Livedo reticularis
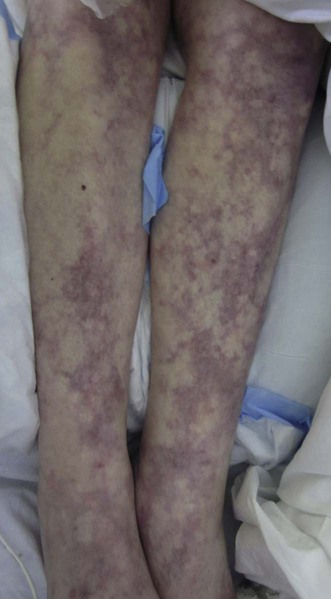
Livedo reticularis (LR) is the net-like mottled violaceous discoloration of the skin secondary to dilatation and stagnation of blood within dermal capillaries. The unaffected normal colored islands of skin are the areas where blood supply is sufficient; in the network areas the supply is insufficient. This commonly occurs on the legs, arms, and trunk, but can be diffuse, and is more pronounced following exposure to cold. LR can be physiological (cutis marmorata), can occur as a primary phenomenon (idiopathic LR) or secondary to a number of diseases that cause dermal vessel wall thickening and/or lumen occlusion such as systemic lupus erythematosus, polyarteritis nodosa, anti-phospholipid syndrome (Chapter 16), cryoglobulinemia, oxolosis, cholesterol emboli, underlying malignancy (as a paraneoplastic phenomenon), and medications. Idiopathic LR may be congenital (cutis marmorata telangiectatica congenita), or associated with painful ulcers (see livedoid vasculitis chapter 134), or with cerebrovascular involvement (Sneddon syndrome).
Specific investigations
Second-line therapies
Third-line therapies








 Aspirin
Aspirin Corticosteroids
Corticosteroids Psoralen plus UVA (PUVA)
Psoralen plus UVA (PUVA) Pentoxifylline + methylprednisolone
Pentoxifylline + methylprednisolone Simvastatin
Simvastatin Withdrawal of causative medications (minocycline or interferon-α2b)
Withdrawal of causative medications (minocycline or interferon-α2b)