Laryngoscopes and tracheal intubation equipment
Laryngoscopes
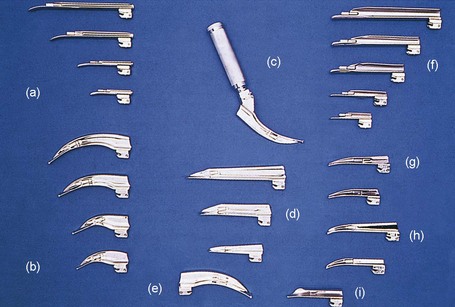
These devices are used to perform direct laryngoscopy and to aid in tracheal intubation (Fig. 7.1).
Components
Mechanism of action
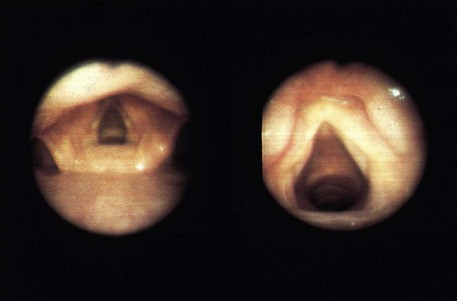
1. Usually the straight blade is used for intubating neonates and infants. The blade is advanced over the posterior border of the relatively large, floppy V-shaped epiglottis which is then lifted directly in order to view the larynx (Fig. 7.3B). There are larger size straight blades that can be used in adults.
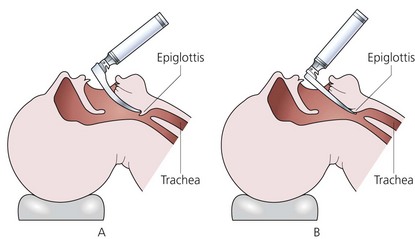
Fig. 7.3 Use of the laryngoscope.
2. The curved blade (Macintosh blade) is designed to fit into the oral and oropharyngeal cavity. It is inserted through the right angle of the mouth and advanced gradually, pushing the tongue to the left and away from the view until the tip of the blade reaches the vallecula. The blade has a small bulbous tip to help lift the larynx (Fig. 7.3A). The laryngoscope is lifted upwards elevating the larynx and allowing the vocal cords to be seen. The Macintosh blade is made in four sizes.
3. In the standard designs, the light source is a bulb screwed on to the blade and an electrical connection is made when the blade is opened ready for use. In more recent designs, the bulb is placed in the handle and the light is transmitted to the tip of the blade by means of fibreoptics (Fig. 7.4). Opening the blade turns the light on by forcing the bulb down to contact the battery terminal.
4. A left-sided Macintosh blade is available. It is used in patients with right-sided facial deformities making the use of the right-sided blade difficult.
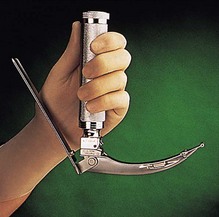
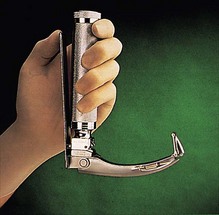
5. The McCoy laryngoscope is based on the standard Macintosh blade. It has a hinged tip which is operated by the lever mechanism present on the back of the handle. It is suited for both routine use and in cases of difficult intubation (Figs 7.5 and 7.6). A more recent McCoy design has a straight blade with a hinged tip. Both the curved and the straight McCoy laryngoscopes use either a traditional bulb in the blade or a lamp mounted in the handle which fibreoptically transmits the light to the blade.
6. A more recent design called the Flexiblade exists, where the whole distal half of the blade can be manoeuvred rather than just the tip, as in the McCoy. This can be achieved using a lever on the front of the handle.
7. The blades are designed to be interchangeable between different manufacturers and laryngoscope handles. Two international standards are used: ISO 7376/2009 (green system) and ISO 7376/1 (red system) with a coloured marking placed on the blade and handle. The two systems have different dimension hinges and with different light source positions. The ‘green system’ is the most commonly used fitting standard.
Problems in practice and safety features
1. The risk of trauma and bruising to the different structures (e.g. epiglottis) is higher with the straight blade.
2. It is of vital importance to check the function of the laryngoscope before anaesthesia has commenced. Reduction in power or total failure due to the corrosion at the electrical contact point is possible.
3. Patients with large amounts of breast tissue present difficulty during intubation. Insertion of the blade into the mouth is restricted by the breast tissue impinging on the handle. To overcome this problem, specially designed blades are used such as the polio blade. The polio blade is at about 120° to the handle allowing laryngoscopy without restriction. The polio blade was first designed to intubate patients ventilated in the iron lung during the poliomyelitis epidemic in the 1950s. A Macintosh laryngoscope blade attached to a short handle can also be useful in this situation.
4. To prevent cross-infection between patients, a disposable blade (Fig. 7.4) is used. A PVC sheath can also be put on the blade of the laryngoscope. The sheath has low light impedance allowing good visibility.
5. Laryngoscope handles must be decontaminated between patients to prevent cross-infection.
Fibreoptic intubating laryngoscope
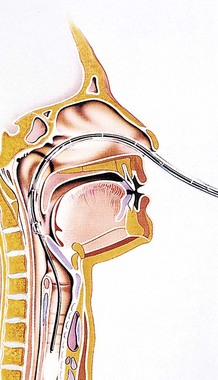
These devices have revolutionized airway management in anaesthesia and intensive care (Fig. 7.7). They are used to perform oral or nasal tracheal intubation (Figs 7.8 and 7.9), to evaluate the airway in trauma, tumour, infection and inhalational injury, to confirm tube placement (tracheal, endobronchial, double lumen or tracheostomy tubes) and to perform tracheobronchial toilet.
Components
1. Control unit which consists of the following:
a) tip deflection control knob (the bending angle range is 60–180° in the vertical plane)
c) diopter adjustment ring (focusing)
d) suction channel which can also be used to insufflate oxygen and administer local anaesthetic solutions.
2. The flexible insertion cord consists of bundles of glass fibres. Each bundle consists of 10 000–15 000 fibres nearly identical in diameter and optical characteristics.
3. Light-transmitting cable to transmit light from an external source.
4. Other equipment may be needed, e.g. endoscopic face mask, oral airway, bite block, defogging agent.
Mechanism of action
1. The fibreoptic laryngoscope uses light transmitted through glass fibres. The fibres used have diameters of 5–20 µm, making them capable of transmitting light and being flexible at the same time.
2. The fibres are coated with a thin external layer of glass (of lower refractive index) thus providing optical insulation of each fibre in the bundle. A typical fibreoptic bundle is composed of up to 10 000 individual glass fibres.
3. Light enters the fibre at a specific angle of incidence. It travels down the fibre, repeatedly striking and being reflected from the external layer of glass at a similar angle of incidence until it emerges from the opposite end.
4. The fibres are ‘coherently’ arranged throughout the bundle. As each fibre carries a very small part of the overall picture, it is essential for the clear transmission of an image that the arrangement of fibres is the same at both ends of the fibreoptic cable.
5. The insertion cords vary in length and diameter. The latter determines the size of the tracheal tube that can be used. Smaller scopes are available for intubating children. The outer diameter ranges from 1.8 to 6.4 mm allowing the use of tracheal tubes of 3.0–7.0-mm internal diameter.
Problems in practice and safety features
1. The intubating fibreoptic laryngoscope is a delicate instrument that can easily be damaged by careless handling. Damage to the fibre bundles results in loss of the image and light in individual fibres which cannot be repaired.
2. The laryngoscope should be cleaned and dried thoroughly as soon as possible after use.
Videolaryngoscopes
Recent advances in miniaturized, high-resolution, digital camera and fibreoptic technology have led to a new generation of ‘crossover’ devices. These videolaryngoscopes, offering indirect laryngoscopy, combine features of both the flexible fibreoptic scopes and the standard rigid laryngoscopes (Fig. 7.10). The images are transmitted using fibreoptics or lenses and prisms with the light pathways encased in a rigid device. The cameras used offer wide views so allowing the user to see around corners, similar to the fibreoptic scopes. Certain designs have a channel that guides the tracheal tube into the trachea.
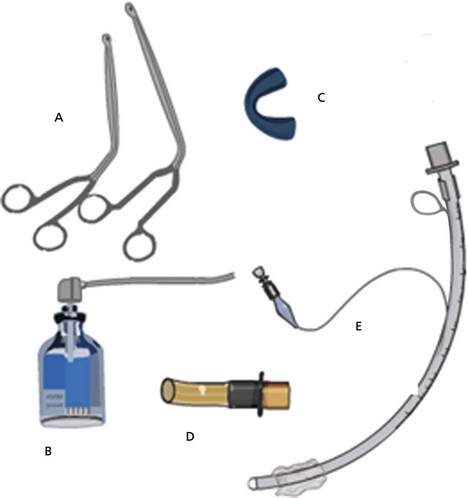
Magill forceps
These forceps are designed for ease of use within the mouth and oropharynx. Magill forceps come in small or large sizes (Fig. 7.11). During tracheal intubation, they can be used to direct the tracheal tube towards the larynx and vocal cords.
Care should be taken to protect the tracheal tube cuff from being damaged by the forceps.
Introducer, bougie, bite guard, local anaesthetic spray, Endotrol tube and Nosworthy airway
1. A local anaesthetic spray is used to coat the laryngeal and tracheal mucosa, usually with lidocaine. This decreases the stimulus of intubation.
2. A bite guard protects the front upper teeth during direct laryngoscopy.
3. The Endotrol tube has a ring-pull on its inner curvature connected to the distal end of the tube. During intubation, the ring-pull can be used to adjust the curvature of the tube.
4. The Nosworthy airway is an example of the many modifications that exist in oropharyngeal airway design. This airway allows the connection of a catheter mount and a breathing system.
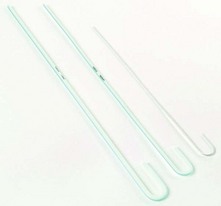
5. An introducer or stylet (Fig. 7.12) is used to adjust the curvature of a tracheal tube to help direct it through the vocal cords.
6. A gum elastic bougie is used when it is difficult to visualize the vocal cords. First, the bougie is inserted through the vocal cords, then the tracheal tube is railroaded over it. Single use intubating bougies are available (Fig. 7.13).
7. The airway exchange catheter (AEC) (Fig. 7.14) allows the exchange of tracheal tubes. It is a long hollow tube that can be inserted through a tracheal tube. This can then be withdrawn and another tracheal tube is inserted over it. Specially designed detachable 15-mm male taper fit and Luer-Lok connectors can be used to provide temporary oxygenation.
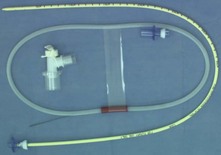
Fig. 7.14 The airway exchange catheter.
8. The Aintree intubation catheter (Fig. 7.15). This catheter is designed to be used with a fibrescope being passed through a laryngeal mask or other supraglottic airway device. It allows any appropriate size of tracheal tube to be inserted into the trachea which would otherwise be limited by the size of tube that could be passed through the supraglottic airway.

Fig. 7.15 The Aintree intubation catheter.
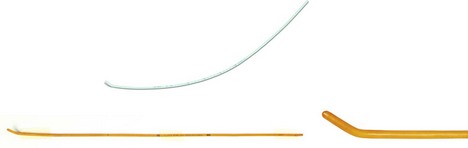
Retrograde intubation set (Fig. 7.16)
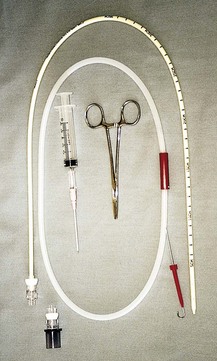
Fig. 7.16 The Cook retrograde intubation set.
Mechanism of action
1. The introducer needle is inserted through the cricothyroid membrane.
2. The guidewire is advanced in a retrograde (cephalic) direction to exit orally or nasally.
3. The hollow guiding catheter is then introduced in an antegrade direction into the trachea. The proximal end of the catheter can be connected to an oxygen supply.
4. A tracheal tube (5 mm or larger) can be introduced over the guiding catheter into the trachea.
Cooper R.J., Laryngoscopy – its past and future. Canadian Journal of Anaesthesia 2004;51:R1–R5. Online. Available at, http://www.springerlink.com/content/y8k03q8966rj8878/
MHRA. Medical device alert: reusable laryngoscope handles – all models and manufacturers (MDA/2011/0096). Online. Available at http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/CON129213, 2011.
Thong S.Y., Lim Y., Video and optic laryngoscopy assisted tracheal intubation – the new era. Anaesthesia and Intensive Care 2009;37:219–233. Online. Available at, http://xa.yimg.com/kq/groups/14982767/1890596062/name/Video+and+optic+laryngoscopy+assisted+tracheal+intubation+%C2%96+the+new+era.pdf
In the following lists, which of the statements (a) to (e) are true?
a) Straight blade laryngoscopes are only used in neonates and infants.
b) The left-sided Macintosh blade is designed for a left-handed anaesthetist.
c) The Macintosh blade is designed to elevate the larynx.
d) The Macintosh polio blade can be used in patients with large breasts.
e) The McCoy laryngoscope can improve the view of the larynx.
2. Light failure during laryngoscopy can be caused by:
3. Concerning retrograde intubation:
a) The introducer needle is inserted at the level of second and third tracheal cartilages.
b) It is a very safe procedure with no complications.
c) A guidewire is inserted in a cephalic direction.
d) Supplemental oxygen can be administered.
e) A tracheal tube (5 mm or larger) can be introduced over the guiding catheter into the trachea.
a) False. Straight blade laryngoscopes can be used for adults, neonates and infants. Because of the shape and size of the larynx in small children, it is usually easier to intubate with a straight blade laryngoscope. The latter can be used in adults, but the curved blade laryngoscope is usually used.
b) False. The left-sided Macintosh blade is designed to be used in cases of difficult access to the right side of the mouth or tongue, e.g. trauma or tumour.
c) True. The Macintosh curved blade is designed to elevate the larynx thus allowing better visualization of the vocal cords.
d) True. The polio blade was designed during the polio epidemic in the 1950s to overcome the problem of intubating patients who were in an ‘iron lung’. In current practice, it can be used in patients with large breasts where the breasts do not get in the way of the handle.
e) True. By using the hinged blade tip, the larynx is further elevated. This improves the view of the larynx.
2. Light failure during laryngoscopy can be caused by:
c) False. This should not cause light failure. It may, however, cause a worse view of the larynx.
e) True. This usually happens in the traditional laryngoscope design where the handle needs good contact with the blade for the current to flow from the batteries to the bulb in the blade. Corrosion at that junction can cause light failure. Laryngoscopes using fibreoptics do not suffer from this problem as the bulb is situated in the handle.
3. Concerning retrograde intubation:
a) False. The needle is inserted through the cricothyroid membrane.
b) False. Retrograde intubation can cause haemorrhage or pneumothorax.
c) True. The guidewire is inserted in a retrograde cephalic direction to exit through the mouth or nose.
d) True. Oxygen can be given through the proximal end of the guiding catheter.