Chapter 51 Lateral Extracavitary Approach to the Thoracolumbar Spine
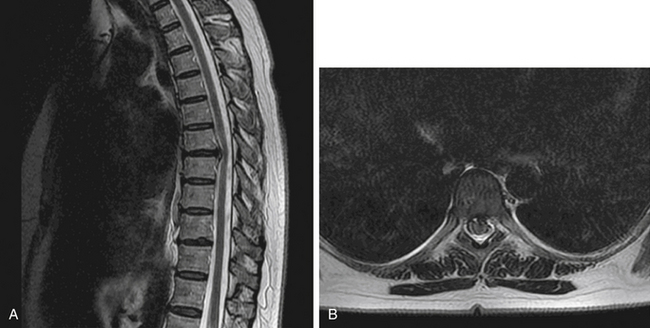
The lateral extracavitary approach (LECA) can be used in the thoracolumbar spine to access both the ventral and dorsal elements of the spinal column. Through this approach, discectomy, spondylectomy, fusion, and deformity reduction may be accomplished. In addition, other approaches, including transpedicular decompression and laminectomy, can be added to allow a 360-degree approach through one incision. LECA was first used as a derivation of lateral costotransversectomy in the treatment of tuberculous spondylitis (Pott disease) by Capener in 1933 and first reported by Seldon in 1935.1 It was also described in 1960 by Hulme, who advocated it as an alternative to laminectomy for ventral thoracic pathology, including disc herniation, secondary to the high incidence of poor surgical outcome of laminectomy attributed to inadequate exposure of ventral elements and the requirement of direct manipulation of the thoracic spinal cord and its extradural vasculature.2 The approach was further refined by Larson et al. at the Medical College of Wisconsin, and it has been applied to traumatic lesions, thoracic disc herniations, tumors, and other pathologic conditions1,3–7 (Figs. 51-1 to 51-5). This approach has recently been modified in a cadaver study to be used via minimally invasive retractor systems for deformity correction.8 Minimally invasive LECA has also been used successfully in thoracic disc herniation.9
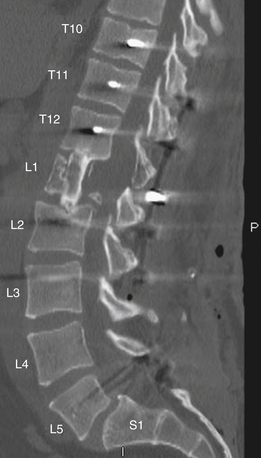
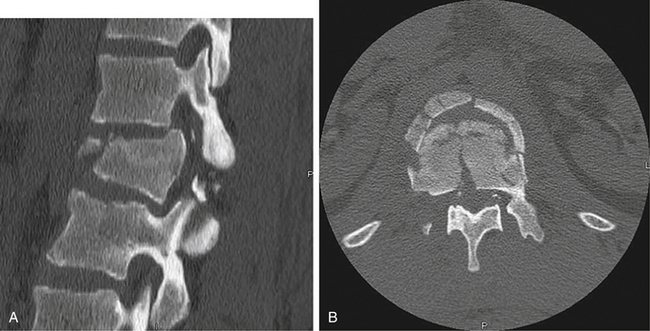
FIGURE 51-4 Postoperative sagittal CT reconstruction of the patient in Figures 51-2 and 51-3. The patient underwent a lateral extracavitary partial corpectomy of L1 with allograft and posterior instrumentation.

FIGURE 51-5 Anteroposterior radiograph demonstrating T10-L3 instrumentation in the patient from Figures 51-2 to 51-4.
This approach can be applied to ventral spinal lesions located between T1 and L5 and, if necessary, can be performed in a bilateral fashion for more extensive pathology.10 In addition to decompression and the removal of pathology, ventrolateral instrumentation can be accomplished through LECA with additional instrumentation placed dorsally as needed.
Operative Technique
Following the induction of general anesthesia, the patient should have a Foley catheter placed and appropriate preoperative antibiotics administered. The Jackson table provides optimal padding and available positioning for LECA, and all pressure points should be checked after positioning. The patient should be safely secured to the table at all points because the bed will be rotated later in the case. For discectomy or fractures, the use of intraoperative monitoring is not essential; for deformity correction and tumor cases, such monitoring may provide an additional measure of safety. Following induction and proper positioning, the next step is appropriate fluoroscopic localization of the lesion. This is critical because the exposure provides a direct view of specific vertebrae, and extending the exposure more than one level in either direction can be difficult. It is imperative to have a clear understanding of the bony anatomy on radiograph before surgery to aid in localization. The typical anatomy of the rib and thoracic spine interface is also an important fact to keep in mind. In most patients a rib abuts disc space in the thoracic spine, and this rib typically corresponds to the caudal vertebrae at the segment.11 For example, at T7, the rib typically articulates with the T6-7 disc space. This anatomy holds true down to the T10-11 space. The 11th and 12th ribs typically articulate with the corresponding vertebral bodies below the disc spaces. It is generally advisable to count ribs in the thoracic spine from above and below and to compare this count with preoperative radiographs for confirmation.
Once the location has been confirmed and marked, attention is given to planning the incision. Various shapes have been used (Fig. 51-6), but the hockey stick–type incision is generally performed. The incision should generally extend from at least one segment cranial to the pathology to one segment caudal to it, with the caudal limb angling out toward the pathologic side with attention paid to the need for approaching the dorsal elements or placing instrumentation. For procedures involving dorsal fixation and fusion, the straight midline portion of the planned incision should extend to the segments to be included in the construct. In the case of single-level discectomy without a need for dorsal exposure, a paramedian incision may be used and may be as small as 5 cm in length.
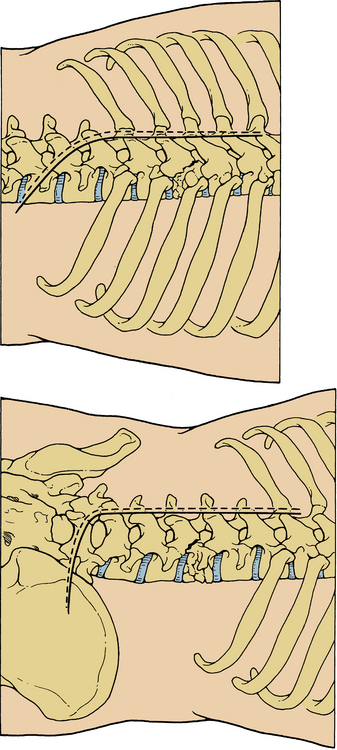
FIGURE 51-6 Two variants of the standard hockey stick–style incision for the lateral extracavitary approach.
After the incision is made, the approach varies little. Usually one rib should be exposed for discectomy; two ribs must be exposed to widen the field for tumor or fracture where a vertebrectomy is planned. At this point, a Doyen rib-stripping tool is used to free the rib of soft tissue and the intercostal vein, artery, and nerve complex that travels on the caudal surface of the rib. The rib is then cut approximately 10 cm from its insertion and disarticulated at the costovertebral joint (Fig. 51-7). This piece can often be removed intact and should be kept for possible use as graft. For lumbar spine pathology, the same general approach applies, with the transverse processes serving the localizing function for which the ribs are used in the thoracic spine. Careful attention must be paid to the location of the nerve roots and possibly prefixed lumbosacral plexus.
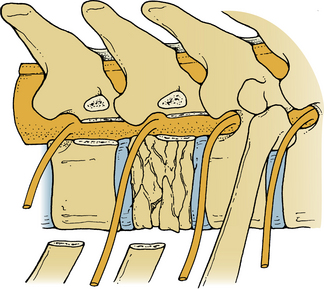
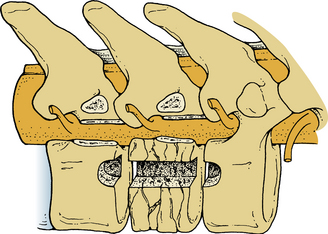
LECA then proceeds in a logical sequence of decompression, stabilization, and fusion. If the surgery is for discectomy, the operation may proceed in a standard fashion at this point, with an anular incision followed by removal of herniated fragments. This incision can be continued through LECA until the opposite side of the thecal sac is visualized. Down-pushing curettes across the disc space may help in accomplishing this. If the goal of the surgery is vertebrectomy, the entire affected body may be removed using a combination of high-speed drill, curettes, and rongeurs. In the case of fractures, it is sometimes safer to leave a few millimeters of bone attached to the dura to prevent injury. To achieve adequate vertebrectomy and proper fusion bed preparation, the disc spaces above and below must also be cleared until the end plates of the rostral and caudal vertebrae are visible (Fig. 51-8). These can then be decorticated using the drill or curettes. After this, the graft material of choice is inserted and lateral plating applied to the upper and lower vertebral bodies. In the case of discectomy, no additional instrumentation is necessary and fusion in the absence of overt instability is unnecessary. If fusion is necessary, the removed rib pieces can be used as structural autograft or alternately taken to the back table and morselized for use with expandable cages (Fig. 51-9). If necessary, dorsal instrumentation can be used as well for further support if overt instability is noted. This instrumentation should be compressed very little to avoid loosening the ventral graft and is best placed before the addition of the interbody or other ventral graft.12
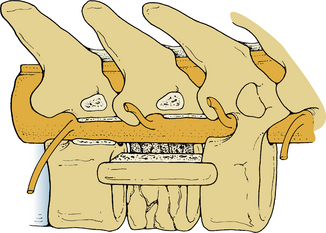
FIGURE 51-9 One possible method of grafting using structural autograft following partial vertebrectomy.
A chest radiograph should be taken in the recovery room to check for pneumothorax, even in the absence of frank pleural wall breech. Patients can be mobilized after recovery from anesthesia, and the average length of stay following discectomy alone is 1 day.12 Length of stay for trauma and neoplasm is longer and often depends on the patient’s other comorbidities. The incidence of pneumothorax following LECA is about 8% (although some report a higher incidence), and infection rates are less than 2%.12,13 Vascular and pleural injuries are rare but possible complications; subarachnoid pleural fistula has been reported but is also rare.14 Postoperative atelectasis and pneumonia are also a concern, as is ileus.1,13,15 If roots must be sacrificed, care should be taken to divide them proximal to the dorsal root ganglion to avoid excessive pain afterward.15
Larson S.J., Holst R.A., Hemmy D.C., Sances A.Jr. Lateral extracavitary approach to traumatic lesions of the thoracic and lumbar spine. J Neurosurg. 1976;45:628-637.
Lifshutz J., Lidar Z., Maiman D. Evolution of the lateral extracavitary approach to the spine. Neurosurg Focus. 2004;16:E12.
Maiman D. Lateral extracavitary apporach to the thoracolumbar spine. In: Wolfla C., Resnick D., editors. Neurosurgical operative atlas: spine and peripheral nerves. New York: Thieme; 2007:156-160.
Maiman D.J., Larson S.J., Benzel E.C. Neurological improvement associated with late decompression of the thoracolumbar spinal cord. Neurosurgery. 1984;14:302-307.
Maiman D.J., Larson S.J., Luck E., El-Ghatit A. Lateral extracavitary approach to the spine for thoracic disc herniation: report of 23 cases. Neurosurgery. 1984;14:178-182.
1. Lifshutz J., Lidar Z., Maiman D. Evolution of the lateral extracavitary approach to the spine. Neurosurg Focus. 2004;16:E12.
2. Hulme A. The surgical approach to thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry. 1960;23:133-137.
3. Arnold P.M., Baek P.N., Stillerman C.B., et al. Surgical management of lumbar neuropathic spinal arthropathy (Charcot joint) after traumatic thoracic paraplegia: report of two cases. J Spinal Disord. 1995;8:357-362.
4. Benzel E.C., Larson S.J. Operative stabilization of the posttraumatic thoracic and lumbar spine: a comparative analysis of the Harrington distraction rod and the modified Weiss spring. Neurosurgery. 1986;19:378-385.
5. Larson S.J., Holst R.A., Hemmy D.C., Sances A.Jr. Lateral extracavitary approach to traumatic lesions of the thoracic and lumbar spine. J Neurosurg. 1976;45:628-637.
6. Maiman D.J., Larson S.J., Benzel E.C. Neurological improvement associated with late decompression of the thoracolumbar spinal cord. Neurosurgery. 1984;14:302-307.
7. McCormick P.C. Surgical management of dumbbell and paraspinal tumors of the thoracic and lumbar spine. Neurosurgery. 1996;38:67-74. discussion 74-65
8. Voyadzis J.M., Gala V.C., O’Toole J.E., et al. Minimally invasive posterior osteotomies. Neurosurgery. 2008;63:204-210.
9. Lidar Z., Lifshutz J., Bhattacharjee S., et al. Minimally invasive, extracavitary approach for thoracic disc herniation: technical report and preliminary results. Spine J. 2006;6:157-163.
10. Steinmetz M.P., Claybrooks R., Krishnaney A., et al. Surgical management of osseous hemangioblastoma of the thoracic spine: technical case report. Neurosurgery. 2005;57:E405. discussion E405
11. Ahmed A., Trost G. Costotransversectomy. In: Wolfla C., Resnick D., editors. Neurosurgical operative atlas: spine and peripheral nerves. New York: Thieme; 2007:151-155.
12. Maiman D. Lateral extracavitary apporach to the thoracolumbar spine. In: Wolfla C., Resnick D., editors. Neurosurgical operative atlas: spine and peripheral nerves. New York: Thieme; 2007:156-160.
13. Resnick D.K., Benzel E.C. Lateral extracavitary approach for thoracic and thoracolumbar spine trauma: operative complications. Neurosurgery. 1998;43:796-802. discussion 802–803
14. Diaz P., Maillo A., Hernandez J., et al. Subarachnoid-pleural fistula as a complication of the lateral-extracavitary approach to thoracic intraspinal neurinoma. Spine (Phila Pa 1976). 1995;20:1515-1518.
15. Maiman D.J., Larson S.J., Luck E., El-Ghatit A. Lateral extracavitary approach to the spine for thoracic disc herniation: report of 23 cases. Neurosurgery. 1984;14:178-182.