Lower Leg, Ankle, and Foot
At least 80% of the general population has foot problems, but these problems can often be corrected by proper assessment, treatment, and, above all, care of the feet. Lesions of the ankle and foot can alter the mechanics of gait resulting in movement impairments and, as a result, cause stress on other lower limb joints, which in turn may lead to pathology in these joints.1
The foot and ankle combine flexibility with stability because of the many bones, their shapes, and their attachments. The lower leg, ankle, and foot have two principal functions: propulsion and support. For propulsion, they act like a flexible lever; for support, they act like a rigid structure that holds up the entire body.
Although the joints of the lower leg, ankle, and foot are discussed separately, they act as functional groups, not as isolated joints. As the terminal part of the lower kinetic chain, the lower leg, ankle, and foot have the ability to distribute and dissipate the different forces (e.g., compressive, shearing, rotary, tensile) acting on the body through contact with the ground.2 This is especially evident during gait. In the foot, the movement occurring at each individual joint is minimal. However, when combined, there normally is sufficient range of motion (ROM) in all of the joints to allow functional mobility as well as functional stability. For ease of understanding, the joints of the foot are divided into three sections: hindfoot (rearfoot), midfoot, and forefoot.
Applied Anatomy
Hindfoot (Rearfoot)
Tibiofibular Joint.
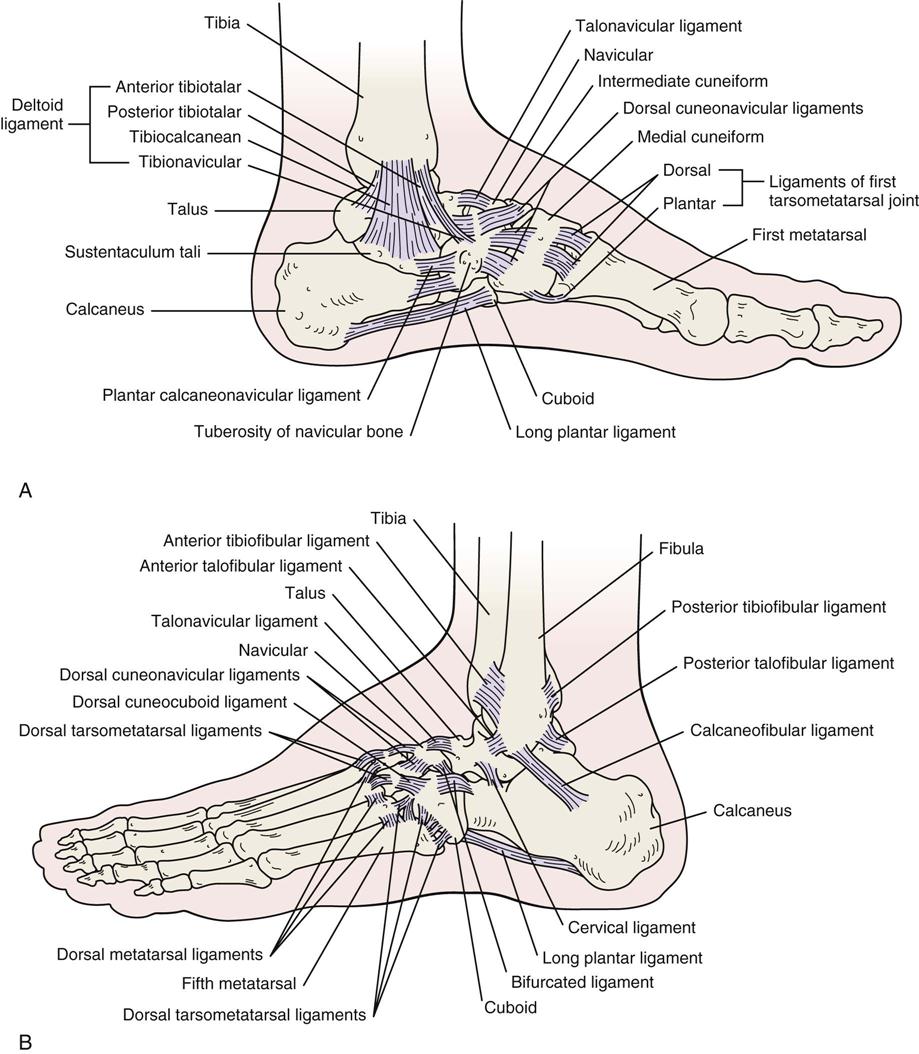
The inferior (distal) tibiofibular joint is a fibrous or syndesmosis type of joint. It is supported by the anterior tibiofibular, posterior tibiofibular, and inferior transverse ligaments as well as the interosseous ligaments (Figure 13-1). The movements at this joint are minimal but allow a small amount of spread (1 to 2 mm) at the ankle joint during dorsiflexion. This same action allows the fibula to move up and down during dorsiflexion and plantar flexion. Dorsiflexion at the ankle joint causes the fibula to move superiorly, putting stress on both the inferior tibiofibular joint at the ankle and the superior tibiofibular joint at the knee. The fibula carries more of the axial load when it is dorsiflexed. On average, the fibula carries about 17% of the axial loading.3 The joint is supplied by the deep peroneal and tibial nerves.
Talocrural (Ankle) Joint.
The talocrural joint is a uniaxial, modified hinge, synovial joint located between the talus, the medial malleolus of the tibia, and the lateral malleolus of the fibula. The talus is shaped so that in dorsiflexion it is wedged between the malleoli, allowing little or no inversion or eversion at the ankle joint. The talus is approximately 2.4 mm (0.1 inch) wider anteriorly than posteriorly. The medial malleolus is shorter, extending halfway down the talus, whereas the lateral malleolus extends almost to the level of the subtalar joint. The joint is supplied by branches of the tibial and deep peroneal nerves.
The talocrural joint is designed for stability, especially in dorsiflexion. In plantar flexion, it is much more mobile. This joint is responsible for the anterior-posterior (dorsiflexion-plantar flexion) movement that occurs in the ankle-foot complex. Its close packed position is maximum dorsiflexion, and its capsular pattern is more a limitation of plantar flexion than of dorsiflexion. This joint is most stable in the dorsiflexed position. The resting position is 10° of plantar flexion, midway between maximum inversion and maximum eversion. The talocrural joint has one degree of freedom, and the movements possible at this joint are dorsiflexion and plantar flexion.
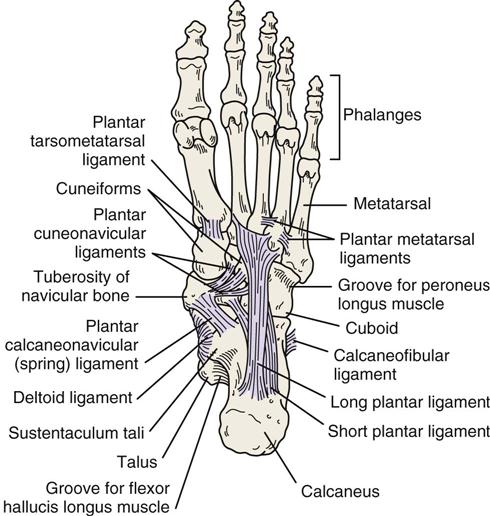
On the medial side of the joint, the major ligament is the deltoid or medial collateral ligament, which consists of four separate ligaments: the tibionavicular, tibiocalcanean, and posterior tibiotalar ligaments superficially, all of which resist talar abduction, and the anterior tibiotalar ligament, which lies deep to the other three ligaments and resists lateral translation and lateral rotation of the talus. On the lateral aspect, the talocrural joint is supported by the anterior talofibular ligament, which provides stability against excessive inversion of the talus; the posterior talofibular ligament, which resists ankle dorsiflexion, adduction (“tilt”), medial rotation, and medial translation of the talus; and the calcaneofibular ligament, which provides stability against maximum inversion at the ankle and subtalar joints. The anterior talofibular ligament is the ligament most commonly injured by a lateral ankle sprain, followed by the calcaneofibular ligament.
Subtalar (Talocalcanean) Joint.
The subtalar joint is a synovial joint having three degrees of freedom and a close packed position of supination. Supporting the subtalar joint are the lateral talocalcanean and medial talocalcanean ligaments. In addition, the interosseous talocalcanean and cervical ligaments limit eversion.
The movements possible at the subtalar joint are gliding and rotation. With injury to the area (e.g., sprain, fracture), this joint and the talocrural joint often become hypomobile, partially because the talus has no muscles attaching to it. Medial rotation of the leg causes a valgus (outward) movement of the calcaneus, whereas lateral rotation of the leg produces a varus (inward) movement of the calcaneus. The axis of the joint is at an angle of 40° to 45° inclined vertically and 15° to 18° to the sagittal plane.
Midfoot (Midtarsal Joints)
In isolation, the midtarsal joints allow only a minimal amount of movement. Taken together, however, they allow significant movement to enable the foot to adapt to many positions without putting undue stress on the joints. Chopart joint refers collectively to the midtarsal joints between the talus-calcaneus and the navicular-cuboid.
Talocalcaneonavicular Joint.
The talocalcaneonavicular joint is a ball-and-socket synovial joint with 3° of freedom. Its close packed position is supination, and the dorsal talonavicular ligament, bifurcated ligament, and plantar calcaneonavicular (spring) ligament support the joint (see Figure 13-1; Figure 13-2). Movements possible at this joint are gliding and rotation.
Cuneonavicular Joint.
The cuneonavicular joint is a plane synovial joint with a close packed position of supination. The movements possible at this joint are slight gliding and rotation.
Cuboideonavicular Joint.
The cuboideonavicular joint is fibrous, its close packed position being supination. The movements possible at this joint are slight gliding and rotation.
Intercuneiform Joints.
The intercuneiform joints are plane synovial joints with a close packed position of supination. The movements possible at these joints are slight gliding and rotation.
Cuneocuboid Joint.
The cuneocuboid joint is a plane synovial joint with a close packed position of supination. The movements of slight gliding and rotation are possible at this joint.
Calcaneocuboid Joint.
The calcaneocuboid joint is saddle shaped with a close packed position of supination. Supporting this joint are the bifurcated ligament, the calcaneocuboid ligament, and the long plantar ligaments. The movement possible at this joint is gliding with conjunct rotation.
Forefoot
Tarsometatarsal Joints.
The tarsometatarsal joints are plane synovial joints with a close packed position of supination. The movement possible at these joints is gliding. Taken together, these joints are referred to as Lisfranc joint.4
Intermetatarsal Joints.
The four intermetatarsal joints are plane synovial joints with a close packed position of supination. The movement possible at these joints is gliding.
Metatarsophalangeal Joints.
The five metatarsophalangeal joints are condyloid synovial joints with 2° of freedom. Their close packed position is full extension. Their capsular pattern is variable for the lateral four joints and more limitation of extension than flexion for the hallux (big toe); their resting position is 10° of extension. The movements possible at these joints are flexion, extension, abduction, and adduction.
Interphalangeal Joints.
The interphalangeal joints are synovial hinge joints with 1° of freedom. The close packed position is full extension, and the capsular pattern is more limitation of flexion than of extension. The resting position of the distal and proximal interphalangeal joints is slight flexion. The movements possible at these joints are flexion and extension.
Patient History
It is important to take a detailed and complete history when assessing the lower leg, ankle, and foot. In addition to the questions listed under the “Patient History” section in Chapter 1 the examiner should obtain the following information from the patient:
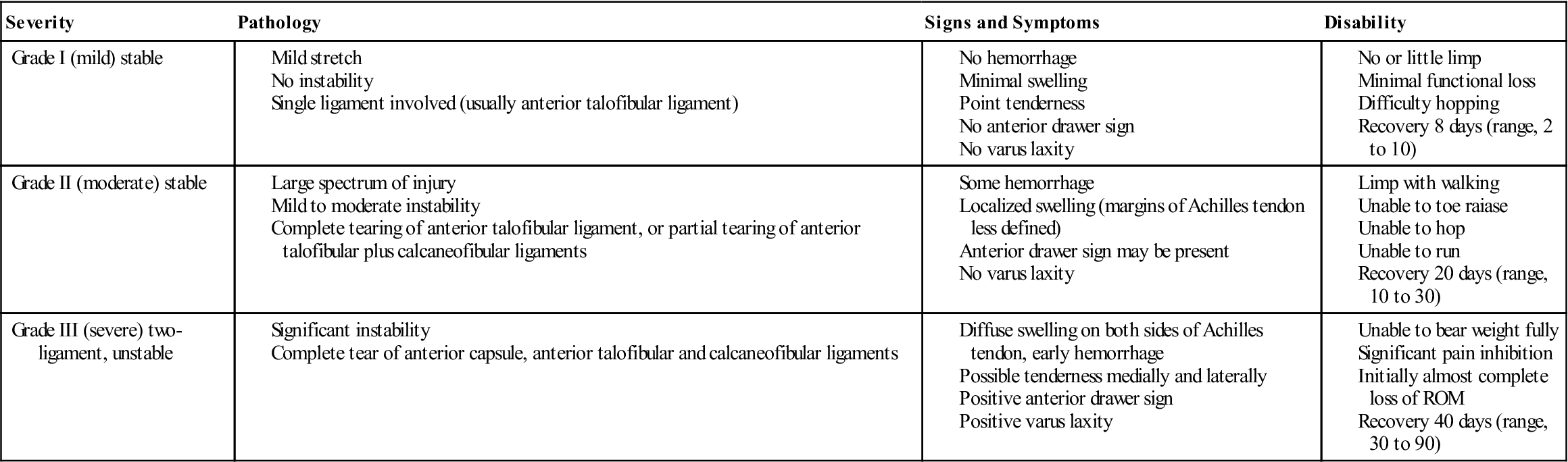
2. What was the mechanism of injury? What was the position of the foot at the time of the injury? Ankle sprains occur most often when the foot is plantar flexed, inverted, and adducted, with injury to the anterior talofibular ligament, anterolateral capsule, and possibly the distal tibiofibular ligament.5,6 This same mechanism can lead to peroneal tendon injury, a malleolar or talar dome fracture, and sinus tarsi syndrome.7,8 Figure 13-3 outlines some of the common mechanisms of injury to the ankle. Table 13-1 outlines the West Point Sprain Grading System that can be used to determine the severity of ankle sprains.9 With injury to the lateral ligaments, the structures (articular surfaces) may be damaged on the medial side owing to compression leading to medial as well as lateral pain.10 In fact, if the lateral ligaments are completely torn and the capsule disrupted, medial pain may predominate. Anterolateral pain without a history of trauma may be the result of anterior impingement especially after injury to the anterior talofibular ligament. Lin et al.11 developed a clinical prediction rule for ankle impingement (see the following box) that would preclude the need for magnetic resonance imaging (MRI). The impingement may be due to thickening of the joint capsule and/or bone spurs adjacent to the anterior talocrural joint.12 Achilles tendinosis or paratenonitis often arises as the result of overuse, increased activity, or change in a high-stress training program. Osteochondral lesions most commonly occur with trauma and may accompany ankle sprains and fractures with symptoms being exacerbated by prolonged weight bearing or high impact activities.13 A dorsiflexion injury, accompanied by a snapping and pain on the lateral aspect that rapidly diminishes, may indicate a tear of the peroneal retinaculum.14 Taunton et al.15 list some causes of overuse injuries in the lower limb.
4. Was the patient able to continue the activity after the injury? If so, the injury is probably not too severe, provided there is no loss of stability. Inability to bear weight, severe pain, and rapid swelling indicate a severe injury.14 Walking is compatible with a second-degree sprain; pain with running usually indicates a first-degree injury.16
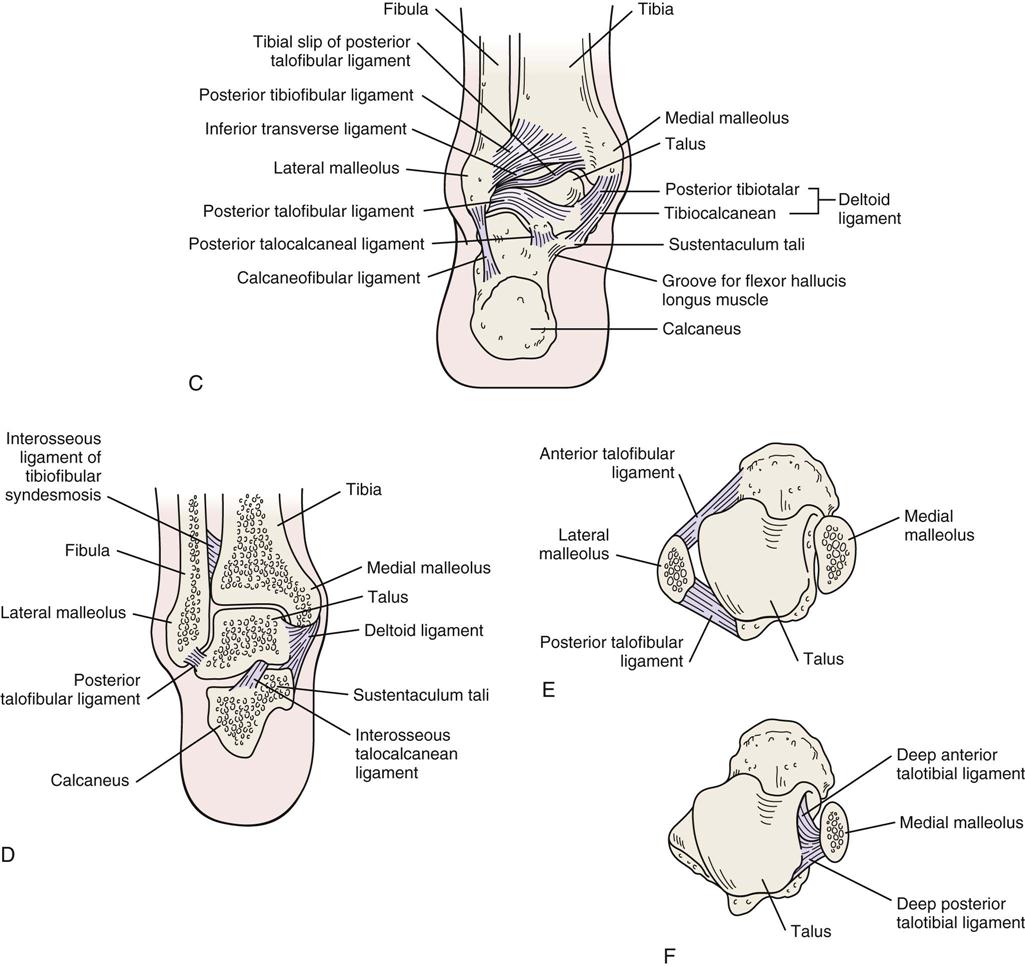
5. Was there any swelling or bruising (ecchymosis) (Figure 13-4, A)? How quickly and where did it develop? This question can elicit some idea of the type of swelling (e.g., blood, synovial, purulent) and whether it is intracapsular or extracapsular. Figure 13-4, B, shows “skate bite” in which there is swelling over the extensor tendons of the foot caused by irritation from doing up stiff ice skates too tight.
6. Are symptoms improving, becoming worse, or staying the same? It is important to know the type of onset (macrotrauma, microtrauma) and the duration and intensity of symptoms (acute, subacute, chronic). Edwards et al.17 outlined some of the chronic causes of leg pain in athletes.
7. What are the sites and boundaries of pain or abnormal sensation? The examiner should note whether the pattern is one of a dermatome, a peripheral nerve, or another painful structure. If pain and other physical findings are “out of proportion” to what would normally be expected with injury especially in the rearfoot/talar region, a more diligent examination including extra radiographic images of the talus and calcaneus may be necessary.18
10. Where is the pain? Does the patient indicate a specific location or area? For example, with shin splints (medial tibial stress syndrome) or a compartment syndrome (acute or chronic type), the patient usually indicates a diffuse area.19–22 With a stress fracture, the area of pain tends to be more specific. Anterolateral ankle impingement demonstrates anterolateral ankle joint tenderness, anterolateral ankle joint swelling (extracapsular), pain with force dorsiflexion and eversion, pain with single leg squat, pain with activities, and possible absence of ankle instability.11 Peroneal tendon problems show posterolateral pain and may be associated with lateral ankle instability.23 Plantar fasciitis is the most common cause of heel pain on the antero-medial aspect of the heel.24 It may be accompanied by a heel spur (see Figure 13-135, C), which is the result of the plantar fasciitis.
14. For active people, especially runners or joggers, the following questions should also be considered25:
a. How long has the patient been running or jogging?
b. On what type of terrain and surface does the patient train?
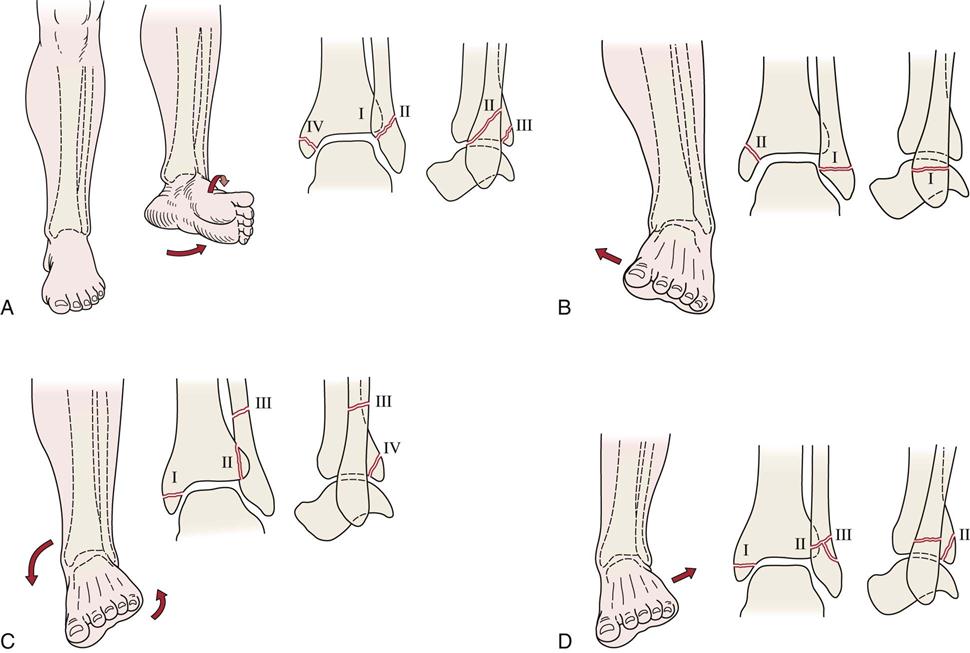
A, Supination-lateral rotation injury. Lateral rotation forces applied to a supinated foot initially result in rupture of the anterior tibiofibular ligament (stage I). As the forces continue, a short oblique fracture of the distal portion of the fibula occurs (stage II). Stage III involves a fracture of the posterior aspect of the tibia. Stage IV is a fracture of the medial malleolus. B, Supination-adduction injury. Adduction forces applied to a supinated foot initially result in a traction or avulsion fracture of the distal portion of the fibula or rupture of the lateral ligaments (stage I). As forces continue, fracture of the medial malleolus or rupture of the deltoid ligament occurs (stage II). The fibular fracture is typically transverse, and that of the medial malleolus is oblique or nearly vertical. C, Pronation-lateral rotation injury. Forces of lateral rotation applied to a pronated foot initially result in rupture of the deltoid ligament or fracture of the medial malleolus (stage I). As forces continue, the anterior tibiofibular ligament is ruptured (stage II). A high fibular fracture (stage III) and fracture of the posterior tibial margin (stage IV) are the final stages in this mechanism of injury. D, Pronation-abduction injury. The first two stages of this injury are identical to those of the pronation-external rotation fracture complex. Stage III is a transverse supramalleolar fibular fracture that may be comminuted laterally. (Redrawn from Resnick D, Kransdorf MJ: Bone and joint imaging, Philadelphia, 2005, WB Saunders, pp. 867–868.)
TABLE 13-1
The West Point Ankle Sprain Grading System
| Criterion | Grade I | Grade II | Grade III |
| Location of tenderness | Anterior talofibular ligament | Anterior talofibular ligament and calcaneofibular ligament | Anterior talofibular ligament, calcaneofibular ligament and posterior talofibular ligament |
| Edema and ecchymosis | Slight and local | Moderate and local | Significant and diffuse |
| Weight-bearing ability | Full or partial | Difficult without crutches | Impossible without significant pain |
| Ligament damage | Stretched | Partial tear | Complete tear |
| Instability | None | None or slight | Definite |
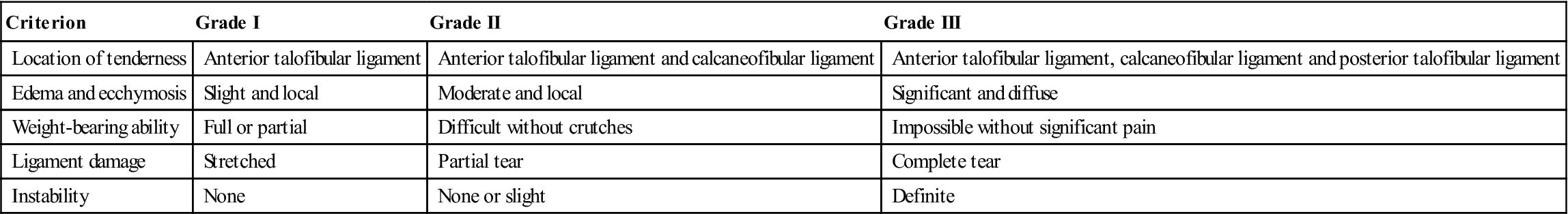
From Dutton M: Dutton’s orthopedic examination, evaluation and intervention, ed 3, New York, 2012, McGraw Hill. Data from Gerber JP, et al: Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int 19:653–660, 1998.
Observation
Observation of the foot is extensive. Because of the stresses the foot is subjected to and because it, like the hand, can project signs of systemic problems and disease, the examiner should carefully and meticulously inspect the foot.
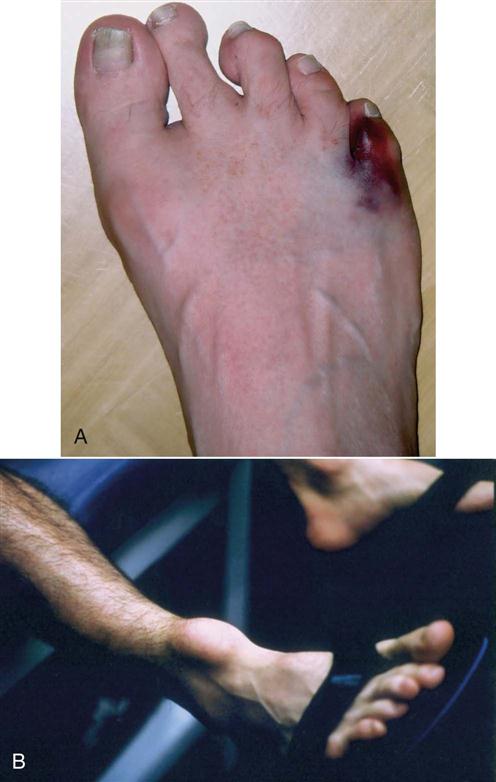
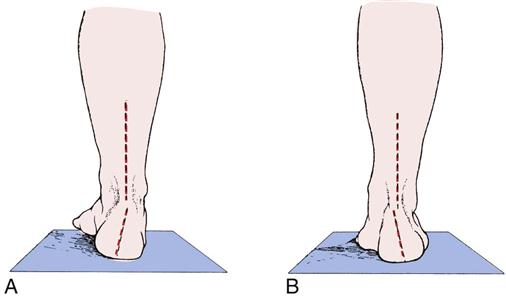
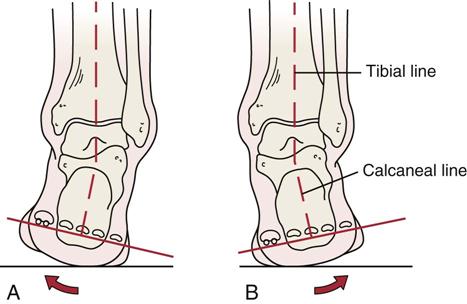
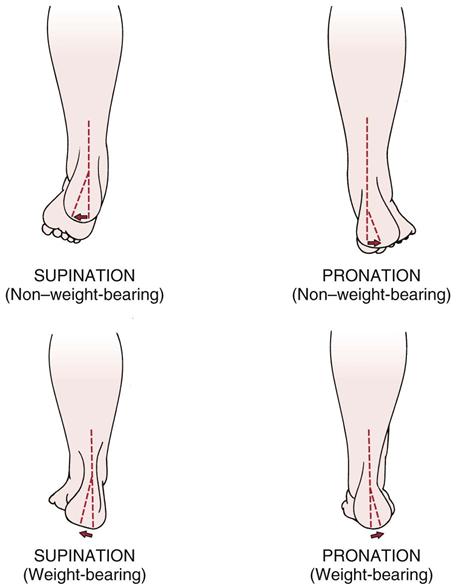
When performing the observation, the examiner should remember to compare the weight-bearing (closed-chain) with the non–weight-bearing (open-chain) posture of the foot.26 During open-chain motion, the talus is considered fixed; during closed-chain motion, the talus moves to help the foot and leg adapt to the terrain and to the stresses that are applied to the foot. Even though the calcaneus is touching a surface in closed-chain movement, for descriptive purposes, it is still considered to be moving. The weight-bearing stance of the foot shows how the body compensates for structural abnormalities (Figure 13-5). The non–weight-bearing posture shows functional and structural abilities without compensation (Figure 13-6). The observation includes looking at the patient from the front, from the side, and from behind in the weight-bearing (standing) position and from the front, from the side, and from behind in the sitting position with the legs and feet not bearing weight. The examiner should note the patient’s willingness and ability to use the feet. The bony and soft-tissue contours of the foot should be normal, and any deviation should be noted. Often, painful callosities may be found over abnormal bony prominences. The examiner should note any scars or sinuses.
Weight-Bearing Position, Anterior View
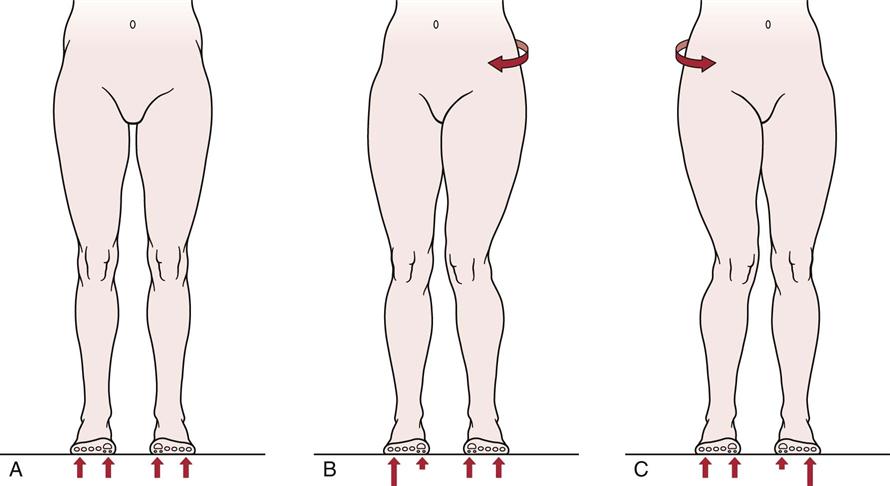
With the patient in a standing position, the examiner should observe whether the patient’s hips and trunk are in normal position. Excessive lateral rotation of the hip or rotation of the trunk away from the opposite hip elevates the medial longitudinal arch of the foot, whereas medial rotation of the hip or trunk rotation toward the opposite hip tends to flatten the arch (Figure 13-7). Medial rotation of the hip can also cause pigeon toes, which is a condition more commonly associated with medial tibial torsion or rotation. If the iliotibial band is tight, the tightness may cause eversion and lateral rotation of the foot.
The examiner should also look at the tibia to note any local or general bone swelling (Figure 13-8). Does the tibia have a normal shape, or is it bowed? Is there any torsional deformity? The medial malleolus usually lies anterior to the lateral malleolus. Pigeon toes, or toe-in deformity, result from a medial tibial torsion deformity; it does not constitute a foot deformity (Table 13-2).
TABLE 13-2
Causes of Toeing-In and Toeing-Out in Children
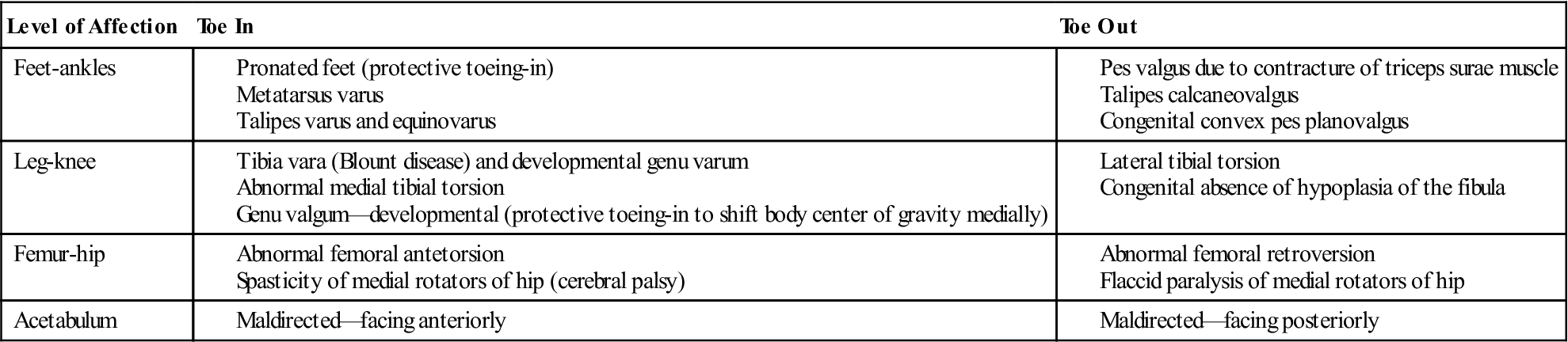
From Tachdjian MO: Pediatric orthopedics, Philadelphia, 1990, WB Saunders, p. 2817.
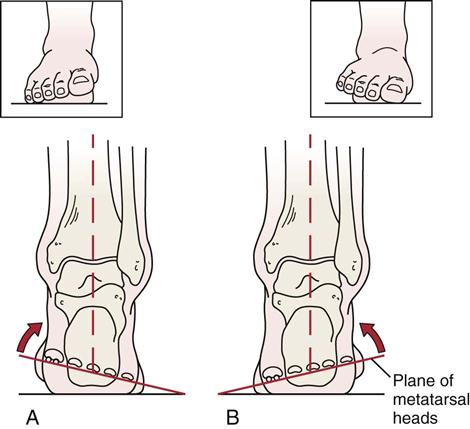
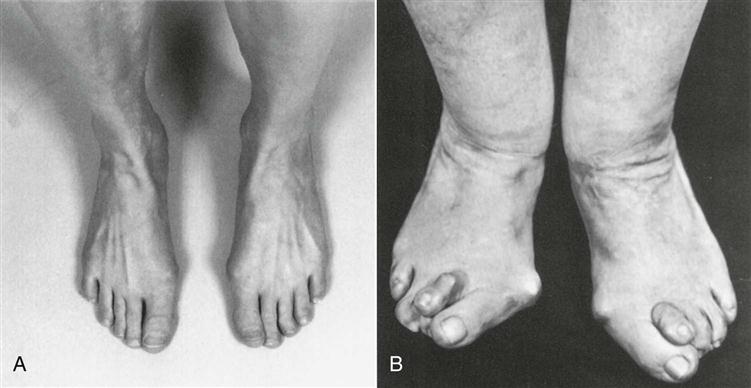
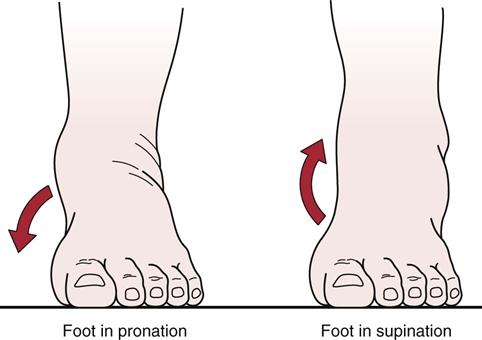
Figure 13-9 shows the anterosuperior view of the feet in the weight-bearing stance. The examiner should note whether there is any asymmetry, malalignment (Table 13-3), or excessive supination or pronation of the foot. Supination of the foot involves inversion and outward rotation of the heel, adduction of the forefoot with inward rotation at the tarsometatarsal joints to maintain contact with the ground and outward rotation at the midtarsal joints, and plantar flexion at the subtalar joint and midtarsal joints so that the medial longitudinal arch is accentuated (Figure 13-10, A). In addition, along with lateral rotation of the talus, there is lateral rotation of the leg in relation to the foot (Figure 13-11). Supination of the foot causes the proximal aspect of the tibia to move posteriorly. It is required during propulsion to give rigidity to the foot and requires less muscle work than pronation.
TABLE 13-3
Malalignment About the Foot and Ankle
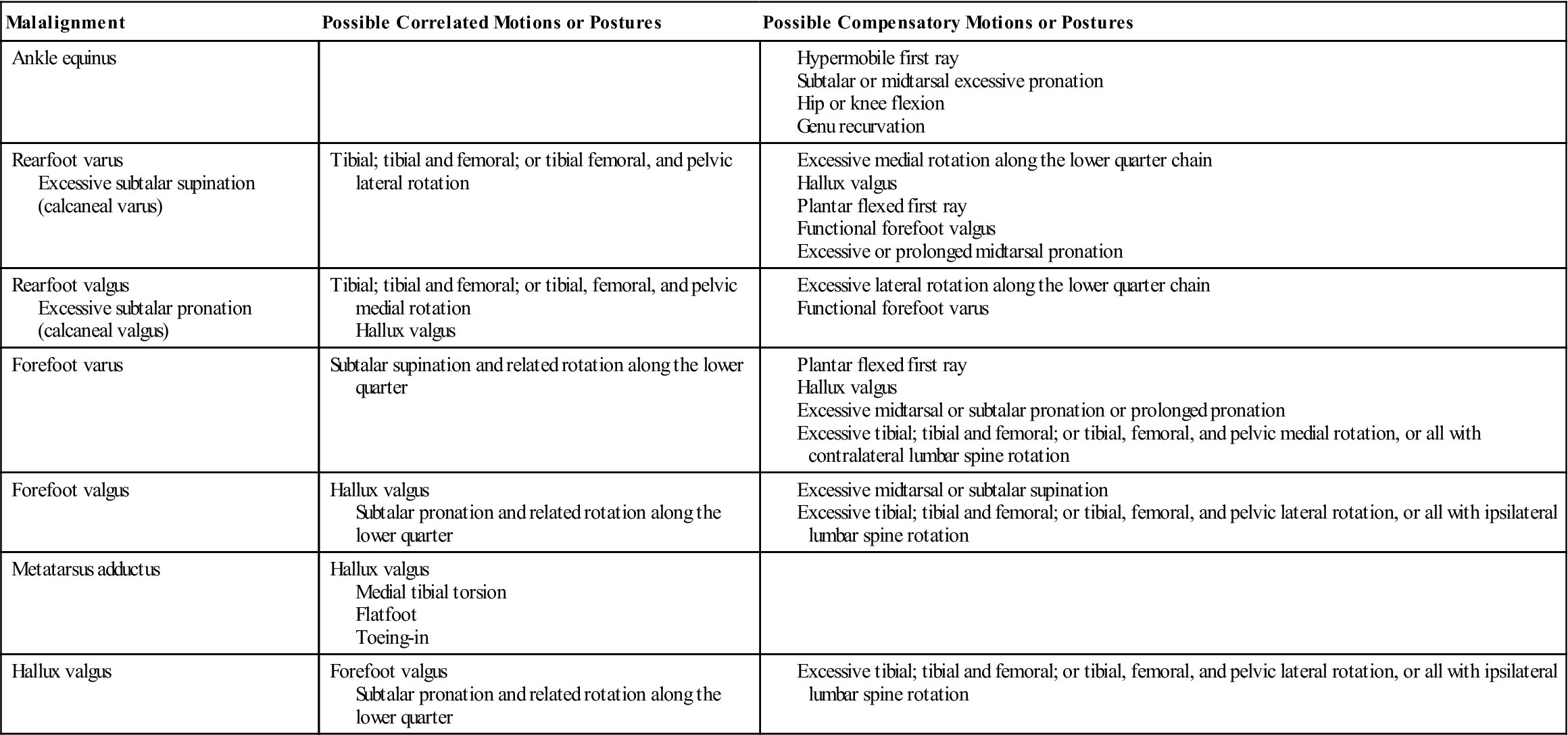
From Riegger-Krugh C, Keysor JJ: Skeletal malalignment of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther 23:166, 1996.
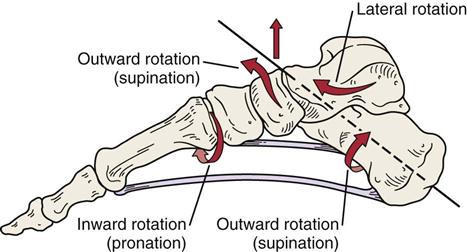
The rear foot and midfoot outwardly rotate (supinate) and the forefoot inwardly rotates (pronates) on the midfoot. As foot is plantar flexed, plantar fascia becomes tight along with ligaments to provide stable foot for push off. (Modified from Richardson JK, Iglarsh ZA, editors: Clinical orthopedic physical therapy, Philadelphia, 1994, WB Saunders, p. 513.)
Pronation of the foot involves eversion and inward rotation of the heel, abduction of the forefoot with outward rotation at the tarsometatarsal joints and inward rotation at the midtarsal joints, and medial rotation of the talus causing medial rotation of the leg in relation to the foot, and dorsiflexion of the subtalar and midtarsal joints (Figure 13-12), resulting in a decrease in the medial longitudinal arch (Figure 13-10, B). This movement causes the proximal aspect of the tibia to move anteriorly. The pronated foot has greater subtalar motion than the supinated foot and requires more muscle work to maintain stance stability than the supinated foot. The foot is much more mobile in this position.
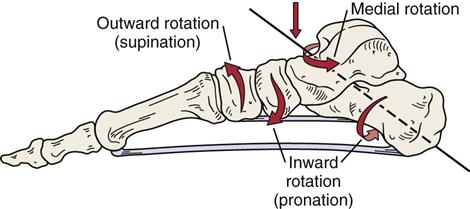
The rear foot and midfoot inwardly rotate (pronate) and the forefoot outwardly rotates (supinates) on the midfoot. Plantar fascia and plantar ligaments become taut as they absorb the ground reaction forces. (Modified from Richardson JK, Iglarsh ZA, editors: Clinical orthopedic physical therapy, Philadelphia, 1994, WB Saunders, p. 513.)
The definitions used in this chapter are the ones preferred by orthopedists and podiatrists. Anatomists and kinesiologists, such as Kapandji, refer to inversion as a combination of adduction and supination and to eversion as a combination of abduction and pronation.27 Lipscomb and Ibrahim28 and Williams and Warwick29 have defined supination and pronation as opposite the terms just mentioned. Because of the confusion in terminology concerning the terms supination and pronation, readers of books and articles on the foot must be careful to discern exactly what each author means.
In the infant, the foot is normally pronated. As the child matures, the foot begins to supinate, accompanied by development of the medial longitudinal arch. The foot also appears to be more pronated in the infant because of the fat pad in the medial longitudinal arch.
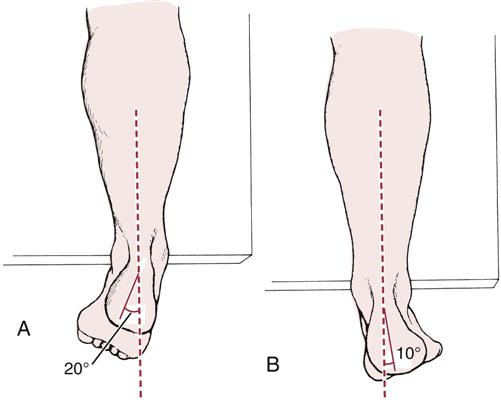
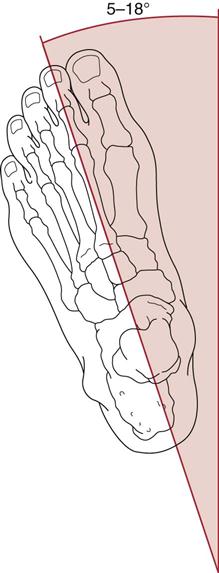
The examiner should note how the patient stands and walks. Normally, in standing, 50% to 60% of the weight is taken on the heel and 40% to 50% is taken by the metatarsal heads. The foot assumes a slight toe-out position. This angle (the Fick angle) is approximately 12° to 18° from the sagittal axis of the body, developing from 5° in children (Figure 13-13).30 Asymmetrical or excessive lateral rotation of the foot may be due to acetabular retroversion, femoral retrotorsion or femoral head neck abnormalities31 (see Chapter 11). During movement, the foot is subjected to high loading, and pathology may cause the gait to be altered. The cumulative force to which each foot is subjected during the day is the equivalent of 639 metric tons in a person who weighs approximately 90 kg, or the equivalent of walking 13 km per day.
When weight-bearing, if the relation of the foot to the ankle is normal, all of the metatarsal bones bear weight, and all of the metatarsal heads lie in the same transverse plane. The forefoot and hindfoot should be parallel to each other and to the floor. The midtarsal joints are in maximum pronation, and the subtalar joint is in neutral position. The subtalar and talocrural joints should be parallel to the floor. Finally, the posterior bisection of the calcaneus and distal one third of the leg should form two vertical, parallel lines.32
If the examiner has noted any asymmetry in standing, the examiner should place the talus (or foot) in neutral (see the “Special Tests” section) to see if the asymmetry disappears. If the asymmetry is present in normal standing, it is a functional asymmetry. If it is still present when the foot is in neutral, it is also an anatomical or structural asymmetry, in which case a structural deformity is probably causing the asymmetry. Leg-heel and forefoot-heel alignment (see the “Special Tests” section) may also be checked, especially if asymmetry is present.
The examiner should note whether the patient uses a cane or other walking aid. Use of a cane in the opposite hand diminishes the stress on the ankle joint and foot by approximately one third.
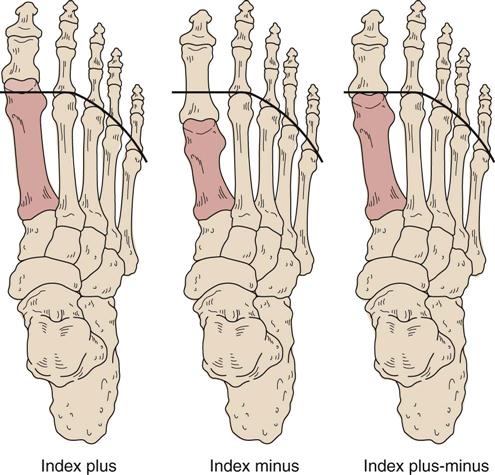
Any prominent bumps or exostoses should be noted, as should any splaying (widening) of the forefoot. Splaying of the forefoot and metatarsus primus varus is more evident in weight-bearing. There are three types of forefoot,33 based on the length of the metatarsal bones (Figure 13-14):
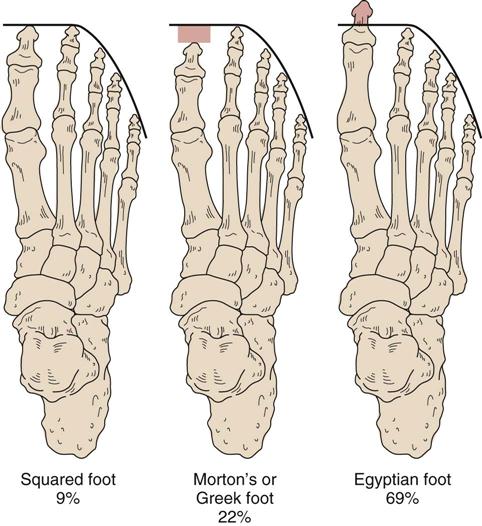
1. Index plus type: The first metatarsal (1) is longer than the second (2), with the others (3, 4, and 5) of progressively decreasing lengths, so that 1 > 2 > 3 > 4 > 5. This can result in an Egyptian type foot (Figure 13-15).
2. Index plus-minus type: The first metatarsal is equal in length to the second metatarsal, with the others progressively diminishing in length, so that 1 = 2 > 3 > 4 > 5. This results in a squared type foot (see Figure 13-15).
3. Index minus type: The second metatarsal is longer than the first and third metatarsals. The fourth and fifth metatarsals are progressively shorter than the third, so that 1 < 2 > 3 > 4 > 5. This results in a Morton’s or Greek type foot (see Figure 13-15).
The examiner should note whether the toenails appear normal. Older individuals have more brittle nails. The examiner should look for warts, calluses, and corns. Warts are especially tender to the pinch (but not to direct pressure), but calluses are not. Plantar warts also tend to separate from the surrounding tissues, but calluses do not. Corns are similar to calluses but have a central nidus. They may be hard (on outside or upper aspect of toes) or soft (between toes) because of moisture.
Any swelling or pitting edema within the Achilles tendon, ankle, and foot should be noted (Figure 13-16). If there is any swelling, the examiner should note whether it is intracapsular or extracapsular. Swelling above the lateral malleolus may be related to a fibular fracture or disruption of the syndesmosis (“high” ankle sprain).34,35 This injury takes a long time to heal and may involve the anterior and/or posterior tibiofibular ligament as well as the ligaments of the talocrural joint. Swelling posterior to the lateral malleolus may indicate peroneal retinacular injury. Lateral ankle sprains initially swell distal to the lateral malleolus, but swelling may spread into the foot if the capsule has been torn (Table 13-4).14 The examiner should also check the patient’s gait for the position of the foot at heel strike, at foot flat, and at toe off. The gait cycle is described in greater detail in Chapter 14.

A, Note pattern of pitting edema on top of the left foot. B, The swelling is intracapsular, as indicated by swelling on both sides of the left Achilles tendon. C, Extracapsular swelling. D, Midtarsal swelling. E, Synovial thickening (not swelling) because of repeated ankle sprains. F, Achilles swelling.
TABLE 13-4
Classification of Ankle Sprains
| Severity | Pathology | Signs and Symptoms | Disability |
| Grade I (mild) stable | |||
| Grade II (moderate) stable | |||
| Grade III (severe) two-ligament, unstable |
From Reid DC: Sports injury assessment and rehabilitation, New York, 1992, Churchill Livingstone, p. 226.
Any vasomotor changes should be recorded, including loss of hair on the foot, toenail changes, osteoporosis as seen on radiographs, and possible differences in temperature between the limbs. Systemic diseases such as diabetes can also lead to foot problems as a result of altered sensation, which facilitates injury.
The examiner should look for any circulatory impairment or presence of varicose veins. Brick-red color or cyanosis when the limb is dependent is an indication of impairment. Does this condition change to rapid blanching, or does it stay normal on elevation of the limbs? Change indicates circulatory impairment.
Weight-Bearing Position, Posterior View
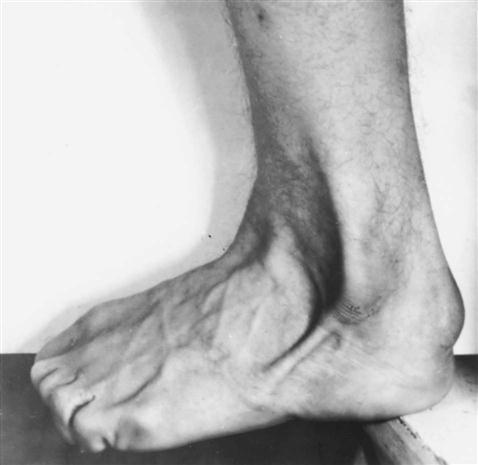
From behind, the examiner compares the bulk of the calf muscles and notes any differences. Variation may be caused by peripheral nerve lesions, nerve root problems, or atrophy resulting from disuse after injury. The Achilles tendons on each side should be compared (see Figure 13-16, F). If a tendon appears to curve out (Figure 13-17), it may indicate a fallen medial longitudinal arch, resulting in a pes planus (flatfoot) condition (Helbing sign).36
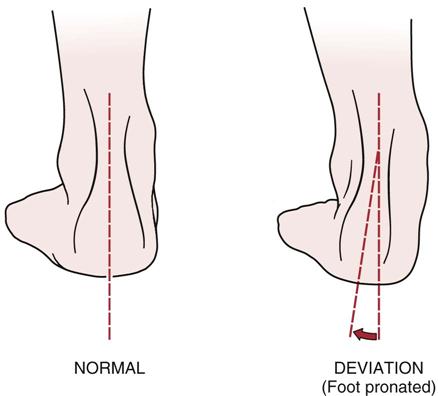
The deviation is often seen with pes planus (flatfoot) and when the medial longitudinal arch is lower or has “dropped.”
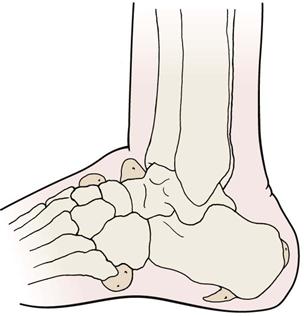
The examiner observes the calcaneus for normality of shape and position. Runners often build up bone and a callus on the heel, producing a “pump bump” (Haglund disease or deformity) as a result of pressure on the heel (Figure 13-18).37–39

The malleoli are compared for positioning. Normally, the lateral malleolus extends farther distally than the medial malleolus; however, the medial malleolus extends farther anteriorly.
Weight-Bearing Position, Lateral View
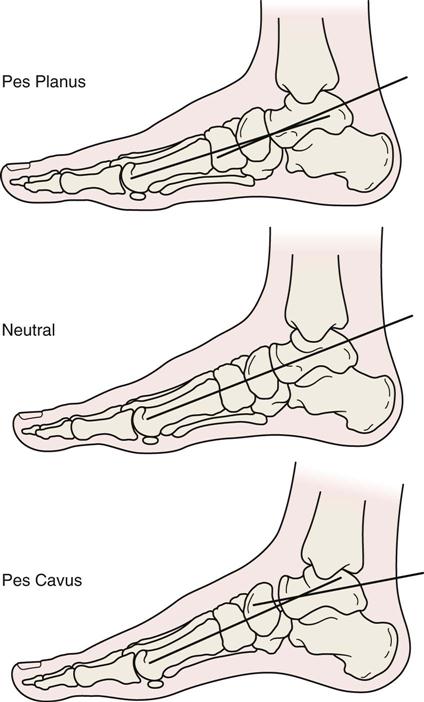
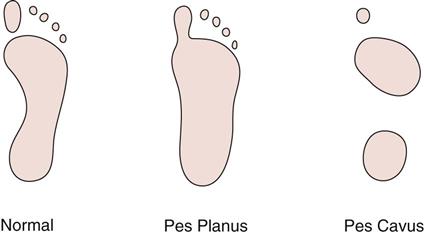
With the side view, the examiner is primarily observing the longitudinal arches of the foot (Figure 13-19). The examiner should note whether the medial arch is higher than the lateral arch (as would be expected). Differences in the arches may often be determined by looking at the footprint patterns (Figure 13-20). The footprint pattern can be established by putting a light film of baby oil and then powder on the patient’s foot and asking the patient to step down on a piece of colored paper.
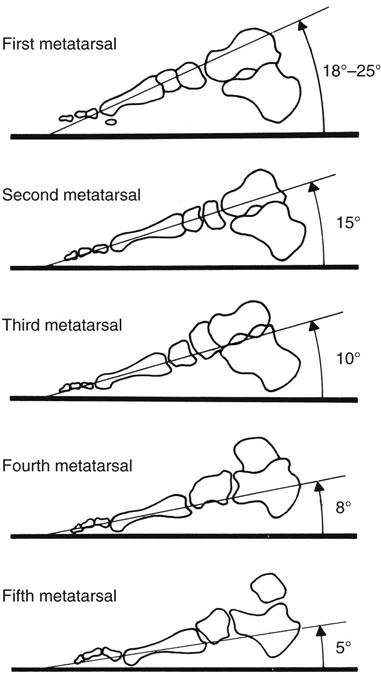
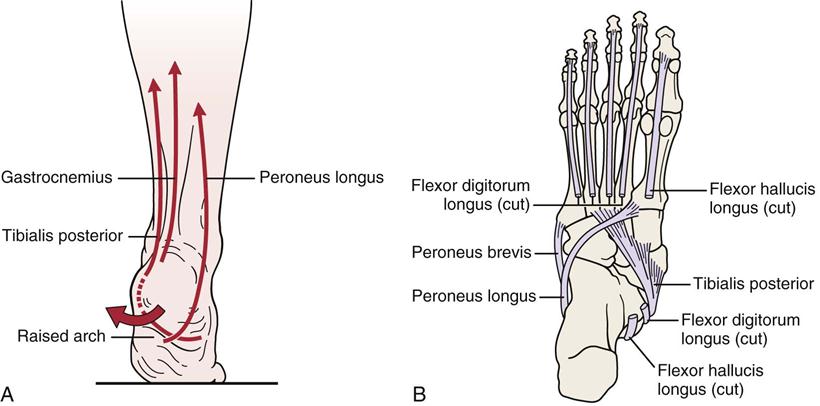
The arches of the feet (Figure 13-21) are maintained by three mechanisms40: (1) wedging of the interlocking tarsal and metatarsal bones; (2) tightening of the ligaments on the plantar aspect of the foot; and (3) the intrinsic and extrinsic muscles of the foot and their tendons, which help to support the arches. The longitudinal arches form a cone as a result of the angle of the metatarsal bones in relation to the floor. With the medial longitudinal arch being more evident, this angle is greater on the medial side. The angle formed by each of the metatarsals with the floor is shown in Figure 13-22.
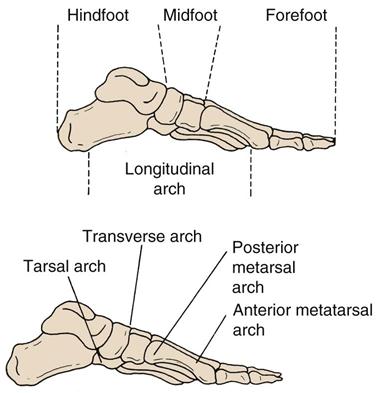
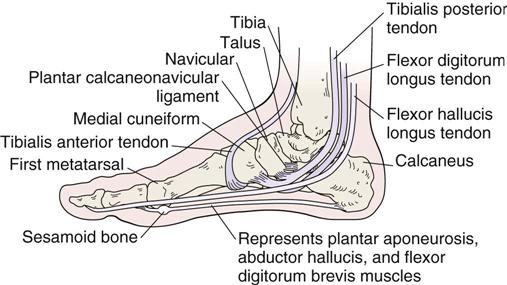
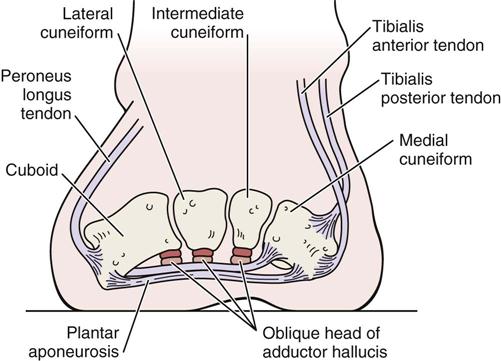
The medial longitudinal arch consists of the calcaneal tuberosity, the talus, the navicular, three cuneiforms, and the first, second, and third metatarsal bones (Figures 13-23 and 13-24). This arch is maintained by the tibialis anterior, tibialis posterior, flexor digitorum longus, flexor hallucis longus, abductor hallucis, and flexor digitorum brevis muscles; the plantar fascia or aponeurosis; and the plantar calcaneonavicular ligament. The plantar aponeurosis plays a major role during the stance and push-off phases of gait, which helps to distribute Achilles tendon forces under the forefoot to the metatarsal heads and phalanges.41
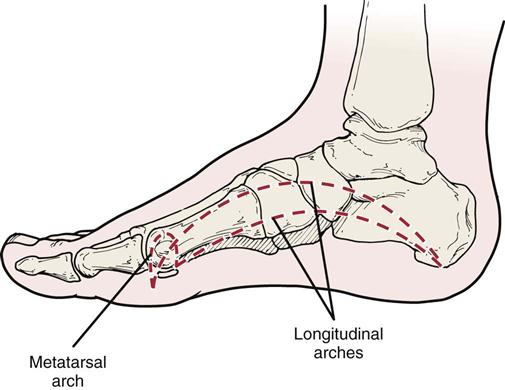
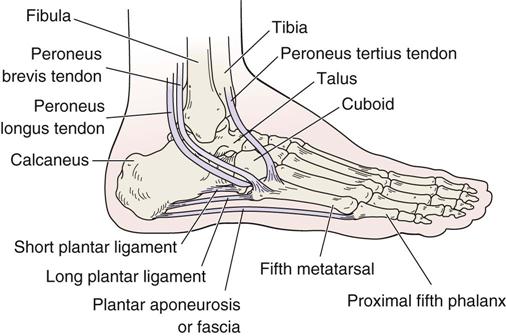
The calcaneus, cuboid, and fourth and fifth metatarsal bones make up the lateral longitudinal arch (Figure 13-25). This arch is more stable and less adjustable than the medial longitudinal arch. The arch is maintained by the peroneus longus, peroneus brevis, peroneus tertius, abductor digiti minimi, and flexor digitorum brevis muscles; the plantar fascia; the long plantar ligament; and the short plantar ligament.40
The transverse arch is maintained by the tibialis posterior, tibialis anterior, and peroneus longus muscles and the plantar fascia (Figure 13-26). This arch consists of the navicular, cuneiforms, cuboid, and metatarsal bones. The arch is sometimes divided into three parts: tarsal, posterior metatarsal, and anterior metatarsal. A loss of the anterior metatarsal arch results in callus formation under the heads of the metatarsal bones (especially the second and third metatarsal heads). The metatarsophalangeal joints are slightly extended when the patient is in the normal standing position because the longitudinal arches of the foot curve down toward the toes.40
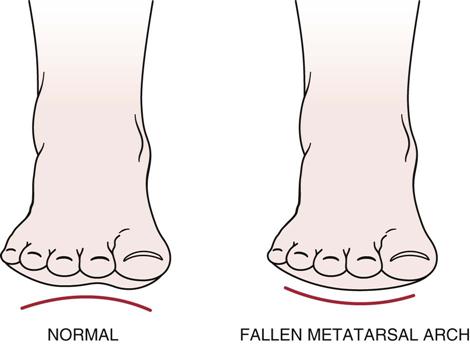
Non–Weight-Bearing Position
With the patient in a supine, non–weight-bearing position, the examiner should look for abnormalities, such as callosities, plantar warts, scars, and sinuses or pressure sores on the soles of the feet, as well as swelling, which is more prominent on the dorsum of the foot. In addition, by looking at the foot from anterior to posterior, as shown in Figure 13-27, the examiner can observe whether the patient has a “fallen” metatarsal arch. Normally, in the non–weight-bearing position, the arch is visible. If the arch falls, callosities are often found over the metatarsal heads. The arch may be reversed, or it may fall because of an equinus forefoot, pes cavus, rheumatoid arthritis, short heel cord, or hammertoes. Abnormal width of one ankle in relation to the other (Keen sign) may be caused by swelling, loss of integrity of the syndesmosis, or a malleolar fracture.
Young children should be assessed for clubfoot deformities, the most common of which is talipes equinovarus (Figures 13-28 and 13-29; Table 13-5). These types of deformities are often associated with other anomalies, such as spina bifida.
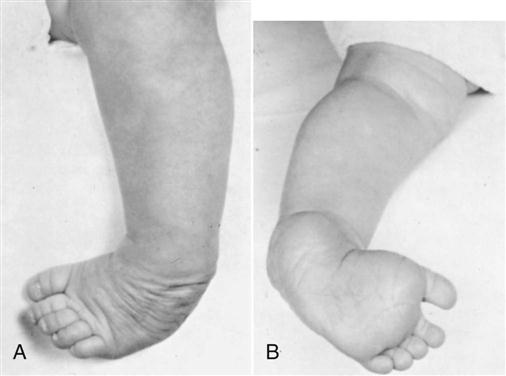
A, Anterior view. B, Posterior view. (From Klenerman L: The foot and its disorders, Boston, 1982, Blackwell Scientific, p. 64.)
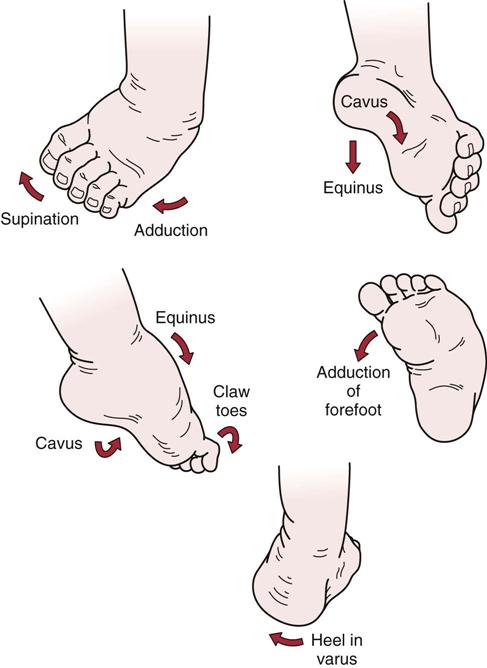
TABLE 13-5
Differential Diagnosis of Postural Clubfoot and Talipes Equinovarus
| Postural Clubfoot | Talipes Equinovarus | |
| Etiology | Intrauterine malposture | Primary germ plasm defect |
| Defective cartilaginous anlage of the talus | ||
| Pathologic Anatomy | ||
| Head and neck of talus | Normal | Medial and plantar tilt |
| Declination angle of talus normal (150° to 155°) | Declination angle of talus decreased (115° to 135°) | |
| Talocalcaneonavicular joint | Normal | Subluxed or dislocated medially and plantarward |
| Effect of manipulation in fetal specimens | Normal alignment of foot can be restored | Talocalcaneonavicular subluxation cannot be reduced unless ligaments connecting navicular to calcaneus, talus, and tibia are sectioned and posterior capsule and ligaments divided |
| Clinical Features | ||
| Severity of deformity | Mild and flexible | Marked and rigid |
| Heel | Normal size | Small, drawn up |
| Relation between navicular and medial malleolus | Normal space between two bones; can insert finger | Navicular abuts medial malleolus: finger cannot be inserted between two bones |
| Lateral malleolus Skin creases on: |
Normal position | Posteriorly displaced with anterior part of talus very prominent in front of it |
| Dorsolateral aspect of foot | Present; normal | Thin or absent |
| Medial and plantar aspects of foot | No furrowed skin | Furrowed skin |
| Posterior aspect of ankle | Normal | Deep crease |
| Calf and leg atrophy | None or very minimal | Moderate to marked |
| Treatment | Passive manipulation followed by retention by adhesive strapping, splint, or cast | Primary open reduction of talocalcaneonavicular joint often required; surgery is conservative |
| Closed methods of reduction often unsuccessful | ||
| Prolonged retentive apparatus essential | ||
| Prognosis | Excellent; result is normal foot | Poor with closed methods |
| Prolonged cast immobilization results in smaller foot and atrophied leg |
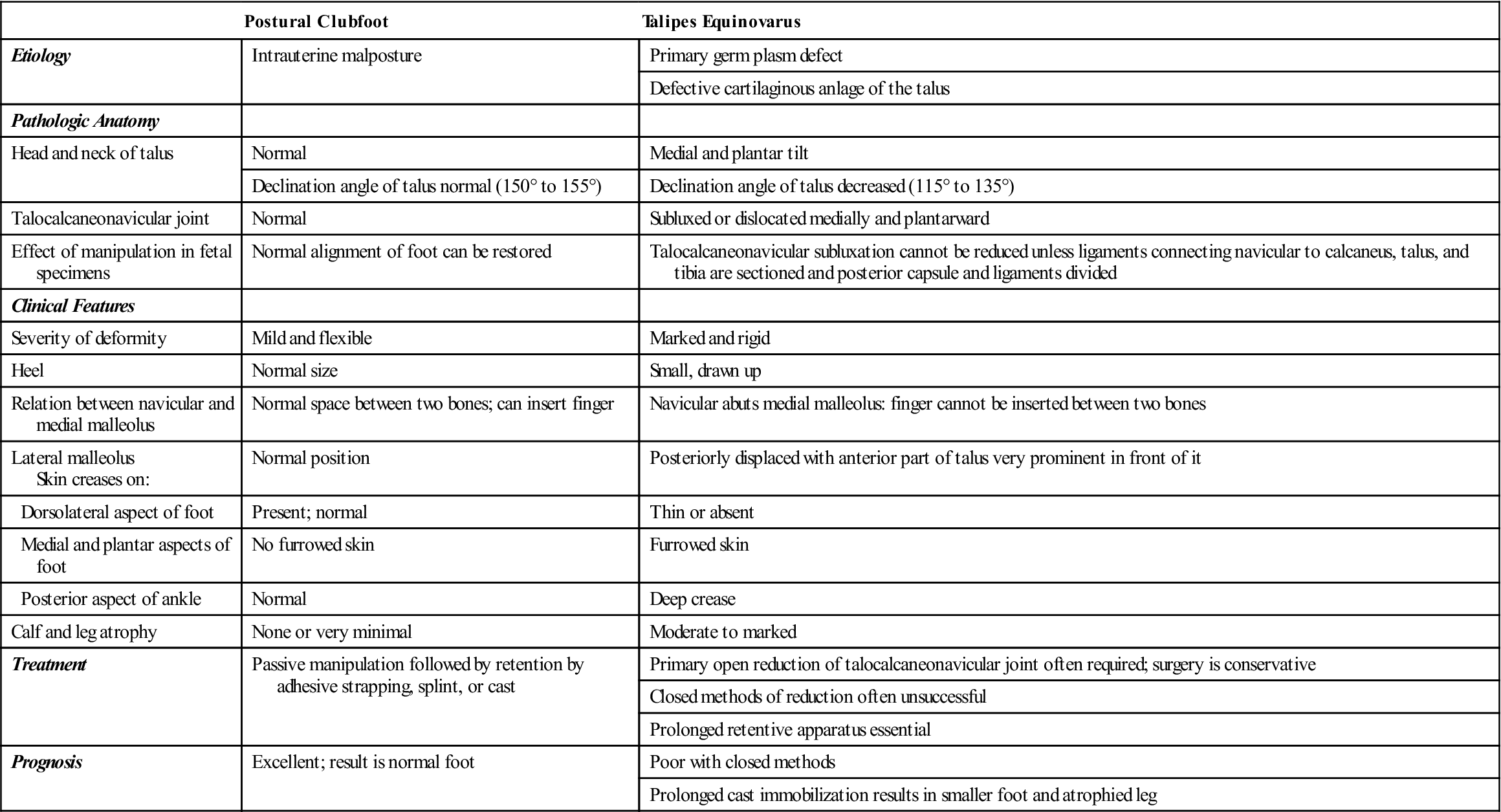
From Tachdjian MO: The child’s foot, Philadelphia, 1985, WB Saunders, p. 163.
Common Deformities, Deviations, and Injuries
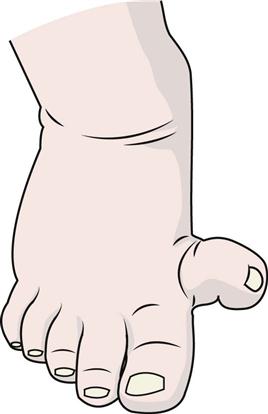
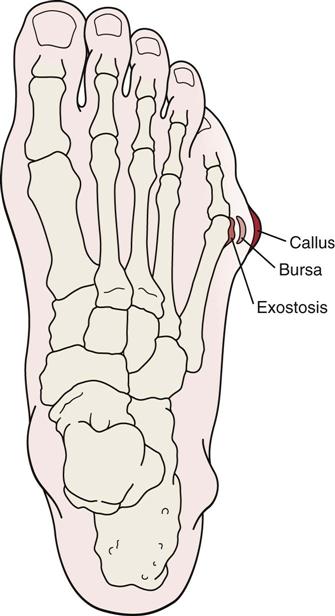
Bunionette (Tailor’s Bunion).
This deformity is characterized by prominence of the lateral aspect of the fifth toe metatarsal head (Figure 13-30).42 If associated with hallux valgus, it results in a splayed foot. It is often associated with a pronated foot.
Claw Toes.
A claw-toe deformity results in hyperextension of the metatarsophalangeal joints and flexion of the proximal and distal interphalangeal joints (Figure 13-31, A). Claw toes usually result from the defective actions of lumbrical and interosseus muscles that cause the toes to become functionless. This condition may be unilateral or bilateral and may be associated with pes cavus, fallen metatarsal arch, spina bifida, or other neurological problems.
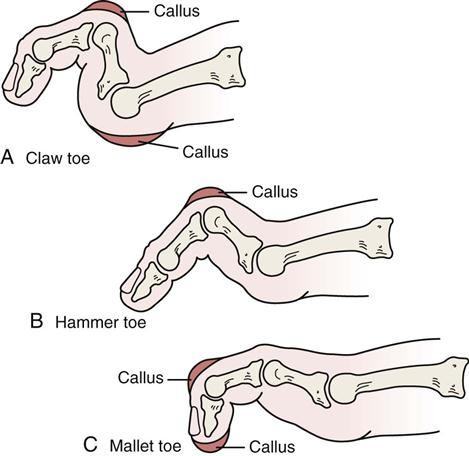
A, Claw toe. Note that the proximal and distal interphalangeal joints are hyperflexed and the metatarsophalangeal joint is dorsally subluxated. B, Hammer toe. Note the flexion deformity of the proximal interphalangeal joints. The distal interphalangeal joint is in neutral position or slight flexion. C, Mallet toe. There is flexion contracture of the distal interphalangeal joint. The proximal interphalangeal and metatarsophalangeal joints are in neutral position.
Clubfoot.
This congenital deformity is relatively common and can take many forms, the most common of which is talipes equinovarus. Its cause is unknown, but there are probably multifactorial genetic causes modified by environmental factors.43 It sometimes coexists with other congenital deformities, such as spina bifida and cleft palate. The flexible form is easily treated, but the resistant type often requires surgery. On assessment, the ROM is limited and the foot has abnormal form (see Figure 13-29).
Crossover Toe.
Crossover toe is the result of weakening of the lateral collateral ligament of the metatarsophalangeal joint and insufficiency of the plantar plate along with the pull of the extrinsic muscles resulting in medial deviation of the toe, most commonly in the second or third toe. It is often associated with hallux valgus.44
Curly Toe.
A curly toe deformity involves a flexion deformity of both the proximal and distal interphalangeal joints with the metatarsophalangeal joint in neutral or flexion, often combined with rotation. It is the result of contracture of flexor digitorum brevis and longus tendons and is most commonly seen in the fifth toe in children.44
Equinus Deformity (Talipes Equinus).
This deformity is characterized by limited dorsiflexion (less than 10°) at the talocrural joint, usually as a result of contracture of the gastrocnemius or soleus muscles or Achilles tendon. It may also be caused by structural bone deformity (primarily in the talus), trauma, or inflammatory disease. The deformity causes increased stress to the forefoot, which may lead to a rocker-bottom foot and excessive pronation at the subtalar joint. This deviation can contribute to conditions such as plantar fasciitis, metatarsalgia, heel spurs, and talonavicular pain.25
Exostosis (Bony Spur).
Exostosis is an abnormal bony outgrowth extending from the surface of the bone (Figure 13-32). It is actually an increase in the bone mass at the site of an irritative lesion in response to overuse, trauma, or excessive pressure. The common areas of occurrence in the foot are on the dorsal aspect of the tarsometatarsal joint, the head of the fifth metatarsal bone, the calcaneus (where it is often called a pump bump or runner’s bump), the insertion of the plantar fascia, and the superior aspect of the navicular bone. Most often these exostoses are the result of poorly fitting footwear that leads to undue pressure on the bone.
Forefoot Valgus.
This structural midtarsal deviation involves eversion of the forefoot on the hindfoot when the subtalar joint is in the neutral position because the normal valgus tilt (35° to 45°) of the head and neck of the talus to its trochlea has been exceeded. With this deformity, during the weight-bearing phase of gait, the midtarsal joint is supinated so that the lateral aspect of the foot is brought into contact with the ground. Like hindfoot valgus, it contributes to decreasing the medial longitudinal arch and, therefore, clinically resembles a planus foot. The prolonged supination can contribute to conditions such as lateral ankle sprains, iliotibial band syndrome, plantar fasciitis, anterior tarsal tunnel syndrome, toe deformities, sesamoiditis, and leg and thigh pain (Figure 13-33, B).25,45
Forefoot Varus.
This structural midtarsal joint deviation involves inversion of the forefoot on the hindfoot when the subtalar joint is in the neutral position. It occurs because the normal valgus tilt (35° to 45°) of the head and neck of the talus to its trochlea has not been achieved.25,45,46 Clinically, it contributes to decreasing the medial longitudinal arch and, therefore, resembles pes planus. With this deformity, during the weight-bearing phase of gait, the midtarsal joint is completely pronated in an attempt to bring the first metatarsal head in contact with the ground. The prolonged rotation that results can contribute to conditions, such as tibialis posterior paratenonitis, patellofemoral syndrome, toe deformities, ligamentous stress (medially), shin splints, plantar fasciitis, postural fatigue, and Morton’s neuroma (Figure 13-33, A).
Hallux Rigidus.
Hallux rigidus is a condition in which dorsiflexion or extension of the big toe is limited because of osteoarthritis of the first metatarsophalangeal joint.47 Hallux rigidus may also be caused by an anatomical abnormality of the foot, an abnormally long first metatarsal bone (index plus type forefoot; see Figure 13-14), pronation of the forefoot, or trauma. There are two types: acute and chronic.
The acute, or adolescent, type occurs primarily in young people with long, narrow, pronated feet and occurs more frequently in boys than in girls. Pain and stiffness in the big toe come on quickly; the pain is described as constant, burning, throbbing, or aching. Tenderness may be palpated over the metatarsophalangeal joint, and the toe is initially held stiff because of muscle spasm. The first metatarsal head may be elevated, large, and tender. The weight distribution pattern in the gait is shown in Figure 13-34.
A, Hallux rigidus gait pattern. B, Normal gait pattern. C, Shoe develops oblique creases with hallux rigidus. (C, Redrawn from Jahss MH: Disorders of the foot, Philadelphia, 1991, WB Saunders, p. 60.)
The second (chronic) type of hallux rigidus is much more common and occurs primarily in adults—again, in men more frequently than in women. It is frequently bilateral and is usually the result of repeated minor trauma resulting in osteoarthritic changes to the metatarsophalangeal joint of the big toe. The toe stiffens gradually, and the pain, once established, persists. The patient complains primarily of pain at the base of the big toe on walking.
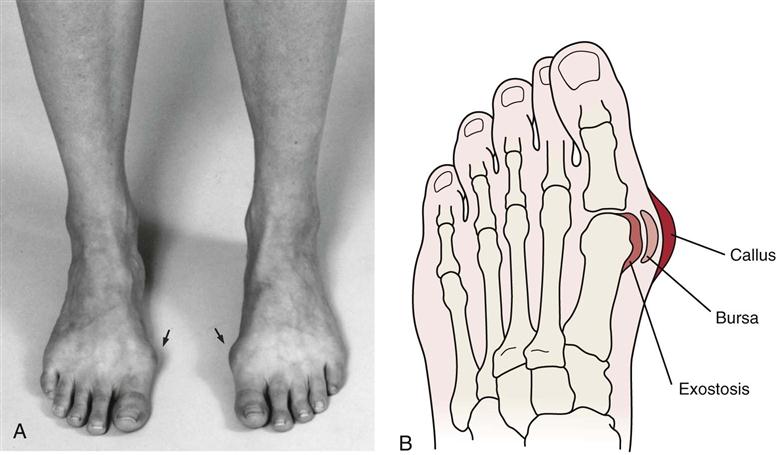
Hallux Valgus.
Hallux valgus is a relatively common condition in which there is medial deviation of the head of the first metatarsal bone in relation to the center of the body and lateral deviation of the head in relation to the center of the foot (Figure 13-35). The cause of hallux valgus is varied. It may result from a hereditary factor and is often familial. Women tend to be affected more than men. Trying to keep up with fashion may be a contributing factor if the patient wears tight or pointed shoes, tight stockings, or high-heeled shoes.48
As the metatarsal bones move medially, the base of the proximal phalanx is carried with it, and the phalanx pivots around the adductor hallucis muscle that inserts into it, causing the distal end as well as the distal phalanx to deviate laterally in relation to the center of the body. The long flexor and extensor muscles then have a bowstring effect as they are displaced to the lateral side of the joint, which can lead to increased stress on the proximal phalanx.49
A callus develops over the medial side of the head of the metatarsal bone, and the bursa becomes thickened and inflamed; excessive bone (exostosis) forms, resulting in a bunion (Figure 13-36).15,50 These three changes—callus, thickened bursa, and exostosis—make up the bunion, a condition separate from hallux valgus, although it is the result of hallux valgus.
In normal persons, the metatarsophalangeal angle (the angle between the longitudinal axis of the metatarsal bone and the proximal phalanx) is 8° to 20° (Figure 13-37). This angle is increased to varying degrees in hallux valgus.
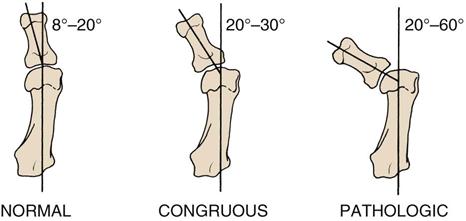
The first type (congruous hallux valgus) is a simple exaggeration of the normal relation of the metatarsal to the phalanx of the big toe. The deformity does not progress, and the valgus deformity is between 20° and 30°. The opposing joint surfaces are congruent. It requires little treatment, and often the biggest problem is cosmetic.
The second type (pathological hallux valgus) is a potentially progressive deformity, increasing from 20° to 60°. The joint surfaces are no longer congruent, and some may even go to subluxation. This type may occur in deviated (early) and subluxed (later) stages.
When looking at the foot, the examiner may find that there is a widening gap between the first and second metatarsal bones (increased intermetatarsal angle) and a lateral deflection of the phalanx at the metatarsophalangeal joint. The joint capsule lengthens on the medial aspect and is contracted on the lateral aspect. The toes rotate on the long axis so that the toenail faces medially because of the pull of the adductor hallucis muscle. Sometimes, the big toe deviates so far that it lies over or under the second toe.
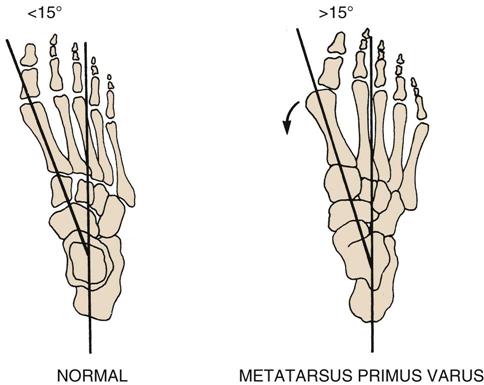
Of all hallux valgus cases, 80% are caused by metatarsus primus varus, in which the intermetatarsal or metatarsal angle is increased to more than 15° (Figure 13-38).51,52 Metatarsus primus varus is an abduction deformity of the first metatarsal bone in relation to the tarsal and other metatarsal bones so that the medial border of the forefoot is curved. Normally, this angle is between 0° and 15°.
Hammer Toe.
A hammer toe deformity consists of an extension contracture at the metatarsophalangeal joint and flexion contracture at the proximal interphalangeal joint; the distal interphalangeal joint may be flexed, straight, or hyperextended (Figure 13-31, B).50,53 The interosseus muscles are unable to hold the proximal phalanx in the neutral position and, therefore, lose their flexion effect. This results in clawing of the toe by the long flexors and extensors leading to and accentuating the deformity. The causes of hammer toe include an imbalance of the synergic muscles, hereditary factors, and mechanical factors, such as poorly fitting shoes or hallux valgus. It is usually seen only in one toe—the second toe. Often, there is a callus or corn over the dorsum of the flexed joint. The condition is often asymptomatic, especially if the hammer toe is flexible or semiflexible. The rigid type of hammer toe is likely to cause the greatest problems.
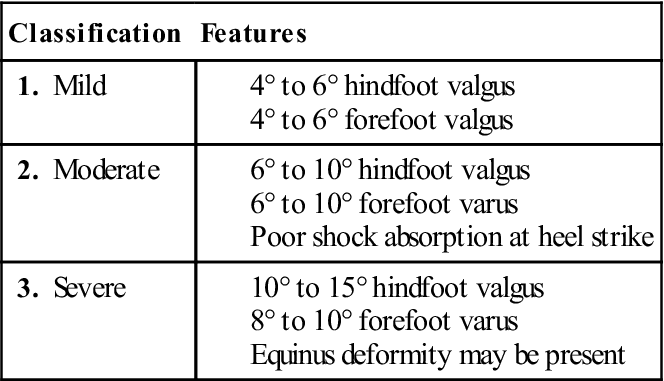
Hindfoot Valgus (Subtalar or Rearfoot Valgus).
This structural deformity involves eversion of the calcaneus when the subtalar joint is in the neutral position. The hindfoot is mobile, which may lead to excessive pronation and limited supination. It may result from genu valgum (knock knees) and may contribute to the appearance of a pes planus foot with the medial longitudinal arch appearing flattened. Because of the increased mobility, it is less likely to cause problems than hindfoot varus. It is often associated with tibia valgus (Figure 13-39, B) and has been associated with posterior tibial tendon insufficiency.54
Hindfoot Varus (Subtalar or Rearfoot Varus).
This structural deviation involves inversion of the calcaneus when the subtalar joint is in the neutral position. The hindfoot is mildly rigid with calcaneal eversion; therefore, pronation is limited. It may contribute to the appearance of a pes cavus foot, making the medial longitudinal arch appear accentuated. It may be the result of tibia varus (genu varum), and, because of the extra subtalar pronation necessary at the beginning of stance, normal supination during early propulsion may be prevented. This deviation can contribute to conditions, such as retrocalcaneal exostosis (pump bumps), shin splints, plantar fasciitis, hamstring strains, and knee and ankle pathology (Figure 13-39, A).25
Mallet Toe.
Mallet toe is associated with a flexion deformity of the distal interphalangeal joint (Figure 13-31, C).50,53 It can occur on any of the four lateral toes. Often, a corn or callus is present over the dorsum of the affected joint. The condition is usually asymptomatic. It is commonly seen with ill-fitting or poorly designed footwear.42
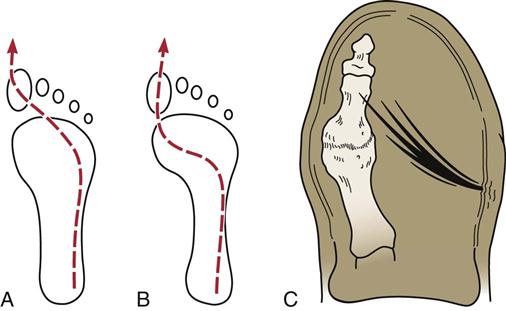
Metatarsus Adductus (Hooked Forefoot).
This deformity is the most common foot deviation in children. It may be seen at birth but often is not noticed until the child begins to stand. The foot appears to be adducted and supinated (kidney shaped with medial deviation), and the hindfoot may or may not be in valgus.55 It may be associated with hip dysplasia. Eighty-five to 90% of cases resolve spontaneously.43
Morton’s (Atavistic or Grecian) Foot.
With a Morton’s foot, the second toe is longer than the first. The length difference may be due to different lengths of the metatarsals (see Figure 13-14). Increased stress is put on this longer toe, and the big toe tends to be hypomobile. There is often hypertrophy of the second metatarsal bone because more stress is put through the second toe. In fact, the second metatarsal can become as large as the first metatarsal. People with this deformity often have difficulty putting on tight-fitting footwear (e.g., skates, ski boots) or dancing (e.g., en pointe in ballet). The different types of feet and their proportional representations in the population are shown in Figure 13-15.
Morton’s Metatarsalgia (Interdigital Neuroma).
Morton’s metatarsalgia (Morton’s neuroma) refers to the formation of an interdigital neuroma as a result of injury to one of the digital nerves (Figure 13-40). Usually, it is the digital nerve between the third and fourth toes, so the examiner must take care to differentially diagnose the condition from a stress fracture of one of the metatarsals in the same area (march fracture). (A stress fracture will be more painful when the bone is palpated and a bone scan would be positive.) Title et al.56 point out that if a Morton’s neuroma is suspected, pressure palpation should be applied on the plantar aspect avoiding counter pressure on the dorsal aspect. Dorsal palpation pain is more likely to be associated with a stress fracture, metatarsophalangeal synovitis, or dorsal neuralgia. While walking or running, the patient is suddenly seized with an agonizing pain on the outer border of the forefoot. The pain is often intermittent, like a cramp, shooting up the side and to the tip of the affected toe or the adjacent two toes. Squeezing the metatarsal bones together elicits pain because of the pressure on the digital nerve. On palpation, pain is more likely to be between the bones rather than on the bone. The condition tends to occur more frequently in women than in men.
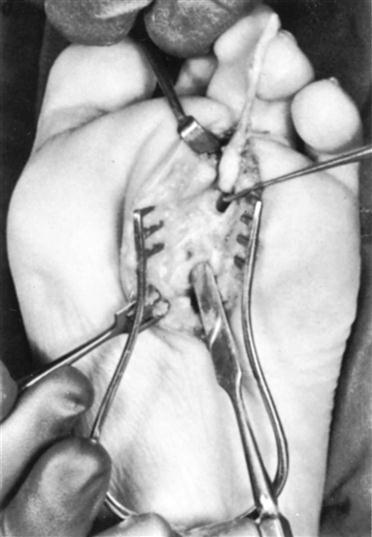
The interdigital nerve to the space between the third and fourth digits has been divided 2 cm above the neuroma and is reflected downward. The plantar digital vessels are shown entering the neuroma. The end of the flat dissector is on the upper margin of the transverse ligament. The end of the probe points to the intermetatarsophalangeal bursa. (From Klenerman L: The foot and its disorders, Boston, 1982, Blackwell Scientific, p. 143.)
Pes Cavus (“Hollow Foot” or Rigid Foot).
A pes cavus may be caused by a congenital problem; a neurological problem, such as spina bifida, poliomyelitis, or Charcot-Marie-Tooth disease; talipes equinovarus; or muscle imbalance. There may also be a genetic factor, because it tends to run in families.
The longitudinal arches are accentuated (Figure 13-41), and the metatarsal heads are lower in relation to the hindfoot so that there is a dropping of the forefoot on the hindfoot at the tarsometatarsal joints (Figure 13-42). The soft tissues of the sole of the foot are abnormally short, which gives the foot a shortened appearance. If the deformity persists, the bones eventually alter their shape, perpetuating the deformity. The heel is normal, at least initially. Claw toes are often associated with the condition because of the dropping of the forefoot combined with the pull of the extensor tendons. The examiner often finds painful callosities beneath the metatarsal heads that are caused by the loss of the metatarsal arch and tenderness along the deformed toes. There is pain in the tarsal region after time because of osteoarthritic changes in these joints.

Note the high medial longitudinal arch, early clawing of the big toe, and the heel in varus. (From Klenerman L: The foot and its disorders, Boston, 1982, Blackwell Scientific, p. 72.)
The longitudinal arches are high on both the medial and lateral aspects so that a lateral longitudinal arch occurs in some severe cases, and the forefoot is thickened and splayed (Table 13-6). The metatarsal heads are prominent on the sole of the foot, and the toes do not touch the ground, even on active or passive movement. This type of deformity leads to a rigid foot with little ability to absorb shock and adapt to stress. People with this deformity have difficulty doing repetitive stress activity (e.g., long-distance running, ballet) and require a cushioning shoe. In severe cases, the cavus foot is often associated with neurological disorders.43
TABLE 13-6
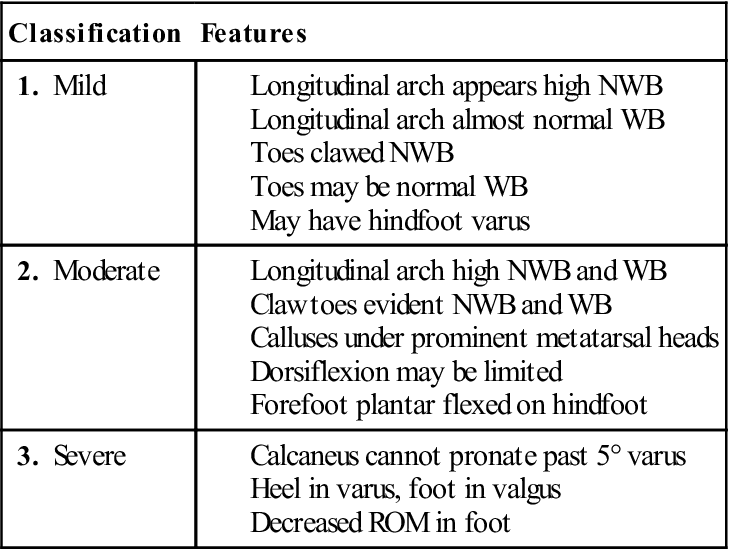
NWB, Non–weight-bearing; ROM, range of motion; WB, weight-bearing.
Pes Planus (Flatfoot or Mobile Foot).
Flatfoot may be congenital, or it may result from trauma, muscle weakness, ligament laxity, dropping of the talar head, paralysis, or a pronated foot. For example, a traumatic flatfoot may follow fracture of the calcaneus. It may also be caused by a postural deformity, such as medial rotation of the hips or medial tibial torsion. It is a relatively common foot deformity that often causes little or no problem. Therefore, the examiner should not necessarily assume that a flat, mobile foot needs to be treated. Because the foot is mobile, patients with flatfoot function well without treatment and often need only a control shoe to avoid problems in prolonged stress situations.
It must be remembered that all infants have flatfeet up to approximately 2 years of age. This appearance in part results from the fat pad in the longitudinal arch and in part from the incomplete formation of the arches. With pes planus, the medial longitudinal arch is reduced so that on standing its borders are close to or in contact with the ground. This results from the hindfoot dropping in relation to the forefoot (see Figure 13-42). If the condition persists into adulthood, it may become a permanent structural deformity, leading to a defect or alteration of the tarsal bones and the talonavicular joints.
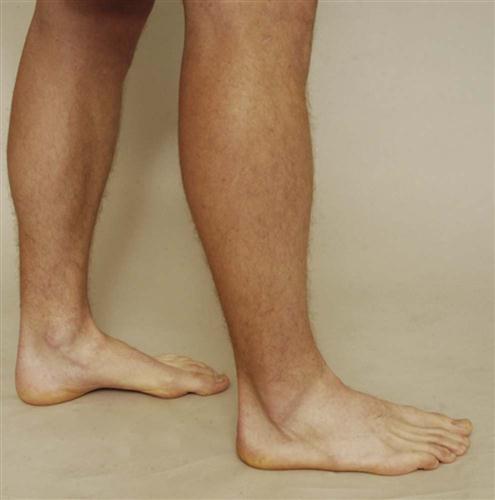
There are two types of flatfoot deformities. The first type (rigid or congenital flatfoot) is relatively rare. The calcaneus is found in a valgus position, whereas the midtarsal region is in pronation. The talus faces medially and downward, and the navicular is displaced dorsally and laterally on the talus. There are accompanying soft-tissue contractures and bony changes. The second type is acquired or flexible flatfoot (Figure 13-43). In this case, the deformity is similar to the rigid flatfoot, but the foot is mobile (Table 13-7); and there are few, if any, soft-tissue contractures and bony changes. It is usually caused by hereditary factors and is sometimes called a hypermobile flatfoot. Flexible flatfoot may result from tibial or femoral torsion, coxa vara, a defect in the subtalar joint, or injury to the posterior tibial tendon.57 If the arch appears when the patient stands on tiptoes, the patient may have a mobile flatfoot. This type of flatfoot seldom needs treatment.
Plantar Flexed First Ray.
This structural deformity occurs when the first ray (big toe) lies lower than the other four metatarsal bones so that the forefoot is everted when the metatarsal bones are aligned. If present congenitally, it is indicative of a cavus foot. In its acquired form, it occurs as compensation for tibia varum (genu varum) with limited calcaneal eversion. This deformity can contribute to the same conditions seen with forefoot valgus.25 The neutral position of the first ray is the position in which the first metatarsal head lies in the same transverse plane as the second through fourth metatarsal heads when they are maximally dorsiflexed.58
Polydactyly.
This developmental anomaly is characterized by the presence of an extra digit or toe (Figure 13-44). It may be seen in isolation or with other anomalies, such as polydactyly of the hands and syndactyly (webbing) of the toes or hands (Figure 13-45). The primary concern with this anomaly is cosmesis.59
Rocker-Bottom Foot.
In the rocker-bottom foot deformity, the forefoot is dorsiflexed on the hindfoot. This results in a “broken midfoot,” so that the medial and longitudinal arches are absent and the foot appears to be bent the wrong way (i.e., convex to the floor instead of the normal concave).
Splay Foot.
This deformity, which is broadening of the forefoot, is often caused by weakness of the intrinsic muscles and associated weakness of the intermetatarsal ligament and dropping of the anterior metatarsal arch.
Turf Toe.
Turf toe is a hyperextension injury (sprain) combined with compressive loading to the metatarsophalangeal joint of the hallux. It can cause a significant functional disability, especially in sports, where the hallux is put under high loads. It is often related to the use of flexible footwear and artificial turf.60–62
Shoes
The examiner looks at the patient’s shoes, both inside and outside, for weight-bearing and wear patterns (Figures 13-46 and 13-47). With the normal foot, the greatest wear on the shoe is beneath the ball of the foot and slightly to the lateral side and the posterolateral aspect of the heel. If shoes are too small or too narrow, they may pinch the feet, causing deformities and affecting normal growth. If shoes are worn out, they offer little support. If shoes are stiff, they limit proper movement of the foot.
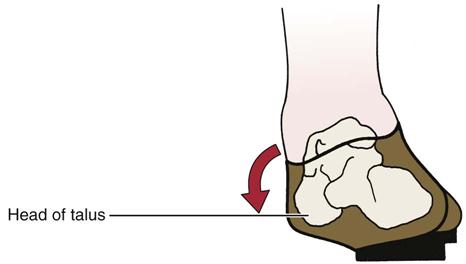
Note the prominence of the talar head.
Platform-type or high-heeled shoes often cause painful knees, because the patient wearing these shoes usually walks with the knees flexed, which may increase the stress on the patella. Continuous wearing of high-heeled shoes may cause the calf muscles to contract and may lead to sore knees and a painful back, because the lumbar spine goes into increased lordotic posture to maintain the center of gravity in its normal position. In addition, these shoes increase the potential for ankle sprains and fractures because a raised center of gravity puts the wearer off balance.
High-heeled and pointed shoes often contribute to hallux valgus, bunions, march fractures, and Morton’s metatarsalgia that may result because the toes are being pushed together. Shoes with a negative heel may lead to hyperextension of the knees and patellofemoral syndrome. High-cut or high-top shoes that cover the medial and lateral malleoli offer more support than low-cut shoes or those that do not cover the malleoli.
Excessive bulging on the medial side of the shoe suggests a valgus or everted foot, whereas excessive bulging on the lateral side suggests an inverted foot. Drop foot resulting from musculature weakness scuffs the toe of the shoe. Oblique forefoot creases in the shoe indicate possible hallux rigidus; absence of forefoot creases indicates no toe-off action during gait.
Examination
As with any assessment, the examiner must compare one side with the other and note any asymmetry. This comparison is necessary because of individual differences among normal people.
Active Movements
The first movements tested during the examination are active, with painful movements being tested last. These movements should be done in both weight-bearing (Figures 13-48 and 13-49) and non–weight-bearing (long leg sitting or supine lying; Figure 13-50) positions, and the examiner should note any differences because foot deformities and deviations in addition to decreased ROM can lead to injury.63 Lindsjo and colleagues advocated testing weight-bearing ROM by putting the test foot on a 30-cm (12-inch) stool for ease of measurement and flexing the knee.64

 Figure 13-48 Active movements (weight-bearing posture).
Figure 13-48 Active movements (weight-bearing posture).A, Plantar flexion. B, Dorsiflexion. C, Supination. D, Pronation. E, Toe extension. F, Toe flexion.
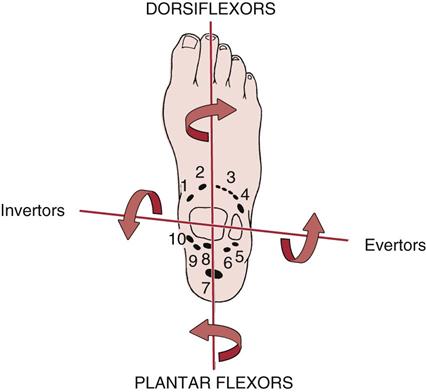
1, Tibialis anterior; 2, extensor hallucis longus; 3, extensor digitorum longus; 4, peroneus tertius; 5, peroneus brevis; 6, peroneus longus; 7, Achilles tendon (soleus and gastrocnemius); 8, flexor hallucis longus; 9, flexor digitorum longus; 10, tibialis posterior.
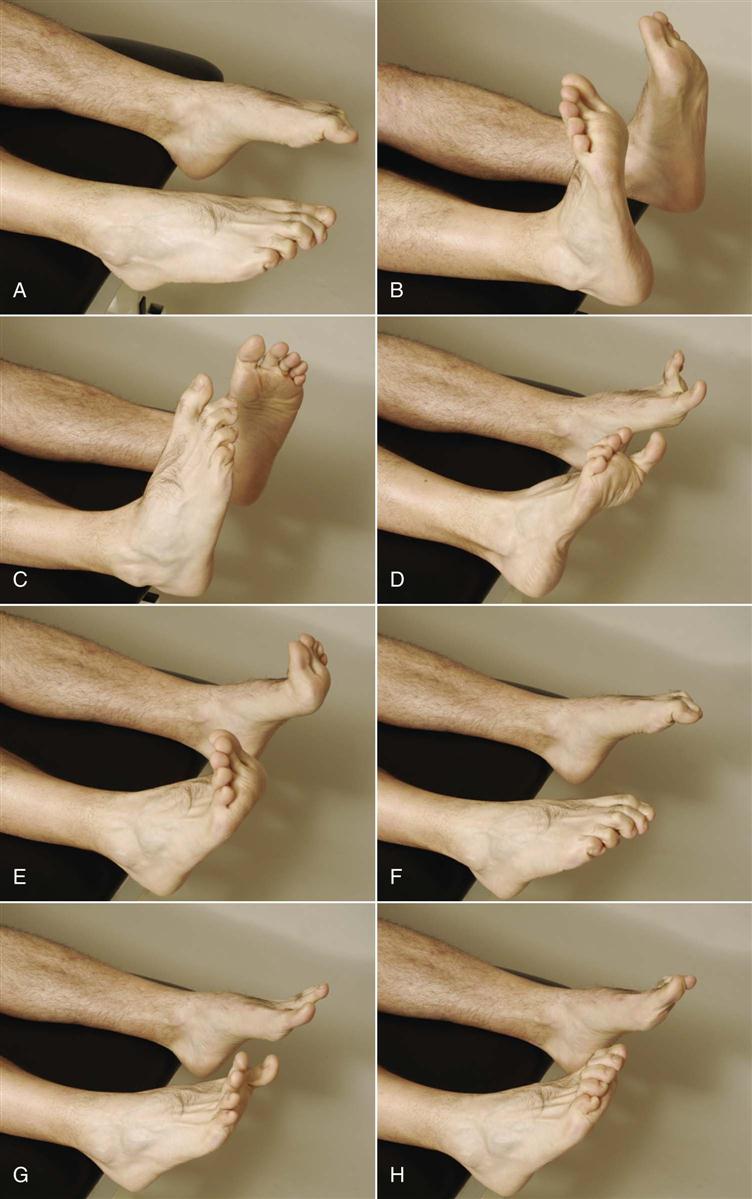
 Figure 13-50 Active movements (non-weight-bearing posture).
Figure 13-50 Active movements (non-weight-bearing posture).A, Plantar flexion. B, Dorsiflexion. C, Supination. D, Pronation. E, Toe extension. F, Toe flexion. G, Toe abduction. H, Toe adduction.
Plantar Flexion
Plantar flexion of the ankle is approximately 50° (see Figure 13-50, A), and the patient’s heel normally inverts when the movement is performed in weight bearing (Figure 13-51). If heel inversion does not occur, the foot is unstable, or there is tibialis posterior weakness or tightness.37,65,66 The tibialis posterior muscle and tendon balance the pull of the peroneal muscles, protect the spring ligament, and invert and stabilize the hindfoot during toe off.67 Pain in the spring ligament as well as the medial midfoot and hindfoot ligaments, hindfoot valgus, plantar flexed talar head, and forefoot abduction should lead the examiner to assessing the tibialis posterior for proper function.37
Dorsiflexion
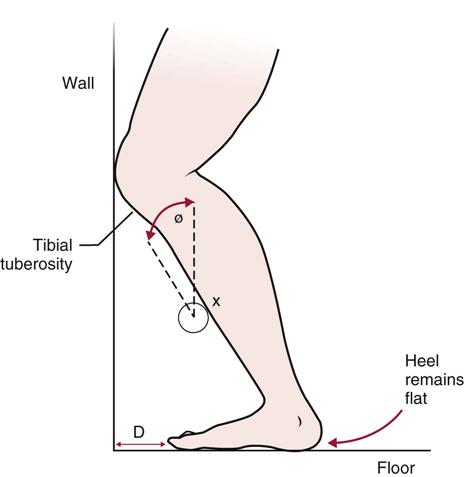
Dorsiflexion of the ankle is usually 20° past the anatomical position (plantigrade), which is with the foot at 90° to the bones of the leg (see Figure 13-50, B). For normal locomotion, 10° of dorsiflexion and 20° to 25° of plantar flexion at the ankle are required. Functional dorsiflexion may be measured by the ankle lunge test ![]() .68,69 For this weight-bearing test, the patient is asked to place one foot perpendicular to a wall and lunge the same knee toward the wall (Figure 13-52, A). The foot is progressively moved away from the wall until the knee barely touches the wall and the foot remains flat on the floor. The distance from the wall to the big toe is measured (Figure 13-52, B). Both sides are compared. If desired, the angle of the tibial shaft to a vertical line can also be measured (Figure 13-53). Differences between sides may be due to a tight Achilles tendon or talocrural restriction.70
.68,69 For this weight-bearing test, the patient is asked to place one foot perpendicular to a wall and lunge the same knee toward the wall (Figure 13-52, A). The foot is progressively moved away from the wall until the knee barely touches the wall and the foot remains flat on the floor. The distance from the wall to the big toe is measured (Figure 13-52, B). Both sides are compared. If desired, the angle of the tibial shaft to a vertical line can also be measured (Figure 13-53). Differences between sides may be due to a tight Achilles tendon or talocrural restriction.70
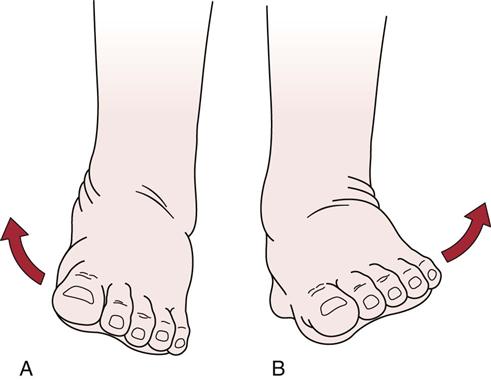
Supination and Pronation
Supination is 45° to 60° and pronation is 15° to 30°, although individuals vary (see Figure 13-50, C and D). It is more important to compare the movement with that of the patient’s normal side (Figures 13-54 and 13-55). Supination combines the movements of inversion, adduction, and plantar flexion; pronation combines the movements of eversion, abduction, and dorsiflexion of the foot and ankle. As the patient does the movement, the examiner should watch for the possibility of subluxation of various tendons. The peroneal tendons are especially prone to subluxation, and their subluxation is evident on eversion (Figure 13-56). If tibialis anterior is weak, supination is affected. If the peronei are weak or the tendons sublux, pronation is affected.
The peroneal tendons pass anterior to the retrofibular sulcus but not anterior to the distal fibula, in contradistinction to traumatic subluxation. (From Kelikian H, Kelikian AS: Disorders of the ankle, Philadelphia, 1985, WB Saunders, p. 765.)
Toe Extension and Flexion
Movement of the toes occurs at the metatarsophalangeal and proximal and distal interphalangeal joints (see Figure 13-50, E and F). Extension of the great toe occurs primarily at the metatarsophalangeal joint (70°); there is minimal or no extension at the interphalangeal joint. For the great toe, 45° flexion occurs at the metatarsophalangeal joint, and 90° occurs at the interphalangeal joint.
For the lateral four toes, extension occurs primarily at the metatarsophalangeal (40°) and distal interphalangeal joints (30°). Extension at the proximal interphalangeal joints is negligible. For the lateral four toes, 40° flexion occurs at the metatarsophalangeal joints, 35° occurs at the proximal interphalangeal joints, and 60° occurs at the distal interphalangeal joints.
Toe Abduction and Adduction
Abduction and adduction of the toes are measured with the second toe as midline. Although the ROM of abduction can be measured, this is not usually done. The common practice is to ask the patient to spread the toes and then bring them back together (see Figure 13-50, G and H). The amount and quality of movement are compared with those of the unaffected side.
If the history has indicated that weight-bearing or non–weight-bearing combined or repetitive movements or sustained postures result in symptoms, these movements should also be tested. The examiner should ask the patient to walk on the toes, heels, and outer and inner borders of the feet. These actions indicate the patient’s muscle power and control and the functional ROM. With a third-degree strain (rupture) of the Achilles tendon, the patient is not able to walk on the toes. Lack of dorsiflexion makes it difficult for the patient to walk on the heels. When the patient walks on the inner or outer borders of the feet, pain and difficulty are experienced in the presence of a subtalar lesion.
The examiner should also check the efficiency of the toes. Are the toes straight and parallel? Is the patient able to flex, extend, adduct, and abduct the toes? The toes have a primarily ambulatory function, although, with training, they can develop a prehensile function. The toes extend the weight-bearing area forward and, by so doing, reduce the load on the metatarsal heads. The great toe also has a primary function of pushing off during gait.
When assessing the active movements, the examiner must remember that peripheral nerve injuries may alter the pattern of movement. For example, the common peroneal nerve may be injured, because it winds around the head of the fibula, resulting in altered nerve conduction to the peroneus longus and brevis muscles (superficial peroneal nerve) or the tibialis anterior, extensor digitorum longus, and extensor hallucis longus (deep peroneal nerve).71 In such cases, the movements controlled by these muscles are altered. In addition, there are sensory changes that must be noted.
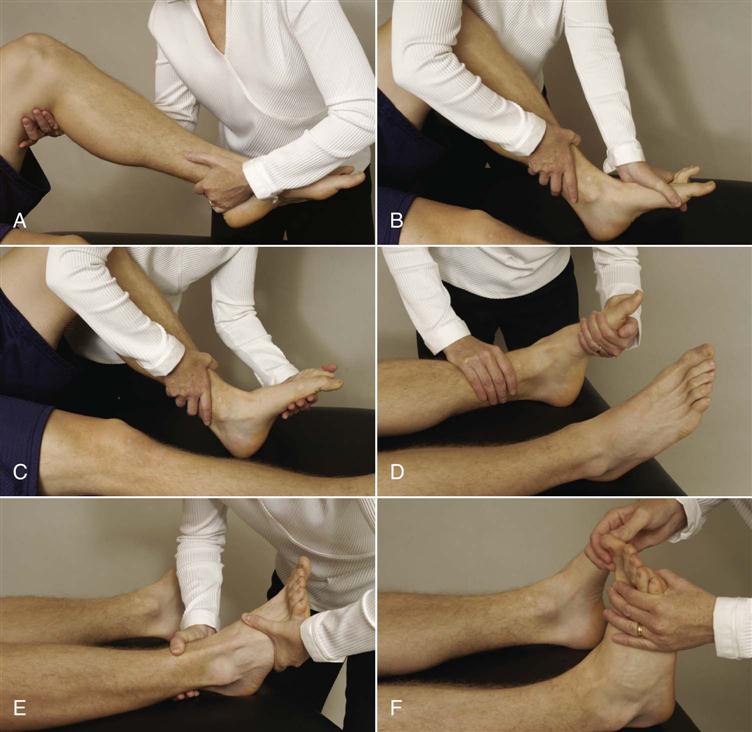
Passive Movements
The passive movements of the lower leg, ankle, and foot are performed with the patient in a non–weight-bearing position (Figure 13-57). As with other joints, if the active ROM is full, overpressure can be applied to test end feel during the active, non–weight-bearing movements to negate the need to do passive movements. Each movement should be carefully checked, especially if deformities or asymmetries have been noticed during the observation. These deformities or asymmetries may cause problems in other areas of the lower kinetic chain. For example, limited dorsiflexion or tight heel cords may lead to anterior knee pain or ankle injuries.72 Because the gastrocnemius is a two-joint muscle, dorsiflexion should be tested with the knee straight to test this muscles for tightness. Testing with the knee bent to 90°, isolates soleus. Stovitz and Coetzee recommended testing the Achilles tendon and its associated muscles with the subtalar joint in neutral with a lateral force applied to the talar neck to lock the foot during testing.66 This eliminates calcaneal eversion or forefoot dorsiflexion from contributing to an apparent normal Achilles tendon. There is greater mobility and flexibility in the Achilles tendon in a baby or young child than there is in an adult. For example, in the newborn, the foot can readily be dorsiflexed passively so that the toes and dorsum of the foot touch the skin over the tibia. In the adult, however, dorsiflexion is limited to 20° more than plantigrade. If the patient can only attain plantigrade (90°), then the gastrocnemius or soleus is tight. If gastrocnemius is tight, the ankle ROM is limited with the knee extended. If soleus is tight, the ankle ROM is limited with the knee flexed. Conversely, increased ankle dorsiflexion (Matles test ![]() ), compared to the other side, may indicate a torn achilles tendon, especially if combined with decreased plantar flexion strength.73 If tibialis posterior is tight, supination of the foot is limited.
), compared to the other side, may indicate a torn achilles tendon, especially if combined with decreased plantar flexion strength.73 If tibialis posterior is tight, supination of the foot is limited.

A, Plantar flexion. B, Dorsiflexion. C, Inversion. D, Eversion. E, Abduction and adduction. F, Toe flexion and extension. G, Toe abduction.
Some movements may be tested in combination to more closely approximate what occurs functionally. For example, instead of testing plantar flexion, adduction, and inversion separately, supination, as a combined movement, may be tested. Similarly, pronation may be tested as a combined movement, instead of dorsiflexion, abduction, and eversion.
During passive movements of the ankle and foot, any capsular patterns should be noted. The capsular pattern of the talocrural joint is more limitation of plantar flexion than of dorsiflexion; the subtalar joint capsular pattern shows more limitation of varus range than of valgus ROM. The midtarsal joint capsular pattern is dorsiflexion most limited, followed by plantar flexion, adduction, and medial rotation. The first metatarsophalangeal joint has a capsular pattern in which extension is most limited, followed by flexion. The pattern for the second through fifth metatarsophalangeal joints is variable. The capsular pattern of the interphalangeal joints is flexion most limited, followed by extension.
Resisted Isometric Movements
The resisted isometric movements are performed to test the contractile tissue around the foot, ankle, and lower leg. The patient is in the sitting or supine lying position, and the patient’s foot is placed in the anatomical position (plantigrade or 90°; Figure 13-58). Table 13-8 shows the muscles acting over the foot and ankle. Strength results may very depending on age and sex.74
A, Knee flexion. B, Dorsiflexion. C, Plantar flexion. D, Supination. E, Pronation. F, Toe extension.
TABLE 13-8
| Action | Muscles Acting | Nerve Supply | Nerve Root Derivation |
| Plantar flexion (flexion) of ankle | 1. Gastocnemius* | Tibial | S1, S2 |
| 2. Soleus* | Tibial | S1, S2 | |
| 3. Plantaris | Tibial | S1, S2 | |
| 4. Flexor digitorum longus | Tibial | S2, S3 | |
| 5. Peroneus longus | Superficial peroneal | L5, S1, S2 | |
| 6. Peroneus brevis | Superficial peroneal | L5, S1, S2 | |
| 7. Flexor hallucis longus | Tibial | S2, S3 | |
| 8. Tibialis posterior | Tibial | L4, L5 | |
| Dorsiflexion (extension) of ankle | 1. Tibialis anterior | Deep peroneal | L4, L5 |
| 2. Extensor digitorum longus | Deep peroneal | L5, S1 | |
| 3. Extensor hallucis longus | Deep peroneal | L5, S1 | |
| 4. Peroneus tertius | Deep peroneal | L5, S1 | |
| Inversion | 1. Tibialis posterior | Tibial | L4, L5 |
| 2. Flexor digitorum longus | Tibial | S2, S3 | |
| 3. Flexor hallucis longus | Tibial | S2, S3 | |
| 4. Tibialis anterior | Deep peroneal | L4, L5 | |
| 5. Extensor hallucis longus | Deep peroneal | L5, S1 | |
| Eversion | 1. Peroneus longus | Superficial peroneal | L5, S1, S2 |
| 2. Peroneus brevis | Superficial peroneal | L5, S1, S2 | |
| 3. Peroneus tertius | Deep peroneal | L5, S1 | |
| 4. Extensor digitorum longus | Deep peroneal | L5, S1 | |
| Flexion of toes | 1. Flexor digitorum longus | Tibial | S2, S3 |
| 2. Flexor hallucis longus | Tibial | S2, S3 | |
| 3. Flexor digitorum brevis | Tibial (medial plantar branch) | S2, S3 | |
| 4. Flexor hallucis brevis | Tibial (medial plantar branch) | S2, S3 | |
| 5. Flexor accessorius (Quadratus plantae) | Tibial (lateral plantar branch) | S2, S3 | |
| 6. Interossei | Tibial (lateral plantar branch) | S2, S3 | |
| 7. Flexor digiti minimi brevis | Tibial (lateral plantar branch) | S2, S3 | |
| 8. Lumbricals (metatarsophalangeal joints) | Tibial (first by medial plantar branch; second through fourth by lateral plantar branch) | S2, S3 | |
| Extension of toes | 1. Extensor digitorum longus | Deep peroneal | L5, S1 |
| 2. Extensor hallucis longus | Deep peroneal | L5, S1 | |
| 3. Extensor digitorum brevis | Deep peroneal (lateral terminal branch) | S1, S2 | |
| 4. Lumbricals (interphalangeal joints) | Tibial (first by medial plantar branch; second through fourth by lateral plantar branch) | S2, S3 | |
| Abduction of toes | 1. Abductor hallucis | Tibial (medial plantar branch) | S2, S3 |
| 2. Abductor digiti minimi | Tibial (lateral plantar branch) | S2, S3 | |
| 3. Dorsal interossei | Tibial (lateral plantar branch) | S2, S3 | |
| Adduction of toes | 4. Adductor hallucis | Tibial (lateral plantar branch) | S2, S3 |
| 5. Plantar interossei | Tibial (lateral plantar branch) | S2, S3 |
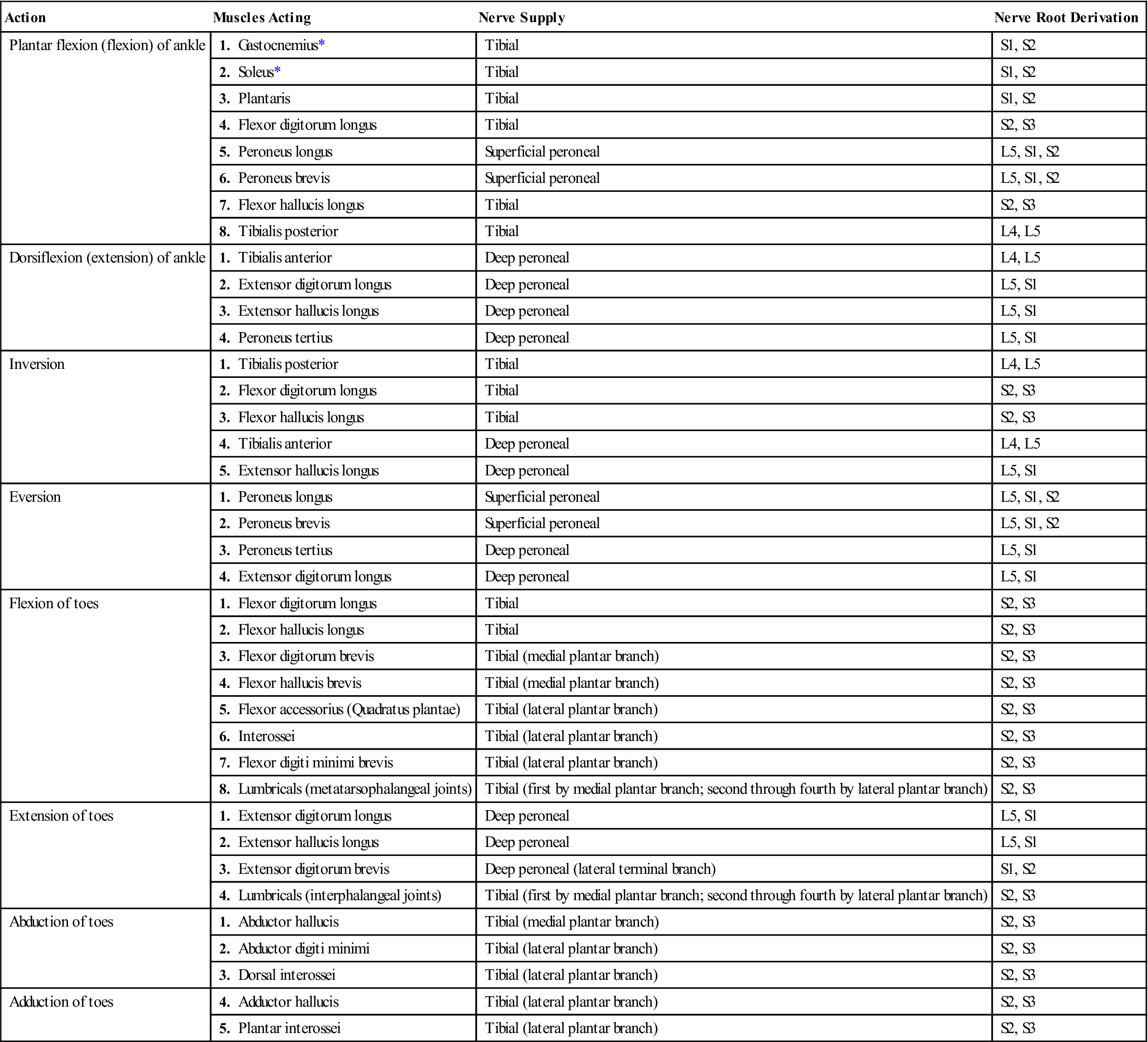
*The gastrocnemius and soleus muscles are sometimes grouped together as the triceps surae muscles.
Dorsiflexion is sometimes tested with the patient’s hip flexed to 45° and the knee flexed to 90°, as illustrated in Figure 13-58, B. Testing with the patient in this position enables the examiner to exert a greater isometric force. Resisted isometric knee flexion must be performed, because the triceps surae (gastrocnemius and soleus muscles together) act on the knee as well as on the ankle and foot.
If the history has indicated that eccentric, concentric, or econcentric muscle action has caused symptoms, these movements should also be tested, but only after the isometric tests have been completed.
Functional Assessment
If the patient is able to do the movements already described with little difficulty, functional tests may be performed to see whether these sequential activities produce pain or other symptoms. Full ROM is often not necessary for the patient to lead a functional life.
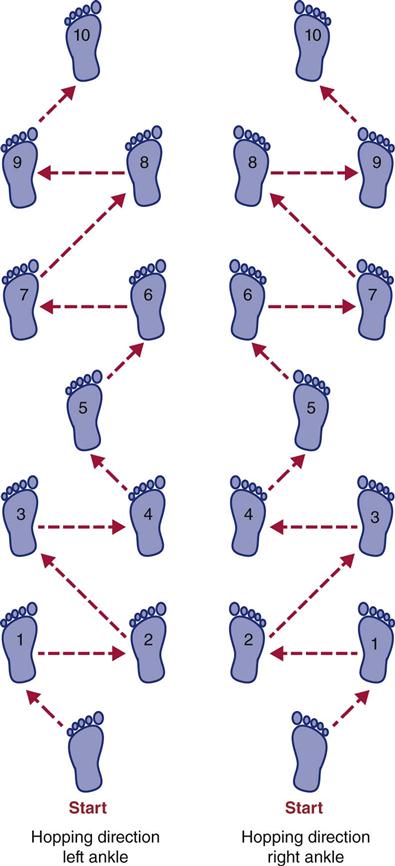
These activities, which are examples only, must be geared to the individual patient. Older patients should not be expected to do some of the activities unless they have been doing these or similar ones in the recent past (Table 13-9). Because the functional tests place a stress on the other lower limb joints (e.g., knee, hip, sacroiliac, lumbar joints), the examiner must ensure that these joints exhibit no pathology before all of the tests are completed. On the other hand, functional tests for other joints in the lower limb (e.g., hop test for the knee) may not be sensitive enough or deficits may be too small to test ankle function.75,76 However, Wikstrom et al.77 felt a modified hop test (jump test) was an effective way to determine functional ankle instability. Eechaute et al.78 likewise, found a multiple hop test ![]() (Figure 13-59) to be a reliable functional test. The test involves standing on two feet, jumping forward half the height of the patient’s vertical jump and landing on one leg (good leg first).
(Figure 13-59) to be a reliable functional test. The test involves standing on two feet, jumping forward half the height of the patient’s vertical jump and landing on one leg (good leg first).
TABLE 13-9
Functional Testing of the Foot and Ankle
| Starting Position | Action | Functional Test |
| Standing on one leg* | Lift toes and forefeet off ground (dorsiflexion) | 10 to 15 Repetitions: Functional |
| 5 to 9 Repetitions: Functionally fair | ||
| 1 to 4 Repetitions: Functionally poor | ||
| 0 Repetitions: Nonfunctional | ||
| Standing on one leg* | Lift heels off ground (plantar flexion) | 10 to 15 Repetitions: Functional |
| 5 to 9 Repetitions: Functionally fair | ||
| 1 to 4 Repetitions: Functionally poor | ||
| 0 Repetitions: Nonfunctional | ||
| Standing on one leg* | Lift lateral aspect of foot off ground (ankle eversion) | 5 to 6 Repetitions: Functional |
| 3 to 4 Repetitions: Functionally fair | ||
| 1 to 2 Repetitions: Functionally poor | ||
| 0 Repetitions: Nonfunctional | ||
| Standing on one leg* | Lift medial aspect of foot off ground (ankle inversion) | 5 to 6 Repetitions: Functional |
| 3 to 4 Repetitions: Functionally fair | ||
| 1 to 2 Repetitions: Functionally poor | ||
| 0 Repetitions: Nonfunctional | ||
| Seated | Pull small towel up under toes or pick up and release small object (i.e., pencil, marble, cottonball) (toe flexion) | 10 to 15 Repetitions: Functional |
| 5 to 9 Repetitions: Functionally fair | ||
| 1 to 4 Repetitions: Functionally poor | ||
| 0 Repetitions: Nonfunctional | ||
| Seated | Lift toes off ground (toe extension) | 10 to 15 Repetitions: Functional |
| 5 to 9 Repetitions: Functionally fair | ||
| 1 to 4 Repetitions: Functionally poor | ||
| 0 Repetitions: Nonfunctional |
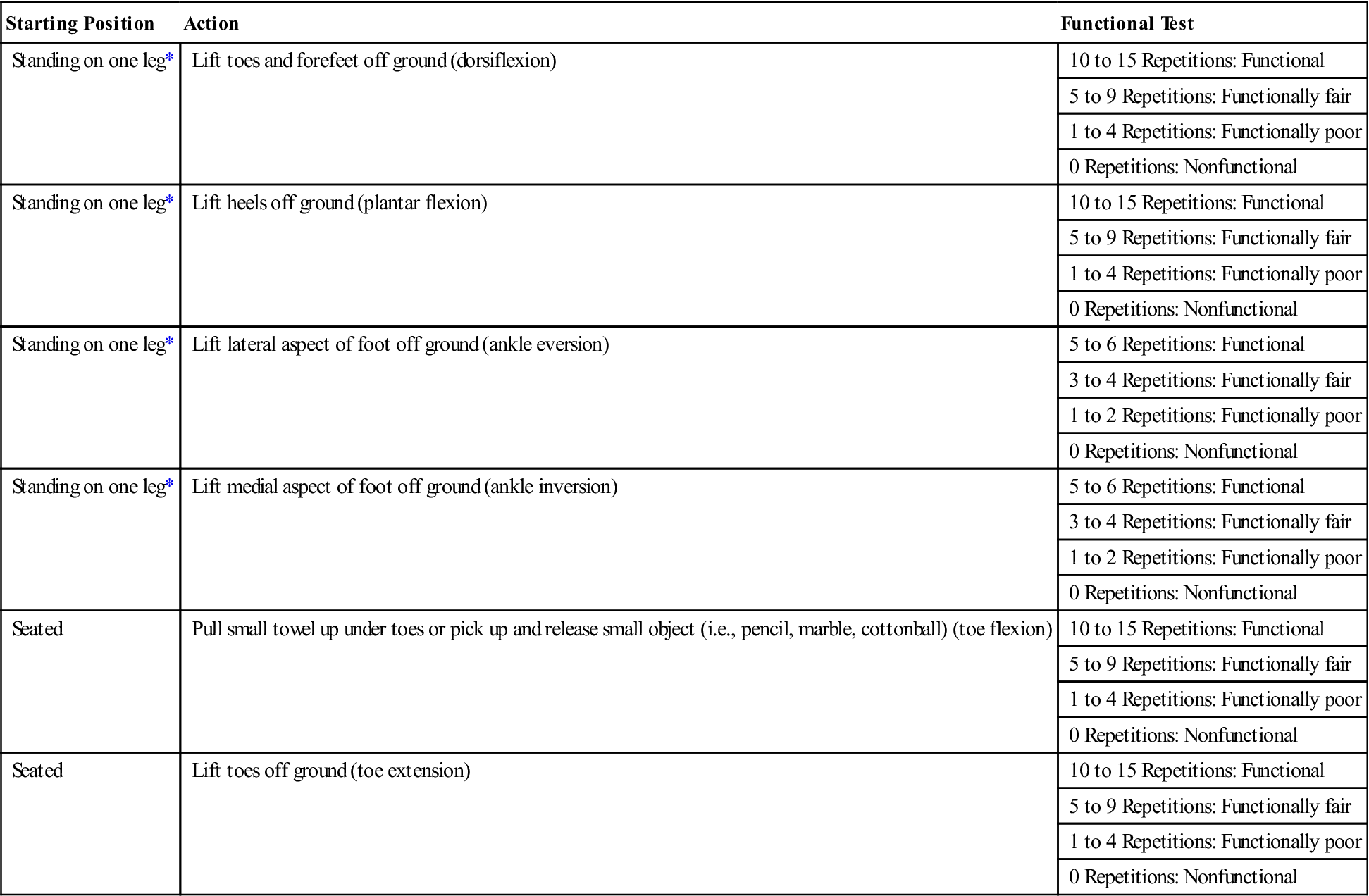
*Hand may hold something for balance only.
Data from Palmer ML, Epler M: Clinical assessment procedures in physical therapy, Philadelphia, 1990, JB Lippincott, pp. 308–310.
Conditions, such as vascular intermittent claudication and anterior compartment syndrome, that occur within a specific time frame must also be considered in an assessment and when considering function.79,80
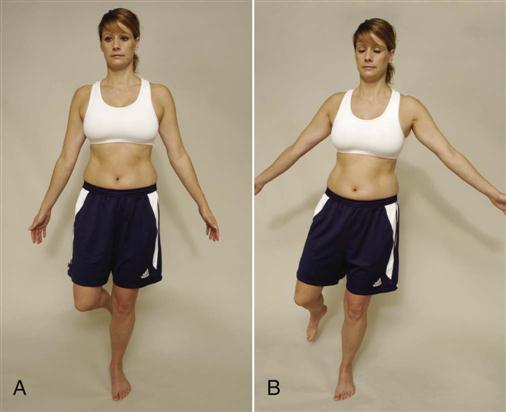
Balance and proprioception are tested by asking the patient to stand on the unaffected leg and then on the affected leg, first with the eyes open and then with the eyes closed. Any differences in balance time or difficulty in balancing give an idea of proprioceptive ability, especially differences that occurred when the patient’s eyes were closed (Figure 13-60).81
Kaikkonen and colleagues82 developed a numerical scoring system to evaluate functional outcome after ankle injury (Table 13-10). The Ankle Joint Functional Assessment Tool (AJFAT) (Figure 13-61), the Foot and Ankle Ability Measure (FAAM) (Figure 13-62), the Foot and Ankle Outcome Score (FAOS) (Figure 13-63), and the Foot Functional Index (FFI) (Figure 13-64),12,83–87 which was developed for an elderly outpatient population, are two other functional tests. Other scales have been developed for specific pathologies (e.g., fractures, osteoarthritis) about the ankle or can be applied to injuries in any part of the lower limb (e.g., Lower Extremity Function Scale (LEF) scale; see Chapter 11).88–98
TABLE 13-10
Scoring Scale for Subjective and Functional Follow-Up Evaluation after Ankle Injury*
| I | Subjective Assessment of the Injured Ankle† | |
| No symptoms of any kind | 15 | |
| Mild symptoms | 10 | |
| Moderate symptoms | 5 | |
| Severe symptoms | 0 | |
| II | Can You Walk Normally? | |
| Yes | 15 | |
| No | 0 | |
| III | Can You Run Normally? | |
| Yes | 10 | |
| No | 0 | |
| IV | Climbing Down Stairs‡ | |
| Less than 18 seconds | 10 | |
| 18 to 20 seconds | 5 | |
| Longer than 20 seconds | 0 | |
| V | Rising on Heels with Injured Leg | |
| More than 40 times | 10 | |
| 30 to 39 times | 5 | |
| Fewer than 30 times | 0 | |
| VI | Rising on Toes with Injured Leg | |
| More than 40 times | 10 | |
| 30 to 39 times | 5 | |
| Fewer than 30 times | 0 | |
| VII | Single-Limbed Stance with Injured Leg§ | |
| Longer than 55 seconds | 10 | |
| 50 to 55 seconds | 5 | |
| Less than 50 seconds | 0 | |
| VIII | Laxity of the Ankle Joints (ADS) | |
| Stable (≤ 5 mm) | 10 | |
| Moderate instability (6 to 10 mm) | 5 | |
| Severe instability (> 10 mm) | 0 | |
| IX | Dorsiflexion Range of Motion, Injured Leg | |
| ≥ 10° | 10 | |
| 5° to 9° | 5 | |
| < 5° | 0 |
*Total: Excellent, 85–100; good, 70–80; fair, 55–65; poor, ≤ 50.
†Pain, swelling, stiffness, tenderness, or giving way during activity (mild, only one of these symptoms is present; moderate, two to three of these symptoms are present; severe, four or more of these symptoms are present).
‡Two levels of staircase (length, 12 m) with 44 steps (height, 13 cm; depth, 22 cm).
§On square beam (10 cm × 10 cm × 30 cm).
From Kaikkonen A, et al: A performance test protocol and scoring scale for the evaluation of ankle injuries. Am J Sports Med 22:465, 1994.
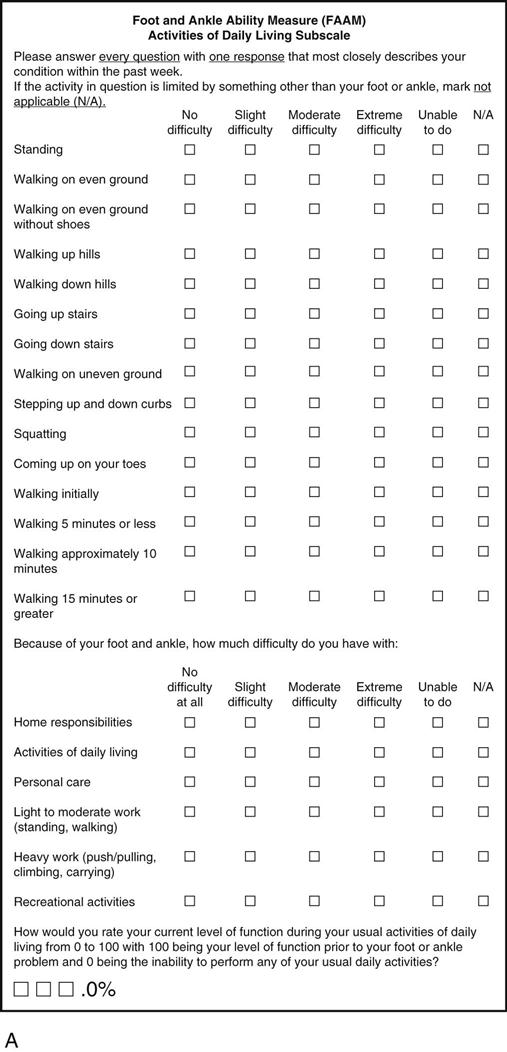
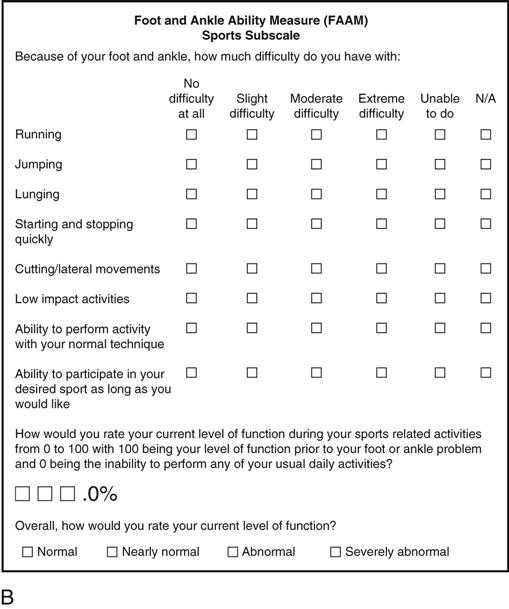
A, Activities of daily living subscale. B, Sports subscale. (From Martin RL, Irrgang JJ, Burdett RG, et al: Evidence of validity for the foot and ankle ability measure [FAAM]. Foot Ankle Int 26[11]:982–983, 2005.)
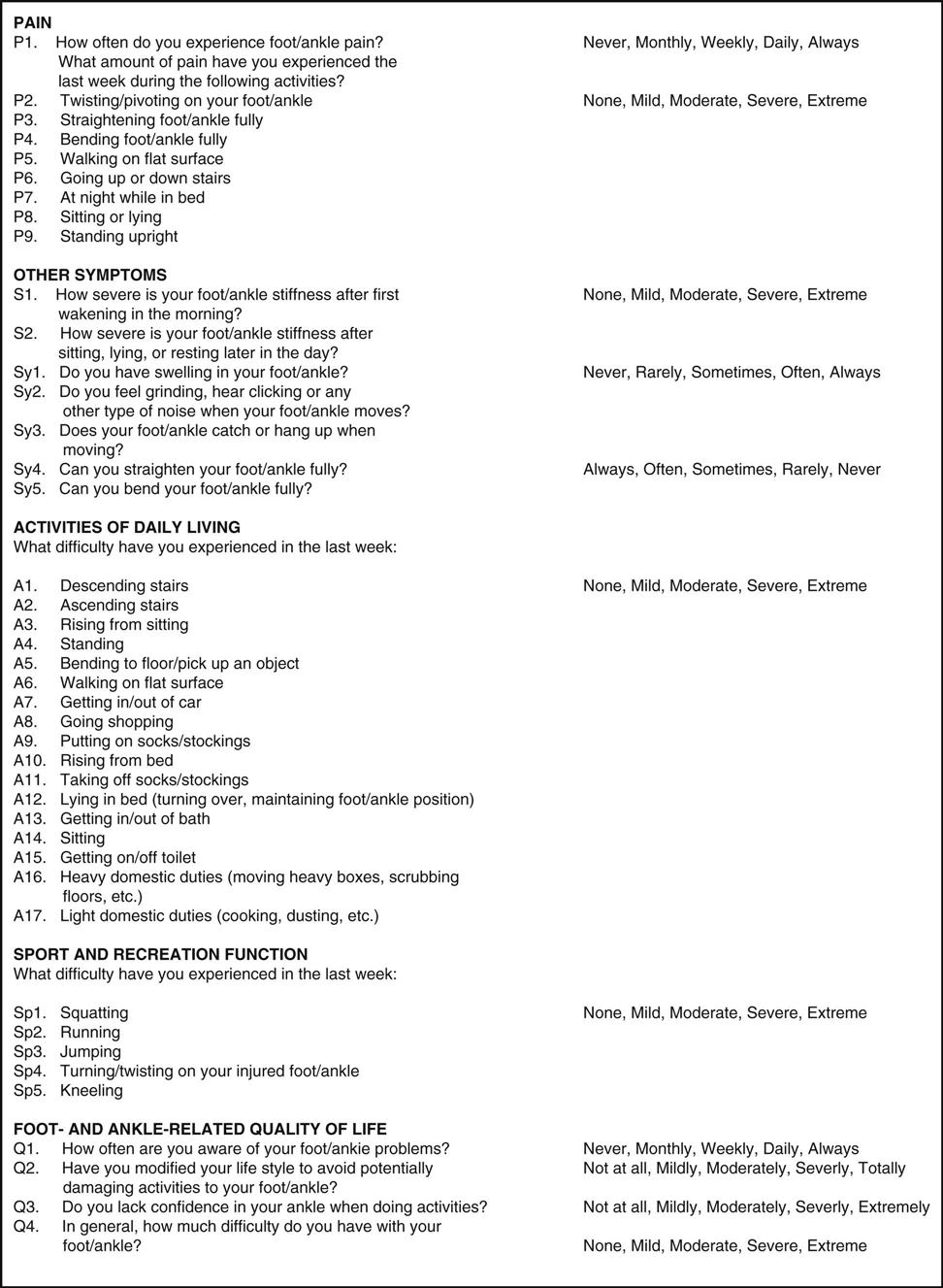
The 42 FAOS items arranged in the five subscales: 1) pain, 2) other symptoms, 3) activities of daily living, 4) sport and recreation function, and 5) foot- and ankle-related quality of life. The five answer options are given after each item. In cases where several following items have identical answer options, the answer options are only given for the first item. (Modified from Roos EM, Brandsson S, Karlsson J: Validation of the foot and ankle outcome scure for ankle ligament reconstruction. Foot Ankle Int 22[10]:790, 2001.)
Special Tests
When assessing the lower leg, ankle, and foot, it is important to always assess the neutral position of the talus in both weight-bearing and non–weight-bearing situations. This will help the examiner to differentiate functional from structural deformities. Other tests that should be carried out include alignment, functional leg length, and tibial torsion tests. Of the other tests, only those that the examiner wishes to use as confirming tests need be performed. Special tests should never be used in isolation but can be used to confirm clinical findings.
For the reader who would like to review them, the reliability, validity, specificity, sensitivity, and odds ratios of some of the special tests used in the lower leg, ankle and foot are available on the Evolve website.
APPENDIX 13-1
| ANKLE CIRCUMFERENCE |
| Reliability |
| ANKLE DORSIFLEXION LUNGE |
| Reliability |
| ANKLE FLEXIBILITY USING LUNGE TEST |
| Reliability |
| ANKLE JOINT POSITION SENSE |
| Reliability |
| ANKLE METER (ANTERIOR DRAWER) |
| Validity |
| ANKLE STRENGTH |
| Reliability |
| ANTERIOR DRAWER TEST | ||
| Reliability | Specificity | Sensitivity |
| ARCH INDEX | |
| Reliability | Validity |
| BRANNOCK DEVICE | |
| Reliability | Validity |
| CALF HEEL RAISES |
| Reliability |
| CHRONIC ANKLE INSTABILITY SCALE (CAIS) |
| Reliability |
| CROSS SIX-METER HOP FOR TIME |
| Reliability |
| CUMBERLAND ANKLE INSTABILITY TOOL (CAIT) | |||
| Reliability | Validity | Specificity | Sensitivity |
| DERIFIELD-THOMPSON TEST |
| Reliability |
| DISTAL TIBIOFIBULAR COMPRESSION TEST |
| Reliability |
| DORSUM HEIGHT | |
| Reliability | Validity |
| DYNAMIC ANTERIOR ANKLE TESTER |
| Reliability |
| EMC DEVICE | |
| Reliability | Validity |
| EQUINOMETER |
| Reliability |
| EXTERNAL ROTATION STRESS TEST |
| Reliability |
| FIGURE-OF-EIGHT METHOD (FOR EDEMA) |
| Reliability |
| FIGURE-OF-EIGHT-20 METHOD | |
| Reliability | Validity |
| FOOT AND ANKLE DISABILITY INDEX (FADI) | ||
| Reliability | Validity | Responsiveness |
| FOOT AND ANKLE OUTCOME SCORE (FAOS) | |
| Reliability | Validity |