3
Lids, Lashes, and Lacrimal System
Eyelid Trauma
Eyelid trauma must be evaluated thoroughly, because seemingly trivial trauma may threaten the viability of the globe. Embedded foreign bodies, incomplete eyelid closure, and lacrimal system damage can all have lasting effects beyond any obvious cosmetic consequences. Trauma can be blunt or sharp, with common examples including fist, motor vehicle accidents, or athletic injury. Ominous mechanism of injury, orbital signs, or massive periocular injury may warrant orbital evaluation including computed tomography (CT) scan.
Contusion
Bruising of eyelid with edema and ecchymosis, usually secondary to blunt injury. Hematomas are often not discrete but infiltrative, involving multiple layers. Unless there is a focal collection of blood, hematomas cannot be effectively evacuated surgically, so the goal of treatment is to reduce further bleeding. Posterior extension into the orbit should be evaluated and, when present, managed accordingly. Ocular involvement is common; traumatic ptosis may occur (mechanical from edema and hematoma, or direct levator injury) and can take up to 6 months to resolve. Usually excellent prognosis if no ocular or bony injuries.
• Cold compresses for up to 45 minutes per hour while awake for 24–48 hours.
• Rule out and treat open globe (see Chapter 4) or other associated ocular trauma.
• Preseptal hematoma (absent orbital signs) is not an indication for canthotomy. Orbital compartment syndrome does not result from preseptal edema /hemorrhage.
Abrasion
Superficial abrasions or mild dermal epithelial abrasions usually heal by secondary intention; rarely require skin grafting.
Avulsion
Tearing or shearing injury to the eyelid resulting in partial or complete severance of eyelid tissue. Surgical repair of eyelid defect depends upon the degree of tissue loss and damage; entirely avulsed remnant should be sought and surgically replaced. Lid-sharing procedures should be avoided in young children owing to the risk of occlusion amblyopia.
When tissue loss is encountered, the approach is individually tailored. Factors such as horizontal eyelid laxity are considered in procedure selection. For example, in an older patient with advanced involutional changes, a defect of up to 30% might be repaired with direct closure, whereas in a younger patient a defect as small as 10% might not be amenable to direct closure without cantholysis. Below are some general treatment guidelines based on defect size.
Upper Lid Defects
• Small (< 33%): Direct closure with or without lateral canthotomy and superior cantholysis.
• Moderate (33–50%): Tenzel semicircular flap advancement, or adjacent tarsoconjunctival flap and full-thickness skin graft.
• Large (> 50%): Lower eyelid bridge flap reconstruction (Cutler–Beard procedure), free tarsoconjunctival graft and skin flap, median forehead flap, or full-thickness lower eyelid switch flap advancement.
Lower Lid Defects
• Small (< 33%): Direct closure with or without lateral canthotomy and inferior cantholysis.
• Moderate (33–50%): Tenzel semicircular flap advancement, or full adjacent tarsoconjunctival flap and full-thickness skin graft.
• Large (> 50%): Upper eyelid tarsoconjunctival pedicle flap with full-thickness skin graft (Hughes procedure), free tarsoconjunctival graft and skin flap, Mustarde’s rotational cheek flap, or anterior lamella reconstruction with retroauricular free skin graft or skin flap advancement.
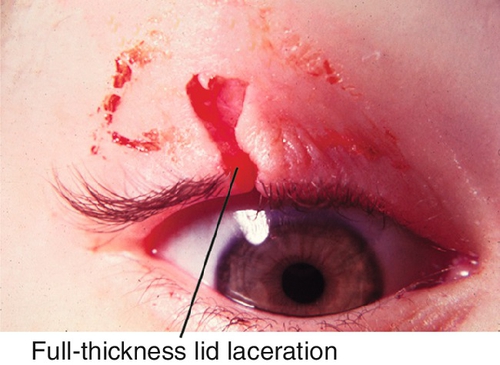
Laceration
Cut in the eyelid involving skin and deeper structures (muscle and fat), usually due to penetrating trauma. Lid lacerations are divided into: (1) no lid margin involvement, (2) lid margin involvement, and (3) canthal angle involvement (tendon and lacrimal gland system). Early, clean wounds usually are repaired successfully but can be complicated by lid notching, entropion, ectropion, or cicatrix; dirty wounds are also at risk for infection.
Lacerations involving the canaliculus (tear duct) at the nasal lid margin between the punctum and the medial canthus of either eyelid can result from a number of mechanisms. Penetrating injury such as that occurring with a dog bite may involve the canaliculus directly. Alternately, they often result from shearing at the eyelid’s weakest point. This may occur in conjunction with lacerations located more laterally on the eyelid and due to their relatively small size are often overlooked. They can be identified on slit-lamp examination of the medial eyelid and confirmed with probing and irrigation. Prognosis is good if repaired early over a stent.
• Fat prolapse into wound suggests orbital septum violation.
• For dirty wounds, systemic antibiotic (dicloxacillin 250–500 mg po qid or cephalexin 250–500 mg po qid for 7–10 days; consider penicillin V 500 mg po qid for animal or human bites).
• Surgical repair of eyelid laceration not involving lid margin: The area around the wound is infiltrated with 2% lidocaine with epinephrine 1 : 100,000. The area is prepped and draped using povidone-iodine (Betadine) solution. The wound is inspected carefully for the presence of foreign bodies. Deep portions are probed to the base of the wound and any septal penetration noted. (Wounds involving levator muscle or levator aponeurosis require layered closure, usually with an extended incision along the major lid crease, and external repair.) Copiously irrigate with saline or bacitracin solution. All tissue should be preserved if possible; only severely necrotic tissue must be excised. Horizontal or arcuate wounds oriented along orbicularis typically are closed in a single layer that includes skin only; gaping wounds or wounds that are oriented transverse to orbicularis are closed in two layers. 6-0 polyglactin interrupted, buried sutures are used to close orbicularis; skin can be closed separately. Some advocate interrupted sutures, whereas others prefer a running stitch. If permanent sutures are used, such as a 6-0 prolene or nylon, they should be removed 5 or 6 days later. Alternatively, an absorbable suture (6-0 fast-absorbing gut) can be used. This is particularly advantageous in children in whom suture removal is challenging or in patients felt unlikely to reliably return for suture removal. Topical and, in most cases of trauma, systemic antibiotics should be prescribed.
• Surgical repair of eyelid laceration involving lid margin, sparing canaliculus: The area around the wound is infiltrated with 2% lidocaine with epinephrine 1 : 100,000. The area is prepped and draped using povidone-iodine (Betadine) solution. The wound is inspected carefully for the presence of foreign bodies. Canalicular involvement is assessed via lacrimal probing and irrigation. All tissue should be preserved, if possible; only severely necrotic tissue must be excised. The lid margin is reapproximated using two to three interrupted 6-0 nylon or 7-0 Vicryl sutures. The initial suture is passed through the meibomian gland orifices, usually in a vertical mattress fashion, to align the tarsus, with one to two additional interrupted sutures to align the lash line. For each suture, it is important that the bites on the two sides are equidistant from the wound margin. It is important to cinch the tarsal suture tightly to evert the reapproximated wound edges slightly; otherwise as the wound heals and stretches a notch may form at the lid margin. These sutures are left long. The margin sutures can be placed untied on Steri-Strips temporarily to allow better exposure for tarsal closure. The remaining tarsus is closed using interrupted lamellar 6-0 polyglactin sutures with the knot on the anterior tarsal surface to avoid erosion to the ocular surface. Attention must be paid to the distance from the lid margin each suture is placed to ensure even reapproximation of the tarsus. In the upper lid it is important to avoid full-thickness bites onto the conjunctival surface, although this is safely tolerated in the lower eyelid. If they were left untied, the lid margin sutures are now tied. Orbicularis is closed using interrupted, buried 6-0 polyglactin sutures. Skin is closed using interrupted 6-0 nylon or fast-absorbing gut sutures. The long ends of the lid margin sutures are incorporated into a skin suture to keep them away from the cornea. The wound is dressed with antibiotic ointment. Skin sutures can be removed in 7–10 days, but the lid margin sutures should remain for 10–14 days to avoid dehiscence of the margin with resultant notching.
• Surgical repair of eyelid laceration involving lid margin and canaliculus: The area around the wound is infiltrated with 2% lidocaine with epinephrine 1 : 100,000. The area is prepped and draped using povidone-iodine (Betadine) solution and inspected carefully with minimal manipulation. Small (0.3 mm) forceps and cotton-tipped applicators are helpful in locating the nasal end of the transected canaliculus. The punctum of the involved canaliculus is dilated and then intubated with a silicone stent with nasolacrimal probes on each end. The first probe is passed through the puncta and the lateral portion of the lacerated canaliculus. It is then inserted into the medial portion of the canaliculus and advanced into the nasolacrimal sac to a hard stop against the lacrimal sac fossa. The nasolacrimal duct is then intubated by slowly rotating the probe in a superior–inferior orientation with slight downward pressure until a path of low resistance is found, which will be the probe passing through the opening of the nasolacrimal duct. The probe is then retrieved from under the inferior turbinate in the nose by using a straight hemostat, groove director, or hook inserted through the naris. The second arm of the tube is advanced through the opposite puncta and retrieved in the same manner, and the tubes are secured at the external naris. The canalicular tear is closed using two to three interrupted 7-0- polyglactin sutures, which are passed through the canalicular walls. Pericanalicular sutures are added as needed. The lid margin is repaired as described above except that there is no tarsus medial to the puncta. The stent is removed after 3 months.
Eyelid Infections
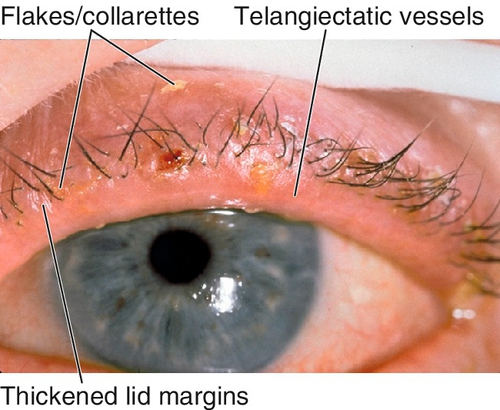
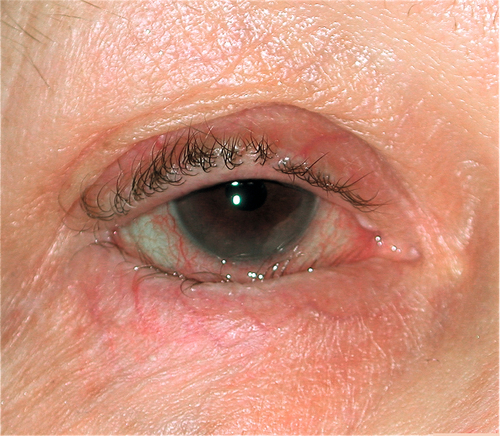
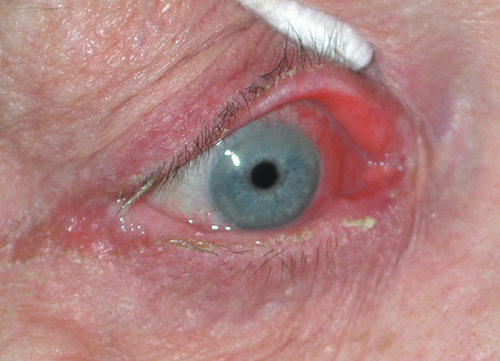
Blepharitis and Meibomitis
Definition
Inflammation of the eyelid margins (blepharitis) and inspissation of the oil-producing sebaceous glands of the lids (meibomitis, meibomian gland dysfunction [MGD]); often occur together. Blepharitis is classified by location (anterior [infectious], posterior [meibomitis, MGD], angular [at lateral canthus]) or etiology.
Etiology
Chronic Staphylococcus or Demodex infection, seborrhea (alone, with staphylococcal superinfection, with meibomian seborrhea, with secondary meibomitis), primary meibomitis, atopic dermatitis, psoriasis, and fungal; angular blepharitis is associated with Moraxella infection. A change in the composition of meibomian gland secretions causes obstruction of the glands, inflammation, and altered tear film. Ocular surface disease results from disruption of the tear film (from bacterial lipolytic exoenzymes and abnormal meibum), epithelial cell death, and inflammation.
Epidemiology
Very common in adult population, prevalence estimated at 12% for anterior blepharitis and 24% for posterior blepharitis; often coexists with dry eye disease (see Chapter 4); also associated with staphylococcal marginal keratitis (see Chapter 5) and acne rosacea (see below).
Symptoms
Itching, red eye, burning, tearing, mild pain, foreign body sensation, filmy vision; often worse on awakening and late in the day.
Signs
Anterior Blepharitis
Crusting /scales along eyelashes (“scurf” [scale fragments] and “collarettes” [scales that encircle base of lash]), loss of eyelashes (madarosis), lid margin redness, conjunctival injection; may develop pannus, phlyctenules, corneal infiltrates, and ulceration.
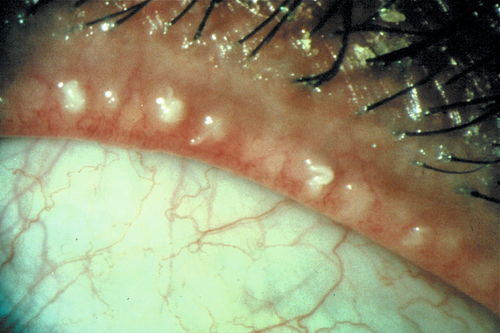
Meibomitis
Thickened and erythematous eyelid margins with telangiectatic blood vessels; atrophic, swollen, pitted, or blocked meibomian glands; turbid, thickened meibum (may have “toothpaste sign”: gentle pressure on lids expresses columns of thick, white sebaceous material; the quality of meibomian gland secretions can be graded on a 0 to 3 scale [i.e., 0 = clear; 1 = cloudy; 2 = granular; 3 = toothpaste]); may have meibomian gland inclusions (visible under the tarsal conjunctiva as yellow bumps), decreased tear break-up time, tear film debris and foam, conjunctival injection, corneal staining (typically inferiorly); may also develop recurrent chalazia /hordeola.
Differential Diagnosis
Dry eye disease, primary herpes simplex virus infection, allergic or infectious conjunctivitis, corneal foreign body, sebaceous cell carcinoma, squamous or basal cell carcinoma, discoid lupus, medicamentosa, ocular cicatricial pemphigoid.
Evaluation
• Complete eye exam with attention to facial skin, lids, meibomian gland orifices, lashes, tear film, conjunctiva, and cornea.
• Biopsy if lesions are suspicious for malignancy (ulcerated, yellow, chronic, scarred, or unilateral lid lesions, often with concomitant corneal pathology).
• Lab tests: Chlamydia cultures (if there is associated chronic follicular conjunctivitis or suspicion of sexually transmitted disease).
Prognosis
Good; flare-ups and remissions are common; maintenance treatment often required indefinitely.
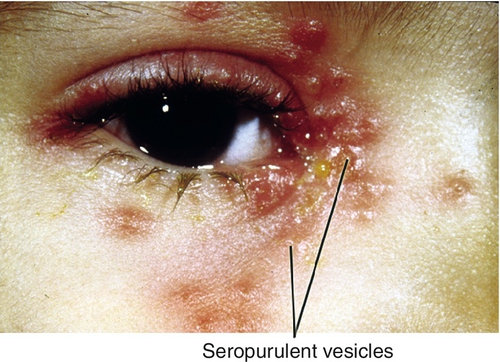
Herpes Simplex Virus
Primary infection due to herpes simplex virus; often mild and unrecognized. Patients may note pain, itching, and redness. Appears as small crops of seropurulent vesicles on the eyelid that eventually rupture and crust over; marginal ulcerative blepharitis, follicular conjunctivitis, punctate or dendritic keratitis, and preauricular lymphadenopathy may also occur.
• Cold compresses bid to qid to affected skin area.
• Systemic antiviral (acyclovir [Zovirax] 400 mg po 5 times /day or famciclovir [Famvir] 500 mg po or valacyclovir [Valtrex] 1 g po tid for 7–10 days).
• Topical antiviral (ganciclovir gel 0.15% [Zirgan] 5 times/day, trifluridine 1% [Viroptic] 9 times /day, or vidarabine 3% [Vira-A] 5 times /day for 1–2 weeks) for patients with blepharoconjunctivitis or corneal involvement.
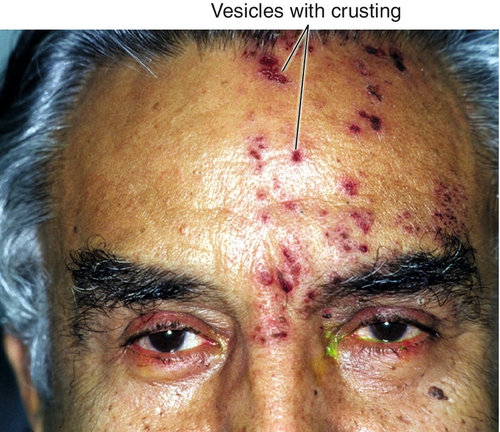
Herpes Zoster Virus
Reactivation of latent varicella zoster virus in the first division of cranial nerve V (herpes zoster ophthalmicus, HZO) usually involving the upper eyelid. Herpes zoster affects 20–30% of the population and increases in incidence and severity with age > 60 years (50% in 85-year-olds), 10–20% of these patients have HZO. Appears as an acute, painful, unilateral, dermatomal maculopapular skin eruption, followed by vesicular ulceration and crusting; new lesions develop for up to 1 week and then resolve in 2–6 weeks. Patients have a prodrome of fever, headache, malaise, and pain (tingling, paresthesias, itching, burning) over the affected cranial nerve V1 dermatome, which may occur without the rash (zoster sine herpete); involvement of the tip or side of the nose (Hutchinson’s sign) is an indicator of ocular involvement (nasociliary branch of the ophthalmic nerve). Ocular involvement occurs in 50% if no antiviral treatment is given; lid scarring may result with entropion, ectropion, trichiasis, lash loss (madarosis), canalicular and punctal stenosis, necrosis, and lid retraction with lagophthalmos and exposure keratitis. Fifty percent develop complications; most common is postherpetic neuralgia (PHN), a neuropathic pain syndrome that continues or occurs after resolution of the rash. PHN also increases in incidence and severity with increasing age (37% in those > 60 years old, 48% in those > 70 years old); other risk factors include severity of pain (prodromal and acute), severity of rash, and ocular involvement.
• Cool saline or aluminum sulfate-calcium acetate (Domeboro) compresses bid to tid.
• Topical antibiotic ointment (erythromycin or bacitracin bid to tid) to affected skin.
• Systemic antiviral (acyclovir [Zovirax] 800 mg po 5 times /day for 7–10 days, or famciclovir [Famvir] 500 mg po or valacyclovir [Valtrex] 1 g po tid for 7 days). If immunocompromised, acyclovir 10–12 mg / kg /day IV, divided q8h for 10–14 days; resistant strains are treated with systemic vidarabine or foscarnet. Antiviral treatment within 72 hours of the rash decreases virus shedding, severity and duration of the rash, acute pain, and incidence of ocular involvement. Treatment with either famciclovir or valacyclovir is preferred to acyclovir because the former two medications reduce the incidence, duration, and severity of PHN.
• Rule out ocular involvement (see Chapters 5 and 6).
• Treatment of PHN consists of one or more of the following agents: tricyclic antidepressants (amitriptyline, doxepin, nortriptyline, or desipramine 25–100 mg po qd), gabapentin (Neurontin 600 mg po 2–6 times a day), pregabalin (Lyrica 300–600 mg po qd), opioids (oxycodone 10–30 mg po bid), topical analgesics (lidocaine 5% ointment, lidocaine-prilocaine cream, or lidoderm 5% patch q4–6h; capsaicin 0.025% [Zostrix] cream is poorly tolerated), and oral steroids (prednisone 60 mg po for 1 week, then 30 mg for 1 week, then 15 mg for 1 week); consider diphenhydramine (Benadryl 25–50 mg po qhs) for postherpetic itching. May rarely require nerve block or botulinum map injections.
• Vaccination in individuals ≥ 60 years old. Safety and efficacy demonstrated in the Shingles Prevention Study (SPS); vaccination reduces the incidence of herpes zoster by 51%, the incidence of PHN by 67%, and the severity and duration if shingles does occur; however, the efficacy of the vaccine decreases with increasing patient age.
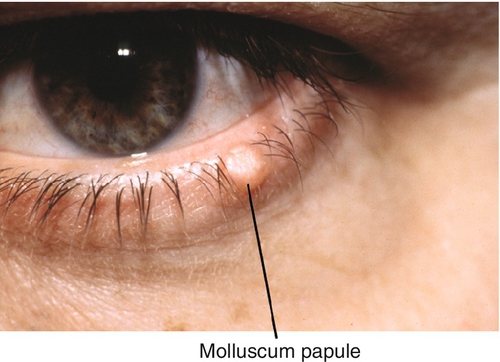
Molluscum Contagiosum
DNA poxvirus infection, typically occurs in children and is spread by direct contact. Usually asymptomatic; appears as shiny dome-shaped waxy papules with central umbilication on the lid or lid margin; papules may appear anywhere on the body. May be associated with chronic follicular conjunctivitis, superficial pannus, and superficial punctate keratitis. Although disease is self-limited, resolution may take years; disseminated disease occurs in patients with acquired immunodeficiency syndrome (AIDS).
Demodicosis
Parasitic hair follicle infection with Demodex folliculorum or D. brevis; associated with blepharitis. Very common infestation but usually asymptomatic; may incite hordeolum formation. Examination of epilated hair follicles reveals sleeves of thin, semitransparent crusting at the base of the lashes.
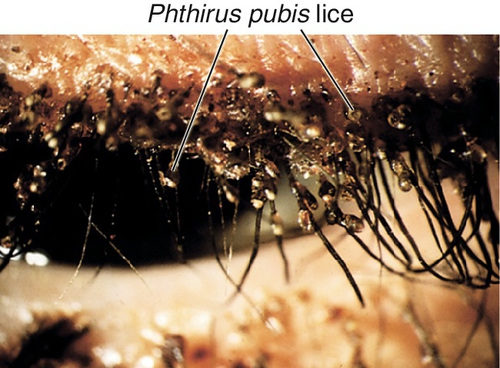
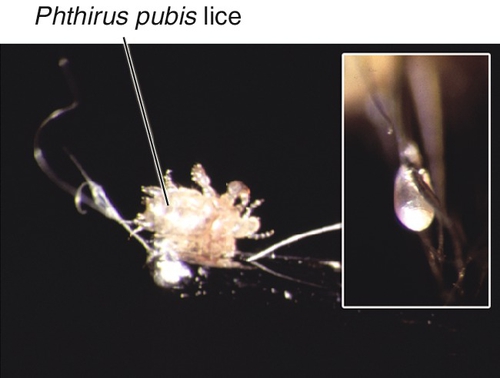
Phthiriasis or Pediculosis
Infestation of eyelashes with lice (Phthirus pubis); usually sexually transmitted or from very close contact with an infected individual. Patients note itching and burning; signs include small, pearly, white nits (eggs) attached to lashes, adult lice, preauricular lymphadenopathy, blood-tinged lids and lashes, blepharoconjunctivitis, conjunctival follicles, and conjunctival injection.
• Mechanical removal of lice and nits with fine forceps.
• Topical ointment (erythromycin or Lacrilube tid for 14 days) to suffocate lice.
• Physostigmine 0.25% ointment × 1, repeat in 1 week, or fluorescein 20% 1–2 drops to lid margins plus delousing creams and shampoo (not for ocular use): permethrin cream rinse 1% (Nix), lindane 1%, γ-benzene hexachloride (Kwell), or pyrethrins liquid with piperonyl butoxide (RID, A-200 Pyrinate liquid). (Warning: Kwell and RID not recommended for pregnant women and children.)
• Discard or thoroughly wash in hot cycle all bedding, linens, and clothing.
• Treat sexual partner.
Leprosy
Chronic infectious disease caused by Mycobacterium leprae, a pleomorphic, acid-fast bacillus. Of the four variants, tuberculoid and lepromatous leprosy can have eyelid involvement, including loss of eyelashes and eyebrows (madarosis), trichiasis, paralytic ectropion, lagophthalmos with exposure keratitis, and reduced blink rate; may develop corneal ulceration and perforation.
• Reduce corneal exposure with temporary or permanent tarsorrhaphy.
Eyelid Inflammations
Chalazion or Hordeolum (Stye)
Definition
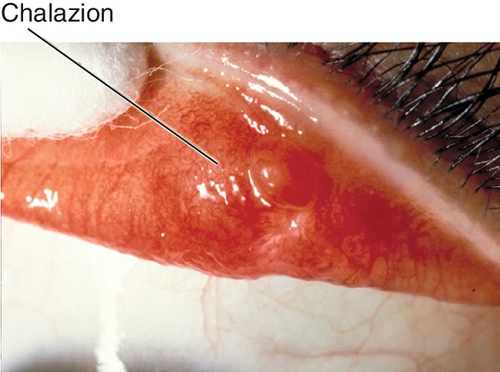
Chalazion
Obstruction and inflammation of meibomian gland with leakage of sebum into surrounding tissue and resultant lipogranuloma formation; often evolving from an internal hordeolum; associated with meibomitis and rosacea.
Hordeolum
Acute bacterial infection of sebaceous eyelid gland; most commonly meibomian gland (internal hordeolum) or gland of Zeis or Moll (external hordeolum); associated with Staphylococcus aureus.
Symptoms
Painful, hot, swollen, red eyelid lump; chronic chalazia become nontender.
Signs
Erythematous subcutaneous nodule, sometimes tender with visible pointing or drainage; usually solitary, but can be multiple or bilateral; occasionally, severe swelling prevents visualization or palpation of a discrete nodule; may have signs of blepharitis, meibomitis and rosacea; may develop super-infection with associated cellulitis.

Figure 3-12 Chalazion of the upper eyelid.
Differential Diagnosis
Preseptal cellulitis, sebaceous cell carcinoma, pyogenic granuloma.
Evaluation
Prognosis
Good; may take weeks to months to resolve fully; recurrence is common (especially in blepharitis or acne rosacea); conservative treatment is recommended; surgical drainage through a posterior incision with curettage and excision of the lipogranulomatous material can lead to scarring and further episodes; steroid injection may produce hypopigmentation or local fat atrophy.
Contact Dermatitis
Definition
Acute skin inflammation resulting from chemical or mechanical irritants, or from immunologic hypersensitivity to an allergic stimulus.
Symptoms
Swelling, redness, itching, tearing, foreign body sensation, and ocular and eyelid discomfort.
Signs
Erythematous, flaking, or crusting rash accompanied by edema; may have vesicular or weeping lesions; lichenified plaques suggest chronic exposure to irritant.
Differential Diagnosis
Herpes simplex, herpes zoster, preseptal cellulitis; chemical, ultraviolet, or thermal burns.
Evaluation
• Complete eye exam with attention to facial skin, lids, conjunctiva, and cornea.
• Consider dermatology consultation.
Prognosis
Usually good; resolution occurs 1–2 weeks after removal of inciting agent; rebound can occur if steroids tapered too rapidly.
Blepharochalasis
Idiopathic, recurrent episodes of painless edema of the upper eyelids with or without redness and itching. Over time, repeated episodes may result in atrophy and laxity of the upper eyelid tissues, causing premature wrinkling of the skin, ptosis, deep superior sulci from fat atrophy, and lacrimal gland prolapse. Typically occurs in young females, first episode usually occurs before the age of 20. Inflammation may be treated acutely with topical steroid ointment; there is no treatment to prevent or shorten the episodes. Blepharoplasty may be helpful in addressing the long-term sequelae of multiple inflammatory episodes.
Madarosis
Definition
Local or diffuse loss of eyelashes or eyebrows or both.
Etiology
Local
Chronic blepharitis, eyelid neoplasm (basal cell, squamous cell, or sebaceous cell carcinoma), burn, trauma, trichotillomania, eyelid infection (zoster, varicella, vaccinia, syphilis, tuberculosis, fungal).
Systemic
Endocrine (hypothyroidism, pituitary insufficiency), dermatologic (psoriasis, seborrheic dermatitis, alopecia syndromes, acne vulgaris, neurodermatitis, ichthyosis, impetigo, lichen planus), medications (topical epinephrine, gold, arsenic, barbiturates, propylthiouracil (PTU), quinine, chemotherapeutic agents), connective tissue disease (systemic lupus erythematosus), chronic malnutrition.
Symptoms
Asymptomatic; may have redness, itching.
Signs
Madarosis; may have lid or skin lesions.
Evaluation
• Evaluation for underlying hormonal or nutritional deficits.
• Consider medical or dermatology consultation.
Prognosis
Depends on underlying etiology.
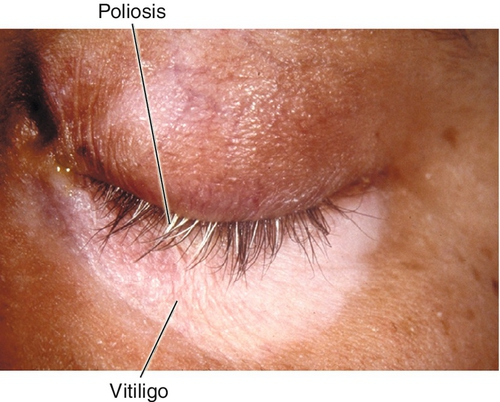
Vitiligo and Poliosis
Total absence of melanin in hair follicles of the eyelashes or eyebrows (poliosis) and in skin (vitiligo), leading to focal patches of white hair or skin; associated with severe dermatitis, Vogt–Koyanagi–Harada syndrome, tuberous sclerosis, localized irradiation, sympathetic ophthalmia, and Waardenburg’s syndrome (autosomal dominant [AD], white forelock, congenital poliosis, nasal root abnormalities, synophrys [hypertrophy and fusion of the eyebrows], congenital deafness, iris heterochromia, and hypertelorism.)
• Treat underlying medical condition.
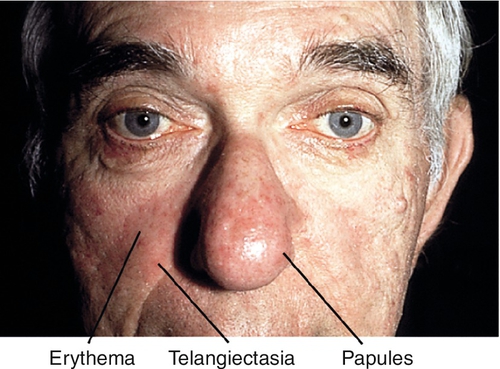
Acne Rosacea
Definition
Chronic inflammatory disorder of the midline facial skin and eyelids.
Etiology
Rosacea is caused by inherent defects in the body’s immune system and vasoregulatory processes and may result from degenerative changes in perivascular collagen resulting in blood vessel dilation and leakage of inflammatory substances into the skin. There is a genetic predilection and it is more common in certain ethnic backgrounds (e.g., Northern European ancestry); more common in women (2–3 ×). Ocular signs and symptoms may occur prior to cutaneous manifestations in 20% of patients; approximately 5% manifest corneal disease. It has also been suggested that the pathophysiology may include an inflammatory response to D. folliculorum or H. pylori. Facial flushing is associated with triggers such as alcohol, spicy foods, caffeine, extreme temperatures, and prolonged sunlight exposure.
Symptoms
Facial flushing, tearing, dry eye, and foreign body sensation.
Signs
Acne, facial and eyelid telangiectasia, flushing most predominantly involving the nose and malar skin, persistent facial erythema, rhinophyma, blepharitis, recurrent chalazia / hordeola, conjunctivitis, keratitis, pannus, decreased tear break-up time, tear film debris and foam.
Evaluation
Prognosis
Clinical course is variable; depends on severity of disease and response to treatment.
Eyelid Malpositions
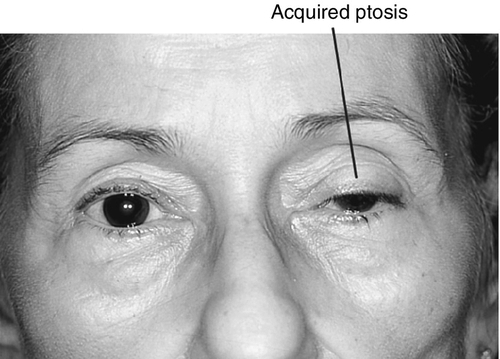
Ptosis
Definition
Drooping of the upper eyelid(s).
Etiology
Aponeurotic (Involutional)
Disinsertion, central dehiscence, or attenuation of the levator aponeurosis causing lowering of the upper eyelid. Most common form of ptosis, often associated with advanced age, eye surgery, ocular trauma, pregnancy, chronic eyelid swelling, and blepharochalasis; good levator function.
Mechanical
Poor upper eyelid elevation due to mass effect of tumors, or to tethering of the eyelid by scarring (cicatricial ptosis); good levator function.
Myogenic
Inherent weakness of levator palpebrae superioris due to muscular disorders including chronic progressive external ophthalmoplegia, myotonic dystrophy, and oculopharyngeal dystrophy; extremely poor levator function.
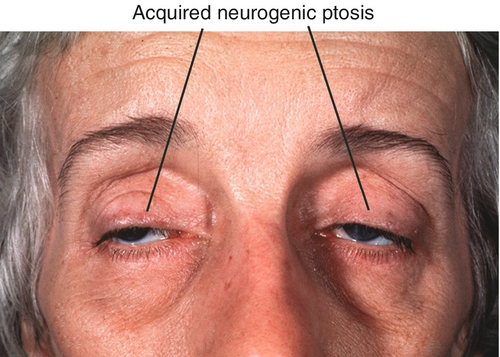
Neurogenic
Defects in innervation to cranial nerve III (oculomotor palsy) or sympathetic input to Müller’s muscle (Horner’s syndrome) or generalized dysfunction of neuromuscular junction such as myasthenia gravis; variable levator function depending on etiology.
Congenital
Poor levator function from birth; usually unilateral, nonhereditary, and myogenic with fibrosis and fat infiltration of levator muscle; rarely results from aponeurosis dehiscence (possibly birth trauma), in which case good levator function would be expected. Congenital Horner’s syndrome (ptosis, miosis, anhidrosis, iris hypopigmentation) with poor Müller’s muscle function from decreased sympathetic tone, or congenital neurogenic with Marcus Gunn jaw-winking syndrome from aberrant connections between cranial nerve V (innervating the pterygoid muscles) and the levator muscle.
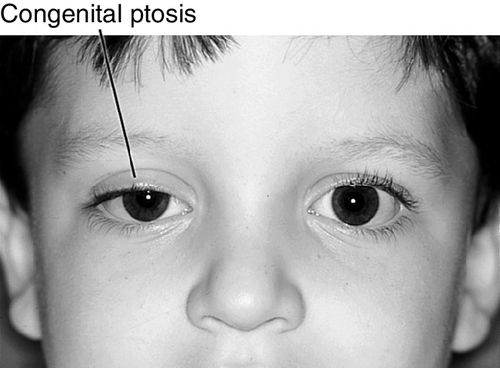
Figure 3-20 Congenital ptosis of the right eye in a child.
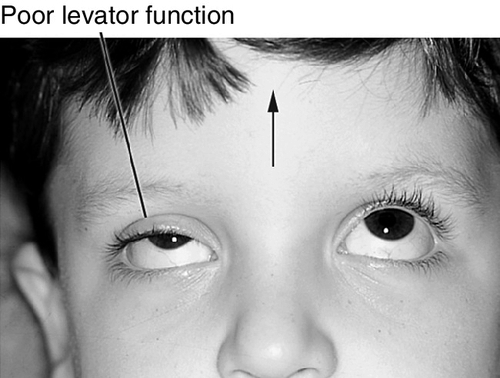
Figure 3-21 Same patient as Figure 3-20, demonstrating poor levator function with upgaze of the right eye. Note reduced levator excursion.
Symptoms
Superior visual field defect, brow ache, loss of depth perception; may have decreased vision (congenital cases with deprivation amblyopia).
Signs
Drooping of upper eyelid(s) with impaired elevation on upgaze, recruitment of brow muscles with brow furrows, higher lid crease and apparently smaller eye on ptotic side, abnormally high contralateral eyelid (Hering’s law); in downgaze, affected lid may be higher than contralateral lid in congenital ptosis (lid lag) and lower in acquired cases; may have decreased visual acuity when visual axis obscured or head tilt with chin-up position when bilateral; other associated abnormalities in congenital ptosis include lagophthalmos, decreased superior rectus function, high astigmatism, anisometropia, strabismus, amblyopia, epicanthus, and blepharophimosis.
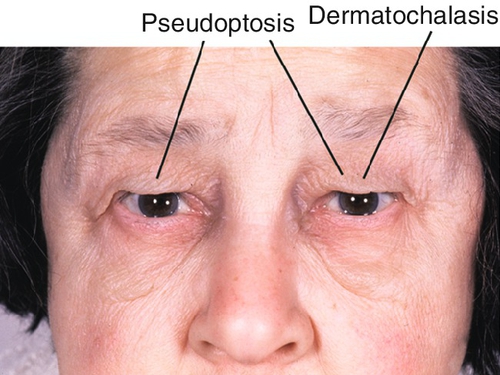
Differential Diagnosis
Dermatochalasis (excess skin of upper eyelids, pseudoptosis), lid swelling, lid tumor, enophthalmos (e.g., orbital floor fracture), hypotropia, contralateral eyelid retraction or proptosis (e.g., thyroid-related ophthalmopathy), and small eye (phthisis bulbi, microphthalmia, anophthalmia).
Evaluation
• Complete eye exam with attention to amblyopia in children, visual acuity, pupils, motility, Bell’s phenomenon, lids, corneal sensation, and cornea.
• Eyelid measurements: margin reflex distance (MRD, distance between upper eyelid margin and corneal light reflex – normal is 4.5 mm), palpebral fissure height, upper lid crease height (high in aponeurotic), and levator function (LF; distance the upper lid margin travels between downgaze and upgaze – normal is greater than 11 mm; normal in aponeurotic, decreased in congenital).
• Consider neurologic evaluation with edrophonium chloride (Tensilon) test to rule out myasthenia gravis.
• Consider phenylephrine 2.5% to stimulate Müller’s muscle and rule out Horner’s syndrome; may also use topical cocaine 4–10% or hydroxyamphetamine 1% or both.
• Check visual field test with and without upper lids being held up by tape or finger (ptosis visual fields) to document visual impairment prior to surgery.
• External photos to document lid appearance prior to surgery.
Prognosis
Excellent for aponeurotic and mechanical ptosis; fair to good for congenital ptosis, depending on the levator function; variable for myogenic and neurogenic ptosis.
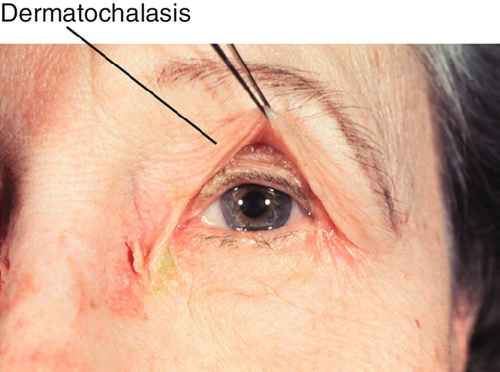
Dermatochalasis
Laxity of the upper eyelid tissues resulting in redundancy of skin and subcutaneous tissue. Frequently associated with herniation of orbital fat through an attenuated orbital septum. May be associated with upper lid ptosis or pseudoptosis (mechanical effect of dermatochalasis). Profound dermatochalasis may result in superior visual field defect. Management is surgical with careful attention given preoperatively to coexisting conditions (e.g., ptosis). Lower lid dermatochalasis, on very rare occasions, may limit vision in downgaze due to extreme orbital fat herniation.
Ectropion
Definition
Eversion of the eyelid margin.
Etiology
Cicatricial
Due to burns (thermal or chemical), ocular trauma (surgical or mechanical), or chronic inflammation with anterior lamellar contraction.
Congenital
Due to vertical shortening of anterior lamella (skin and orbicularis oculi), rarely isolated, may be associated with blepharophimosis syndrome (blepharophimosis, ptosis, epicanthus inversus, and telecanthus).
Inflammatory
Due to chronic eyelid skin inflammation (atopic dermatitis, herpes zoster infections, rosacea).
Involutional
Due to horizontal lid laxity and tissue relaxation, followed by lid elongation, sagging, and conjunctival hypertrophy; usually involves lower eyelid; most frequent cause of ectropion in adults.
Mechanical
Due to lid edema, bulky lid tumors, orbital fat herniation, or lid-riding spectacles.
Paralytic
Usually follows cranial nerve VII (Bell’s) palsy; can be temporary.
Symptoms
Tearing, chronic eyelid or ocular irritation, or asymptomatic.
Signs
Eversion of eyelid margin, conjunctival keratinization, injection and hypertrophy, superficial punctate keratitis, dermatitis (from chronic tearing and rubbing); may have corneal ulceration or scarring.
Evaluation
• Complete eye exam with attention to lids, orbicularis function, lateral canthal tendon laxity, herniated fat and scarring, conjunctiva, and cornea.
Prognosis
Usually good with surgical treatment; cicatricial and inflammatory ectropion are prone to recurrence; paralytic ectropion may resolve spontaneously within 6 months after Bell’s palsy.
Entropion
Definition
Inversion of the eyelid margin; may affect either eyelid, although the lower lid is affected more frequently.
Etiology
Cicatricial
Due to posterior lamella (tarsus and conjunctiva) shortening with lid inversion and rubbing of lashes and lid margin on globe; associated with Stevens–Johnson syndrome, ocular cicatricial pemphigoid, trachoma, herpes zoster, eye surgery, ocular trauma, thermal or chemical burns, and chronic conjunctivitis from long-term topical glaucoma medications.
Congenital
Due to structural tarsal plate defects, shortened posterior lamellae, or eyelid retractor dysgenesis; horizontal tarsal kink is an unusual form of congenital entropion that usually affects the upper eyelid.
Involutional
Most common cause of entropion in older patients, usually affects lower lid; predisposing factors include horizontal lid laxity, overriding preseptal orbicularis, disinserted or atrophied lid retractors, and involutional enophthalmos.
Spastic
Due to ocular inflammation or irritation; often occurs following eye surgery in patients with early underlying involutional changes.
Symptoms
Tearing, foreign body sensation, and red eye.
Signs
Inturned eyelid margin, keratinized eyelid margins (cicatricial), horizontal lid laxity, overriding preseptal orbicularis, enophthalmos, symblepharon (cicatricial), conjunctival injection, superficial punctate keratitis; may have corneal ulceration or scarring.
Differential Diagnosis
Trichiasis, distichiasis, blepharospasm.
Evaluation
• Complete eye exam with attention to lids, lid tone (snapback test), lower lid margin (sagging), medial and lateral canthal tendons, inferior fornix (unusually deep), digital eversion test at the inferior border of tarsus to distinguish involutional from cicatricial entropion (involutional rotates, cicatricial does not).
Prognosis
Good except for autoimmune or inflammatory-related cicatricial entropion.
Blepharospasm
Definition
Bilateral, uncontrolled, episodic contraction of the orbicularis oculi.
Essential Blepharospasm
Thought to be caused by a disorder of the basal ganglia; usually with gradual onset during the fifth to seventh decades; some association with other movement disorders, and high incidence of movement disorders among first-degree relatives.
Meige’s Syndrome
Essential blepharospasm with facial grimacing; may have cog-wheeling in the neck and extremities.
Symptoms
Uncontrollable blinking, squeezing, or twitching of eyelids or facial muscles.
Signs
Spasms of orbicularis oculi or facial muscles; may prevent examiner from prying open lids during episodes; may be absent during sleep ![]() (see Video 3-1).
(see Video 3-1).
Differential Diagnosis
Reflex blepharospasm (caused by eyelid irritation, dry eye, entropion, trichiasis, contact lens overuse, or meningeal irritation), hemifacial spasm, facial myokymia, Tourette’s syndrome, tic douloureux (trigeminal neuralgia), Parkinson’s disease, Huntington’s disease, basal ganglia infarct.
Evaluation
• Complete eye exam with attention to cranial nerves, motility, and lids.
• Consider head magnetic resonance imaging (MRI) with attention to the posterior fossa for atypical history or presentation.
Prognosis
Good with appropriate therapy; in most cases, repeat injections every few months are needed indefinitely.
Bell’s Palsy
Definition
Acutely acquired, isolated, peripheral facial paralysis of unknown cause involving the facial nerve (CN VII).
Etiology
By definition, the etiology is unknown; neural inflammation has been identified by MRI and on autopsy; herpes virus is thought to play a role in most cases.
Symptoms
Acute onset of unilateral facial paralysis over a period of 24 hours, often accompanied by headache and numbness; dry eye, foreign body sensation, tearing, drooling, dysarthria, and dysphagia. Long-term symptoms include oral–ocular synkinesis, gustatory lacrimation, decreased vision, corneal irritation.
Signs
Unilateral facial paralysis including all divisions of CN VII. Chronic signs include brow ptosis, ipsilateral hypertonicity, lagophthalmos, exposure keratopathy with epiphora, ulceration, and scarring.

Figure 3-26 Patient with left-sided Bell’s palsy. Note hypertonicity on left side of face.

Figure 3-27 Same patient as Figure 3-26 with left-sided Bell’s palsy during attempted lid closure. Note the large lagophthalmos and good Bell’s reflex of the left eye.
Table 3-1
House–Brackmann Facial Nerve Grading System
| Grade | Description | Characteristics |
| I | Normal | Normal facial function |
| II | Mild dysfunction | Very slight weakness found on close inspection; good forehead function; complete and quick eyelid closure |
| III | Moderate dysfunction | Obvious but not disfiguring asymmetry; mild synkinesis; slight forehead movement; complete eyelid closure with effort |
| IV | Moderately severe dysfunction | Disfiguring asymmetry; no forehead movement; incomplete eyelid closure |
| V | Severe dysfunction | Barely perceptible facial movement; incomplete eyelid closure |
| VI | Total paralysis | No movement |
Adapted from House JW, Brackmann DE: Facial nerve grading system, Otolaryngol Head Neck Surg 93:146, 1985.
Differential Diagnosis
Tumor of parotid gland or facial nerve, trauma (temporal bone fracture), congenital facial nerve palsy, herpes zoster cephalicus, central nervous system (CNS) disease, postsurgical.
Evaluation
• Complete eye exam with attention to cranial nerves, lids, orbicularis function, brow position, lower lid retraction, and cornea.
• Delayed onset with progression over more than 1 week requires MRI of facial nerve and CT of temporal bone.
• Additional cranial nerve involvement requires further brain stem investigation.
Prognosis
Typically excellent with most patients returning to nearly complete function (grade 2); 90% of function returns within 1 year, 99% within 2 years.
Floppy Eyelid Syndrome
Definition
Chronic papillary conjunctivitis with lax tarsi, spontaneous eyelid eversion, and loss of eyelid–globe contact when lying prone.
Etiology
Nocturnal lid eversion with rubbing of the tarsal conjunctiva against bedding.
Epidemiology
Often occurs in obese men with obstructive sleep apnea, also associated with keratoconus.
Symptoms
Chronically red and irritated eyes, particularly upon awakening; mild mucous discharge.
Signs
Loose, rubbery eyelids (particularly upper lids), very easily everted, palpebral conjunctival papillae, conjunctival injection, superficial punctate keratitis.
Differential Diagnosis
Giant papillary conjunctivitis, adult inclusion conjunctivitis, superior limbic keratoconjunctivitis, vernal keratoconjunctivitis, atopic keratoconjunctivitis, medicamentosa.
Evaluation
• Formal sleep study to evaluate for obstructive sleep apnea.
Prognosis
Excellent.
Trichiasis
Definition
Misdirected eyelashes.
Etiology
Entropion, cicatricial eye disease, chronic eyelid inflammation, or idiopathic.
Symptoms
Red eye, foreign body sensation, and tearing.
Signs
Eyelashes directed toward and rubbing against the eye, conjunctival injection, superficial punctate keratitis; may have corneal scarring in chronic cases.
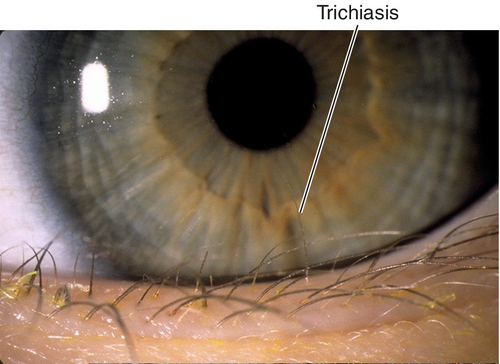
Figure 3-29 Trichiasis demonstrating posterior misdirection of eyelid lashes touching the corneal epithelium. Not to be confused with distichiasis (see Figure 3-32).
Differential Diagnosis
Distichiasis (ectopic eyelashes).
Evaluation
• Complete ophthalmic history and eye exam with attention to lids, lashes, conjunctiva, and cornea.
Prognosis
Frequent recurrences with mechanical technique, usually good with permanent removal.
Congenital Eyelid Anomalies
Ankyloblepharon
Partial or complete eyelid fusion. Severe forms may be associated with craniofacial abnormalities. Prognosis usually good unless severe associated defects.
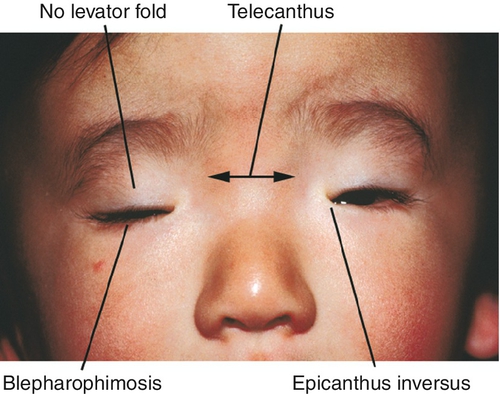
Blepharophimosis
Tight, foreshortened (vertically and horizontally) palpebral fissures with poor eyelid function and no levator fold. May be sporadic or part of congenital syndrome (AD) with blepharophimosis, blepharoptosis, epicanthus inversus, and telecanthus. Prognosis depends on extent of syndrome and need for additional surgery. Mapped to chromosome 3q2 (FOXL2 gene).
• Surgery usually is performed at 4–5 years of age to allow nasal bridge to develop fully.
• Congenital syndrome: consider staged oculoplastic repair with medial canthoplasty via Y–V plasty and transnasal wiring, followed by frontalis suspension for ptosis 3 to 4 months later, and finally full-thickness skin graft from periauricular or supraclavicular area.
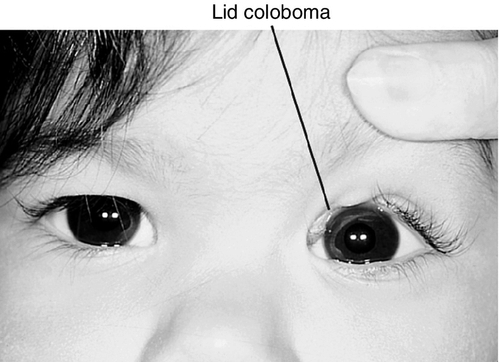
Coloboma
Small notch to full-thickness defect of the eyelid due to incomplete union of frontonasal or maxillary mesoderm at the eyelid margin, usually superonasal and unilateral. Inferolateral defects are often bilateral and associated with systemic anomalies such as mandibulofacial dysostosis (AD; Treacher Collins syndrome); corneal exposure and dryness may occur. Small defects (< 25%) have good prognosis; prognosis of medium and larger defects depends on location and associated abnormalities. Associated with microphthalmos, iris coloboma, and anterior polar cataract.
• Topical lubrication with preservative-free artificial tears or ointments up to q1h.
• Surgical repair (delay until preschool age): small defects (< 25%) via pentagonal resection with direct layered closure, medium defects (25–50%) via Tenzel flap with or without lateral cantholysis, large defects (> 50%) via myocutaneous flap or full-thickness lid rotation flap.
• Beware of lid-sharing procedures in children because occlusion amblyopia may result.
Cryptophthalmos
Congenital defects of the first, second, and third wave of neural crest migration leading to abnormal lid and anterior eye structure development, including partial or complete absence of eyebrow, palpebral fissure, eyelashes, and conjunctiva; may have hidden or buried eye with smooth skin stretching from brow to cheek; more posterior orbital structures are usually normal. Prognosis often poor due to underlying structural ocular defects.
Distichiasis
Ectopic eyelashes growing posterior to or out of the meibomian gland orifices. May be congenital or acquired (i.e., from chronic inflammation), sometimes hereditary. Lashes are usually shorter, softer, and finer than normal cilia, and may or may not contact the conjunctival and corneal surfaces; usually well tolerated. In congenital distichiasis, the embryonic pilosebaceous units inappropriately develop into hair follicles. Treat if corneal involvement exists, but with caution because treatment can be more damaging than disease.
• Epilation, tarsal fracture surgery, electrolysis, cryotherapy, or laser thermal ablation in more severe cases.
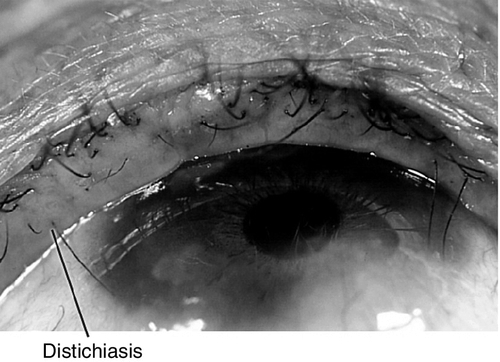
Figure 3-32 Distichiasis with lashes originating from meibomian gland orifice.
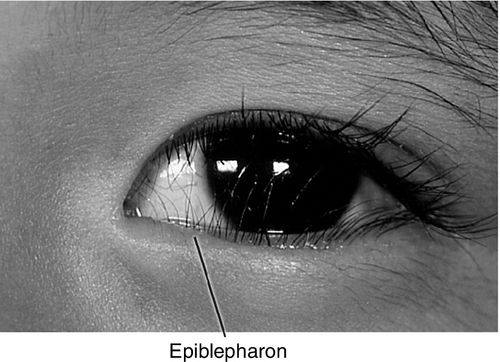
Epiblepharon
Redundant skin and orbicularis muscle leading to inward rotation of the lower eyelid margins, turning lashes against the globe; usually resolves spontaneously. More common in Asians. Prognosis excellent even if surgery necessary.
• Conservative treatment in infants, because condition tends to resolve with facial maturation.
• Subciliary myocutaneous excision is extremely effective; care is taken to avoid overexcision with resultant ectropion.
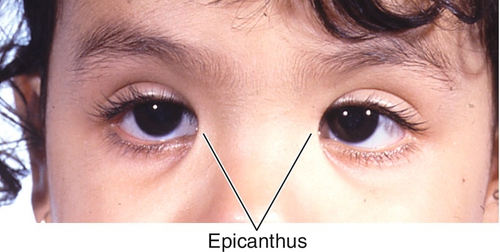
Epicanthus
Crescentic vertical skin folds in the medial canthal area overlying the medial canthal tendon; usually bilateral. Caused by immature facial bones or redundant skin and underlying tissue. May be most prominent superiorly (epicanthus tarsalis), inferiorly (epicanthus inversus), or equally distributed (epicanthus palpebralis). Epicanthus tarsalis is frequently associated with Asian eyelids, while epicanthus inversus is associated with blepharophimosis syndrome. Good prognosis.
• If due to facial bone immaturity, delay treatment.
• When treatment required (delay until preschool age), Z-plasty or Y–V plasty often effective; eyelid crease construction may be required.
Euryblepharon
Horizontal widening of the palpebral fissure, often temporally; usually involves the lower eyelid with an antimongoloid appearance due to inferior insertion of the lateral canthal tendon. Patients have a poor blink, poor lid closure, and lagophthalmos with exposure keratitis. Usually good prognosis.
• Topical lubrication with preservative-free artificial tears in mild cases.
• If symptoms severe and corneal pathology exists, full-thickness eyelid resection with repositioning of lateral canthal tendon may be required. If necessary, vertical eyelid lengthening can be achieved with skin grafts.
Microblepharon
Rare, bilateral, vertical foreshortening of the eyelids, sometimes causing exposure and dry eye symptoms; may be related to cryptophthalmos. Usually stable with good prognosis if no exposure keratitis exists.
• Topical lubrication with preservative-free artificial tears in mild cases.
• Pedicle rotation skin flaps from cheek or brow, eyelid-sharing procedures, or full-thickness skin grafts for severe exposure with a normal globe.
• Beware of lid-sharing procedures in children because occlusion amblyopia may result.
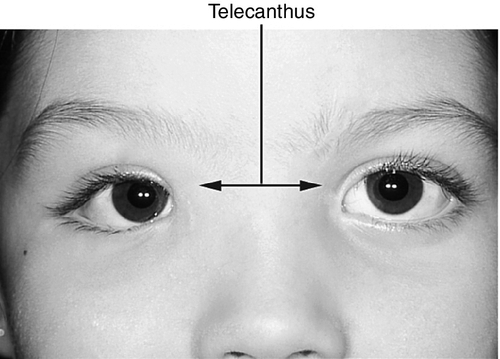
Telecanthus
Increased distance between medial canthi caused by long medial canthal tendons (in contrast to hypertelorism in which the distance between the medial walls of the orbits is increased). Most frequent ocular finding in fetal alcohol syndrome; also associated with Waardenburg’s syndrome and blepharophimosis syndrome. Good prognosis.
• Transnasal wiring to shorten distance between medial canthi and remove excess medial canthal skin.
Benign Eyelid Tumors
Pigmented Benign Eyelid Tumors
Acquired Nevus
Darkly pigmented lesion that contains modified melanocytes called nevocellular nevus cells. Classified according to location in skin: junctional (epidermis), compound (epidermis and dermis), or dermal (dermis); may contain hair. Malignant transformation rare, although the Halo nevus, a type of compound nevus, is associated with remote cutaneous malignant melanoma. The Spitz nevus, another type of compound nevus, may be confused histologically with malignant melanoma in children and young adults.
• No treatment usually required.
• Consider excision for cosmesis, chronic irritation, or evidence of malignant transformation.
Ephelis (Freckle)
Focal regions of cutaneous melanocytic overactivity; cells slightly larger than normal. Found in sun-exposed areas; occurs in individuals with fair complexions. No malignant potential.
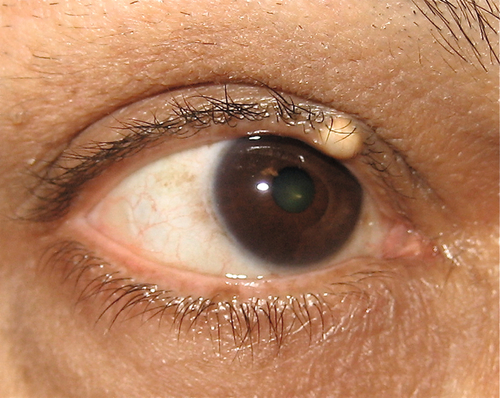
Oculodermal Melanocytosis (Nevus of Ota)
Unilateral, blue-gray, pigmented macule; usually in the distribution of the first and second division of cranial nerve V with ipsilateral melanocytosis of the sclera and uveal tract; 10% bilateral; melanosis of the ipsilateral orbit and leptomeninges may occur. Histologically, composed of dermal fusiform dendritic melanocytes. May be present at birth or during the first year of life. Increased risk of congenital glaucoma; risk of malignant transformation is very low; however, cutaneous and ocular melanoma can occur, especially in Caucasians.
• No treatment usually required.
• Periodic examinations to monitor for evidence of malignant transformation.
Seborrheic Keratosis
Waxy, pigmented, hyperkeratotic, plaque-like, crusty lesion; occurs in the elderly. Histologically, composed of intradermal proliferation of basal epithelioid cells. Irritation is frequent; no malignant potential.
• Shave excision or curettage for small lesions.
• Complete surgical excision for larger lesions.
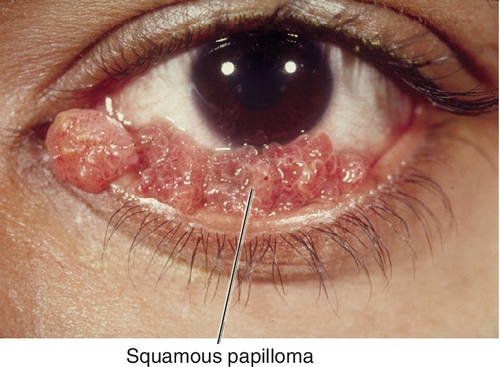
Squamous Papilloma
Most common benign eyelid growth; occurs in older adults. Benign hyperplasia of the squamous epithelium; may be sessile or pedunculated with color similar to that of skin; grows slowly and in groups. Etiology is unclear; viral papillomas are found in groups and more common in children, whereas the elderly usually develop individual or widely spaced papillomas that are not thought to be viral in origin. Histologically, papillomas display epithelial hyperkeratosis and acanthosis around a central vascular core.
Verruca Vulgaris (Viral Papilloma)
Viral-related growth with potential for malignant transformation. Usually asymptomatic; appears as a pedunculated or sessile hyperemic mass on eyelid or tarsal conjunctiva with minimal surrounding inflammation. Associated with human papilloma virus (strains 6, 11, and 16). Frequently resolves spontaneously.
• Observation if small and no inflammation.
• Larger or multiple lesions may be entirely excised, scraped, cauterized, or treated with cryo- therapy; satellite lesions are thought to respond to initial treatment of selected lesions.
Nonpigmented Benign Eyelid Tumors
Xanthelasma
Xanthomas of the eyelids that appear as flat or slightly elevated creamy yellow plaques; usually bilateral, involving the medial upper lids. Histologically composed of foamy histiocytes surrounded by localized inflammation. Occurs in older patients; most patients with xanthelasma are normolipidemic. Systemic diseases that demonstrate xanthomatosis include biliary cirrhosis, diabetes, pancreatitis, renal disease, and hypothyroidism. Xanthelasma is the least specific of the xanthomas (nodular, tendinous, eruptive, and plaques). Excellent prognosis, usually recur after excision.
• Lab tests: In extreme cases, serum cholesterol and triglycerides.
• Full-thickness excision with flaps or grafts, carbon dioxide laser treatment, or chemical cauterization with trichloroacetic acid as needed.
Moll’s Gland Cyst (Hidrocystoma, Sudoriferous Cyst)
Benign cystic lesion resulting from abnormal proliferation of apocrine secretory gland (gland of Moll); also known as sudoriferous cyst or cystadenoma. Smooth, translucent, and several millimeters in size; usually slow-growing and painless; frequently involves the eyelid, particularly the inner canthus in a peripunctal location. No predilection for race or gender but more common in adults than in children. Differential diagnosis includes cystic basal cell carcinoma and milia (pilosebaceous cysts). Recurrence after complete excision is rare, but incision alone to drain the fluid contained within the hidrocystoma typically results in recurrence.
• Marsupialization or complete excision.
• Peripunctal excision may require canalicular probing to avoid or detect canalicular injury.
Epidermal Inclusion Cyst
Firm, freely mobile, subepithelial lesion (1–5 mm in diameter); cyst contains cheesy keratin material produced by cyst lining. Thought to arise from occluded surface epithelium or pilosebaceous follicles. Often has a central pore representing the remaining pilar duct, or occasionally a dark or even black center indicating oxidized keratin. Multiple epidermal inclusion cysts may be associated with Gardner’s syndrome or Torre’s syndrome.
Inverted Follicular Keratosis
Small, solitary, benign lesion with a nodular or verrucous appearance. Occurs in older adults; male predilection. May arise over months and is thought to have a viral etiology. Histologically, lobular acanthosis of the epithelium with squamous and basal cell proliferation; represents a type of irritated seborrheic keratosis.
Milia
Multiple, umbilicated, well-circumscribed, pinhead-sized, elevated, round, white nodules (1–3 mm in diameter). May arise spontaneously, or after trauma, radiation, herpes zoster ophthalmicus, or epidermolysis bullosa. Thought to represent retention follicular cysts caused by blockage of pilosebaceous units.
Sebaceous (Pilar) Cyst
Yellow, elevated, smooth, subcutaneous tumor with central comedo plug caused by sebaceous or meibomian gland obstruction; occurs in the elderly. Less common than epithelial inclusion cysts; may be associated with chalazia.
• Complete surgical excision with inclusion of epithelial lining.
Pilomatrixoma (Calcifying Epithelioma of Malherbe)
Small (< 3 cm), solitary, firm, nodular lesion consisting of cells that demonstrate features of hair cells; slow, progressive growth; usually flesh-colored but may have a red or purple hue. Occur in the head and neck, often along the brow or lid. More common in Caucasians; slight female predilection. Differential diagnosis includes dermoid cyst, preseptal cellulitis, and cutaneous abscess. Histology reveals characteristic calcification. Recurrence after complete excision is rare.
• Biopsy or complete surgical excision.
Vascular Benign Eyelid Tumors
Capillary Hemangioma
Most common pediatric eyelid tumor, usually appears within 1 month of life with a bluish subcutaneous mass and normal overlying dermis, or as a superficial vascular lesion (sometimes erroneously called strawberry nevus) representing hamartomatous growth of capillary blood vessels. Rapid growth occurs in two phases with peaks at 3 and 8 months; spontaneous involution begins after 1 year and may proceed up to 10 years; slight female predilection.
Possible amblyopia due to occlusion of the visual axis or induced astigmatism; myopia or strabismus may occur. Prognosis usually good if visual axis clear and no amblyopia.
• Routine follow-up visits to monitor for amblyopia and refractive error.
• Large lesions may be treated with intralesional steroid injection, systemic corticosteroids, or surgical excision. Interferon (Lupron) should be avoided due to spastic diplegia. Pulsed dye laser may be useful in treating the superficial component of some lesions.
• Consider topical timolol 0.5% applied bid for several months.
Lymphangioma
Congenital malformation with a predilection for the head and neck. Around the eye, the orbit is more often involved. The eyelid can be involved, but is rarely involved in isolation (see Chapter 1).
Port Wine Stain (Nevus Flammeus)
Congenital venular malformation often confused with eyelid hemangioma. Always present at birth and follows dermatomal distribution. Typically lighter with a more purple hue than hemangioma; facial involvement may include any or multiple branches of the trigeminal nerve (CN V); does not blanch on palpation. Risk of glaucoma (from increased venous pressure) and the Sturge–Weber syndrome (facial port wine stain, choroidal “hemangioma”, intracranial vascular anomalies [see Phakomatoses section in Chapter 10]) occurs primarily in patients with V1 and V2 involvement; risk of Sturge–Weber with isolated V1 involvement is extremely small.
• Early examination for choroidal involvement and glaucoma is critical.
• Pulsed dye laser treatment is recommended as early as 1 month of life.
• Cranial nerve V2 involvement is an indication for MRI of the brain.
Malignant Eyelid Tumors
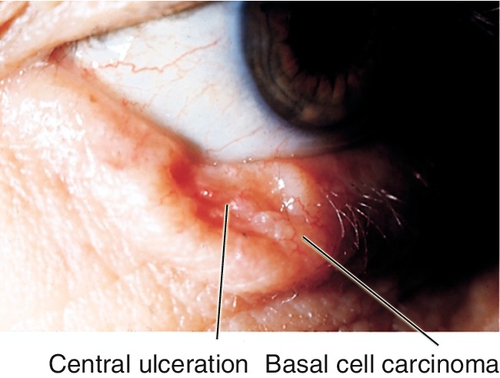
Basal Cell Carcinoma
Firm, pearly nodule or flatter, less well-defined lesion with central ulceration, telangiectasia, madarosis (lash loss), and inflammation. Associated with ultraviolet radiation exposure and fair skin. Most common (90%) malignant eyelid tumor; occurs in older adults with male predilection (2 : 1). Usually found on lower lid (67%) followed in frequency by upper lid (20%), medial canthus (10%), and lateral canthus (3%). Locally invasive, but rarely metastatic (usually occurs with canthal involvement). Two growth patterns:
Nodular
Most common; appears as small, painless, umbilicated nodule with sharp pearly borders and superficial telangiectasia that can be ulcerative (“rodent ulcer”); rarely pigmented; less invasive. Nests of cells with peripheral palisading on histopathologic examination.
Morpheaform or Sclerosing
Appears as flat, indurated plaque that lacks distinct margins; often ulcerated; more invasive. Associated with nevoid basal cell carcinoma syndrome, linear unilateral basal cell nevus, and Bazex syndrome. Excellent prognosis with appropriate treatment, but 2–10% local recurrence; metastasis in 0.02–0.1%.
• Protect against further sun damage.
• Complete surgical excision with margin controls (frozen sectioning); Mohs micrographic surgery sometimes useful in preserving critical eyelid tissue.
• Extremely advanced cases involving both upper and lower lids may benefit rarely from external beam irradiation.
• Canthal tumors require orbital CT scan to evaluate posterior (orbital) involvement. Radiation or cryotherapy should not be used in these lesions, because posterior portions of the tumor may go untreated.
Squamous Cell Carcinoma
Flat or slightly elevated, scaly, ulcerated, erythematous plaque, often arising from actinic keratosis (better prognosis), may also arise from Bowen’s disease (in situ) and radiation dermatosis. Constitutes less than 5% of malignant eyelid tumors (although second most common it is 40–50 times less common than basal cell carcinoma). Usually found on lower lid with lid margin involvement. Risk factors include sun exposure, radiation injury, fair skin, or other irritative insults; male predilection. Potentially metastatic (low) and locally invasive (faster growth than basal cell carcinoma), regional lymph node spread from eyelids occurs in 13–24% of cases. Prognosis varies with tumor size, degree of differentiation, underlying etiology, and depth of tumor invasion.
• Protect against further sun damage.
• Incisional or excisional biopsy with wide surgical margins (wider than basal cell carcinoma).
• Adjunctive radiation, cryotherapy, or chemotherapy, or a combination.
• Postseptal involvement typically requires orbital exenteration.
Actinic Keratosis
Most common precancerous skin lesion; 25% develop squamous cell carcinoma. Round, scaly, flat, or papillary keratotic growth with surrounding erythema; found in sun-exposed areas. Occurs in older adults with fair complexions. Histologically, cellular atypia with mitotic figures and hyperkeratosis; squamous carcinoma-in-situ.
• Periocular lesions require incisional or excisional biopsy to rule out malignant lesions.
• Cryotherapy or additional surgery can be performed once diagnosis is confirmed.
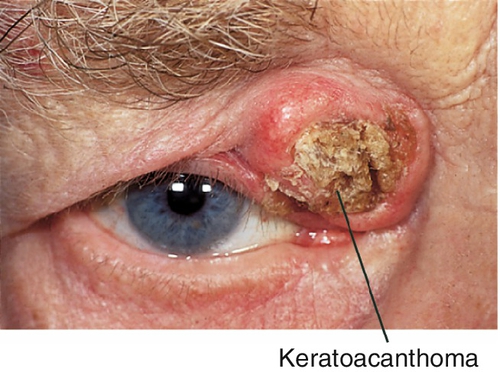
Keratoacanthoma
Rapidly growing lesion usually found in sun-exposed areas with a central ulcerated, keratin-filled crater and hyperkeratotic margins; occurs in older adults. Lid or lash involvement may cause permanent damage; spontaneous resolution is common. A form of pseudoepitheliomatous hyperplasia; neither distinction is used any longer in some pathology laboratories, where these lesions are all classified as squamous carcinomas. May have viral origin; multiple keratoacanthomas occur in Ferguson–Smith syndrome.
• Complete surgical excision is treatment of choice for single lesions.
Sebaceous Cell Carcinoma
Highly malignant, rare neoplasm of the sebaceous glands in the caruncle or lids; most common in fifth to seventh decades. May masquerade as chronic unilateral blepharitis (20–50% of patients) or recurrent chalazion; usually found on upper lid. Constitutes 1–15% of malignant eyelid tumors (approximately equal incidence to squamous carcinoma of the eyelid, and 40–50 times less common than basal cell carcinoma); female predilection. Sometimes related to previous radiotherapy. Pagetoid spread common (discontinuous areas of tumor spread through epithelium). Cardinal signs include madarosis, poliosis, and thick, red lid margin inflammation; tumor is typically yellow and hard; lymphadenopathy common. Poor prognosis when symptomatic for longer than 6 months (38% mortality vs 14% for less than 6 months), size greater than 2 cm (60% mortality vs 18% when < 1 cm), upper and lower lid involvement (83% mortality), poor differentiation, and local vascular or lymphatic infiltration. Muir–Torre syndrome (multiple internal malignancies and external sebaceous tumors) is more common in sebaceous gland hyperplasia than sebaceous carcinoma.
• Orbital exenteration required in advanced cases.
• Palliative radiation.
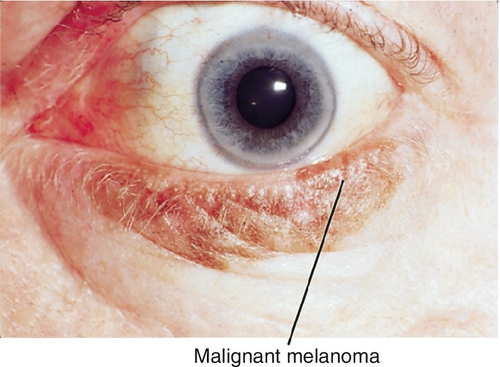
Malignant Melanoma
Tan, black, or gray nodule or plaque with irregular, notched borders; often rapidly growing with color changes. Most lethal primary skin tumor, but rare (< 1% of eyelid malignancies); prognosis related to histology, depth of invasion, and tumor thickness. Acral lentiginous melanoma does not occur in the eyelids. Orderly growth with stage 1: localized disease without lymph node spread; stage 2: palpable regional lymph nodes (preauricular from upper lid, submandibular from lower lid); and stage 3: distant metastases; choroidal melanoma may reach lids via extrascleral extension into orbit. Fair prognosis for stage 1, poor for stages 2 and 3. Three histologic types:
Nodular Melanoma
Very rare on eyelid (10% of cases), aggressive, worst prognosis.
Superficial Spreading Melanoma
Most common (80% of cases), onset usually 20–60 years of age. Presents as flat, variegated, multicolored lesion that invades dermis, rapidly leading to raised nodule.
Lentigo Maligna Melanoma
Ten percent of cases, related to sun exposure, usually in the elderly. Appears as flat, tan-brown lesion with irregular borders that enlarges radially with black flecks; largest when identified, often due to underdiagnosis.
• Orbital exenteration and neck dissection required in advanced cases.
• Dermatologic evaluation.
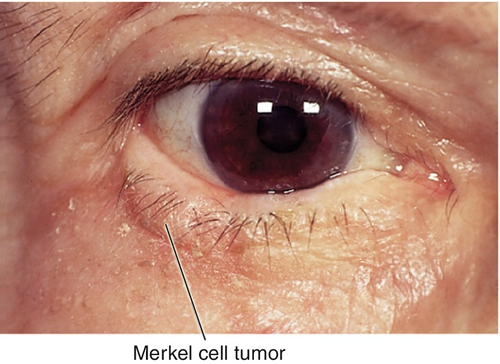
Merkel Cell Tumor
Rare, rapidly growing, solitary, violaceous, vascularized, occasionally ulcerated tumor of the amino precursor uptake and decarboxylation (APUD) system; usually found in sun-exposed areas. Onset in seventh decade; reported only in Caucasians. Potential for recurrence and lymphatic spread with lymph node enlargement. Generally poor prognosis due to early spread after local excision alone, 39% recur locally and 46% recur regionally; after adjuvant radiation therapy or node dissection, 26% recur locally and 22% regionally; 67% tumor mortality for locoregional spread.
• Lymph node resection.
• Supplemental radiation therapy.
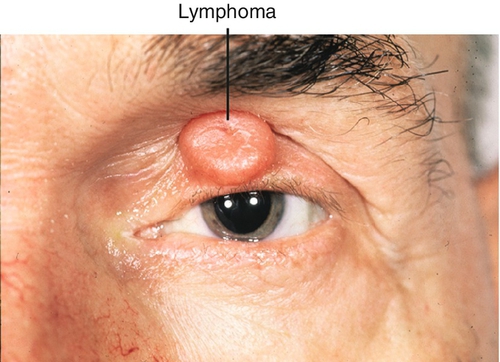
Metastatic Tumors
Metastatic eyelid lesions are very rare. Female predilection; occur in older adults. Primary sites include breast and lung (most common) carcinoma, cutaneous malignancies, gastrointestinal and genitourinary carcinomas, and lymphoma. Three patterns: (1) single nontender nodule, (2) painless diffuse induration, (3) ulcerating lesion of eyelid skin or conjunctiva. Evidence of primary tumor elsewhere, lymph node enlargement; usually poor prognosis but variable.
• Local excision, radiation, or observation.
• Systemic treatment for primary tumor.
Kaposi’s Sarcoma
Soft-tissue sarcoma usually associated with acquired immunodeficiency syndrome (AIDS), may also rarely occur in Africans and older men of Mediterranean descent; very malignant in immunocompromised patients. Appears as violaceous nodules on the eyelids that are nontender and progress over several months; may have associated distortion of the eyelid with entropion, edema, trichiasis, and corneal scarring.
• May require cryotherapy, radiotherapy, chemotherapy, immunotherapy, or a combination.
Systemic Diseases
Neurofibromatosis
Definition
Neurofibromatosis (NF) is one of the classic phakomatoses and is an AD inherited disorder of the neuroectodermal system, affecting primarily neural-crest-derived tissue (Schwann cells and melanocytes), manifesting with neural, cutaneous, and ocular hamartomas. The disorder displays highly variable expressivity. Two types:
NF-1 (Von Recklinghausen’s Disease)
Mapped to chromosome 17q with a prevalence of 1 in 3000; 50% of cases represent new mutations. NF-1 is a developmental syndrome caused by germline mutations in neurofibromin, a protein that appears to be a negative regulator of the ras oncogene signal transduction pathway. Diagnosis requires two or more of the following criteria:
(1) Six or more café-au-lait spots 15 mm or larger in adults, 5 mm or larger in children.
(2) Two or more neurofibromas; or one plexiform neurofibroma.
(3) Axillary or inguinal freckling.
(4) Optic nerve or tract glioma.
(5) Two or more iris Lisch nodules.
(6) Characteristic osseous lesion (i.e., sphenoid dysplasia).
(7) First-degree relative with NF-1 by these criteria.
NF-2 (Bilateral Acoustic Neurofibromatosis)
Mapped to chromosome 22q11-13.1 (“Merlin” gene) with a prevalence of 1 in 60,000; 50% of cases represent new mutations. The gene product (Merlin or Schwannomin) is thought to be involved in tumor suppression. Diagnostic criteria include:
(1) Bilateral acoustic neuromas.
(2) First-degree relative with NF-2 and either a single acoustic neuroma or two of the following: glioma, neurilemoma, meningioma, neurofibroma, or a premature posterior subcapsular cataract.
Signs
NF-1
Café-au-lait spots, neurofibromas (fibroma molluscum), plexiform neurofibromas (bag of worms), intertriginous freckling, CNS and spinal cord gliomas, meningiomas, nerve root neurofibromas, intracranial calcifications, mild intellectual deficit, kyphoscoliosis and pseudoarthroses, gastrointestinal neurofibromas, pheochromocytoma, plus various other malignant tumors.
NF-1 Ocular Findings
Lisch nodules (iris melanocytic hamartomas), eyelid café-au-lait spots, neurofibromas, and plexiform neurofibroma; may have ipsilateral congenital glaucoma, proptosis secondary to tumors or bony defects, conjunctival neurofibromas, enlarged corneal nerves, diffuse uveal thickening, choroidal hamartomas, retinal astrocytic and combined hamartomas, optic nerve glioma.
NF-2
Paucity of cutaneous lesions (few or small café-au-lait spots), bilateral acoustic neuromas, CNS and spinal cord gliomas, meningiomas, nerve root neurofibromas, intracranial calcifications, pheochromocytoma, plus various other malignant tumors.
NF-2 Ocular Findings
Premature posterior subcapsular cataracts (40%), combined retinal hamartomas, optic nerve meningioma, and glioma; no Lisch nodules.
Evaluation
• Lab tests: Complete blood count (CBC), electrolytes, and urine catecholamines (vanillylmandelic acid, metanephrine).
• Brain and orbital MRI or CT scan.
• Audiography for patients with NF-2.
• Intelligence testing.
Prognosis
Increased morbidity if associated with CNS or other malignant neoplasm.
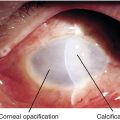
Sarcoidosis
Idiopathic multisystem disease, with abnormalities in cell-mediated and humoral immunity and granulomatous inflammation in many organs; commonly affects the lungs, skin, and eyes including the eyelid skin, lacrimal gland and sac, and nasolacrimal duct. May cause redness, pain, swelling of involved lids or lacrimal glands (usually bilateral), painless subcutaneous nodular masses of eyelids, ptosis, diplopia, severe cicatrizing conjunctival inflammation, conjunctival nodules, keratoconjunctivitis sicca, band keratopathy, granulomatous anterior or posterior uveitis, cataract, chorioretinitis, retinal periphlebitis or neovascularization, optic nerve disease, glaucoma, and orbital involvement. Variable prognosis depending on organs involved.
• Biopsy of conjunctival, lacrimal, or eyelid nodule (with stains to rule out acid-fast bacteria).
• Lab tests: Angiotensin converting enzyme (ACE), CBC, lysozyme, serum calcium, chest radiographs, and purified protein derivative (PPD) and controls; additional tests may be ordered by pulmonologist or internist and include chest CT and gallium scans.
• Sarcoid dacryoadenitis is treated with systemic corticosteroids. Tuberculosis must be ruled out prior to initiating therapy.
• Uveitis is treated with topical corticosteroids (see Chapter 6).
• Retinal consultation as indicated.
• Treatment of systemic disease (steroids and chemotherapy) by internist.
Amyloidosis
Definition
Group of diseases (systemic or localized; primary or secondary) characterized by abnormal protein production and tissue deposition.
Etiology
Nonfamilial and familial forms. Familial amyloidosis (AD) is caused by substitution errors in coding of prealbumin. Associated with multiple myeloma.
Symptoms
Asymptomatic; may notice eyelid discoloration, droopy eyelids, dryness, decreased vision, diplopia, floaters.
Signs
Systemic Findings
Polyarthralgias, pulmonary infiltrates, waxy, maculopapular skin lesions, renal failure, postural hypotension, congestive heart failure, and gastrointestinal bleeds.
Familial form
Autonomic dysfunction, peripheral neuropathies, and cardiomyopathy.
Ocular Findings
Decreased visual acuity; may have flat or nodular purpuric lesions of the eyelids, lacrimal gland, caruncle, or conjunctiva (ruptured, fragile, amyloid-infiltrated blood vessels in abnormal tissue), or may occur without hemorrhage as elevated, yellowish, waxy eyelid papules; ptosis, proptosis, ophthalmoplegia, dry eye, corneal deposits, iris stromal infiltrates, vitreous opacities, retinal vascular occlusions, cotton-wool spots, retinal neovascularization, and compressive optic neuropathy.

Figure 3-60 Amyloidosis of the right upper eyelid causing ptosis.
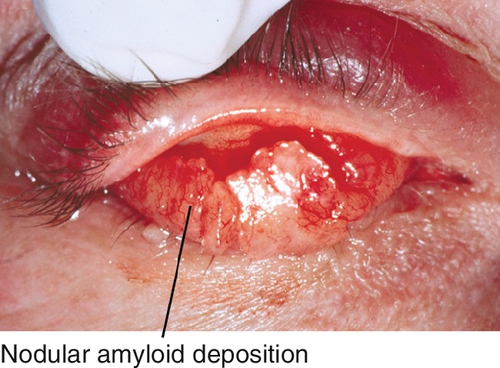
Figure 3-61 Same patient as Figure 3-60, demonstrating thickened everted eyelid with plaque-like appearance.
Evaluation
• Lab tests: CBC, serum and urine protein electrophoresis, serum total protein, albumin and globulin, liver function tests, blood urea nitrogen (BUN) and creatinine, erythrocyte sedimentation rate (ESR), ANA, rheumatoid factor (RF), VDRL, FTA-ABS, urinalysis, PPD and controls, chest radiographs, electrocardiogram (ECG), bone scan.
• Diagnosis made by biopsy (birefringence and dichroism with Congo red stain, metachromasia with crystal violet, and fluorescence with thioflavine-T).
• Medical consultation.
Prognosis
Variable depending on systemic involvement; very poor when associated with multiple myeloma.
Canaliculitis
Definition
Inflammation of the canaliculus (duct between the punctum and lacrimal sac), often resulting in recurrent conjunctivitis.
Etiology
Actinomyces israelii (Streptothrix), a filamentous anaerobic (or facultative anaerobic) Gram-positive rod, is the most common cause; other organisms include Candida albicans, Aspergillus, Nocardia asteroides, and herpes simplex or zoster virus; more common in middle-aged women; usually insidious onset.
Symptoms
Medial eyelid tenderness, tearing, and redness.
Signs
Erythema and swelling of punctum and adjacent tissue (“pouting punctum”), follicular conjunctivitis around medial canthus, expression of discharge from punctum, concretions in canaliculus, grating sensation on lacrimal duct probing, dilated canaliculus on dacryocystography.
Differential Diagnosis
Conjunctivitis, dacryocystitis, nasal lacrimal duct obstruction, and carunculitis.
Evaluation
• Complete ophthalmic history with attention to history of recurrent conjunctivitis and tearing.
• Complete eye exam with attention to lids, lacrimal system, expression of discharge from punctum, and conjunctiva.
• Compression medial to the punctum observing for discharge.
• Lab tests: Culture and Gram stain (Actinomyces branching filaments and sulfur granules on Gram stain).
• Probing and possible irrigation to determine patency of canalicular system.
• Consider dacryocystography to confirm a dilated canaliculus, concretions, or normal outflow function in the lower excretory system.
Prognosis
Often good; depends on infecting organism.
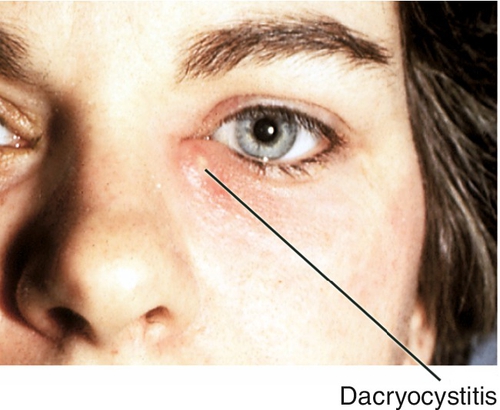
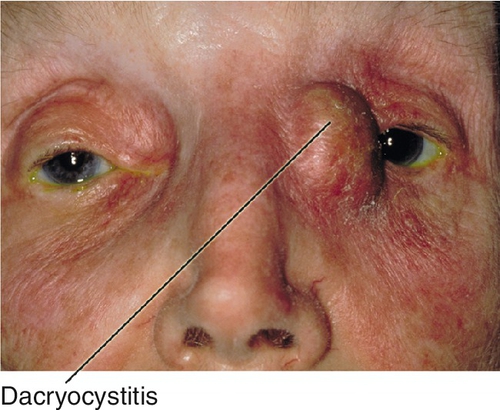
Dacryocystitis
Definition
Acute or chronic infection of the lacrimal sac, often with overlying cellulitis.
Etiology
Streptococcus pneumoniae, Staphylococcus species, and Pseudomonas species; Haemophilus influenzae (nontypeable) in children. Associated with conditions that cause lacrimal sac tear stasis and predispose to infection, including strictures, long and narrow nasolacrimal ducts, lacrimal sac diverticulum, trauma, dacryoliths, congenital or acquired nasolacrimal duct obstruction, and inflammatory sinus and nasal problems.
Symptoms
Pain, swelling, and redness over nasal portion of lower eyelid with tearing and crusting; may have fever.
Signs
Edema and erythema below the medial canthal tendon with lacrimal sac swelling; tenderness on palpation of the lacrimal sac, expression of discharge from the punctum; may have fistula formation or lacrimal sac cyst.
Differential Diagnosis
Ethmoid sinusitis, preseptal or orbital cellulitis, lacrimal sac neoplasm, dacryocystocele (infants) and encephalocele (infants, blue mass above medial canthal tendon), and facial abscess.
Evaluation
• Complete eye exam with attention to lids, lacrimal system, expression of discharge from punctum, digital massage of lacrimal sac, motility, exophthalmometry, and conjunctiva.
• Lab tests: Culture and Gram stain any punctal discharge (chocolate agar in children).
• Do not probe nasolacrimal duct during acute infection.
• Orbital CT scan for limited motility, proptosis, sinus disease, or atypical cases not responding to antibiotic therapy.
Prognosis
Good; usually responds to therapy, but surgery almost always required; if untreated, sequelae include mucocele formation, recurrent lacrimal sac abscess, orbital cellulitis, and infectious keratitis.
Nasolacrimal Duct Obstruction
Definition
Obstruction of the nasolacrimal duct.
Etiology
Congenital
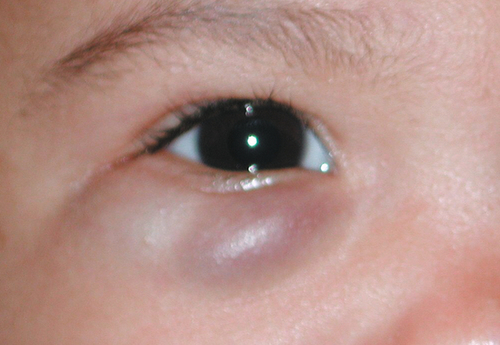
Most frequently due to an imperforate membrane over the valve of Hasner at the nasal end of the duct; occurs clinically in 2–4% of full-term infants at 1–2 weeks of age; bilateral in one-third of cases. Spontaneous opening frequently occurs 1–2 months after birth; may be complicated by acute dacryocystitis.
Acquired
Due to chronic sinus disease, involutional stenosis, dacryocystitis, or naso-orbital trauma; uncommonly caused by obstruction from neoplasm such as nasal /sinus or lacrimal sac /duct tumors. Involutional stenosis is the most common cause in older individuals; female predilection (2 : 1); may be associated with granulomatous diseases such as Wegener’s granulomatosis and sarcoidosis; increased risk of dacryocystitis.
Symptoms
Tearing, discharge, crusting, recurrent conjunctivitis.
Signs
Watery eyes, eyelash crusting and debris, mucus reflux from punctum with compression over the lacrimal sac, medial lower eyelid erythema.
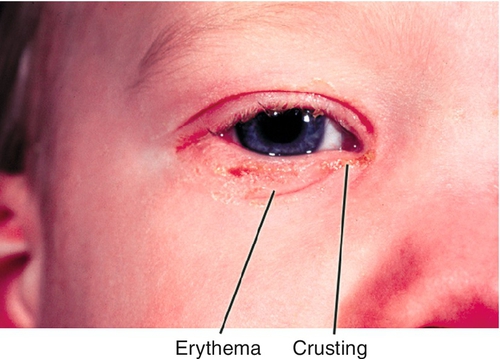
Figure 3-65 Nasolacrimal duct obstruction with tearing, crusting of eyelids, and lower lid erythema.
Differential Diagnosis
Congenital Tearing
Congenital glaucoma, trichiasis, conjunctivitis, nasal lacrimal duct anomalies (punctal atresia), dacryocystocele, corneal abrasion, corneal trauma from forceps delivery, ocular surface foreign body.
Acquired Tearing
Conjunctivitis, trichiasis, entropion, ectropion, corneal abnormalities, dry eye syndrome, blepharitis, punctal stenosis, canalicular stenosis.
Evaluation
• Dye disappearance test with fluorescein, particularly helpful in infants.
• Jones I test: Fluorescein is instilled in conjunctival cul-de-sac; a cotton-tipped applicator is used to attempt fluorescein retrieval via the external naris. Positive test result indicates functional blockage.
• Jones II test: Nasolacrimal irrigation with saline following positive Jones I test; fluorescein retrieval is attempted once again. Positive test result indicates anatomic blockage.
• Nasolacrimal irrigation: 23-gauge cannula mounted on 3–5 mL syringe is inserted into canaliculus, and irrigation is attempted. Retrograde flow through opposite canaliculus and punctum indicates nasolacrimal blockage. Reflux through same punctum indicates canalicular obstruction. Successful irrigation into nose and throat eliminates anatomic blockage but does not rule out functional blockage.
• Consider orbital and sinus CT scan for atypical demographics or presentation.
• Consider nasal endoscopy especially before surgical intervention.
Prognosis
Excellent for congenital; often good for acquired, depends on cause of obstruction.
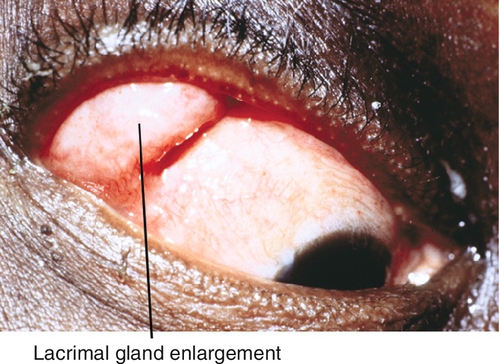
Dacryoadenitis
Definition
Inflammation of the lacrimal gland.
Etiology
Usually of idiopathic, noninfectious origin, viral, bacterial, or rarely parasitic etiology.
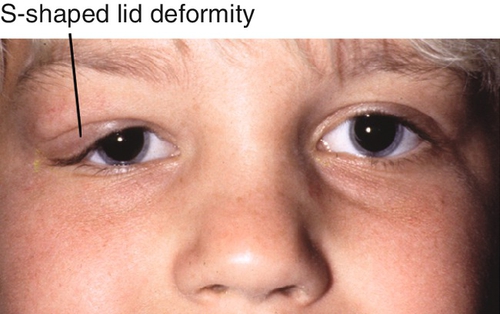
Acute
Most commonly due to infection (Staphylococcus species, mumps, Epstein–Barr virus, herpes zoster, or Neisseria gonorrhoeae); palpebral lobe affected more frequently than orbital lobe; most cases associated with systemic infection; typically occurs in children and young adults.
Chronic
More common than acute form; usually due to inflammatory disorders including idiopathic orbital inflammation, sarcoidosis, thyroid-related ophthalmopathy, Sjögren’s syndrome, and benign lymphoepithelial lesions; also with syphilis and tuberculosis.
Symptoms
Acute
Temporal upper eyelid redness, swelling, and pain with tearing and discharge.
Chronic
Temporal upper eyelid swelling; occasional redness and discomfort.
Signs
Acute
Edema, tenderness, and erythema of upper eyelid with S-shaped deformity, enlarged and erythematous lacrimal gland (palpebral lobe), preauricular lymphadenopathy, and fever; may have inferonasal globe displacement and proptosis if orbital lobe involved.
Chronic
Tenderness in superotemporal area of upper eyelid, globe displacement, restricted ocular motility, and enlarged lacrimal gland.
Differential Diagnosis
Malignant lacrimal gland neoplasm, preseptal or orbital cellulitis, viral conjunctivitis, chalazion, dermoid tumor, lacrimal gland cyst (dacryops).
Evaluation
Acute
• Lab tests: culture and Gram stain of discharge, CBC with differential; consider blood cultures for suspected systemic involvement.
• Orbital CT scan for proptosis, motility restriction, or suspected mass.
Chronic
• Lab tests: Chest radiographs, CBC with differential, ACE, lysosyme, VDRL, FTA-ABS, PPD and controls.
• Orbital CT scan.
• Consider chest CT scan or gallium scan.
• Consider lacrimal gland biopsy if diagnosis uncertain or malignancy suspected.
Prognosis
Depends on etiology; most infections respond well to treatment.
Lacrimal Gland Tumors
Approximately 50% of all lacrimal gland masses are inflammatory; the other 50% are neoplasms. Of these, 50% are of epithelial origin while 50% are primarily lymphoproliferative (see Chapter 1). Of all epithelial tumors, 50% are pleomorphic adenomas (benign mixed tumors), and 50% are malignant. Lacrimal gland lesions appear in the superotemporal quadrant of the orbit. Patients often have inferior and medial globe displacement, limitation of ocular movements, lid edema and erythema, and a palpable mass under the superotemporal orbital rim. Conditions that may present in a similar fashion include dermoids, sarcoidosis, idiopathic orbital inflammation, and dacryops.
Benign Mixed Cell Tumor (Pleomorphic Adenoma)
Most common epithelial tumor of the lacrimal gland, usually appearing insidiously in the fourth and fifth decades, often with inferior and medial displacement of the globe. A firm, circumscribed mass can be palpated under the superior temporal orbital rim, often with bony remodeling (not osteolytic) on radiographic images. Histologically, these tumors contain a pseudocapsule, a double row of epithelial cells forming lumens, and stroma containing spindle-shaped cells with mucinous, osteoid, or cartilaginous metaplasia. Complete resection is critical in order to avoid malignant degeneration. Excellent prognosis if tumor is excised completely.
• Orbital CT scan: Well-circumscribed mass with lacrimal gland fossa enlargement.
• Fine-needle aspiration biopsy of the lacrimal gland may be useful in some cases.
• En bloc excision via a lateral orbitotomy; rupture of pseudocapsule may lead to recurrence and malignant transformation. Incisional biopsy should be avoided.
Malignant Mixed Cell Tumor (Pleomorphic Adenocarcinoma)
Occurs in the elderly with pain and rapid progression; contains the same epithelial and mesenchymal features of pleomorphic adenoma, but with malignant components; associated with longstanding or incompletely excised pleomorphic adenomas. Treatment and prognosis are similar to adenoid cystic carcinoma (see below).
Adenoid Cystic Carcinoma (Cylindroma)
Most common malignant tumor of the lacrimal gland, rapid onset with infiltrative capacity; associated with pain due to perineural invasion; bony erosion and proptosis common. CT scan shows a poorly defined mass with adjacent bony destruction. Histologically, the tumor is composed of densely staining, small cells that grow in nests, tubules, or a Swiss cheese (cribriform) pattern; the basaloid pattern carries the worst prognosis. Five-year survival rate is 47%, and at 15 years is only 22%; major cause of death is intracranial extension due to perineural spread.
• Orbital CT scan: Irregular mass with or without adjacent bony erosion
• En bloc resection with wide margins including orbital rim at a minimum. Orbital exenteration with adjunctive chemotherapy and irradiation may be required, and must be discussed with each patient on a case-by-case basis.