Chapter 53 Laminotomy, Laminectomy, Laminoplasty, and Foraminotomy
Positioning
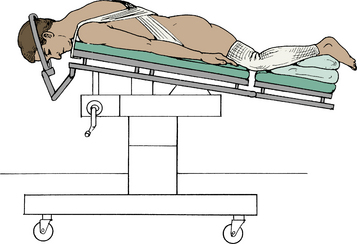
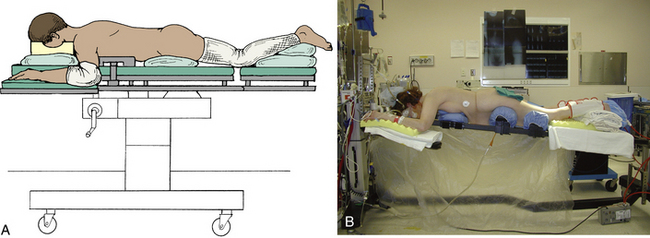
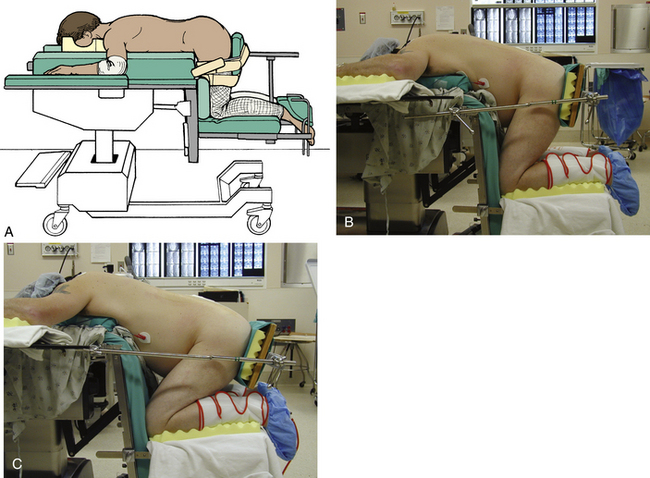
Positioning for thoracic and lumbar decompressive surgery is dictated by the level of the spine being operated upon. Exposure of the upper thoracic spine requires that the patient be prone with the neck moderately flexed, the arms at the side, and the shoulders depressed (Fig. 53-1). Middle and lower thoracic spine exposure requires that the patient be prone, with the arms either at the side or abducted at the shoulders and flexed at the elbows (Fig. 53-2). We recommend that head tongs, such as Gardner-Wells tongs, be used to allow the head to hang freely, thereby avoiding external pressure on the eyes and reducing intraocular pressure. In addition, we prefer that the head of the bed be elevated to reduce facial swelling, which can contribute to airway edema (see Fig. 53-2B). Lumbar exposure may be facilitated in either the prone position, kneeling position (Fig. 53-3), knee-chest position, or lateral decubitus position. The important common feature of all of these positions is the absence of abdominal compression, reducing intra-abdominal pressure and epidural bleeding. It is important to limit hip and knee flexion to approximately 90 degrees or slightly greater to avoid hyperflexion of the knees, which can result in calf swelling and possible compartment syndrome (see Fig. 53-3C). The prone and kneeling position, as compared with the lateral decubitus position, allows complete exposure of the dorsal elements from the cranium to the sacrum. It allows the surgical assistant to have an adequate view of the vertebral column and allows at least four hands to be available to help with the procedure. Surgeries are currently rarely done in the lateral decubitus position. There are, however, potential disadvantages of the prone position. These include restriction of thoracic expansion, compression of the abdominal viscera (producing increased venous pressure in the epidural venous plexus), and the potential for ocular and peripheral nerve compression. These disadvantages can be obviated by use of a Jackson operating table with Gardner-Wells skull traction, as was noted earlier in the chapter (see Fig. 53-2B). This setup allows the abdomen to hang freely, thereby eliminating abdominal compression, and suspends the head, thereby eliminating the potential for ocular pressure and facial abrasions.
To position for upper thoracic procedures (T1-5), the head is placed in three-point fixation using Mayfield tongs (see Fig 53-1) to provide stability to the lower cervical and upper thoracic spine. Ophthalmic ointment is applied to the eyes, which are taped shut prior to prone positioning. If head tongs are not employed, plastic goggles may be utilized to minimize the risk of pressure on the eyes. Compression stockings and serial venous compression devices should be placed on the patient’s legs to reduce the likelihood of deep venous thrombosis and possible pulmonary embolus. In turning the patient to the prone position, care is taken to prevent twisting the neck. The patient is log-rolled onto soft bolsters that extend from the shoulders to the pelvis, allowing the weight to be carried at these four points and allowing the chest to expand and the abdomen to be free from compression. The skeletal head holder is positioned so that the cervical spine is mildly flexed (“military position”). All bony prominences, particularly the elbows, are padded, and the arms are tucked to the side. Exposure can be facilitated by using 3-inch-wide adhesive tape to depress the shoulders by extending the tape from the tip of one shoulder to the opposite side of the table in a crisscross fashion, ensuring that the cross occurs at the thoracolumbar region and does not involve the upper thoracic region. Care must be exercised to avoid extreme shoulder depression, which can produce a traction injury to the brachial plexus. The operative table is then tilted in a mild, reverse Trendelenburg position to elevate the head in relation to the feet and to place the upper thoracic vertebrae parallel to the floor (see Figs. 53-1 and 53-2B).
Positioning for lumbar spine exposure may be prone, lateral decubitus position, or knee-chest position. Our preference is either the kneeling position on an Andrews operating table (see Fig. 53-3A) or modified kneeling frame (see Fig. 53-3B) or the knee-chest position. These positions avoid abdominal compression, thereby reducing epidural bleeding. It is important to check preoperatively that the patient is able to flex both hips and knees to 90 degrees. The kneeling types of positioning are generally not appropriate for patients who weigh more than 300 pounds because of the risk of pressure blisters on the knees with prolonged kneeling. For most adults, this is an excellent method of positioning for lumbar exposures. The authors have used this position without difficulty for many patients in the late stages of pregnancy. If the Andrews table is used, it is important to measure the chest-to-knee distance accurately before turning the patient to the prone position. As with all face-down positioning, eye protection is necessary, and venous compression stockings and alternating leg compression devices (pneumatic compression stockings) are important. The patient’s feet should be padded before they are placed in the stirrups of the Andrews table. As the patient is being slid into the knee-chest position, it is important to keep sliding until the thighs are flexed 90 to 95 degrees. The buttocks board should be placed high on the buttocks so that it does not compress the sciatic nerves in the upper thigh. The arms are abducted 90 degrees at the shoulders, and the elbows are flexed 90 degrees, with padding of the axilla and the elbow to prevent peripheral nerve compression.
Decompression
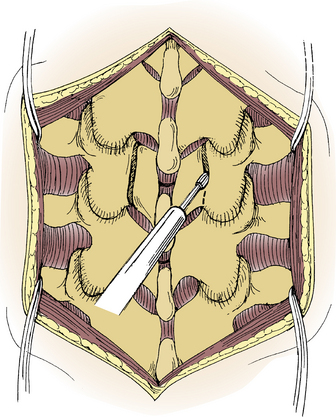
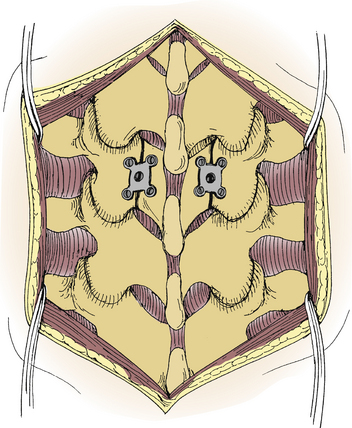
In decompressing a highly stenotic canal at the spinal cord level, it is always safer to begin the decompression at a normal or minimally stenotic segment rather than at the most stenotic segment. Decompression of a highly stenotic L4-5 segment, for example, is more safely initiated at the L5-S1 level, which is rarely severely narrowed. Thinning the lamina with a high-speed bur will facilitate decompression by permitting use of a smaller Kerrison rongeur having a smaller foot plate. Trying to force a bigger rongeur with a larger foot plate into a stenotic canal can result in inadvertent injury to the spinal cord or cauda equina (Fig. 53-4). An alternative technique is to use a high-speed bur to create bilateral troughs in order to remove the lamina en bloc. This also offers the option to leave the dorsal arch intact so that it may be replaced and secured with miniplate fixation if considering a laminoplasty (Fig. 53-5). Although not commonly performed in the lumbar spine, this has been described as an option in a skeletally immature spine to prevent a delayed spine deformity.
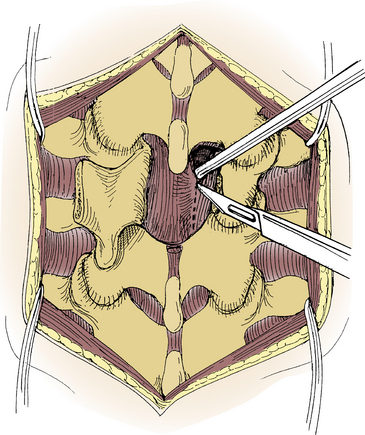
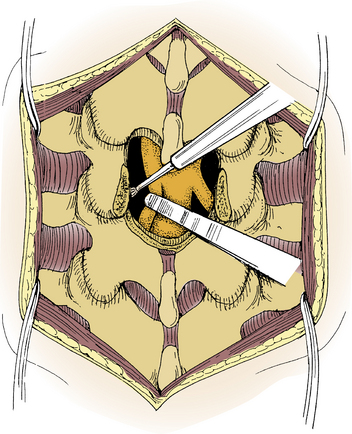
Some surgeons prefer to remove as much bone as possible before removing the ligamentum flavum, since the latter provides additional protection to the underlying nerves or spinal cord. Since the ligamentum flavum attaches approximately halfway up on the ventral surface of the cephalad lamina, removal of the inferior half of the lamina exposes the origin of the ligamentum. A small straight or angled curette can be used to separate the ligamentum from the ventral surface of the lamina to facilitate insertion of a Kerrison punch. A dural separator can then be passed beneath the ligamentum, which can then be incised longitudinally by using a scalpel and then removed piecemeal with a Kerrison rongeur (Fig. 53-6). It is essential that the ligament be completely free of any adhesions to the underlying dura before it is removed. When the dura is tightly adherent to the overlying ligamentum flavum or to a synovial cyst, dural tears are more likely to occur. Great care and gentle dissection are required to free such adhesions before the ligament is removed.
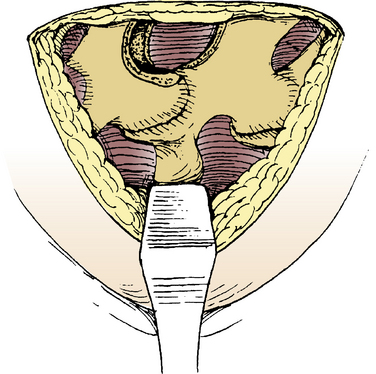
The laminectomy may be widened by undercutting the facet joints by using a high-speed bur, a Kerrison rongeur, or even a sharp chisel. Since large bites with an angled punch could result in excessive bone removal from the facet joint or the pars interarticularis, a high-speed bur may be used to thin the lamina so that a smaller punch can be used to remove residual compressive bone without injuring the facet joint. In using a high-speed bur to undercut the facet joint, a cottonoid should be placed over the dura for protection (Fig. 53-7). Although not commonly used any more, a sharp chisel can also be used to loosen the bone before removing it with a small angled Kerrison punch. Epidural venous bleeders should be controlled with bipolar coagulation, and bone bleeding can be reduced with bone wax. If a lumbar facet is inadvertently fractured, the fractured fragments are generally removed.
Although inadvertent durotomy may occur with either a high-speed power bur or a Kerrison rongeur, it is the latter that is the most common cause of dural injury. When a durotomy is encountered, it is important that it be repaired promptly. In general, it is better to repair a durotomy when it is noted rather than later in the case, as loss of the turgidity of the intact dural sac with its enclosed cerebrospinal fluid will result in excessive bleeding from loss of the tamponade effect of the full dural sac on the epidural vessels. Most durotomies can be repaired by direct suture of the defect. The author prefers a running #6-0 or #5-0 silk suture if possible. The use of end sutures, in which each end of the durotomy is sutured with a separate suture to allow gentle retraction and elevation by a surgical assistant, facilitates closure by elevating and profiling the defect. This technique also separates the edges of the dura from the underlying nerve roots or spinal cord, thereby reducing the likelihood of inadvertent incarceration of the underlying neural structures. The dural repair can then be augmented with a fibrin glue sealant if necessary. If direct suturing is not possible because of the location of the tear, a piece of fascia, a collagen matrix patch, or fibrin sealant may be used.
Lumbar laminoplasty, in a manner analogous to that performed in the cervical spine, has been described.1 Although rarely performed, it may have a role in the skeletally immature patient with central stenosis, as described previously.2 The lamina of the stenotic segment may be hinged and opened on the opposite side, using a small plate to keep the hinged side open, or the lamina can be removed and reapplied by using miniplates and screws bilaterally (see Fig. 53-5).
The amount of bone and ligament removal required for unilateral neural compression from disc herniation or focal, unilateral stenosis is dictated by the extent of concomitant pathology and the ease with which the primary compressing pathology can be accessed. Usually, decompression is required only to the proximal origin (insertion) of the ligamentum flavum (Fig. 53-8).
Wound Closure
It is important to obtain a good closure of the deep thoracolumbar fascia, since this provides the major strength of the closure. The deep thoracolumbar fascia should be closed with a heavy, interrupted, absorbable suture, although a nonabsorbable suture can be used. If a durotomy has occurred, an oversewn, running, locking suture of the deep fascia should be performed in addition to the interrupted deep suture to provide a watertight closure. The subcutaneous tissues are then closed with an interrupted inverted absorbable suture material. In the upper thoracic region in which there is tension from the pectoral girdle muscles, the skin may be closed with interrupted mattress sutures or staples with deep retention sutures over bolsters to prevent separation of the wound. The wound is then covered with a light, dry, sterile dressing. The sutures are normally kept in place in the upper thoracic spine for approximately 2 weeks.
Kawaguchi Y., Kanamori M., Ishihara H., et al. Clinical and radiographic results of expansive lumbar laminoplasty in patients with spinal stenosis. J Bone Joint Surg [Am]. 2004;86:1698-1703.
Tsuji H., Itoh T., Sekido H., et al. Expansive laminoplasty for lumbar spinal stenosis. Int Orthop. 1990;14:309-314.
1. Tsuji H., Itoh T., Sekido H., et al. Expansive laminoplasty for lumbar spinal stenosis. Int Orthop. 1990;14:309-314.
2. Kawaguchi Y., Kanamori M., Ishihara H., et al. Clinical and radiographic results of expansive lumbar laminoplasty in patients with spinal stenosis. J Bone Joint Surg [Am]. 2004;86:1698-1703.