on the medial side of the foot in the groove between the medial malleolus and the heel (calcaneal tuberosity) and by the overlying flexor retinaculum.
Fig. 6.92 Finding the tarsal tunnel—the gateway to the foot.
The posterior tibial artery and tibial nerve enter the foot through the tarsal tunnel. The tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus also pass through the tarsal tunnel in compartments formed by septa of the flexor retinaculum.
The order of structures passing through the tunnel from the anteromedial to posterolateral are the tendon of the tibialis posterior, the tendon of the flexor digitorum longus, the posterior tibial artery and associated veins, the tibial nerve, and the tendon of the flexor hallucis longus (‘Tom, Dick, and a very nervous Harry’).
Extensor retinacula
Two extensor retinacula strap the tendons of the extensor muscles to the ankle region and prevent tendon bowing during extension of the foot and toes (Fig. 6.93):
Fig. 6.93 Extensor retinacula.
The tendons of the extensor digitorum longus and fibularis tertius pass through a compartment on the lateral side of the proximal foot. Medial to these tendons, the dorsalis pedis artery (terminal branch of the anterior tibial artery), the tendon of the extensor hallucis longus muscle, and finally the tendon of the tibialis anterior muscle pass under the extensor retinacula.
Fibular retinacula
Fibular (peroneal) retinacula bind the tendons of the fibularis longus and fibularis brevis muscles to the lateral side of the foot (Fig. 6.94):
 A superior fibular retinaculum extends between the lateral malleolus and the calcaneus.
A superior fibular retinaculum extends between the lateral malleolus and the calcaneus.
Fig. 6.94 Fibular retinacula. Lateral view, right foot.
At the fibular trochlea, a septum separates the compartment for the tendon of the fibularis brevis muscle above from that for the fibularis longus below.
Arches of the foot
The bones of the foot do not lie in a horizontal plane. Instead, they form longitudinal and transverse arches relative to the ground (Fig. 6.95), which absorb and distribute downward forces from the body during standing and moving on different surfaces.
Fig. 6.95 Arches of the foot. A. Longitudinal arches, right foot. B. Transverse arch, left foot.
Longitudinal arch
The longitudinal arch of the foot is formed between the posterior end of the calcaneus and the heads of the metatarsals (Fig. 6.95A). It is highest on the medial side where it forms the medial part of the longitudinal arch and lowest on the lateral side where it forms the lateral part.
Transverse arch
The transverse arch of the foot is highest in a coronal plane that cuts through the head of the talus and disappears near the heads of the metatarsals where these bones are held together by the deep transverse metatarsal ligaments (Fig. 6.95B).
Ligaments and muscles support the arches of the foot (Fig. 6.96):
Plantar aponeurosis
The plantar aponeurosis is a thickening of deep fascia in the sole of the foot (Fig. 6.97). It is firmly anchored to the medial process of the calcaneal tuberosity and extends forward as a thick band of longitudinally arranged connective tissue fibers. The fibers diverge as they pass anteriorly and form digital bands, which enter the toes and connect with bones, ligaments, and dermis of the skin.
Fig. 6.97 Plantar aponeurosis.
Distal to the metatarsophalangeal joints, the digital bands of the plantar aponeurosis are interconnected by transverse fibers, which form superficial transverse metatarsal ligaments.
The plantar aponeurosis supports the longitudinal arch of the foot and protects deeper structures in the sole.
Fibrous sheaths of toes
The tendons of the flexor digitorum longus, flexor digitorum brevis, and flexor hallucis longus muscles enter fibrous digital sheaths or tunnels on the plantar aspect of the digits (Fig. 6.98). These fibrous sheaths begin anterior to the metacarpophalangeal joints and extend to the distal phalanges. They are formed by fibrous arches and cruciate (cross-shaped) ligaments attached posteriorly to the margins of the phalanges and to the plantar ligaments associated with the metatarsophalangeal and interphalangeal joints.
Fig. 6.98 Fibrous digital sheaths.
These fibrous tunnels hold the tendons to the bony plane and prevent tendon bowing when the toes are flexed. Within each tunnel, the tendons are surrounded by a synovial sheath.
Extensor hoods
The tendons of the extensor digitorum longus, extensor digitorum brevis, and extensor hallucis longus pass into the dorsal aspect of the digits and expand over the proximal phalanges to form complex dorsal digital expansions (“extensor hoods”) (Fig. 6.99).
Fig. 6.99 Extensor hoods.
Each extensor hood is triangular in shape with the apex attached to the distal phalanx, the central region attached to the middle (toes II to V) or proximal (toe I) phalanx, and each corner of the base wrapped around the sides of the metatarsophalangeal joint. The corners of the hoods attach mainly to the deep transverse metatarsal ligaments.
Many of the intrinsic muscles of the foot insert into the free margin of the hood on each side. The attachment of these muscles into the extensor hoods allows the forces from these muscles to be distributed over the toes to cause flexion of the metatarsophalangeal joints while at the same time extending the interphalangeal joints (Fig. 6.99). The function of these movements in the foot is uncertain, but they may prevent overextension of the metatarsophalangeal joints and flexion of the interphalangeal joints when the heel is elevated off the ground and the toes grip the ground during walking.
Intrinsic muscles
Intrinsic muscles of the foot originate and insert in the foot:
 the extensor digitorum brevis and extensor hallucis brevis on the dorsal aspect of the foot (Table 6.10, Fig. 6.100);
the extensor digitorum brevis and extensor hallucis brevis on the dorsal aspect of the foot (Table 6.10, Fig. 6.100);
Table 6.10 Muscle of the dorsal aspect of the foot (spinal segments in bold are the major segments innervating the muscle)
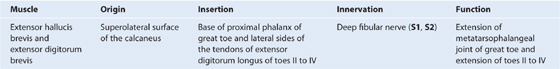
Fig. 6.100 Extensor digitorum brevis muscle.
All intrinsic muscles of the foot are innervated by the medial and lateral plantar branches of the tibial nerve except for the extensor digitorum brevis, which is innervated by the deep fibular nerve. The first two dorsal interossei also may receive part of their innervation from the deep fibular nerve.
First layer
There are three components in the first layer of muscles, which is the most superficial of the four layers in the sole of the foot and is immediately deep to the plantar aponeurosis (Table 6.11, Fig. 6.101). From medial to lateral, these muscles are the abductor hallucis, flexor digitorum brevis, and abductor digiti minimi.
Table 6.11 First layer of muscles in the sole of the foot (spinal segments in bold are the major segments innervating the muscle)
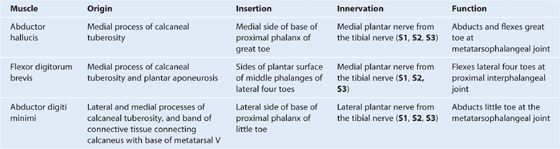
Fig. 6.101 First layer of muscles in the sole of the foot.
Second layer
The second muscle layer in the sole of the foot is associated with the tendons of the flexor digitorum longus muscle, which pass through this layer, and consists of the quadratus plantae and four lumbrical muscles (Table 6.12, Fig. 6.102).
Table 6.12 Second layer of muscles in the sole of the foot (spinal segments in bold are the major segments innervating the muscle)
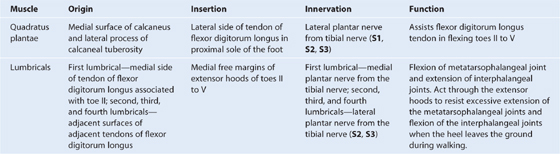
Fig. 6.102 Second layer of muscles in the sole of the foot.
Third layer
There are three muscles in the third layer in the sole of the foot (Table 6.13, Fig. 6.103):
 Two (the flexor hallucis brevis and adductor hallucis) are associated with the great toe.
Two (the flexor hallucis brevis and adductor hallucis) are associated with the great toe.
 The third (the flexor digiti minimi brevis) is associated with the little toe.
The third (the flexor digiti minimi brevis) is associated with the little toe.
Table 6.13 Third layer of muscles in the sole of the foot (spinal segments in bold are the major segments innervating the muscle)
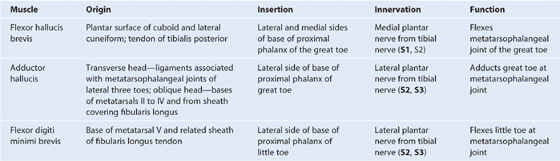
Fig. 6.103 Third layer of muscles in the sole of the foot.
Fourth layer
There are two muscle groups in the deepest muscle layer in the sole of the foot, the dorsal and plantar interossei (Table 6.14, Fig. 6.104).
Table 6.14 Fourth layer of muscles in the sole of the foot (spinal segments in bold are the major segments innervating the muscle)
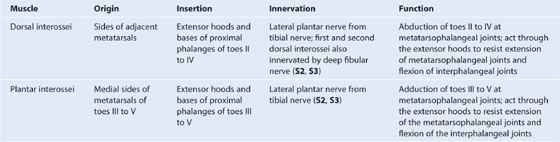
Fig. 6.104 Fourth layer of muscles in the sole of the foot.
Arteries
Blood supply to the foot is by branches of the posterior tibial and dorsalis pedis (dorsal artery of the foot) arteries.
Posterior tibial artery and plantar arch
The posterior tibial artery enters the foot through the tarsal tunnel on the medial side of the ankle and posterior to the medial malleolus. Here it bifurcates into a small medial plantar artery and a much larger lateral plantar artery (Fig. 6.105).
Fig. 6.105 Arteries in the sole of the foot.
Lateral plantar artery
The lateral plantar artery passes anterolaterally into the sole of the foot, first deep to the proximal end of the abductor hallucis muscle and then between the quadratus plantae and flexor digitorum brevis muscles (Fig. 6.105). It reaches the base of metatarsal V where it lies in the groove between the flexor digitorum brevis and abductor digiti minimi muscles. From here, the lateral plantar artery curves medially to form the deep plantar arch, which crosses the deep plane of the sole on the metatarsal bases and the interossei muscles.
Between the bases of metatarsals I and II, the deep plantar arch joins with the terminal branch (deep plantar artery) of the dorsalis pedis artery, which enters the sole from the dorsal side of the foot.
Major branches of the deep plantar arch include:
 a digital branch to the lateral side of the little toe;
a digital branch to the lateral side of the little toe;
 four plantar metatarsal arteries, which supply digital branches to adjacent sides of toes I to V and the medial side of the great toe; and
four plantar metatarsal arteries, which supply digital branches to adjacent sides of toes I to V and the medial side of the great toe; and
Medial plantar artery
The medial plantar artery passes into the sole of the foot by passing deep to the proximal end of the abductor hallucis muscle (Fig. 6.105). It supplies a deep branch to adjacent muscles and then passes forward in the groove between the abductor hallucis and the flexor digitorum brevis muscles. It ends by joining the digital branch of the deep plantar arch, which supplies the medial side of the great toe.
Near the base of metatarsal I, the medial plantar artery gives rise to a superficial branch, which divides into three vessels that pass superficial to the flexor digitorum brevis muscle to join the plantar metatarsal arteries from the deep plantar arch.
Dorsalis pedis artery
The dorsalis pedis artery is the continuation of the anterior tibial artery and begins as the anterior tibial artery crosses the ankle joint (Fig. 6.106). It passes anteriorly over the dorsal aspect of the talus, navicular, and intermediate cuneiform bones, and then passes inferiorly, as the deep plantar artery, between the two heads of the first dorsal interosseous muscle to join the deep plantar arch in the sole of the foot.
Fig. 6.106 Dorsalis pedis artery.
Branches of the dorsalis pedis artery include lateral and medial tarsal branches, an arcuate artery, and a first dorsal metatarsal artery (Fig. 6.106):
The dorsal metatarsal arteries connect with perforating branches from the deep plantar arch and similar branches from the plantar metatarsal arteries.
Surface anatomy
Finding the dorsalis pedis artery
The nature of the dorsalis pedis pulse (Fig. 6.107) is important for assessing peripheral circulation because the dorsalis pedis artery is the farthest palpable vessel from the heart. Also, it is the lowest palpable artery in the body when a person is standing.
Fig. 6.107 Finding the dorsalis pedis artery.
The dorsalis pedis artery passes onto the dorsal aspect of the foot and anteriorly over the tarsal bones where it lies between and is parallel to the tendon of the extensor hallucis longus and the tendon of the extensor digitorum longus to the second toe. It is palpable in this position. The terminal branch of the dorsalis pedis artery passes into the plantar surface of the foot between the two heads of the first dorsal interosseous muscle.
Veins
There are interconnected networks of deep and superficial veins in the foot. The deep veins follow the arteries. Superficial veins drain into a dorsal venous arch on the dorsal surface of the foot over the metatarsals (Fig. 6.108):
Fig. 6.108 Superficial veins of the foot.
Nerves
The foot is supplied by the tibial, deep fibular, superficial fibular, sural, and saphenous nerves:
 All five nerves contribute to cutaneous or general sensory innervation.
All five nerves contribute to cutaneous or general sensory innervation.
Tibial nerve
The tibial nerve enters the foot through the tarsal tunnel posterior to the medial malleolus. In the tunnel, the nerve is lateral to the posterior tibial artery, and gives origin to medial calcaneal branches, which penetrate the flexor retinaculum to supply the heel. Midway between the medial malleolus and the heel, the tibial nerve bifurcates with the posterior tibial artery into (Fig. 6.109):
 a large medial plantar nerve, and
a large medial plantar nerve, and
 a smaller lateral plantar nerve.
a smaller lateral plantar nerve.
Fig. 6.109 Lateral and medial plantar nerves. A. Sole of the right foot. B. Cutaneous distribution.
The medial and lateral plantar nerves lie together between their corresponding arteries.
Medial plantar nerve
The medial plantar nerve is the major sensory nerve in the sole of the foot (Fig. 6.109B). It innervates skin on most of the anterior two-thirds of the sole and adjacent surfaces of the medial three and one-half toes, which includes the great toe. In addition to this large area of plantar skin, the nerve also innervates four intrinsic muscles—the abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, and the first lumbrical.
The medial plantar nerve supplies a digital branch (proper plantar digital nerve) to the medial side of the great toe and then divides into three nerves (common plantar digital nerves) on the plantar surface of the flexor digitorum brevis, which continue forward to supply proper plantar digital branches to adjacent surfaces of toes I to IV. The nerve to the first lumbrical originates from the first common plantar digital nerve.
Lateral plantar nerve
The lateral plantar nerve is an important motor nerve in the foot because it innervates all intrinsic muscles in the sole, except for the muscles supplied by the medial plantar nerve (the abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, and first lumbrical; Fig. 6.109). It also innervates a strip of skin on the lateral side of the anterior two-thirds of the sole and the adjacent plantar surfaces of the lateral one and one-half digits.
The lateral plantar nerve enters the sole of the foot by passing deep to the proximal attachment of the abductor hallucis muscle. It continues laterally and anteriorly across the sole between the flexor digitorum brevis and quadratus plantae muscles, supplying branches to both these muscles, and then divides near the head of metatarsal V into a deep and superficial branch (Fig. 6.109).
The superficial branch of the lateral plantar nerve gives rise to a proper plantar digital nerve, which supplies skin on the lateral side of the little toe and to a common plantar digital nerve, which divides to supply proper plantar digital nerves to skin on the adjacent sides of toes IV and V.
The proper plantar digital nerve to the lateral side of the little toe also innervates the flexor digiti minimi brevis and the dorsal and plantar interossei muscles between metatarsals IV and V.
The deep branch of the lateral plantar nerve is motor and accompanies the lateral plantar artery deep to the long flexor tendons and the adductor hallucis muscle. It supplies branches to the second to fourth lumbrical muscles, the adductor hallucis muscle, and all interossei except those between metatarsals IV and V, which are innervated by the superficial branch.
Clinical app
Morton’s neuroma
A Morton’s neuroma is an enlarged common plantar nerve, usually in the third interspace between the third and fourth toes. In this region of the foot the lateral plantar nerve often unites with the medial plantar nerve. As the two nerves join, the resulting nerve is typically larger in diameter than those of the other toes. Also, it is in a relatively subcutaneous position, just above the fat pad of the foot close to the artery and the vein. Above the nerve is the deep transverse metatarsal ligament, which is a broad strong structure holding the metatarsals together. Typically, as the patient enters the “push off” phase of walking the interdigital nerve is sandwiched between the ground and the deep transverse metatarsal ligament. The forces tend to compress the common plantar nerve, which can be irritated, in which case there is usually some associated inflammatory change and thickening.
Typically, patients experience pain in the third interspace, which may be sharp or dull and is usually worsened by wearing shoes and walking.
Deep fibular nerve
The deep fibular nerve innervates the extensor digitorum brevis, contributes to the innervation of the first two dorsal interossei muscles, and supplies general sensory branches to the skin on the adjacent dorsal sides of the first and second toes and to the web space between them (Fig. 6.110).
Fig. 6.110 A. Terminal branches of superficial and deep fibular nerves in the foot. B. Cutaneous distribution.
The deep fibular nerve enters the dorsal aspect of the foot on the lateral side of the dorsalis pedis artery, and is parallel with and lateral to the tendon of the extensor hallucis longus muscle. Just distal to the ankle joint, the nerve gives origin to a lateral branch, which innervates the extensor digitorum brevis from its deep surface.
The deep fibular nerve continues forward on the dorsal surface of the foot, penetrates deep fascia between metatarsals I and II near the metatarsophalangeal joints, and then divides into two dorsal digital nerves, which supply skin over adjacent surfaces of toes I and II down to the beginning of the nail beds (Fig. 6.110).
Small motor branches, which contribute to the supply of the first two dorsal interossei muscles, originate from the deep fibular nerve before it penetrates deep fascia.
Superficial fibular nerve
The superficial fibular nerve is sensory to most skin on the dorsal aspect of the foot and toes except for skin on adjacent sides of toes I and II (which is innervated by the deep fibular nerve) and skin on the lateral side of the foot and little toe (which is innervated by the sural nerve; Fig. 6.110).
The superficial fibular nerve penetrates deep fascia on the anterolateral side of the lower leg and enters the dorsal aspect of the foot in superficial fascia. It gives rise to cutaneous branches and dorsal digital nerves along its course.
Sural nerve
The sural nerve is a cutaneous branch of the tibial nerve that originates high in the leg. It enters the foot in superficial fascia posterior to the lateral malleolus close to the short saphenous vein. Terminal branches innervate skin on the lateral side of the foot and dorsolateral surface of the little toe (Fig. 6.110B).
Saphenous nerve
The saphenous nerve is a cutaneous branch of the femoral nerve that originates in the thigh. Terminal branches enter the foot in superficial fascia on the medial side of the ankle and supply skin on the medial side of the proximal foot (Fig. 6.110B).
Clinical app
Dermatomes and myotomes in the lower limb
General sensory and somatic motor innervation of the lower limb is by peripheral nerves emanating from the lumbar and sacral plexuses on the posterior abdominal and pelvic walls. These plexuses are formed by the anterior rami of L1 to L3 and most of L4 (lumbar plexus) and L4 to S5 (sacral plexus).
Nerves originating from the lumbar and sacral plexuses and entering the lower limb carry fibers from spinal cord levels L1 to S3. As a consequence of this innervation, lumbar and upper sacral nerves are tested clinically by examining the lower limb. In addition, clinical signs (such as pain, pins and needles, paresthesia, and fascicular muscle twitching) resulting from any disorder affecting these spinal nerves (e.g., herniated intervertebral disc in the lumbar region) appear in the lower limb.
Dermatomes in the lower limb are shown in Figure 6.111. Regions that can be tested for sensation and are reasonably autonomous (have minimal overlap) are:
 lower medial side of the thigh—L3
lower medial side of the thigh—L3
 medial side of the great toe (digit I)—L4
medial side of the great toe (digit I)—L4
Fig. 6.111 Dermatomes of the lower limb. Dots indicate autonomous zones (i.e., with minimal overlap).
Selected joint movements are used to test myotomes (Fig. 6.112). For example:
 Flexion of the hip is controlled primarily by L1 and L2.
Flexion of the hip is controlled primarily by L1 and L2.
 Extension of the knee is controlled mainly by L3 and L4.
Extension of the knee is controlled mainly by L3 and L4.
 Knee flexion is controlled mainly by L5 to S2.
Knee flexion is controlled mainly by L5 to S2.
 Plantarflexion of the foot is controlled predominantly by S1 and S2.
Plantarflexion of the foot is controlled predominantly by S1 and S2.
 Adduction of the digits is controlled by S2 and S3.
Adduction of the digits is controlled by S2 and S3.
Fig. 6.112 Movements generated by myotomes.
Clinical app
Testing sensory innervation carried by major peripheral nerves in the lower limb
In addition to innervating major muscle groups, each of the major peripheral nerves originating from the lumbar and sacral plexuses carries general sensory information from patches of skin (Fig. 6.113). Sensation from these areas can be used to test for peripheral nerve lesions:
 The obturator nerve innervates the medial side of the thigh.
The obturator nerve innervates the medial side of the thigh.
 The tibial part of the sciatic nerve innervates the lateral side of the ankle and foot.
The tibial part of the sciatic nerve innervates the lateral side of the ankle and foot.
 The common fibular nerve innervates the lateral side of the leg and the dorsum of the foot.
The common fibular nerve innervates the lateral side of the leg and the dorsum of the foot.
Clinical app
Tendon taps in the lower limb
In an unconscious patient, both somatic sensory and somatic motor functions of spinal cord levels can be tested using tendon reflexes:
 A tap on the patellar ligament at the knee tests predominantly L3 and L4.
A tap on the patellar ligament at the knee tests predominantly L3 and L4.
Clinical app
Gait and gait defects
The body’s center of gravity lies just anterior to the anterior edge of the SII vertebra in the pelvis. During walking, many anatomic features of the lower limbs contribute to minimizing fluctuations in the body’s center of gravity and thereby reduce the amount of energy needed to maintain locomotion and produce a smooth, efficient gait (Fig. 6.114). They include pelvic tilt in the coronal plane, pelvic rotation in the transverse plane, movement of the knees toward the midline, flexion of the knees, and complex interactions between the hip, knee, and ankle. As a result, during walking, the body’s center of gravity normally fluctuates only 5 cm in both vertical and lateral directions.
Fig. 6.114 Some of the determinants of gait.
Any pathology that alters the determinants of gait changes the gait pattern and increases the amount of energy required to walk.

 PT Case Studies
PT Case Studies Medical Clinical Case Studies
Medical Clinical Case Studies Clinical Cases
Clinical Cases The gluteal region is posterolateral and between the iliac crest and the fold of skin (gluteal fold) that defines the lower limit of the buttocks. The major bone of the gluteal region is the pelvic bone.
The gluteal region is posterolateral and between the iliac crest and the fold of skin (gluteal fold) that defines the lower limit of the buttocks. The major bone of the gluteal region is the pelvic bone. Anteriorly, the thigh is between the inguinal ligament and the knee joint—the hip joint is just inferior to the middle third of the inguinal ligament, and the posterior thigh is between the gluteal fold and the knee. The bone of the thigh is the femur.
Anteriorly, the thigh is between the inguinal ligament and the knee joint—the hip joint is just inferior to the middle third of the inguinal ligament, and the posterior thigh is between the gluteal fold and the knee. The bone of the thigh is the femur. The foot is distal to the ankle joint. Bones of the foot are the tarsals, metatarsals, and phalanges.
The foot is distal to the ankle joint. Bones of the foot are the tarsals, metatarsals, and phalanges.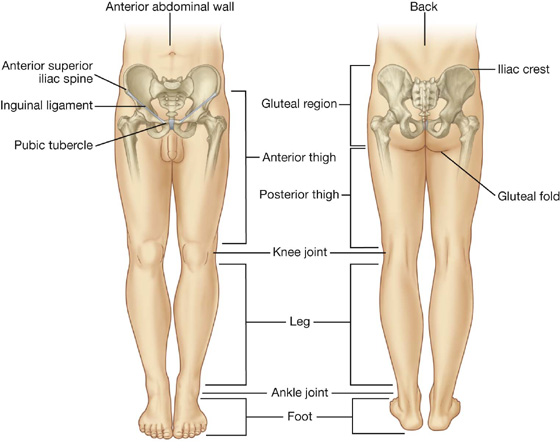

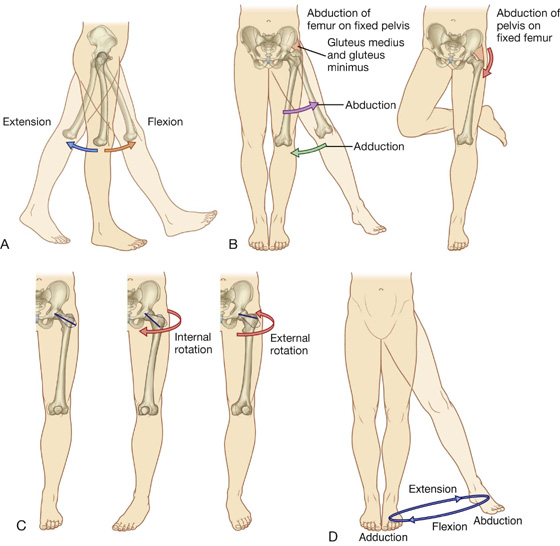
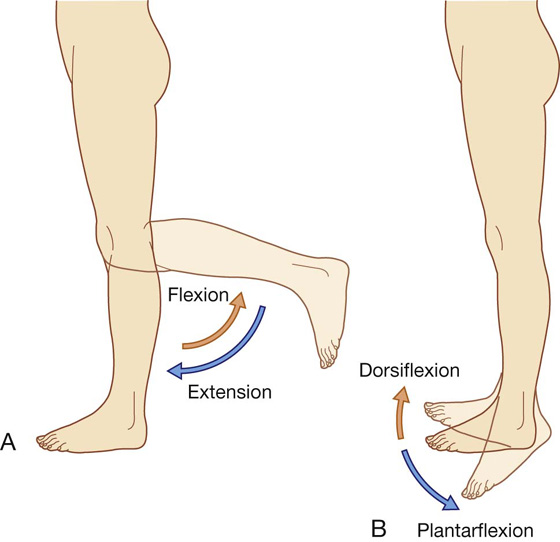
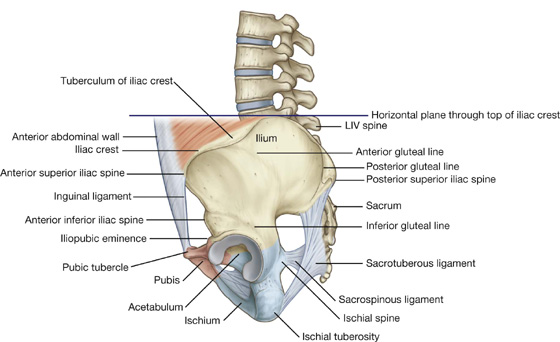
 The inferior gluteal line originates just superior to the anterior inferior iliac spine and curves inferiorly across the bone to end near the posterior margin of the acetabulum.
The inferior gluteal line originates just superior to the anterior inferior iliac spine and curves inferiorly across the bone to end near the posterior margin of the acetabulum. The anterior gluteal line originates from the lateral margin of the iliac crest between the anterior superior iliac spine and the tuberculum of iliac crest, and arches inferiorly across the ilium to disappear just superior to the upper margin of the greater sciatic foramen.
The anterior gluteal line originates from the lateral margin of the iliac crest between the anterior superior iliac spine and the tuberculum of iliac crest, and arches inferiorly across the ilium to disappear just superior to the upper margin of the greater sciatic foramen. The posterior gluteal line descends almost vertically from the iliac crest to a position near the posterior inferior iliac spine.
The posterior gluteal line descends almost vertically from the iliac crest to a position near the posterior inferior iliac spine.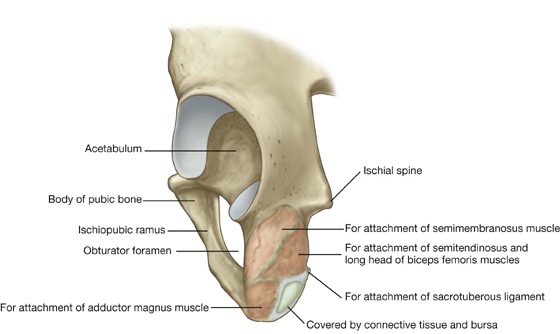
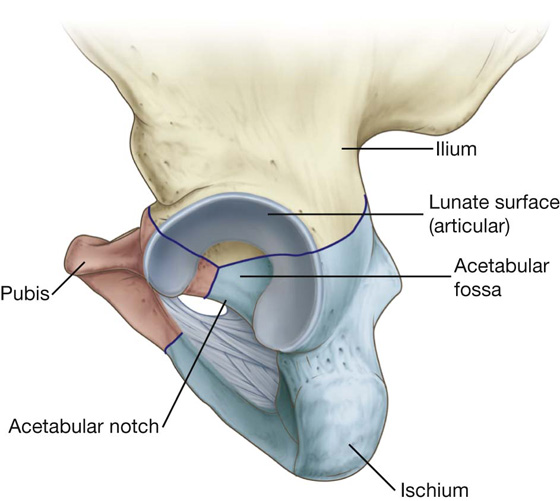
 Type 1 injuries occur without disruption of the bony pelvic ring (e.g., a fracture of the iliac crest). These types of injuries are unlikely to represent significant trauma, though in the case of a fracture of the iliac crest, blood loss needs to be assessed.
Type 1 injuries occur without disruption of the bony pelvic ring (e.g., a fracture of the iliac crest). These types of injuries are unlikely to represent significant trauma, though in the case of a fracture of the iliac crest, blood loss needs to be assessed. Type 2 injuries occur with a single break in the bony pelvic ring. An example of this would be a single fracture with diastasis (separation) of the pubic symphysis.
Type 2 injuries occur with a single break in the bony pelvic ring. An example of this would be a single fracture with diastasis (separation) of the pubic symphysis. Type 3 injuries occur with double breaks in the bony pelvic ring. These include bilateral fractures of the pubic rami, which may produce urethral damage.
Type 3 injuries occur with double breaks in the bony pelvic ring. These include bilateral fractures of the pubic rami, which may produce urethral damage.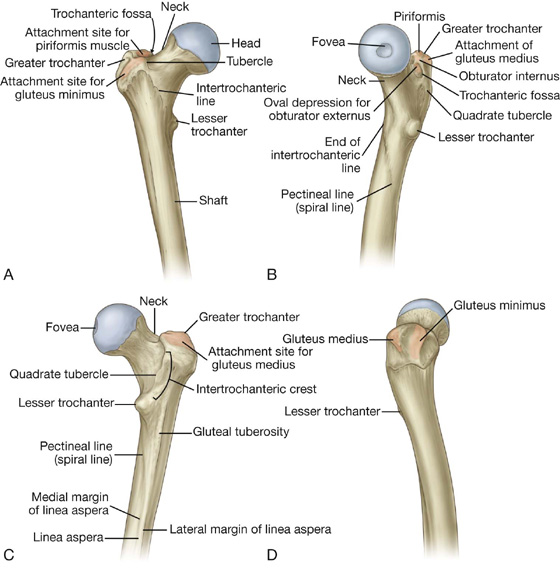
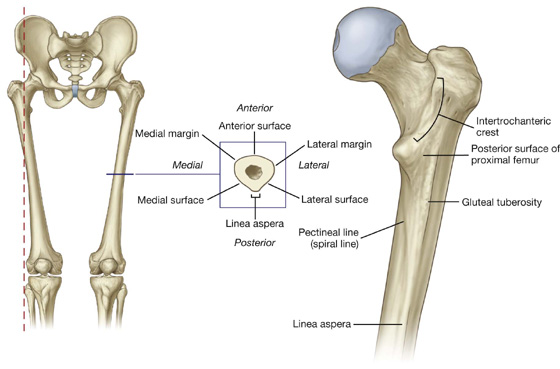
 The pectineal line curves anteriorly under the lesser trochanter and joins the intertrochanteric line.
The pectineal line curves anteriorly under the lesser trochanter and joins the intertrochanteric line. The gluteal tuberosity is a broad linear roughening that curves laterally to the base of the greater trochanter.
The gluteal tuberosity is a broad linear roughening that curves laterally to the base of the greater trochanter.
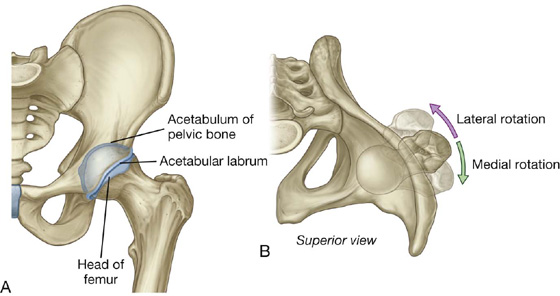

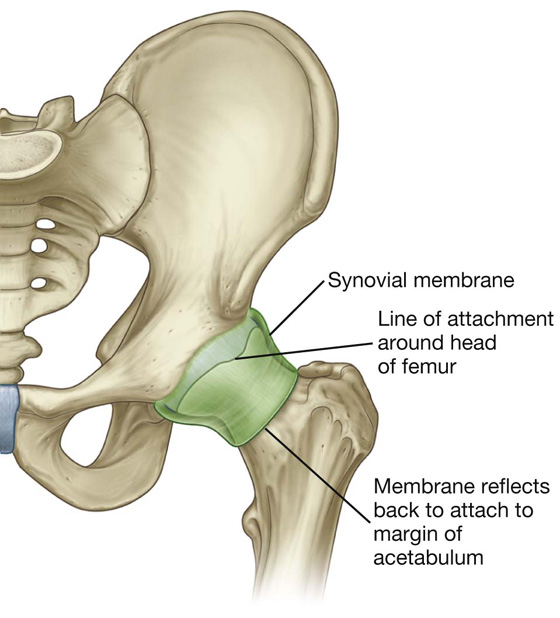


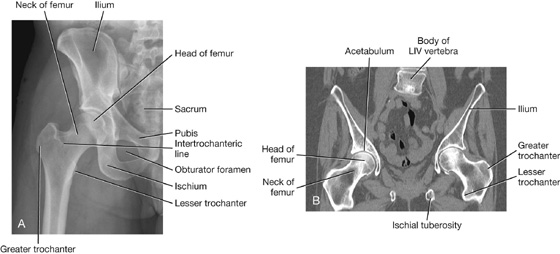
 Obturator canal — an almost vertically oriented passageway at the anterosuperior edge of the obturator foramen. The obturator canal connects the abdominopelvic region with the medial compartment of the thigh.
Obturator canal — an almost vertically oriented passageway at the anterosuperior edge of the obturator foramen. The obturator canal connects the abdominopelvic region with the medial compartment of the thigh.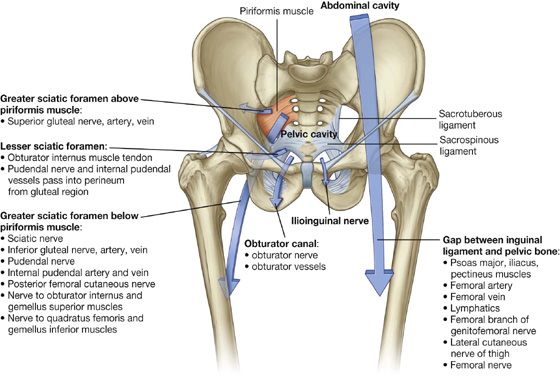
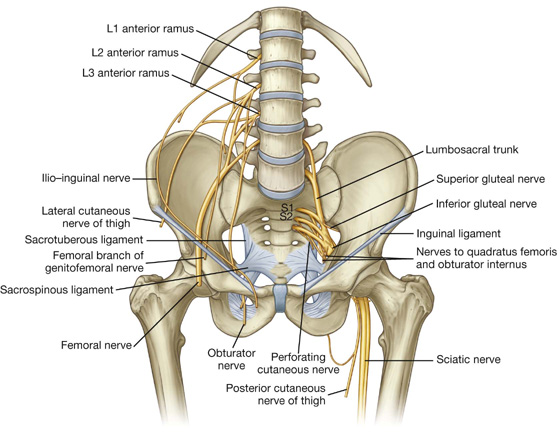
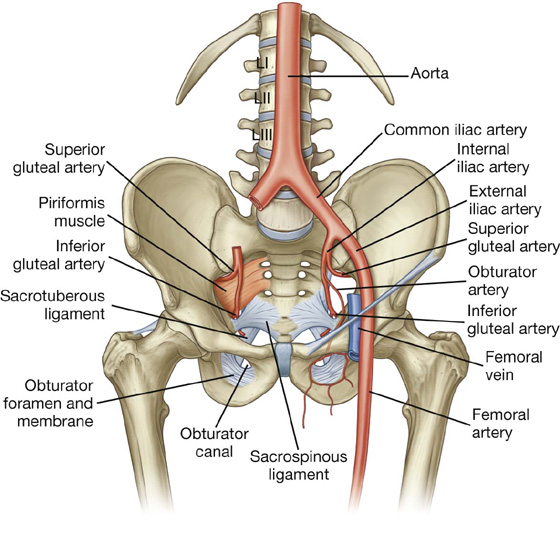

 The small saphenous vein originates from the lateral side of the dorsal venous arch, ascends up the posterior surface of the leg, and then penetrates deep fascia to join the popliteal vein posterior to the knee; proximal to the knee, the popliteal vein becomes the femoral vein.
The small saphenous vein originates from the lateral side of the dorsal venous arch, ascends up the posterior surface of the leg, and then penetrates deep fascia to join the popliteal vein posterior to the knee; proximal to the knee, the popliteal vein becomes the femoral vein.

 The tensor fasciae latae muscle is partially enclosed by and inserts into the superior and anterior aspects of the iliotibial tract.
The tensor fasciae latae muscle is partially enclosed by and inserts into the superior and anterior aspects of the iliotibial tract.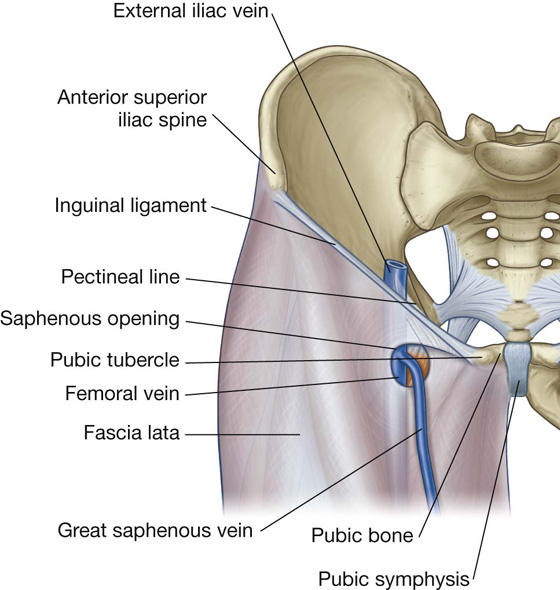
 The medial border is the medial margin of the adductor longus muscle in the medial compartment of the thigh.
The medial border is the medial margin of the adductor longus muscle in the medial compartment of the thigh. The lateral margin is the medial margin of the sartorius muscle in the anterior compartment of the thigh.
The lateral margin is the medial margin of the sartorius muscle in the anterior compartment of the thigh. The floor of the triangle is formed medially by the pectineus and adductor longus muscles in the medial compartment of the thigh and laterally by the iliopsoas muscle descending from the abdomen.
The floor of the triangle is formed medially by the pectineus and adductor longus muscles in the medial compartment of the thigh and laterally by the iliopsoas muscle descending from the abdomen. The apex of the femoral triangle points inferiorly and is continuous with a fascial canal (adductor canal), which descends medially down the thigh and posteriorly through an aperture in the lower end of one of the largest of the adductor muscles in the thigh (the adductor magnus muscle) to open into the popliteal fossa behind the knee.
The apex of the femoral triangle points inferiorly and is continuous with a fascial canal (adductor canal), which descends medially down the thigh and posteriorly through an aperture in the lower end of one of the largest of the adductor muscles in the thigh (the adductor magnus muscle) to open into the popliteal fossa behind the knee.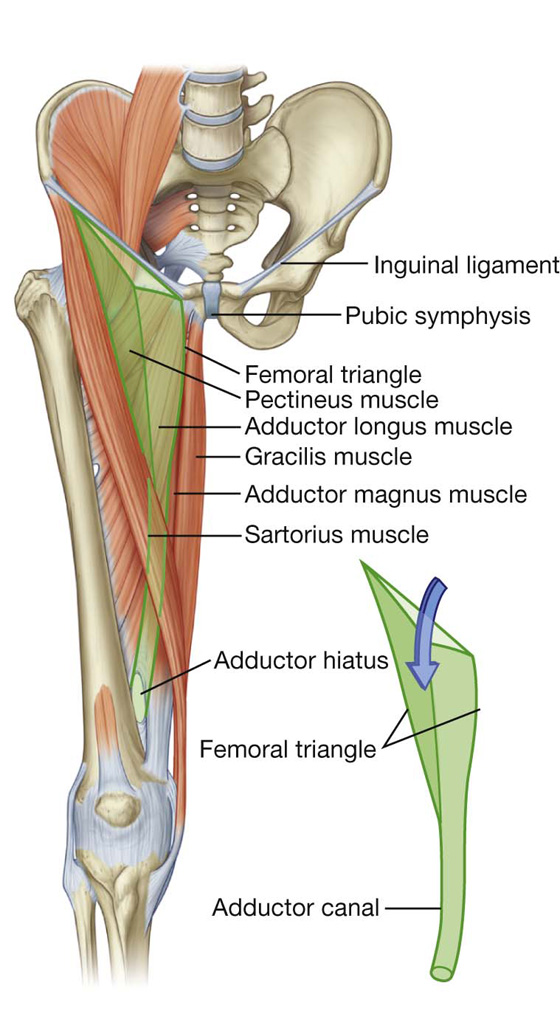
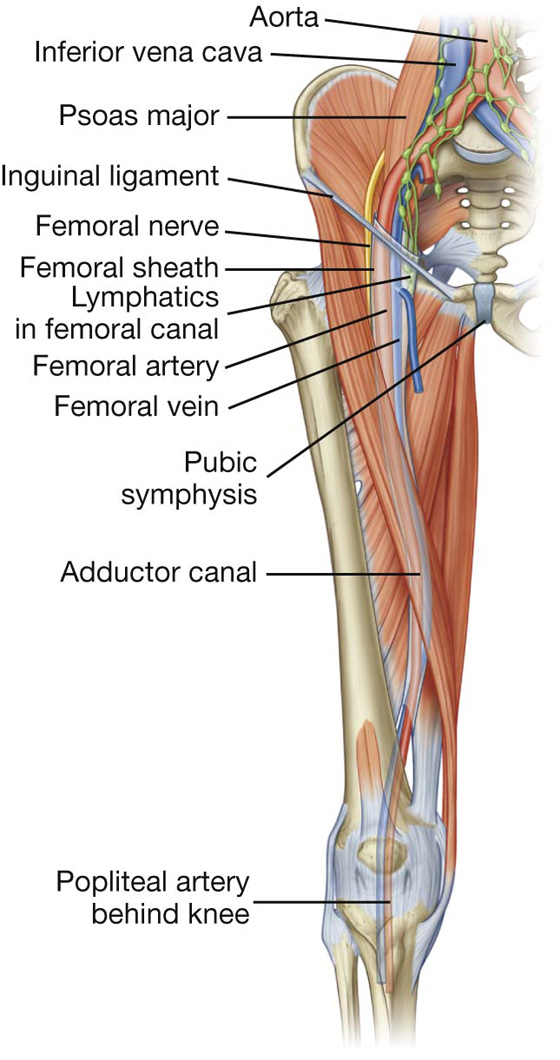
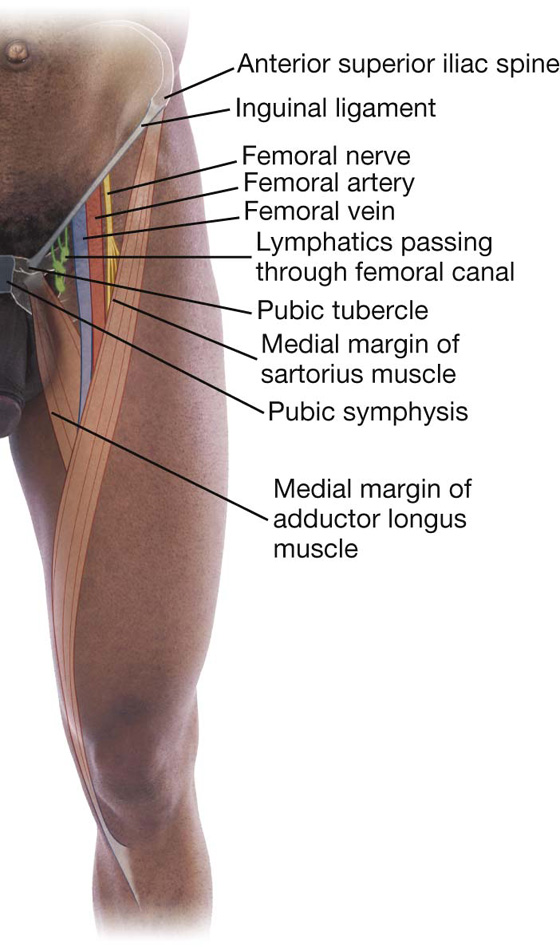
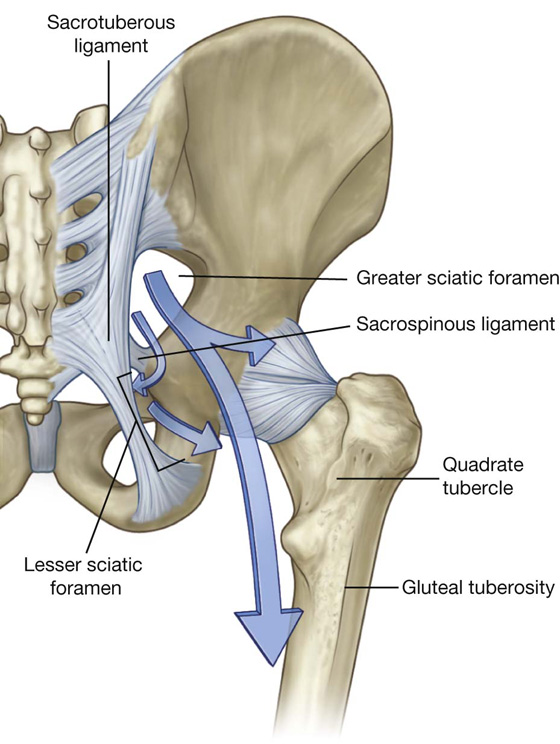
 a deep group of small muscles, which are mainly lateral rotators of the femur at the hip joint and include the piriformis, obturator internus, gemellus superior, gemellus inferior, and quadratus femoris;
a deep group of small muscles, which are mainly lateral rotators of the femur at the hip joint and include the piriformis, obturator internus, gemellus superior, gemellus inferior, and quadratus femoris; a more superficial group of larger muscles, which mainly abduct and extend the hip and include the gluteus minimus, gluteus medius, and gluteus maximus. An additional muscle in this group, the tensor fasciae latae, stabilizes the knee in extension by acting on a specialized longitudinal band of deep fascia (the iliotibial tract) that passes down the lateral side of the thigh to attach to the proximal end of the tibia in the leg.
a more superficial group of larger muscles, which mainly abduct and extend the hip and include the gluteus minimus, gluteus medius, and gluteus maximus. An additional muscle in this group, the tensor fasciae latae, stabilizes the knee in extension by acting on a specialized longitudinal band of deep fascia (the iliotibial tract) that passes down the lateral side of the thigh to attach to the proximal end of the tibia in the leg.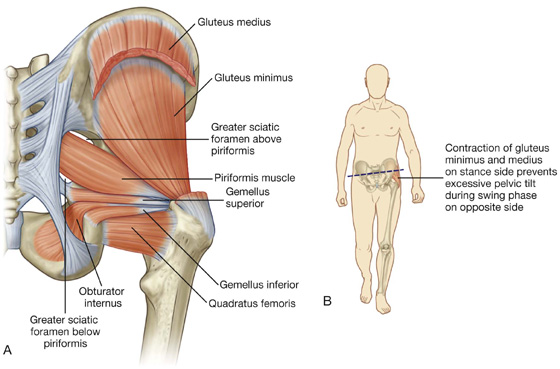
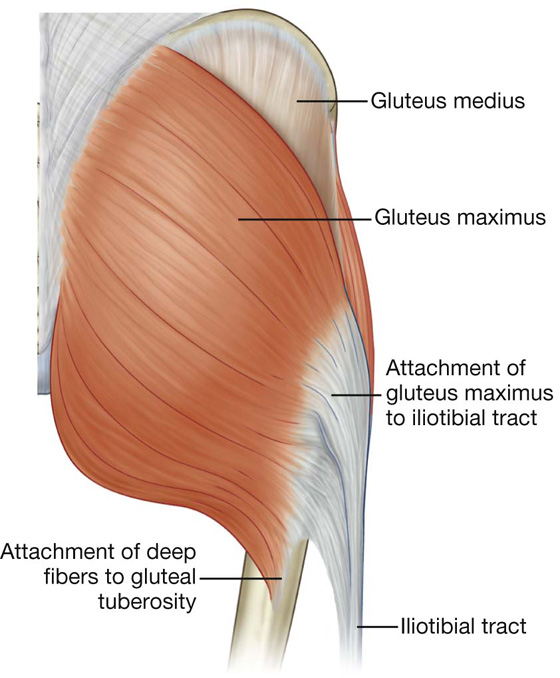
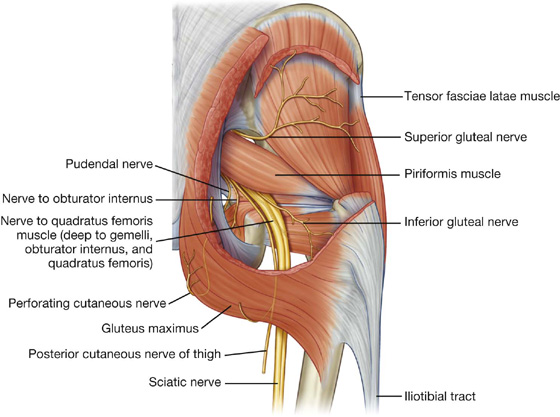
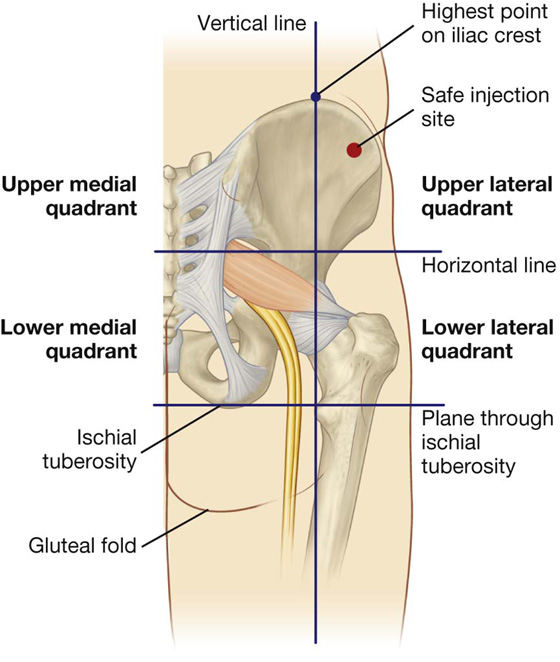
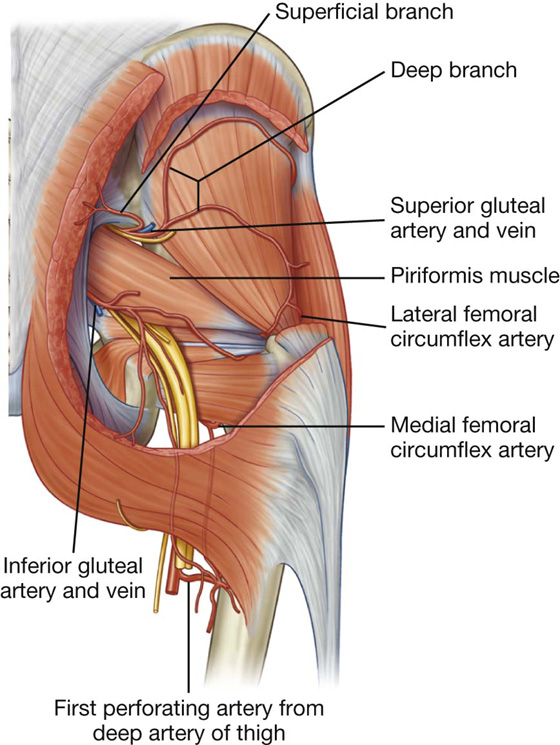
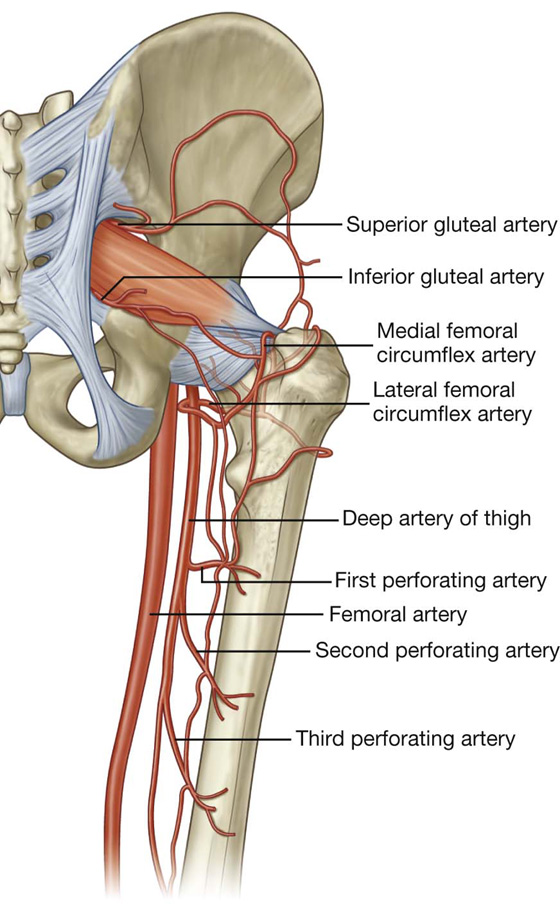
 Posteriorly, it is separated from the gluteal region by the gluteal fold superficially, and by the inferior margins of the gluteus maximus and quadratus femoris on deeper planes.
Posteriorly, it is separated from the gluteal region by the gluteal fold superficially, and by the inferior margins of the gluteus maximus and quadratus femoris on deeper planes.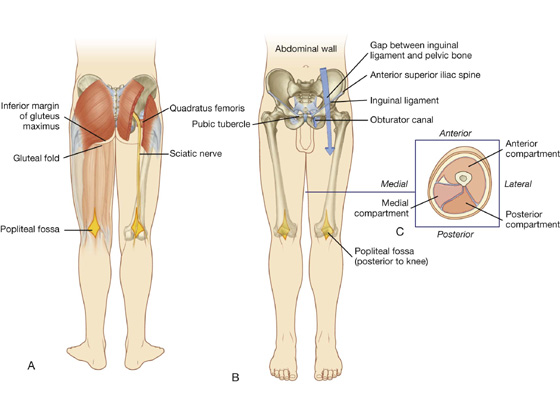

 Its apex is pointed inferiorly for attachment to the patellar ligament, which connects the patella to the tibia.
Its apex is pointed inferiorly for attachment to the patellar ligament, which connects the patella to the tibia.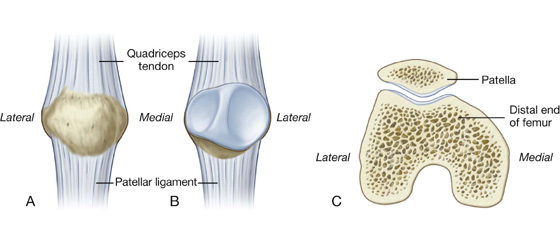
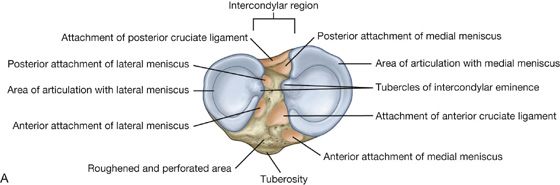
 The anterior border is sharp and descends from the tibial tuberosity, where it is continuous superiorly with a ridge that passes along the lateral margin of the tuberosity and onto the lateral condyle.
The anterior border is sharp and descends from the tibial tuberosity, where it is continuous superiorly with a ridge that passes along the lateral margin of the tuberosity and onto the lateral condyle. The interosseous border is a subtle vertical ridge that descends along the lateral aspect of the tibia from the region of bone anterior and inferior to the articular facet for the head of the fibula.
The interosseous border is a subtle vertical ridge that descends along the lateral aspect of the tibia from the region of bone anterior and inferior to the articular facet for the head of the fibula. The medial border is indistinct superiorly, where it begins at the anterior end of the groove on the posterior surface of the medial tibial condyle, but is sharp in the midshaft.
The medial border is indistinct superiorly, where it begins at the anterior end of the groove on the posterior surface of the medial tibial condyle, but is sharp in the midshaft.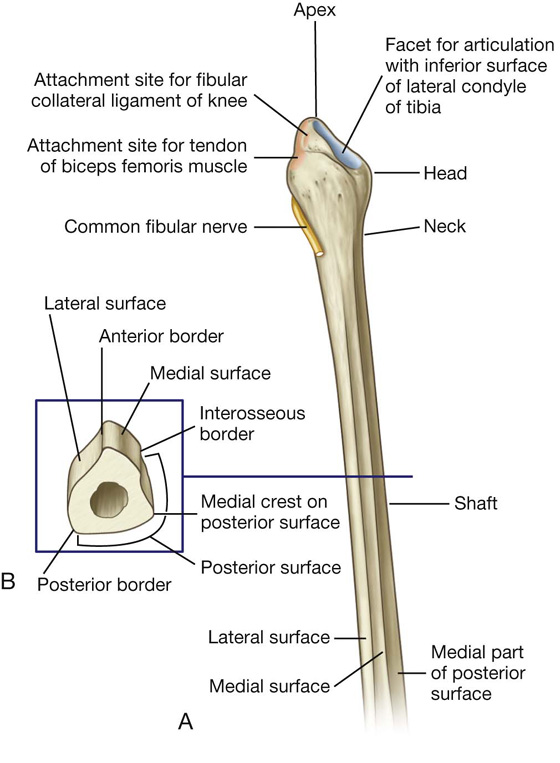
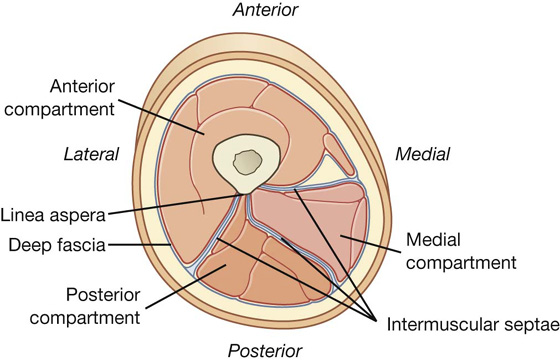
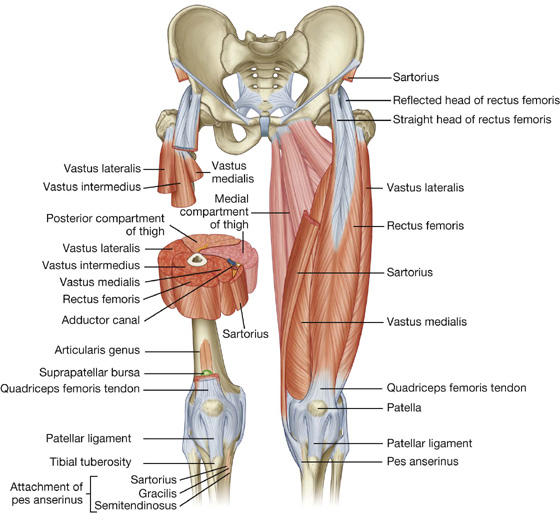
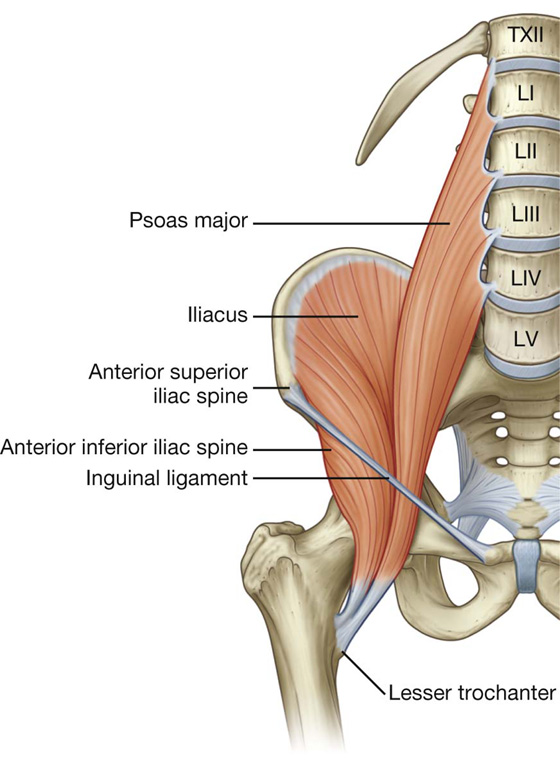
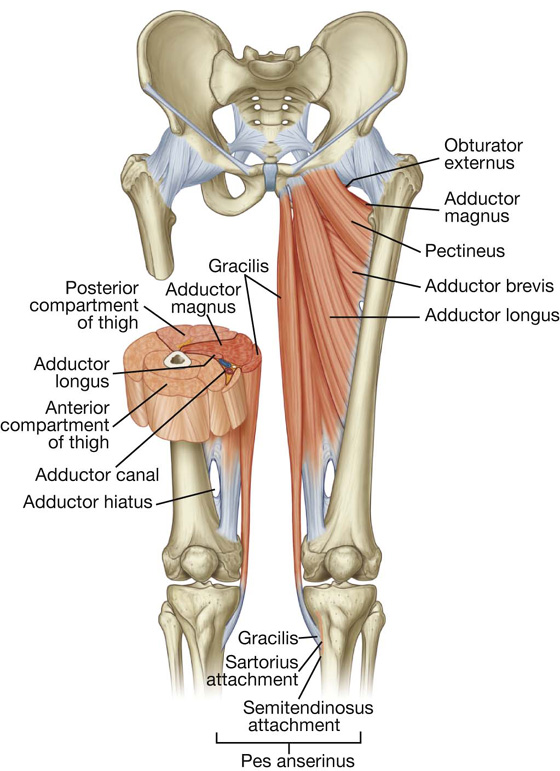
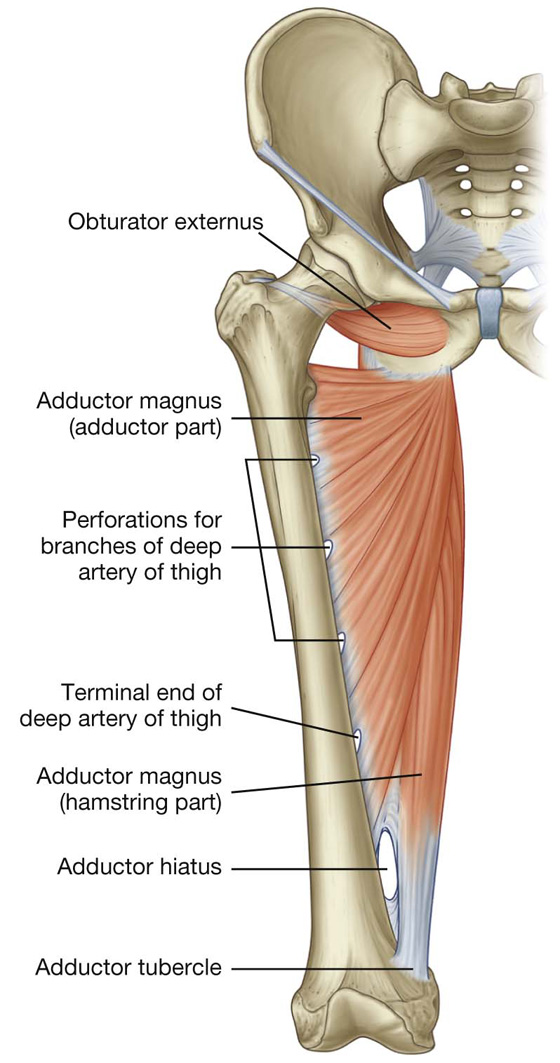
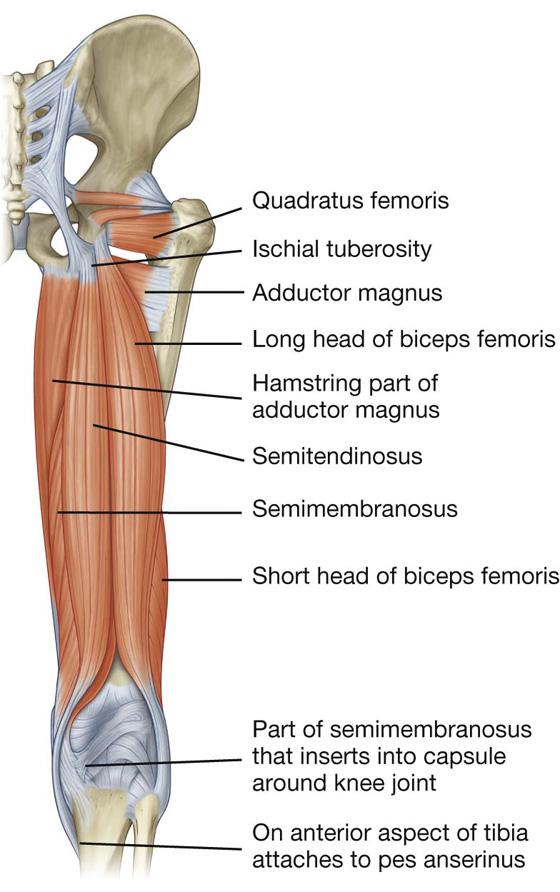
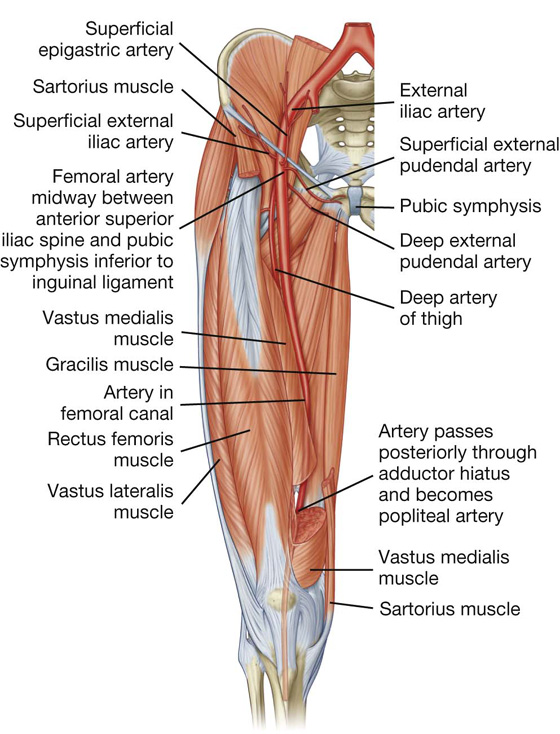
 posteriorly between the pectineus and adductor longus muscles and then between the adductor longus and adductor brevis muscles; and
posteriorly between the pectineus and adductor longus muscles and then between the adductor longus and adductor brevis muscles; and then travels inferiorly between the adductor longus and adductor magnus, eventually penetrating through the adductor magnus to connect with branches of the popliteal artery behind the knee.
then travels inferiorly between the adductor longus and adductor magnus, eventually penetrating through the adductor magnus to connect with branches of the popliteal artery behind the knee.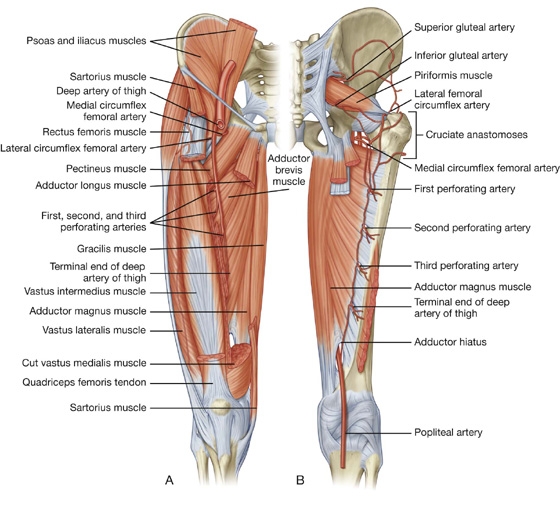
 One vessel (ascending branch) ascends laterally deep to the tensor fasciae latae muscle and connects with a branch of the medial circumflex femoral artery to form a channel, which circles the neck of the femur and supplies the neck and head of the femur.
One vessel (ascending branch) ascends laterally deep to the tensor fasciae latae muscle and connects with a branch of the medial circumflex femoral artery to form a channel, which circles the neck of the femur and supplies the neck and head of the femur. One vessel (descending branch) descends deep to the rectus femoris, penetrates the vastus lateralis muscle and connects with a branch of the popliteal artery near the knee.
One vessel (descending branch) descends deep to the rectus femoris, penetrates the vastus lateralis muscle and connects with a branch of the popliteal artery near the knee. One branch ascends to the trochanteric fossa and connects with branches of the gluteal and lateral circumflex femoral arteries.
One branch ascends to the trochanteric fossa and connects with branches of the gluteal and lateral circumflex femoral arteries. The other branch passes laterally to participate with branches from the lateral femoral circumflex artery, the inferior gluteal artery, and the first perforating artery in forming an anastomotic network of vessels around the hip.
The other branch passes laterally to participate with branches from the lateral femoral circumflex artery, the inferior gluteal artery, and the first perforating artery in forming an anastomotic network of vessels around the hip.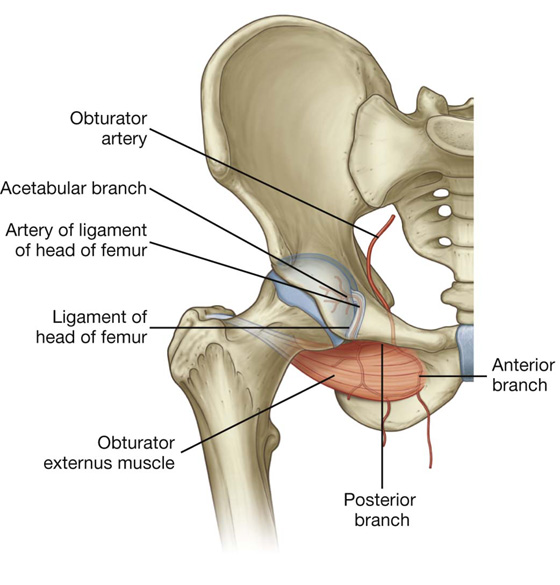
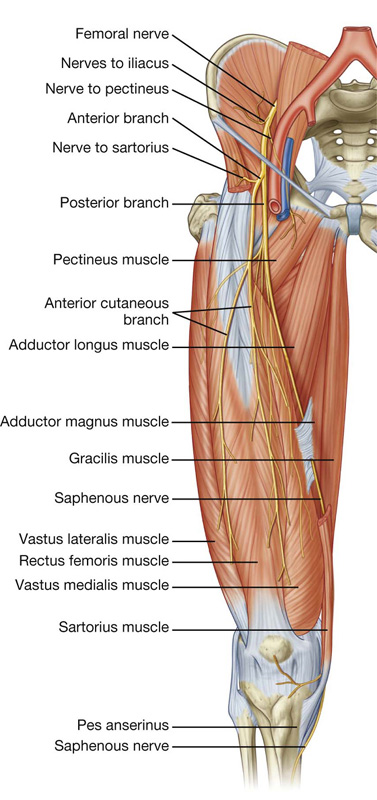
 anterior cutaneous branches, which penetrate deep fascia to supply skin on the front of the thigh and knee;
anterior cutaneous branches, which penetrate deep fascia to supply skin on the front of the thigh and knee; numerous motor nerves, which supply the quadriceps femoris muscle (rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis muscles) and the sartorius muscle; and
numerous motor nerves, which supply the quadriceps femoris muscle (rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis muscles) and the sartorius muscle; and one long cutaneous nerve, the saphenous nerve, which supplies skin as far distally as the medial side of the foot.
one long cutaneous nerve, the saphenous nerve, which supplies skin as far distally as the medial side of the foot. The posterior branch descends behind the adductor brevis muscle and on the anterior surface of the adductor magnus muscle, and supplies the obturator externus and adductor brevis muscles and the part of adductor magnus that attaches to the linea aspera.
The posterior branch descends behind the adductor brevis muscle and on the anterior surface of the adductor magnus muscle, and supplies the obturator externus and adductor brevis muscles and the part of adductor magnus that attaches to the linea aspera. The anterior branch descends on the anterior surface of the adductor brevis muscle and is behind the pectineus and adductor longus muscles—it supplies branches to the adductor longus, gracilis, and adductor brevis muscles, and often contributes to the supply of the pectineus muscle, and cutaneous branches innervate the skin on the medial side of the thigh.
The anterior branch descends on the anterior surface of the adductor brevis muscle and is behind the pectineus and adductor longus muscles—it supplies branches to the adductor longus, gracilis, and adductor brevis muscles, and often contributes to the supply of the pectineus muscle, and cutaneous branches innervate the skin on the medial side of the thigh.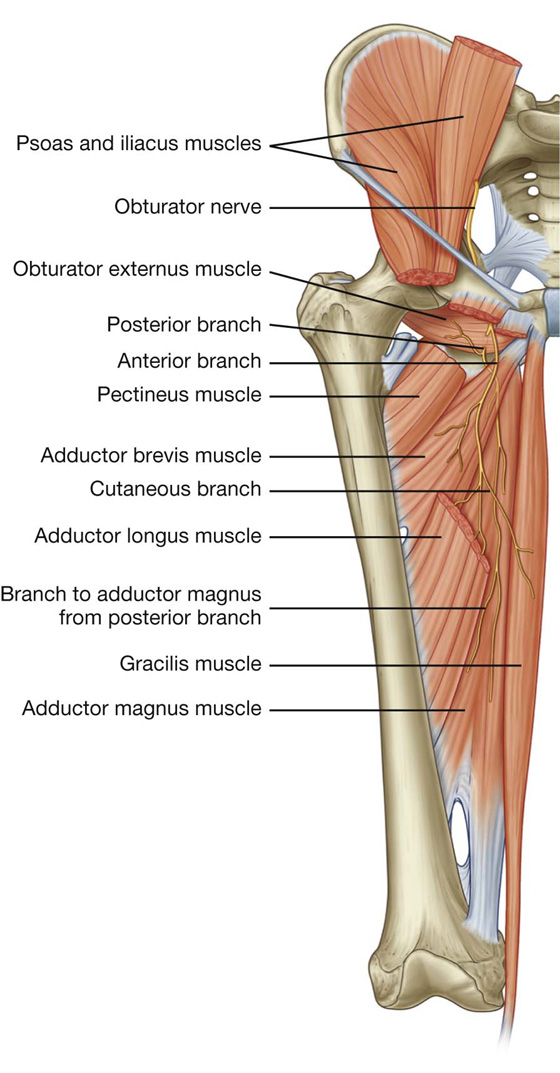
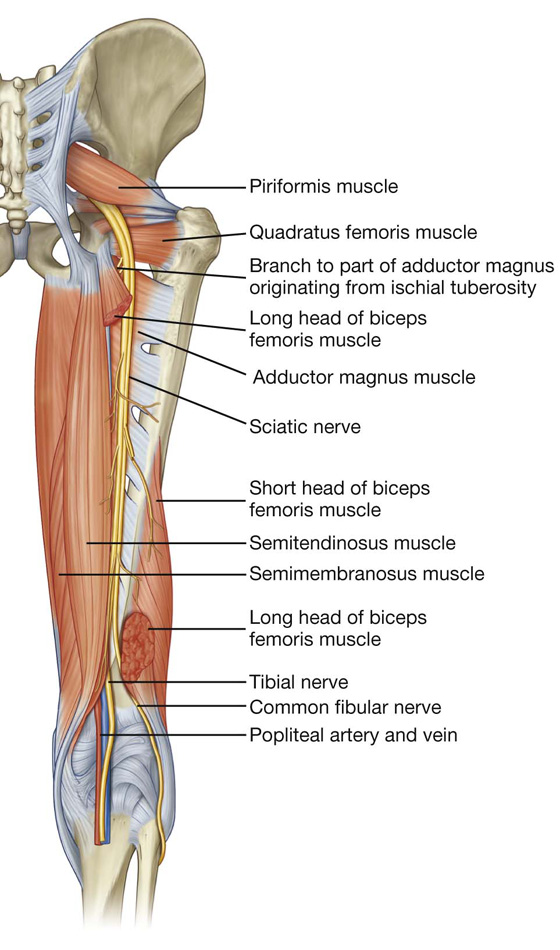
 all intrinsic muscles in the sole of the foot except for the first two dorsal interossei muscles, which are innervated by the deep fibular nerve, and
all intrinsic muscles in the sole of the foot except for the first two dorsal interossei muscles, which are innervated by the deep fibular nerve, and skin on the posterolateral side of the lower half of the leg and lateral side of the ankle, foot, and little toe, and skin on the sole of the foot and toes.
skin on the posterolateral side of the lower half of the leg and lateral side of the ankle, foot, and little toe, and skin on the sole of the foot and toes. the articulation between the patella and the femur, which allows the pull of the quadriceps femoris muscle to be directed anteriorly over the knee to the tibia without tendon wear.
the articulation between the patella and the femur, which allows the pull of the quadriceps femoris muscle to be directed anteriorly over the knee to the tibia without tendon wear.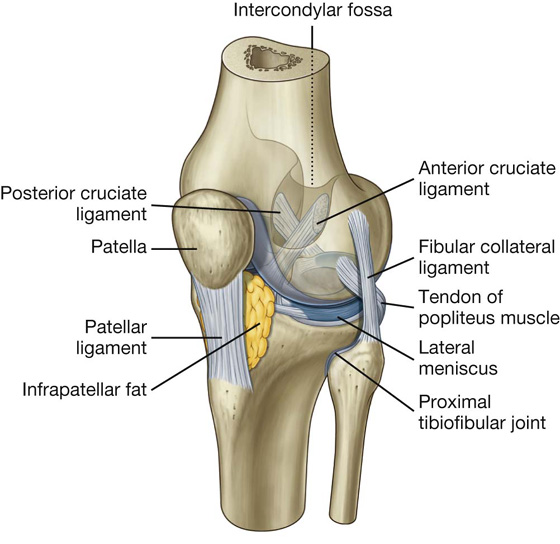
 the two femoral condyles, and
the two femoral condyles, and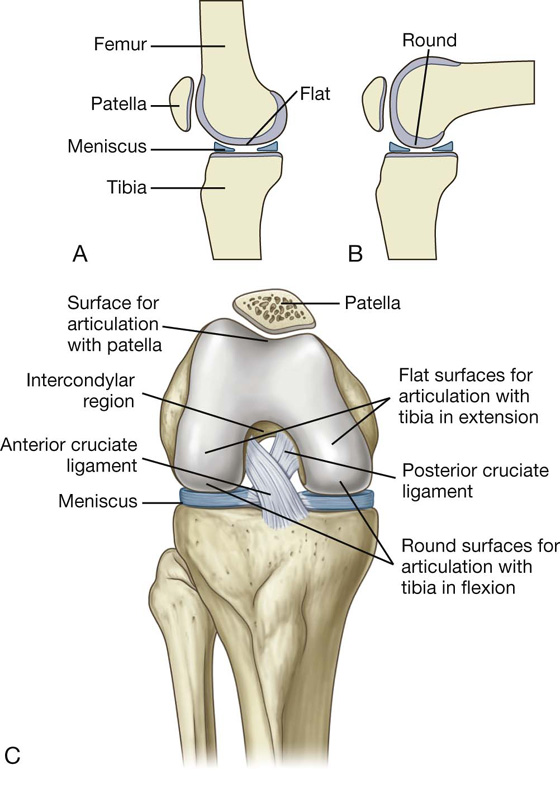
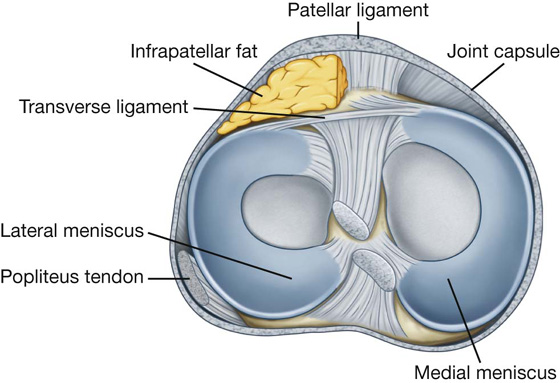
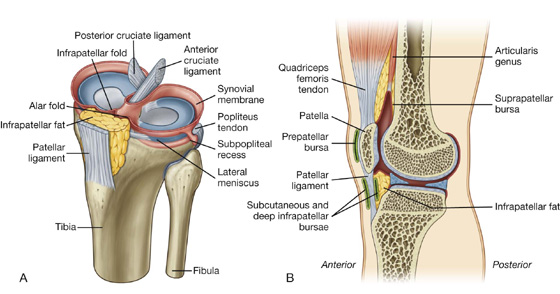
 On the medial side of the knee joint, the fibrous membrane blends with the tibial collateral ligament and is attached on its internal surface to the medial meniscus.
On the medial side of the knee joint, the fibrous membrane blends with the tibial collateral ligament and is attached on its internal surface to the medial meniscus. Laterally, the external surface of the fibrous membrane is separated by a space from the fibular collateral ligament and the internal surface of the fibrous membrane is not attached to the lateral meniscus.
Laterally, the external surface of the fibrous membrane is separated by a space from the fibular collateral ligament and the internal surface of the fibrous membrane is not attached to the lateral meniscus. Anteriorly, the fibrous membrane is attached to the margins of the patella where it is reinforced with tendinous expansions from the vastus lateralis and vastus medialis muscles, which also merge above with the quadriceps femoris tendon and below with the patellar ligament.
Anteriorly, the fibrous membrane is attached to the margins of the patella where it is reinforced with tendinous expansions from the vastus lateralis and vastus medialis muscles, which also merge above with the quadriceps femoris tendon and below with the patellar ligament.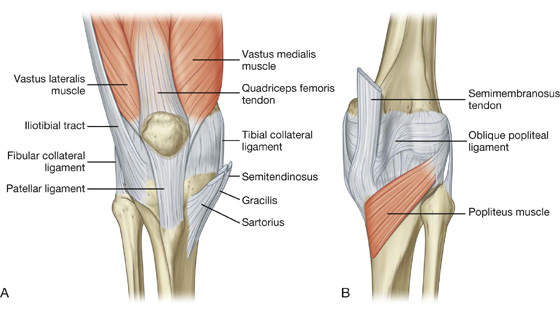
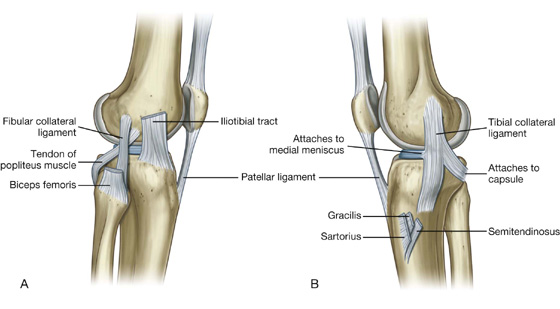
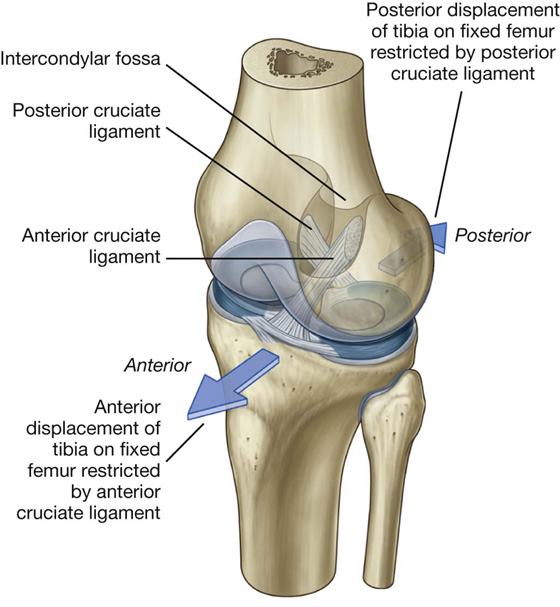
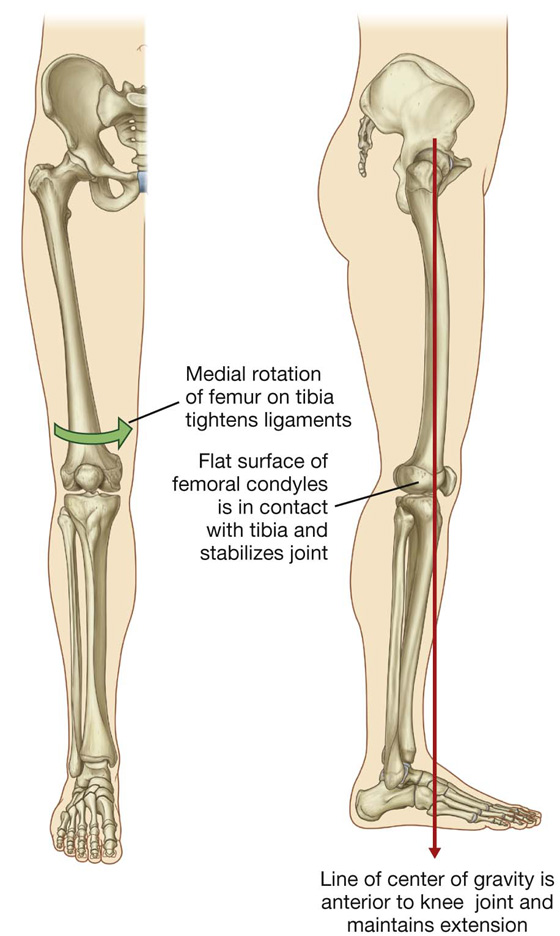
 In flexion, the surfaces are the curved and rounded areas on the posterior aspects of the femoral condyles.
In flexion, the surfaces are the curved and rounded areas on the posterior aspects of the femoral condyles. As the knee is extended, the surfaces move to the broad and flat areas on the inferior aspects of the femoral condyles.
As the knee is extended, the surfaces move to the broad and flat areas on the inferior aspects of the femoral condyles.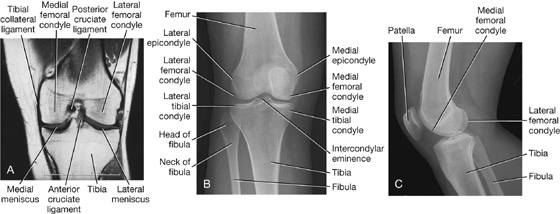
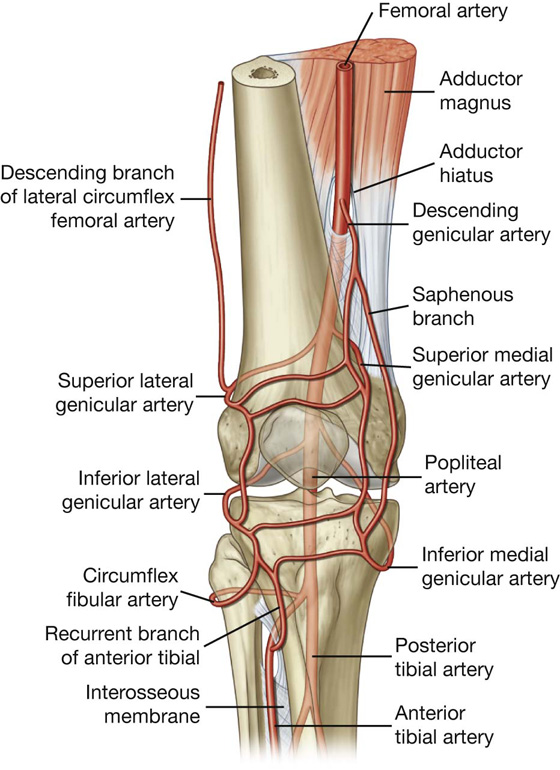
 Posterior drawer test—a positive posterior drawer test occurs when the proximal head of a supine patient’s tibia can be pushed posteriorly on the femur. The knee is flexed to approximately 90° with the foot in the neutral position. If the tibial plateau moves posteriorly, the posterior cruciate ligament is torn.
Posterior drawer test—a positive posterior drawer test occurs when the proximal head of a supine patient’s tibia can be pushed posteriorly on the femur. The knee is flexed to approximately 90° with the foot in the neutral position. If the tibial plateau moves posteriorly, the posterior cruciate ligament is torn.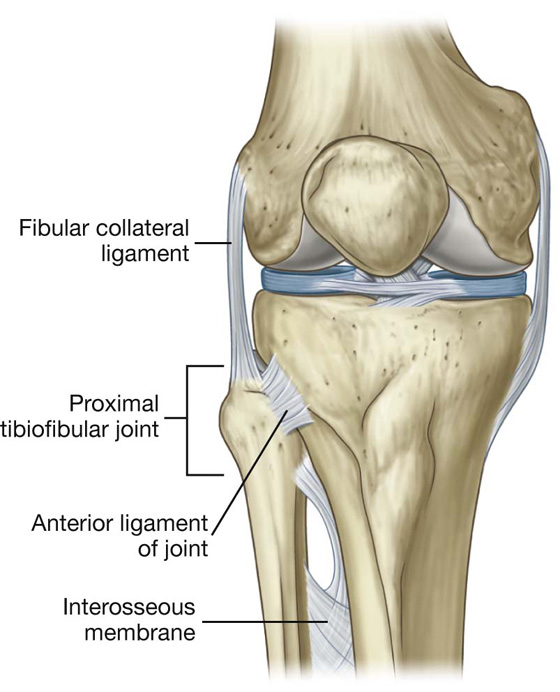
 The margins of the upper part of the diamond are formed medially by the distal ends of the semitendinosus and semimembranosus muscles and laterally by the distal end of the biceps femoris muscle.
The margins of the upper part of the diamond are formed medially by the distal ends of the semitendinosus and semimembranosus muscles and laterally by the distal end of the biceps femoris muscle. The margins of the smaller lower part of the space are formed medially by the medial head of the gastrocnemius muscle and laterally by the plantaris muscle and the lateral head of the gastrocnemius muscle.
The margins of the smaller lower part of the space are formed medially by the medial head of the gastrocnemius muscle and laterally by the plantaris muscle and the lateral head of the gastrocnemius muscle. The floor of the fossa is formed by the capsule of the knee joint and adjacent surfaces of the femur and tibia, and, more inferiorly, by the popliteus muscle.
The floor of the fossa is formed by the capsule of the knee joint and adjacent surfaces of the femur and tibia, and, more inferiorly, by the popliteus muscle. The roof is formed by deep fascia, which is continuous above with the fascia lata of the thigh and below with deep fascia of the leg.
The roof is formed by deep fascia, which is continuous above with the fascia lata of the thigh and below with deep fascia of the leg.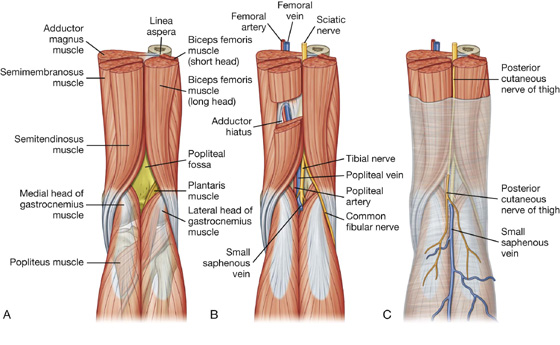
 The tibial nerve descends vertically through the popliteal fossa and exits deep to the margin of plantaris muscle to enter the posterior compartment of leg.
The tibial nerve descends vertically through the popliteal fossa and exits deep to the margin of plantaris muscle to enter the posterior compartment of leg. The common fibular nerve exits by following the biceps femoris tendon over the lower lateral margin of the popliteal fossa, and continues to the lateral side of the leg where it swings around the neck of the fibula and enters the lateral compartment of leg.
The common fibular nerve exits by following the biceps femoris tendon over the lower lateral margin of the popliteal fossa, and continues to the lateral side of the leg where it swings around the neck of the fibula and enters the lateral compartment of leg.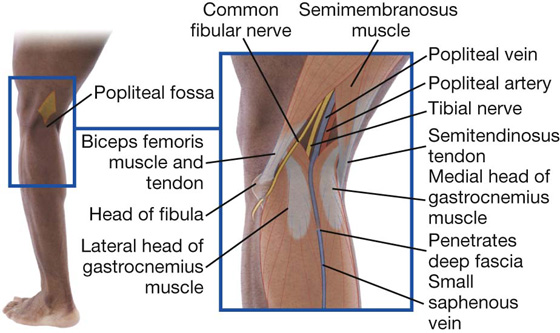
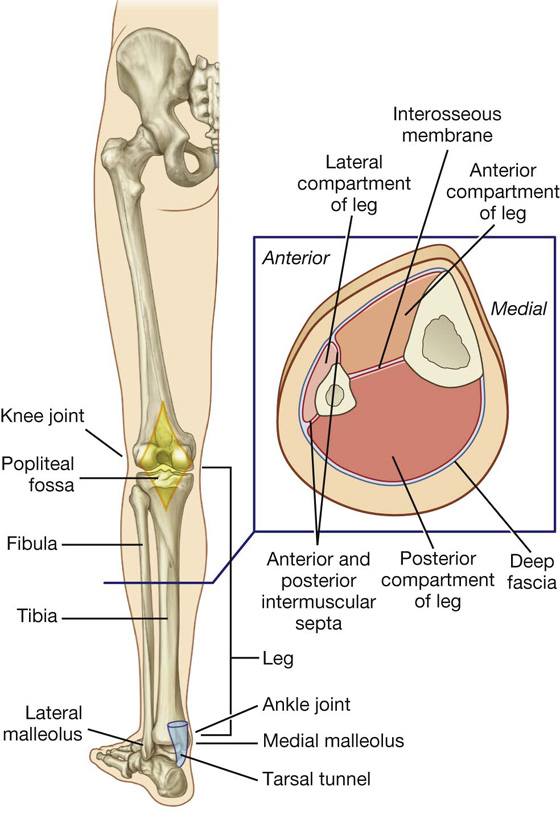
 an interosseous membrane, and
an interosseous membrane, and The interosseous border of the tibia is connected, by the interosseous membrane, along its length to the interosseous border of the fibula.
The interosseous border of the tibia is connected, by the interosseous membrane, along its length to the interosseous border of the fibula.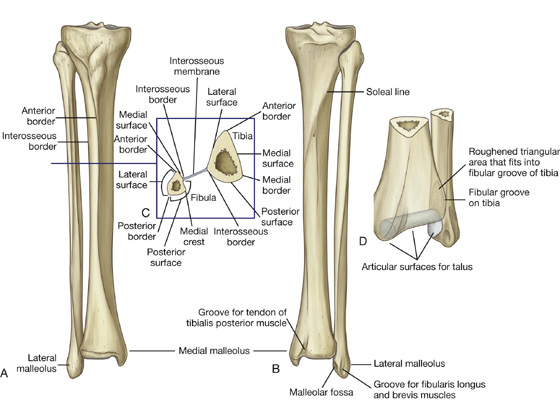
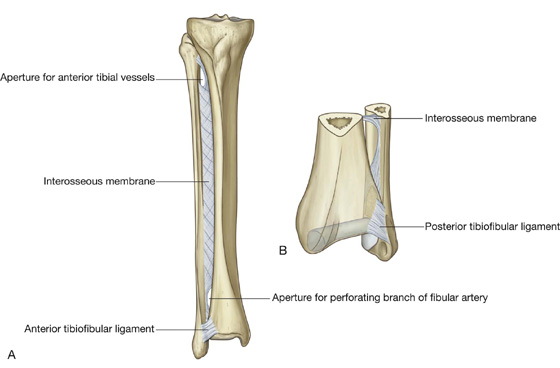
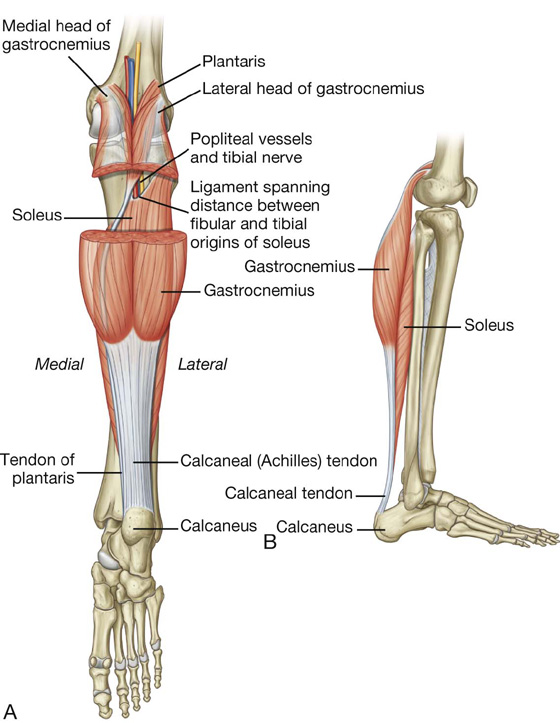
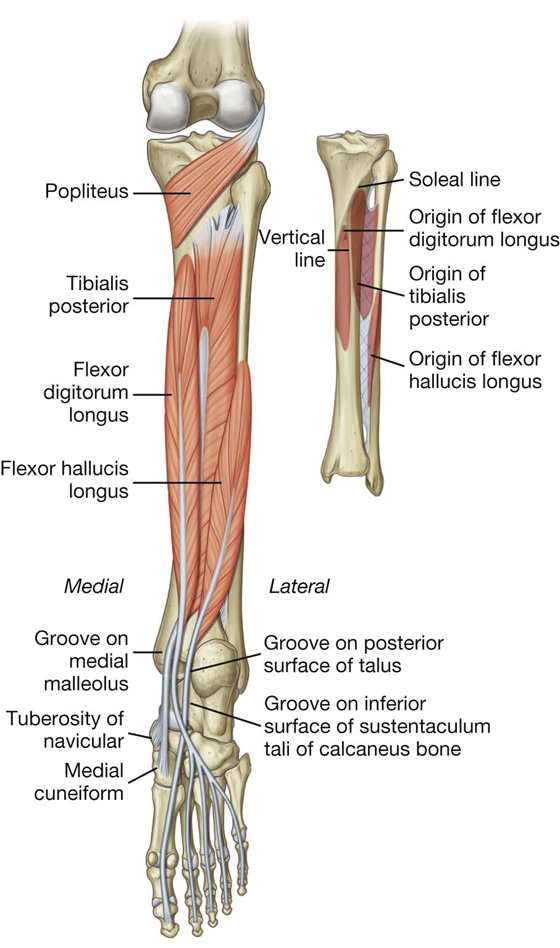
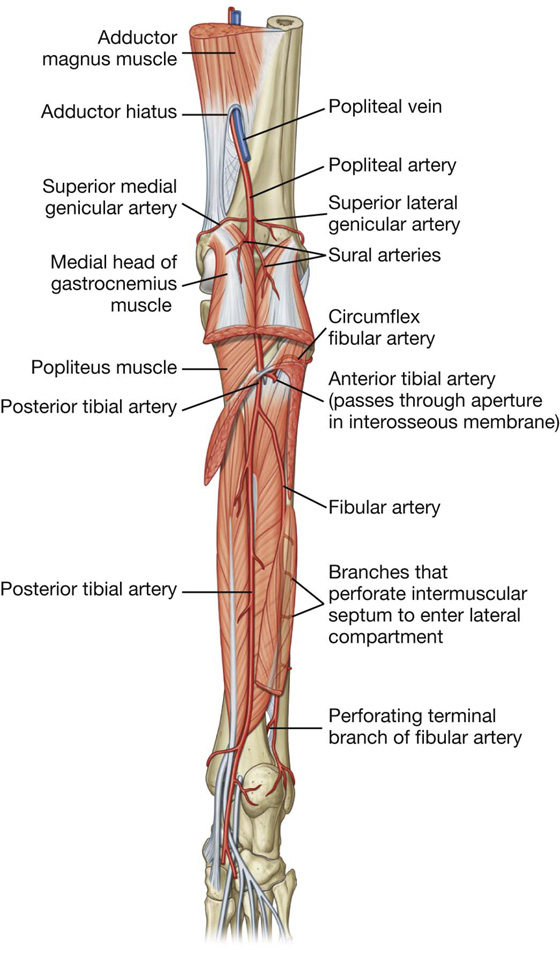
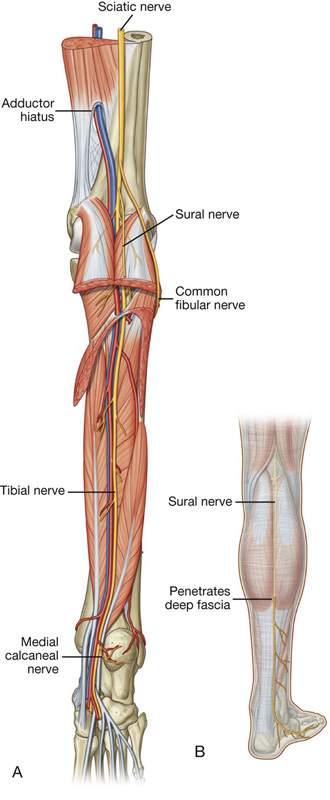
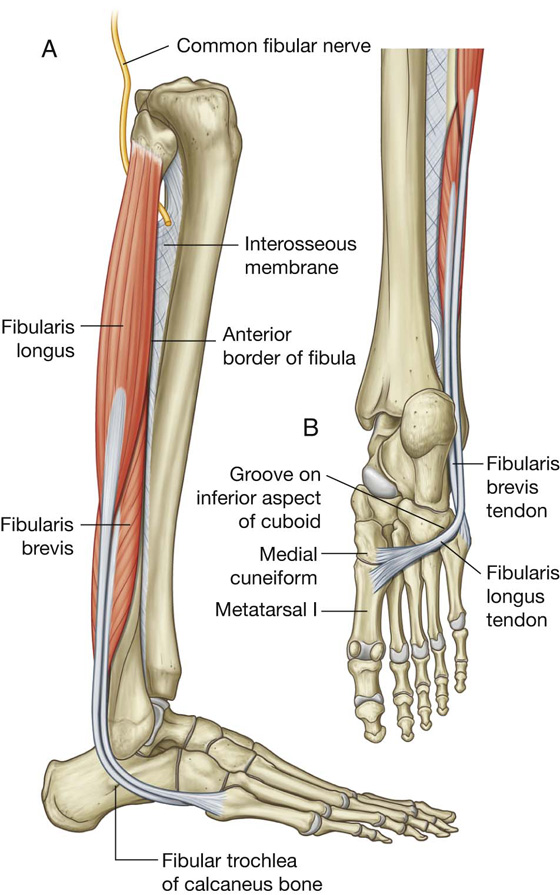
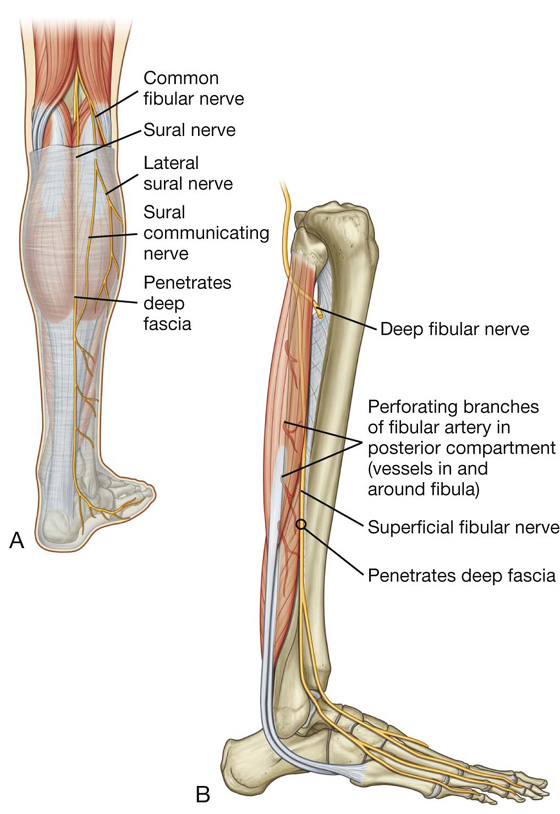
 the deep fibular nerve.
the deep fibular nerve.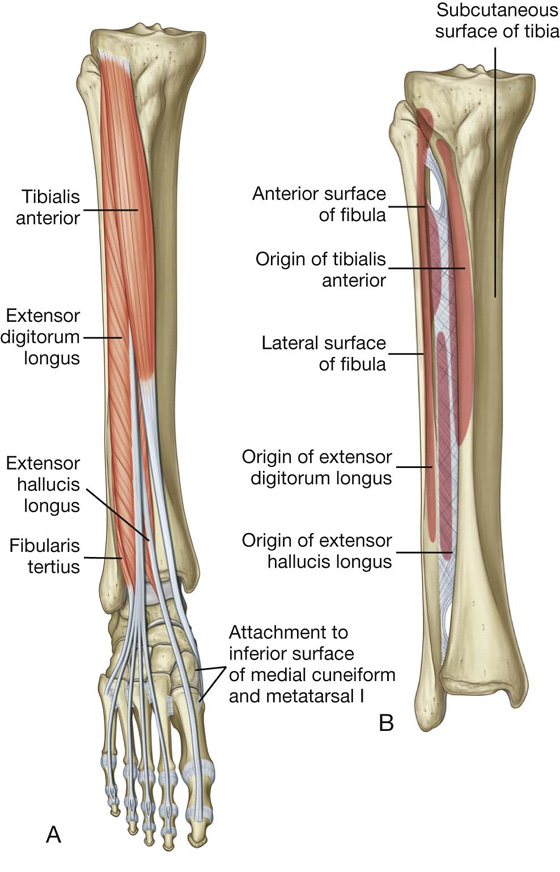
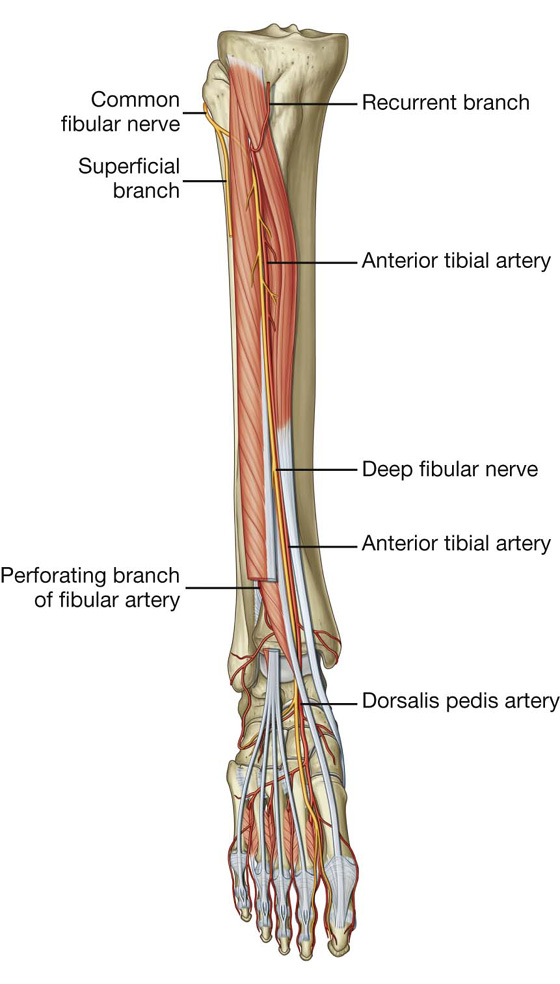
 then continues into the dorsal aspect of the foot where it innervates the extensor digitorum brevis, contributes to the innervation of the first two dorsal interossei muscles, and supplies the skin between the great and second toes.
then continues into the dorsal aspect of the foot where it innervates the extensor digitorum brevis, contributes to the innervation of the first two dorsal interossei muscles, and supplies the skin between the great and second toes.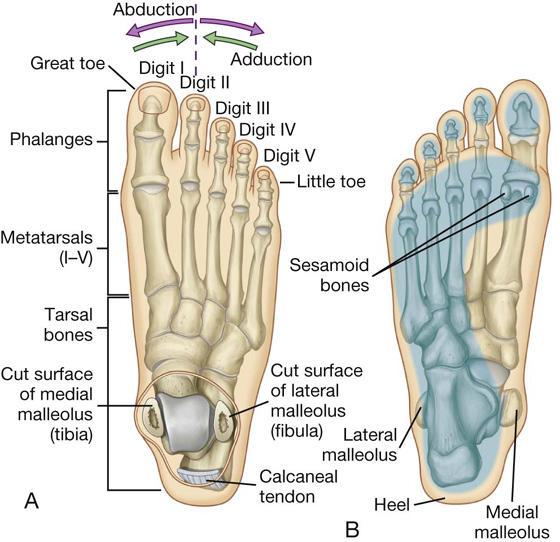
 the phalanges, which are the bones of the toes—each toe has three phalanges, except for the great toe, which has two.
the phalanges, which are the bones of the toes—each toe has three phalanges, except for the great toe, which has two.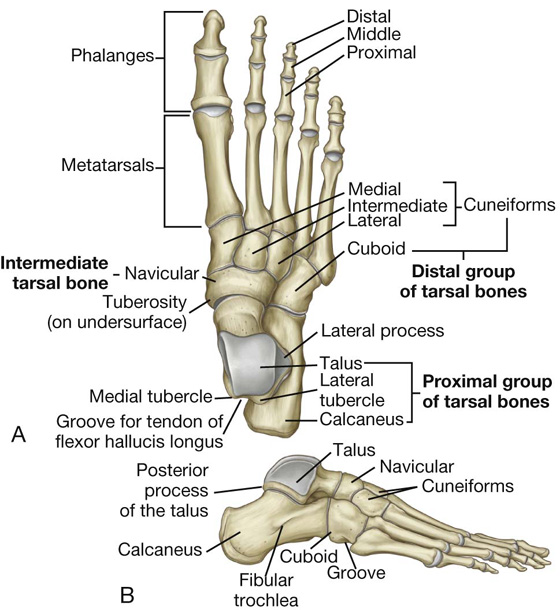
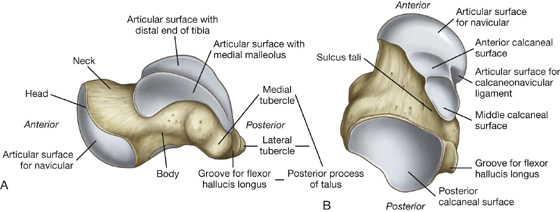
 The other facet, medial to the facets for articulation with the calcaneus, articulates with a ligament—the plantar calcaneonavicular ligament (spring ligament)—which connects the calcaneus to the navicular under the head of the talus.
The other facet, medial to the facets for articulation with the calcaneus, articulates with a ligament—the plantar calcaneonavicular ligament (spring ligament)—which connects the calcaneus to the navicular under the head of the talus. The upper (trochlear) surface of this elevated region articulates with the inferior end of the tibia.
The upper (trochlear) surface of this elevated region articulates with the inferior end of the tibia.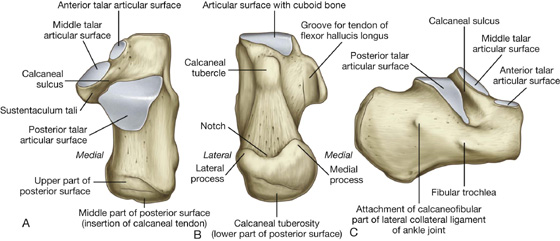
 The lower part curves forward, is covered by subcutaneous tissue, is the weight-bearing region of the heel, and is continuous onto the plantar surface of the bone as the calcaneal tuberosity.
The lower part curves forward, is covered by subcutaneous tissue, is the weight-bearing region of the heel, and is continuous onto the plantar surface of the bone as the calcaneal tuberosity. The anterior talar articular surface is small and articulates with the corresponding anterior facet on the head of the talus.
The anterior talar articular surface is small and articulates with the corresponding anterior facet on the head of the talus. The posterior talar articular surface is large and is approximately near the middle of the superior surface of the calcaneus.
The posterior talar articular surface is large and is approximately near the middle of the superior surface of the calcaneus.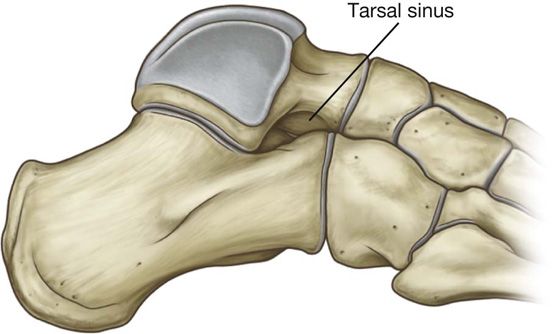
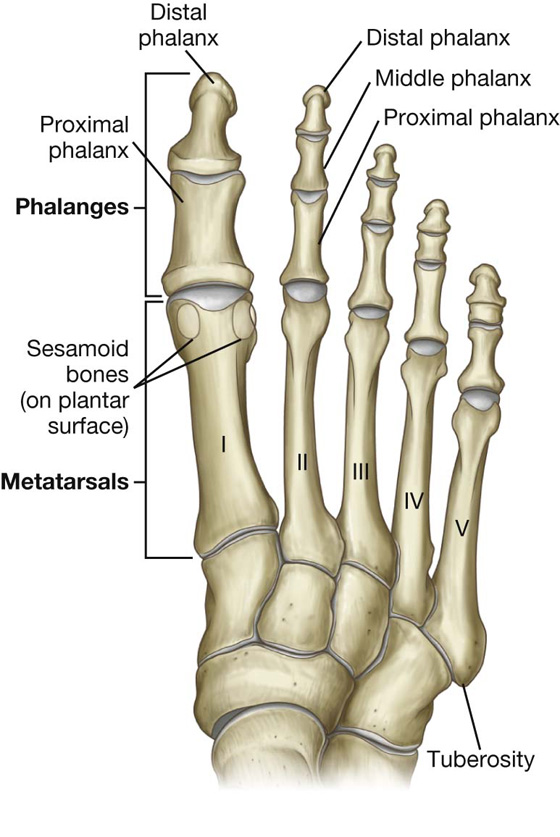
 The head of each distal phalanx is nonarticular and flattened into a crescent-shaped plantar tuberosity under the plantar pad at the end of the digit.
The head of each distal phalanx is nonarticular and flattened into a crescent-shaped plantar tuberosity under the plantar pad at the end of the digit.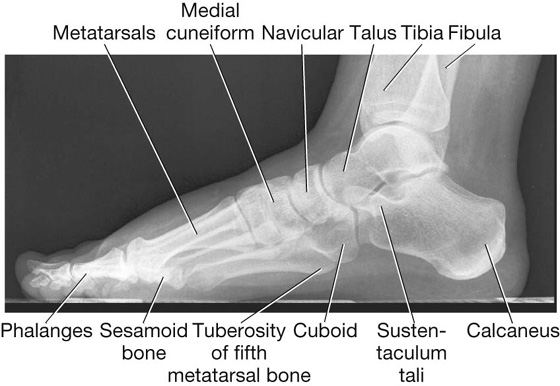
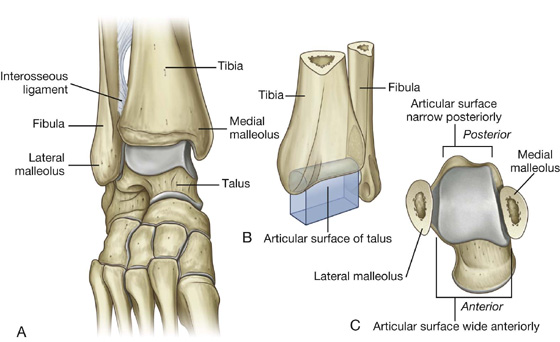
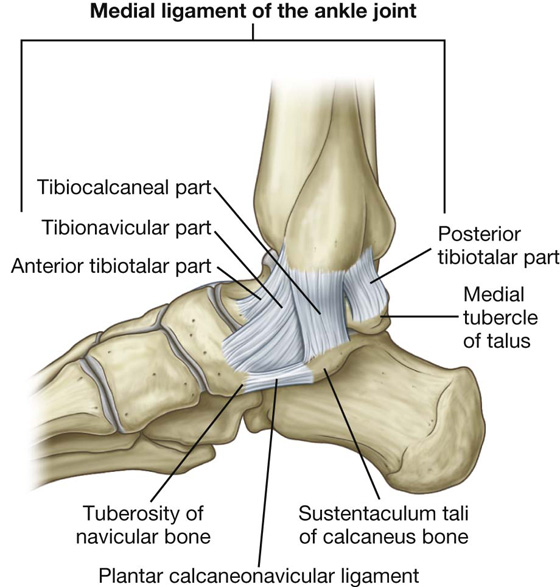
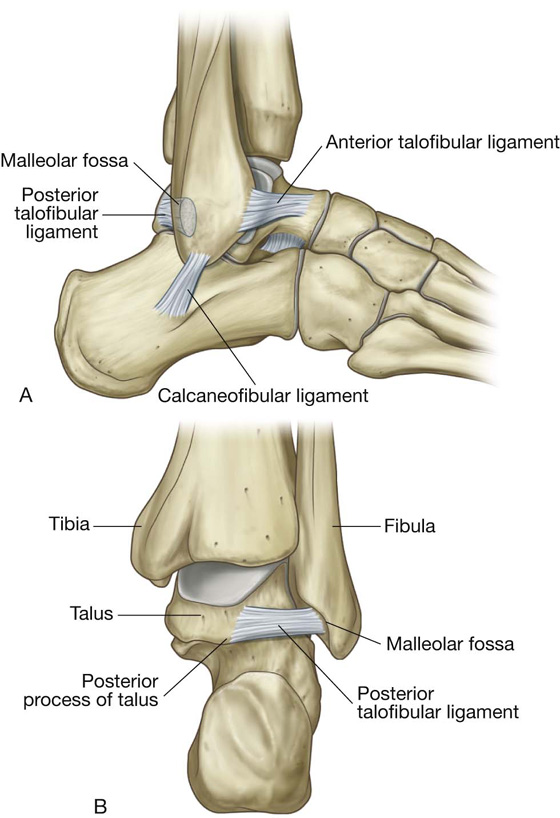
 The part that attaches in front to the tuberosity of the navicular and the associated margin of the plantar calcaneonavicular ligament (spring ligament), which connects the navicular bone to the sustentaculum tali of the calcaneus bone behind, is the tibionavicular part of the medial ligament.
The part that attaches in front to the tuberosity of the navicular and the associated margin of the plantar calcaneonavicular ligament (spring ligament), which connects the navicular bone to the sustentaculum tali of the calcaneus bone behind, is the tibionavicular part of the medial ligament. The tibiocalcaneal part, which is more central, attaches to the sustentaculum tali of the calcaneus bone.
The tibiocalcaneal part, which is more central, attaches to the sustentaculum tali of the calcaneus bone. The fourth part (the anterior tibiotalar part) is deep to the tibionavicular and tibiocalcaneal parts of the medial ligament and attaches to the medial surface of the talus.
The fourth part (the anterior tibiotalar part) is deep to the tibionavicular and tibiocalcaneal parts of the medial ligament and attaches to the medial surface of the talus. The anterior talofibular ligament is a short ligament, and attaches the anterior margin of the lateral malleolus to the adjacent region of the talus.
The anterior talofibular ligament is a short ligament, and attaches the anterior margin of the lateral malleolus to the adjacent region of the talus. The posterior talofibular ligament runs horizontally backward and medially from the malleolar fossa on the medial side of the lateral malleolus to the posterior process of the talus.
The posterior talofibular ligament runs horizontally backward and medially from the malleolar fossa on the medial side of the lateral malleolus to the posterior process of the talus. The calcaneofibular ligament is attached above to the malleolar fossa on the posteromedial side of the lateral malleolus and passes posteroinferiorly to attach below to a tubercle on the lateral surface of the calcaneus.
The calcaneofibular ligament is attached above to the malleolar fossa on the posteromedial side of the lateral malleolus and passes posteroinferiorly to attach below to a tubercle on the lateral surface of the calcaneus.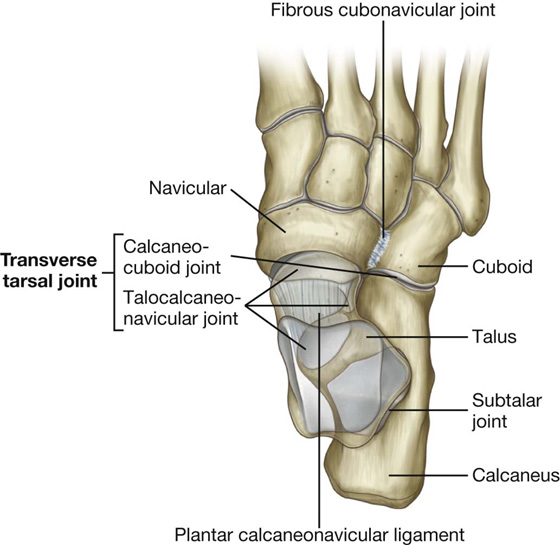
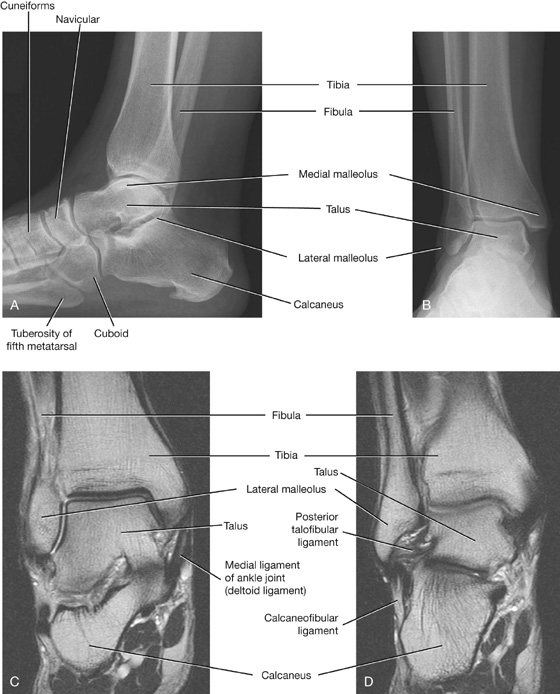
 Pronation is rotating the front of the foot laterally relative to the back of the foot, and supination is the reverse movement.
Pronation is rotating the front of the foot laterally relative to the back of the foot, and supination is the reverse movement.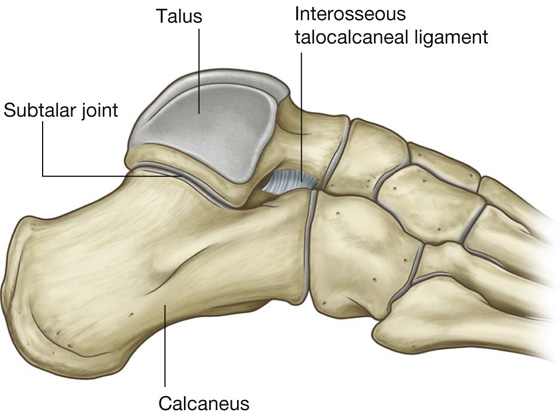
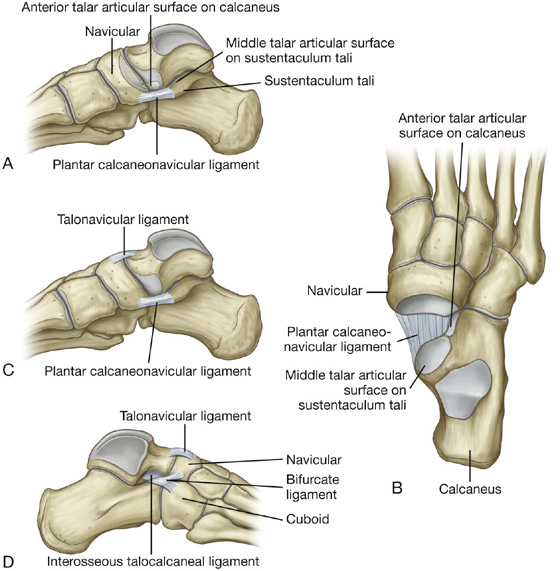
 superiorly by the talonavicular ligament, which passes between the neck of the talus and adjacent regions of the navicular, and
superiorly by the talonavicular ligament, which passes between the neck of the talus and adjacent regions of the navicular, and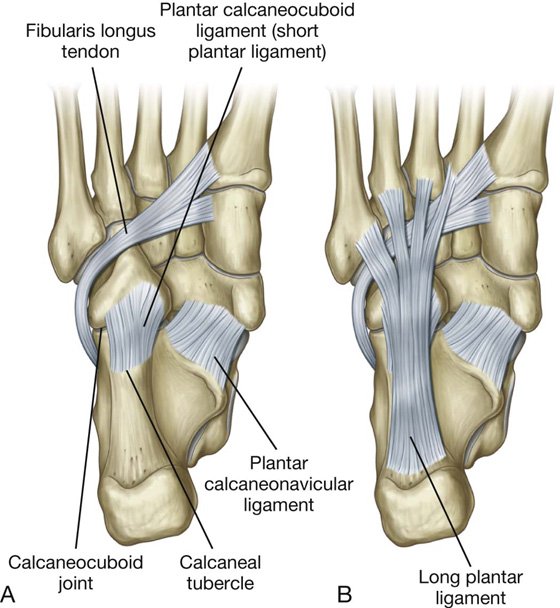
 Posteriorly, it attaches to the inferior surface of the calcaneus between the tuberosity and the calcaneal tubercle.
Posteriorly, it attaches to the inferior surface of the calcaneus between the tuberosity and the calcaneal tubercle. Anteriorly, it attaches to a broad ridge and a tubercle on the inferior surface of the cuboid bone behind the groove for the fibularis longus tendon.
Anteriorly, it attaches to a broad ridge and a tubercle on the inferior surface of the cuboid bone behind the groove for the fibularis longus tendon.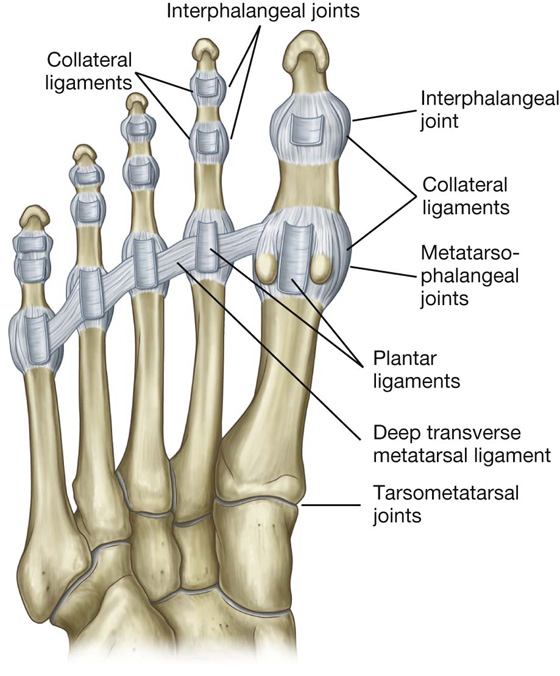
 a depression formed by the medial malleolus of the tibia, the medial and posterior surfaces of the talus, the medial surface of the calcaneus, and the inferior surface of the sustentaculum tali of the calcaneus; and
a depression formed by the medial malleolus of the tibia, the medial and posterior surfaces of the talus, the medial surface of the calcaneus, and the inferior surface of the sustentaculum tali of the calcaneus; and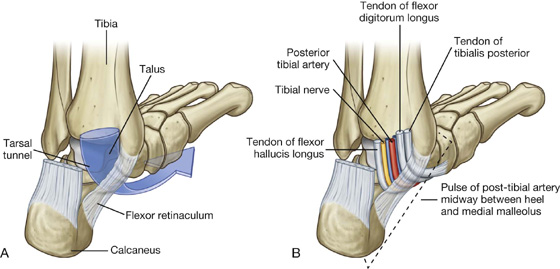
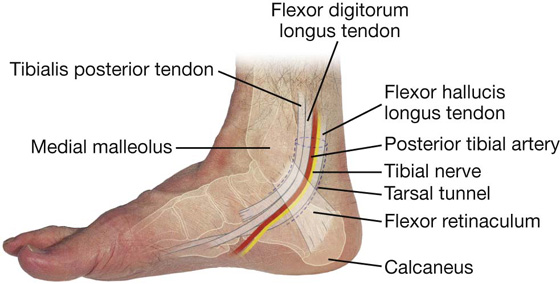
 A superior extensor retinaculum is a thickening of deep fascia in the distal leg just superior to the ankle joint and attached to the anterior borders of the fibula and tibia.
A superior extensor retinaculum is a thickening of deep fascia in the distal leg just superior to the ankle joint and attached to the anterior borders of the fibula and tibia. An inferior retinaculum is Y-shaped, attached by its base to the lateral side of the upper surface of the calcaneus, and crosses medially over the foot to attach by one of its arms to the medial malleolus, whereas the other arm wraps medially around the foot and attaches to the medial side of the plantar aponeurosis.
An inferior retinaculum is Y-shaped, attached by its base to the lateral side of the upper surface of the calcaneus, and crosses medially over the foot to attach by one of its arms to the medial malleolus, whereas the other arm wraps medially around the foot and attaches to the medial side of the plantar aponeurosis.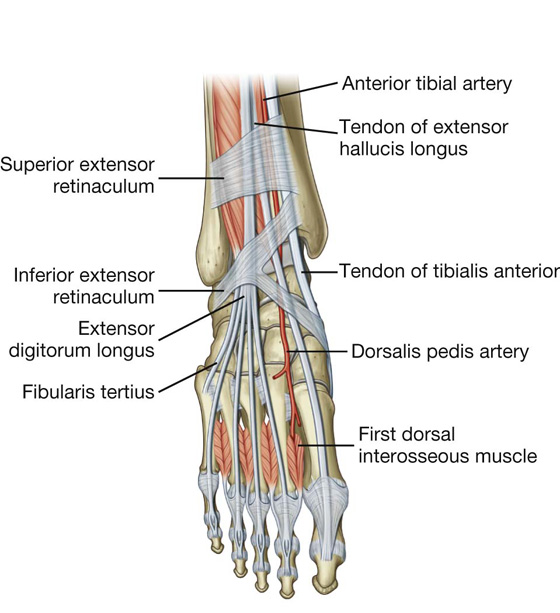
 An inferior fibular retinaculum attaches to the lateral surface of the calcaneus around the fibular trochlea and blends above with the fibers of the inferior extensor retinaculum.
An inferior fibular retinaculum attaches to the lateral surface of the calcaneus around the fibular trochlea and blends above with the fibers of the inferior extensor retinaculum.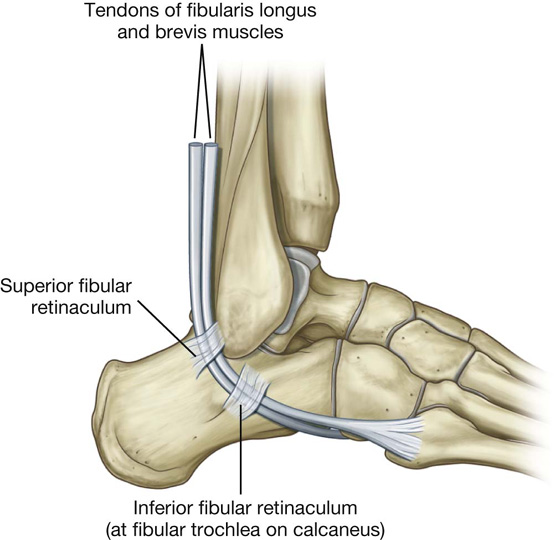
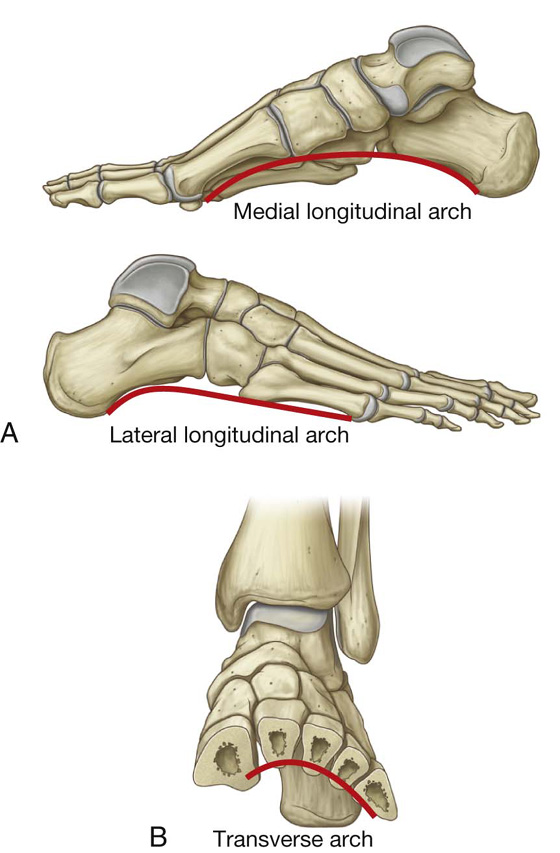
 Ligaments that support the arches include the plantar calcaneonavicular (spring ligament), plantar calcaneocuboid (short plantar ligament), long plantar ligament, and the plantar aponeurosis.
Ligaments that support the arches include the plantar calcaneonavicular (spring ligament), plantar calcaneocuboid (short plantar ligament), long plantar ligament, and the plantar aponeurosis. Muscles that provide dynamic support for the arches during walking include the tibialis anterior and posterior, and the fibularis longus.
Muscles that provide dynamic support for the arches during walking include the tibialis anterior and posterior, and the fibularis longus.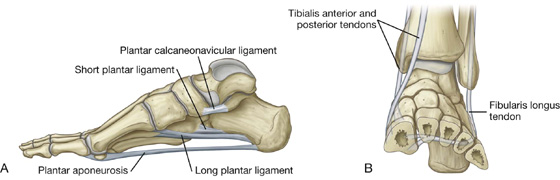
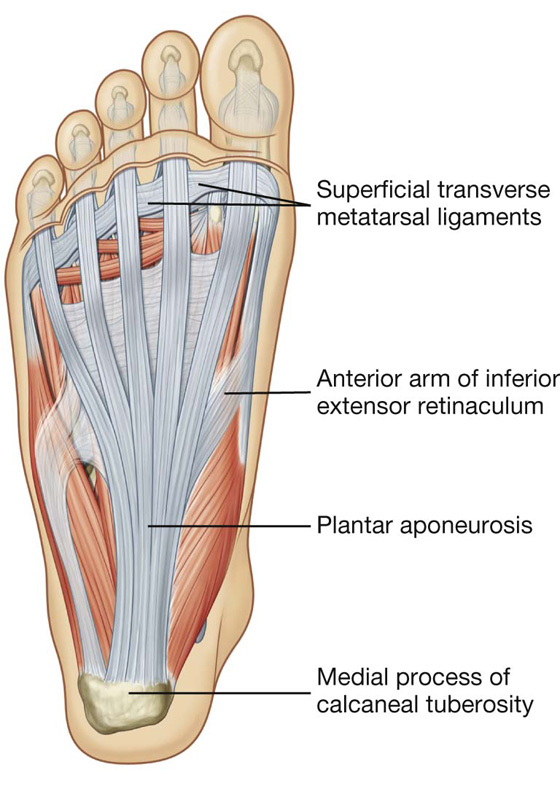
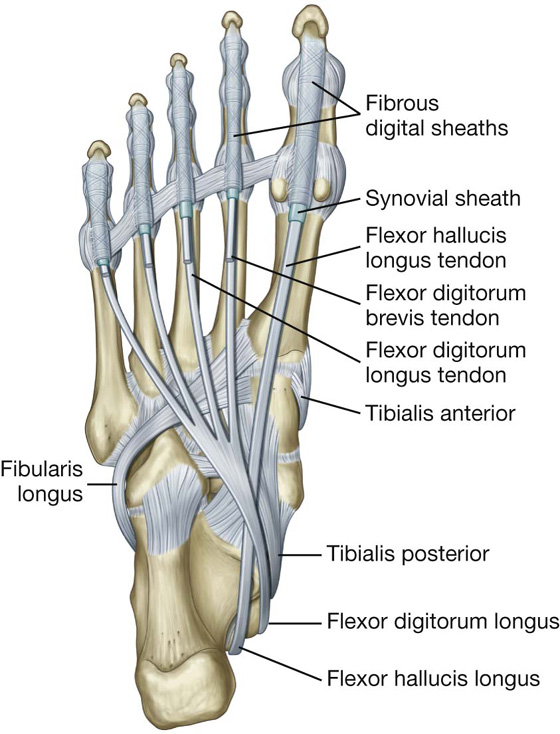
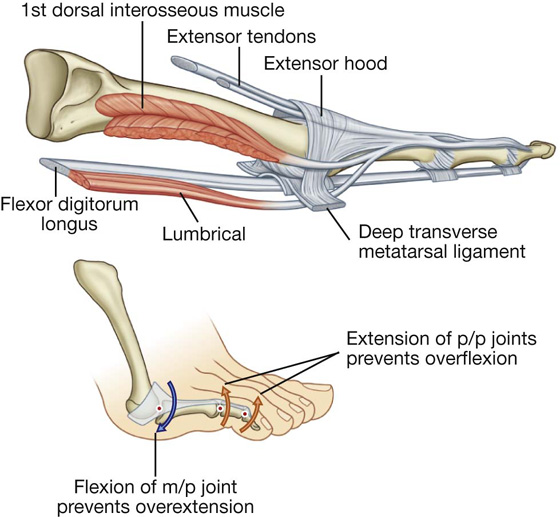
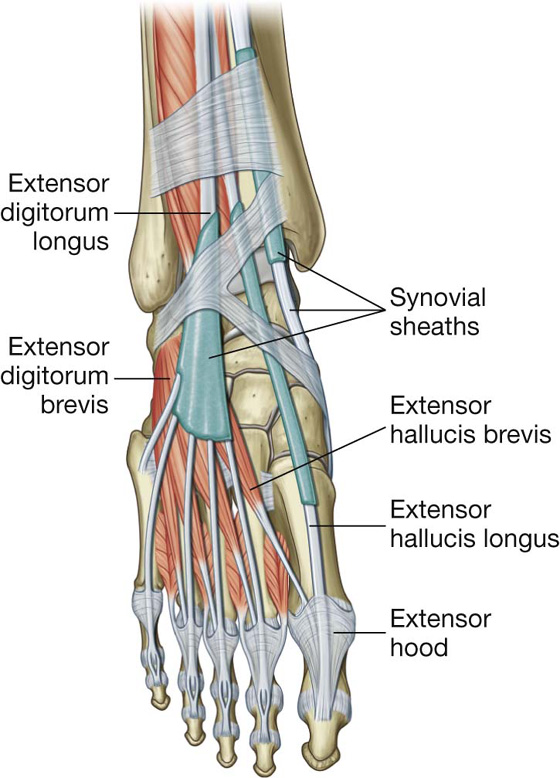
 all other intrinsic muscles are on the plantar side of the foot, where they are organized into four layers.
all other intrinsic muscles are on the plantar side of the foot, where they are organized into four layers.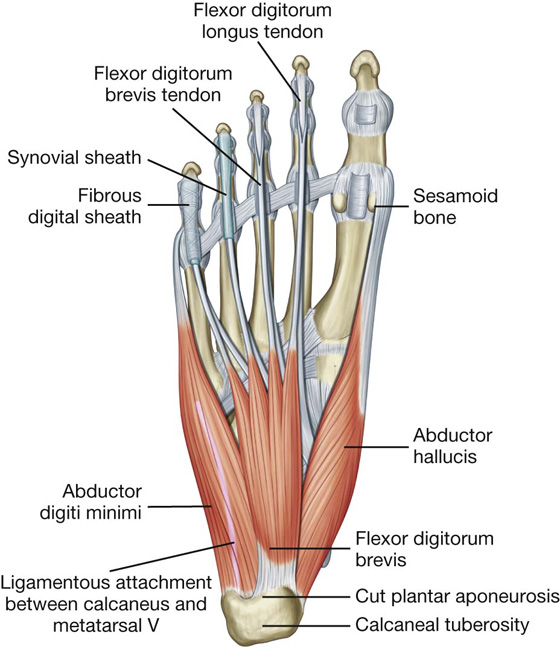
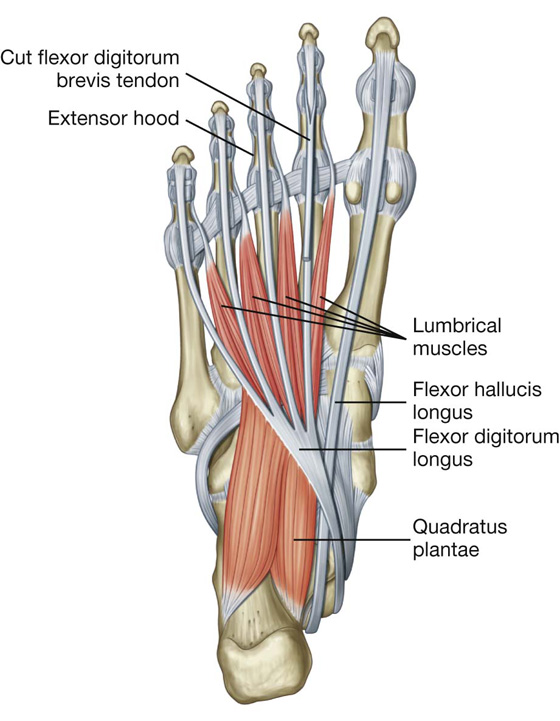
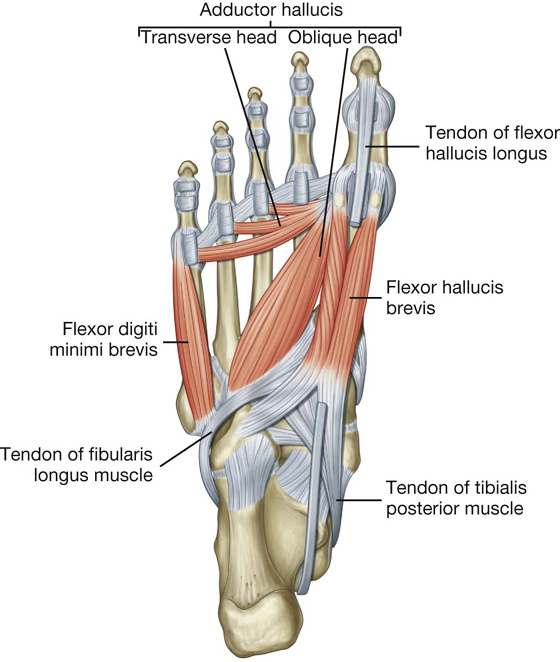
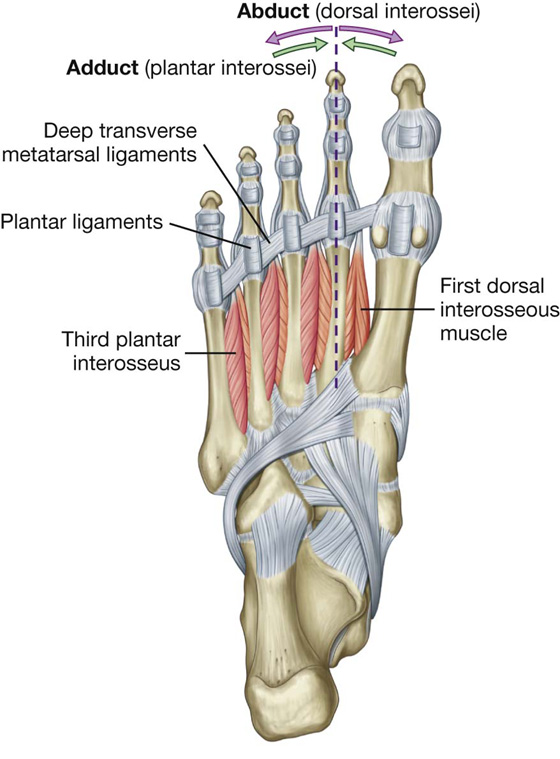
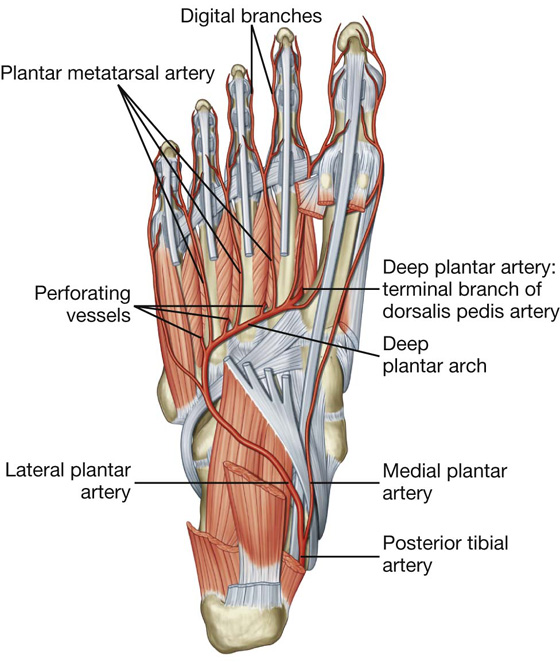
 three perforating arteries, which pass between the bases of metatarsals II to V to anastomose with vessels on the dorsal aspect of the foot.
three perforating arteries, which pass between the bases of metatarsals II to V to anastomose with vessels on the dorsal aspect of the foot.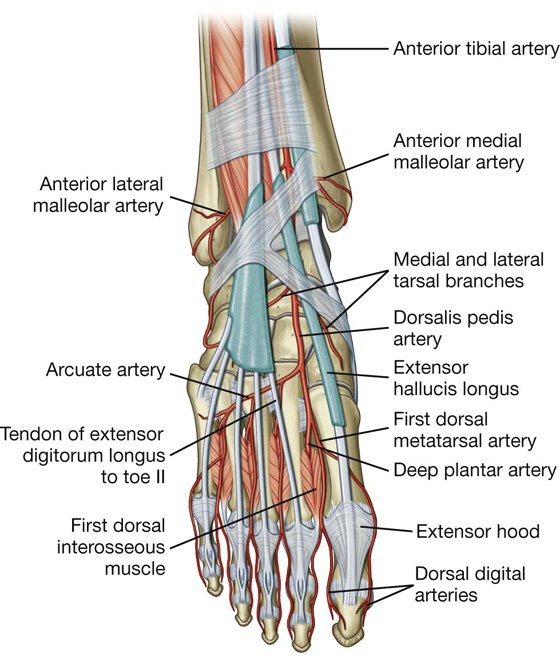
 The tarsal arteries pass medially and laterally over the tarsal bones, supplying adjacent structures and anastomosing with a network of vessels formed around the ankle.
The tarsal arteries pass medially and laterally over the tarsal bones, supplying adjacent structures and anastomosing with a network of vessels formed around the ankle. The arcuate artery passes laterally over the dorsal aspect of the metatarsals near their bases and gives rise to three dorsal metatarsal arteries, which supply dorsal digital arteries to adjacent sides of digits II to V, and to a dorsal digital artery that supplies the lateral side of digit V.
The arcuate artery passes laterally over the dorsal aspect of the metatarsals near their bases and gives rise to three dorsal metatarsal arteries, which supply dorsal digital arteries to adjacent sides of digits II to V, and to a dorsal digital artery that supplies the lateral side of digit V. The first dorsal metatarsal artery (the last branch of the dorsalis pedis artery before the dorsalis pedis artery continues as the deep plantar artery into the sole of the foot) supplies dorsal digital branches to adjacent sides of the great and second toes.
The first dorsal metatarsal artery (the last branch of the dorsalis pedis artery before the dorsalis pedis artery continues as the deep plantar artery into the sole of the foot) supplies dorsal digital branches to adjacent sides of the great and second toes.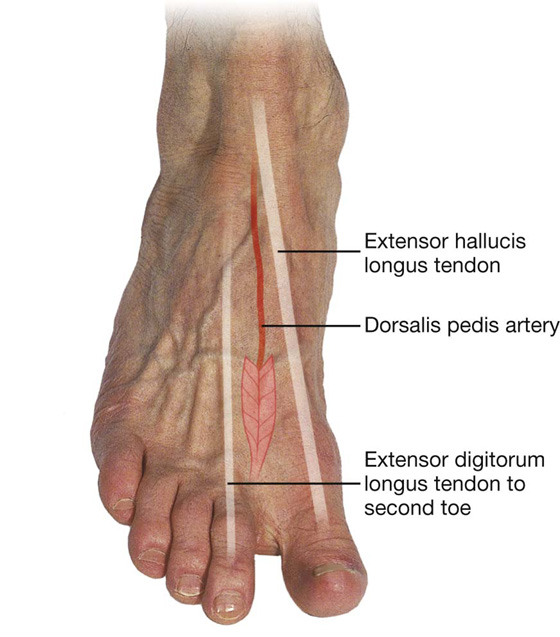
 The great saphenous vein originates from the medial side of the arch and passes anterior to the medial malleolus and onto the medial side of the leg.
The great saphenous vein originates from the medial side of the arch and passes anterior to the medial malleolus and onto the medial side of the leg. The small saphenous vein originates from the lateral side of the arch and passes posterior to the lateral malleolus and onto the back of the leg.
The small saphenous vein originates from the lateral side of the arch and passes posterior to the lateral malleolus and onto the back of the leg.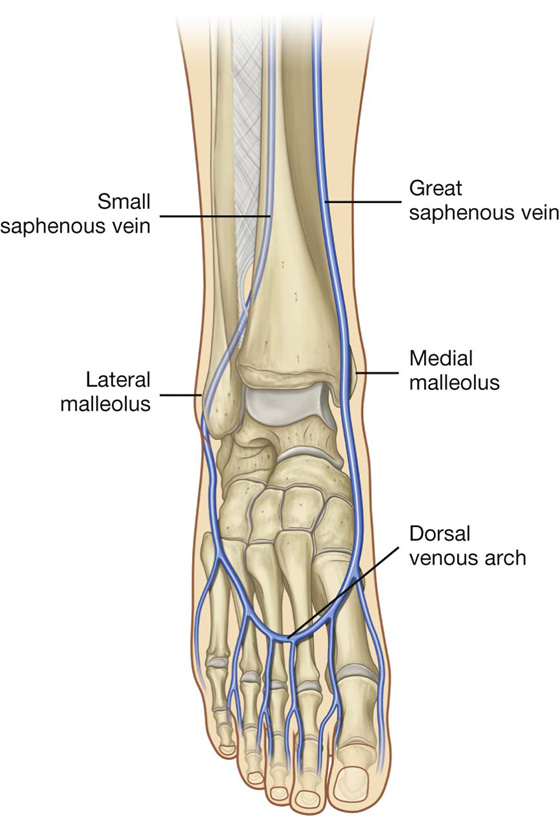
 The tibial nerve innervates all intrinsic muscles of the foot except for the extensor digitorum brevis, which is innervated by the deep fibular nerve.
The tibial nerve innervates all intrinsic muscles of the foot except for the extensor digitorum brevis, which is innervated by the deep fibular nerve. The deep fibular nerve often also contributes to the innervation of the first and second dorsal interossei.
The deep fibular nerve often also contributes to the innervation of the first and second dorsal interossei.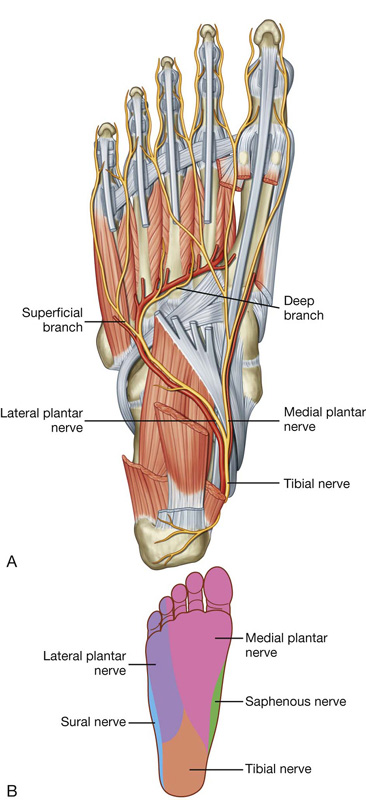
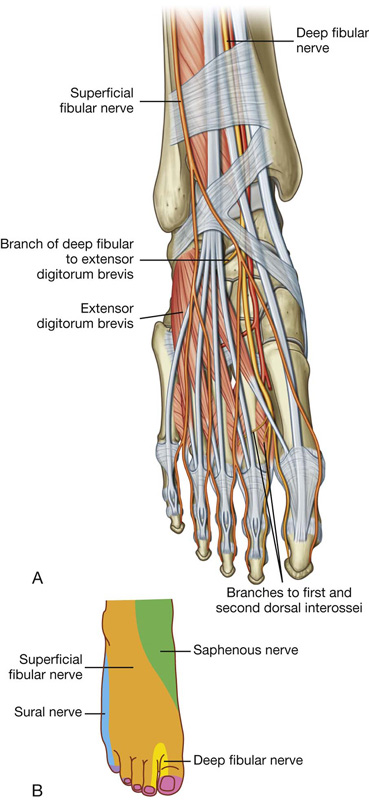
 over the inguinal ligament—L1
over the inguinal ligament—L1 lateral side of the thigh—L2
lateral side of the thigh—L2 medial side of digit II—L5
medial side of digit II—L5 little toe (digit V)—S1
little toe (digit V)—S1 back of the thigh—S2
back of the thigh—S2 skin over the gluteal fold—S3
skin over the gluteal fold—S3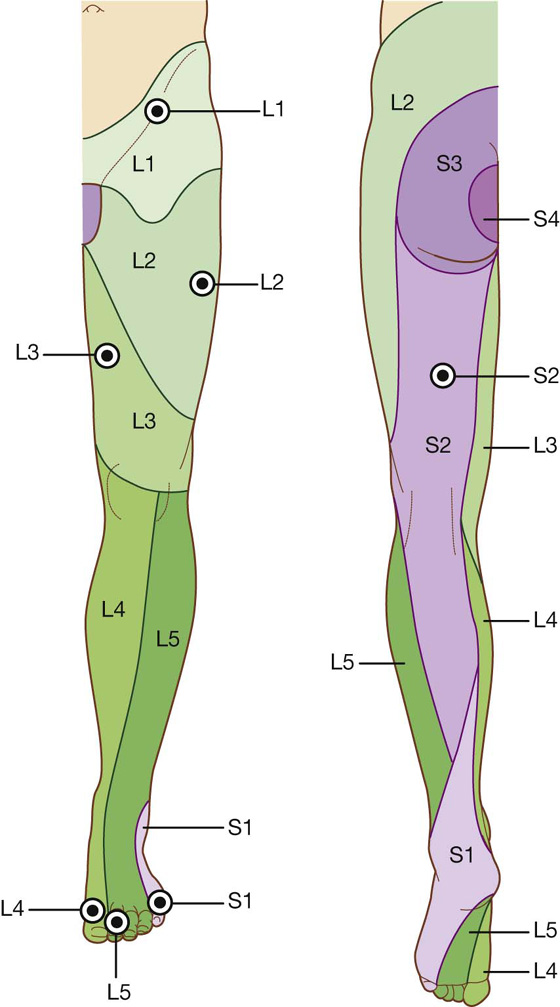
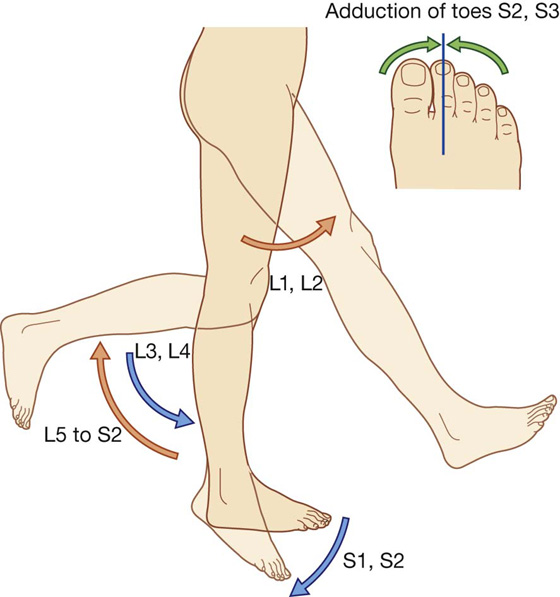
 The femoral nerve innervates skin on the anterior thigh, medial side of the leg, and medial side of the ankle.
The femoral nerve innervates skin on the anterior thigh, medial side of the leg, and medial side of the ankle.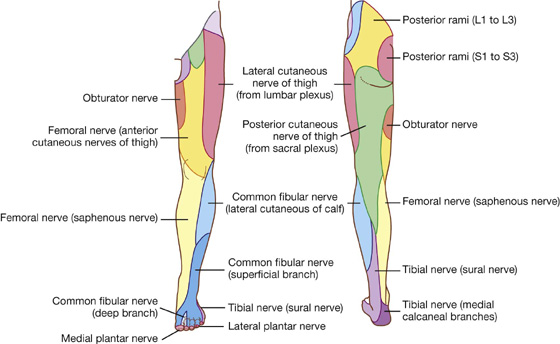
 A tendon tap on the calcaneal tendon posterior to the ankle (tendon of gastrocnemius and soleus) tests S1 and S2.
A tendon tap on the calcaneal tendon posterior to the ankle (tendon of gastrocnemius and soleus) tests S1 and S2.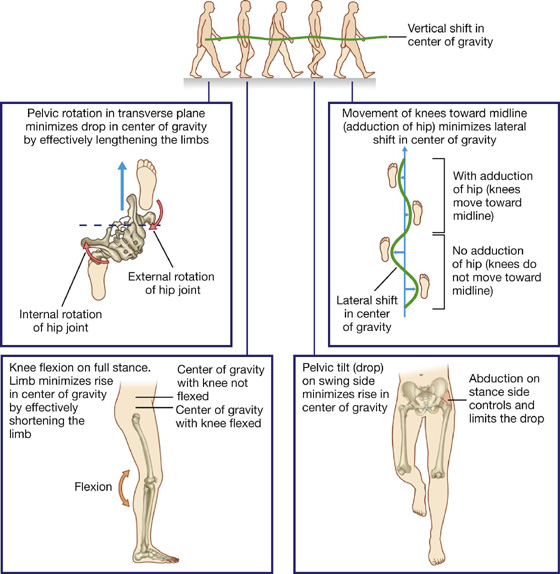
 femoral pulse in the femoral triangle—femoral artery inferior to the inguinal ligament and midway between the anterior superior iliac spine and the pubic symphysis
femoral pulse in the femoral triangle—femoral artery inferior to the inguinal ligament and midway between the anterior superior iliac spine and the pubic symphysis popliteal pulse in the popliteal fossa—popliteal artery deep in the popliteal fossa medial to the midline
popliteal pulse in the popliteal fossa—popliteal artery deep in the popliteal fossa medial to the midline posterior tibial pulse in the tarsal tunnel—posterior tibial artery posteroinferior to the medial malleolus in the groove between the medial malleolus and the heel (calcaneal tuberosity)
posterior tibial pulse in the tarsal tunnel—posterior tibial artery posteroinferior to the medial malleolus in the groove between the medial malleolus and the heel (calcaneal tuberosity) dorsalis pedis pulse on the dorsal aspect of the foot—dorsalis pedis artery as it passes distally over the tarsal bones between the tendon of the extensor hallucis longus and the tendon of the extensor digitorum longus to the second toe
dorsalis pedis pulse on the dorsal aspect of the foot—dorsalis pedis artery as it passes distally over the tarsal bones between the tendon of the extensor hallucis longus and the tendon of the extensor digitorum longus to the second toe