40
Labour
Introduction
Labour is defined as the onset of regular uterine activity associated with effacement and dilatation of the cervix and descent of the presenting part through the cervix. The control and timing of delivery is crucial in the survival of any species and, in most, the interval between conception and parturition varies little. This is not the case in human pregnancy, where delivery can occur many weeks before or after the expected date.
Labour in humans is surprisingly hazardous. Evolution ought to have favoured those mothers who deliver without problems, and yet, for those without access to good medical care, the lifetime risk of dying from labour and postnatal complications may be ≥ 10%.
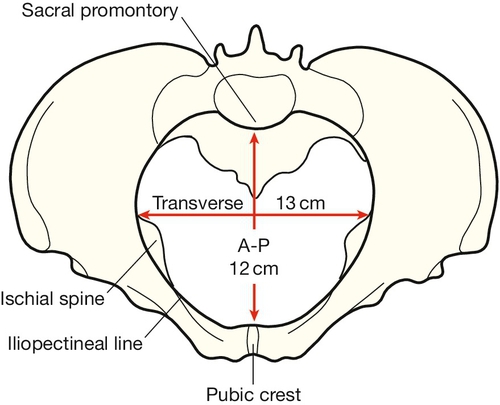
Apes are able to give birth with little problem. Their pelvises are relatively large, the fetal head is relatively small and the fetus is born facing anteriorly. When the Australopithecines adopted an upright posture around 4 million years ago, the pelvic shape became narrower in the anteroposterior plane to allow more efficient weight transfer from the trunk to the femurs. As the fetal head was still relatively small, the Australopithecines were also able to deliver without much problem, although the head was this time in the transverse position.
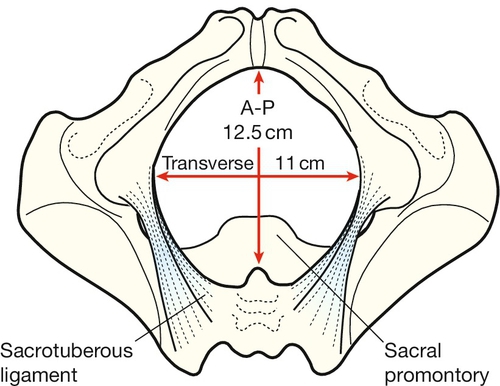
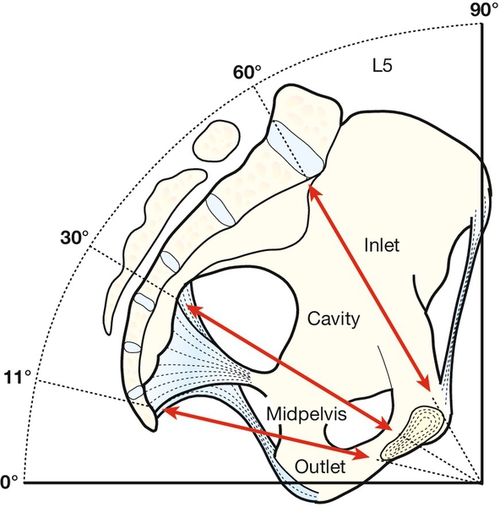
With further evolution 1.5 million years ago, to Homo erectus and then Homo sapiens, the volume of the brain increased from around 500 mL to 1000–2000 mL. This increased the chance of the head being bigger than the pelvis (cephalopelvic disproportion) and to deliver successfully, it became necessary for the head to rotate during delivery. The head entered the pelvic brim in the transverse position, as the inlet is widest in the transverse plane, but rotated at the pelvic floor to the anteroposterior plane, which is the widest diameter of the pelvic outlet.
This process requires efficient uterine activity and is aided by ‘moulding’ of the fetal head. Moulding is possible because the individual skull bones are unfused and can therefore move or even override each other to form the most efficient shape for delivery. The pelvic ligaments, particularly the cartilaginous joint of the symphysis pubis, relax antenatally under the influence of a hormone called relaxin, to maximize the pelvic diameters. Successful delivery also requires the fetus to enter the pelvis in the appropriate position. When these criteria are not met, problems may occur and these are discussed further in Chapter 45. The difficulty with human delivery, then, is related to the balance between our need to run (and therefore have a narrow pelvis) and our need to think (and therefore have a big head).
Primigravid compared with multigravid labour
There is a considerable difference between the labour of a primigravida (a mother having her first labour) and that of a parous woman who has had a previous vaginal delivery (Table 40.1). A successful vaginal delivery first time around usually leads to subsequent deliveries being relatively uneventful. Conversely, a caesarean section in a first labour can lead to subsequent obstetric problems.
Table 40.1
The difference between a normal primigravid and multigravid labour
| Primigravida | Multigravida |
| Unique psychological experience | |
| Inefficient uterine action is common, therefore labour is often longer | Uterine action is efficient and genital tract stretches more easily, therefore labour is usually shorter |
| The functional capacity of the pelvis is not known – cephalopelvic disproportion is a possibility | Cephalopelvic disproportion is rare. If it does occur, it is usually secondary to some serious problem |
| Serious injury to the child is relatively more common. The incidence of instrumental delivery is higher | Serious injury to the child is rare. Furthermore, the risk of birth injury is less when the baby is born by propulsion rather than traction |
| Uterus is virtually immune to rupture | There is a small risk of uterine rupture, particularly if there is a pre-existing caesarean section scar |
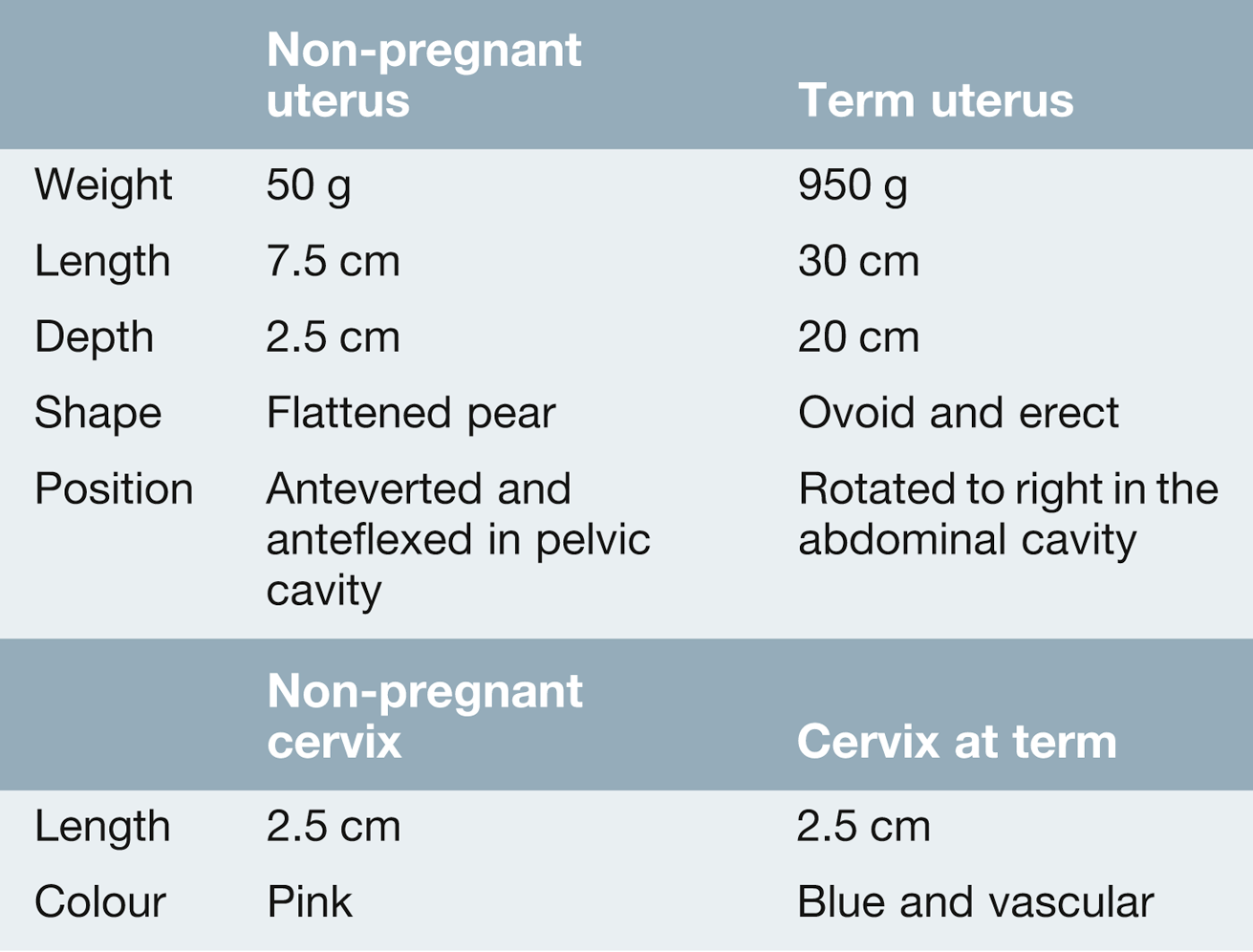
The uterus during pregnancy
The uterus is a thick-walled hollow organ, normally located entirely, in the non-pregnant state, within the lesser pelvis (Table 40.2). The smooth muscle fibres interdigitate to form a single functional muscle which increases markedly during pregnancy, mainly by hypertrophy (an increase in size of cells) and to a lesser extent, by hyperplasia (an increase in the number of smooth muscle cells).
From early pregnancy onwards, the uterus contracts intermittently, and the frequency and amplitude of these contractions increase as labour approaches. These ‘Braxton Hicks’ contractions are irregular, low frequency and high amplitude in character and are only occasionally painful. They normally begin at a ‘pacemaker point’ close to the junction of the uterus and the fallopian tube and spread from this point downwards. Intensity is maximal at the fundus (where the muscle is thickest), intermediate at the mid-zone and least at the lower segment.
The initiation of labour
The mechanisms controlling the onset of labour are different for different mammals. In some mammals, it is the changing levels of oestrogen and progesterone which regulate the timing of onset. In other animals, for example sheep, there is some evidence that the fetal adrenal secretion of corticosteroids is the responsible trigger. In humans, however, despite major advances in molecular biology and the science of reproduction, there is still much that is not known about the physiological processes involved in the initiation of labour. Any proposed mechanism must therefore be considered to be a hypothesis.
It seems that there is a balance between pro-pregnancy factors and pro-labour factors (Box 40.1), the pro-pregnancy factors promoting pregnancy continuation and the pro-labour factors stimulating the onset of labour. Labour may be triggered when the pro-pregnancy factors become overwhelmed by increasing levels of the pro-labour factors, although why this should occur at one particular point remains uncertain. There is some limited evidence that the human fetus may play a role in regulating this balance, but the mother also has a role.
Pro-pregnancy factors
Progesterone is derived from the corpus luteum for the first 8 weeks or so of pregnancy and thereafter from the placenta. It has the direct effect of decreasing uterine oxytocin receptor sensitivity and therefore promotes uterine smooth muscle relaxation. That it plays a significant pro-pregnancy role is illustrated by the fact that the progesterone antagonist mifepristone increases myometrial contractility, and has been successfully used to induce labour. Nitric oxide, a highly reactive free radical, is also a pro-pregnancy factor. Some studies have observed a fall in uterine nitric oxide synthetase activity as pregnancy advances, but these findings are not confirmed in other studies. Catecholamines act directly on the myometrial cell membrane to alter contractility and beta-sympathomimetics are used as tocolytics to suppress preterm labour. The specific roles for catecholamines in physiological terms and the role of the hormone relaxin are unclear.
Pro-labour factors
Oxytocin, a nonapeptide from the posterior pituitary, is a potent stimulator of uterine contractility. Circulating levels, however, do not change as term approaches. Oestrogen levels do increase, and oestrogens increase oxytocin receptor expression within the uterus. This gradual rise may be mediated in part by fetal adrenocorticotrophic hormone (ACTH). Prostaglandin levels also increase prior to the onset of labour. These are synthesized from arachidonic acid by cyclo-oxygenase (COX), and COX-2 enzyme expression in the fetal membranes has been observed to double by the time labour begins. Prostaglandins promote cervical ripening and stimulate uterine contractility both directly and by upregulation of oxytocin receptors, and there is some evidence that the increased levels may be mediated by maternal corticotrophin-releasing hormone (CRH) secretion.
The mechanism of normal labour and delivery
(See also Clinical pelvic anatomy, Chapter 1.)
The mechanism of labour involves effacement and then dilatation of the cervix, followed by expulsion of the fetus by uterine contraction. The lower part of the uterus is anchored to the pelvis by the transverse cervical (or cardinal) ligaments, as well as the uterosacral ligaments, allowing the shortening uterine muscle to drive the fetus downwards (Box 40.2).
Cervical ripening
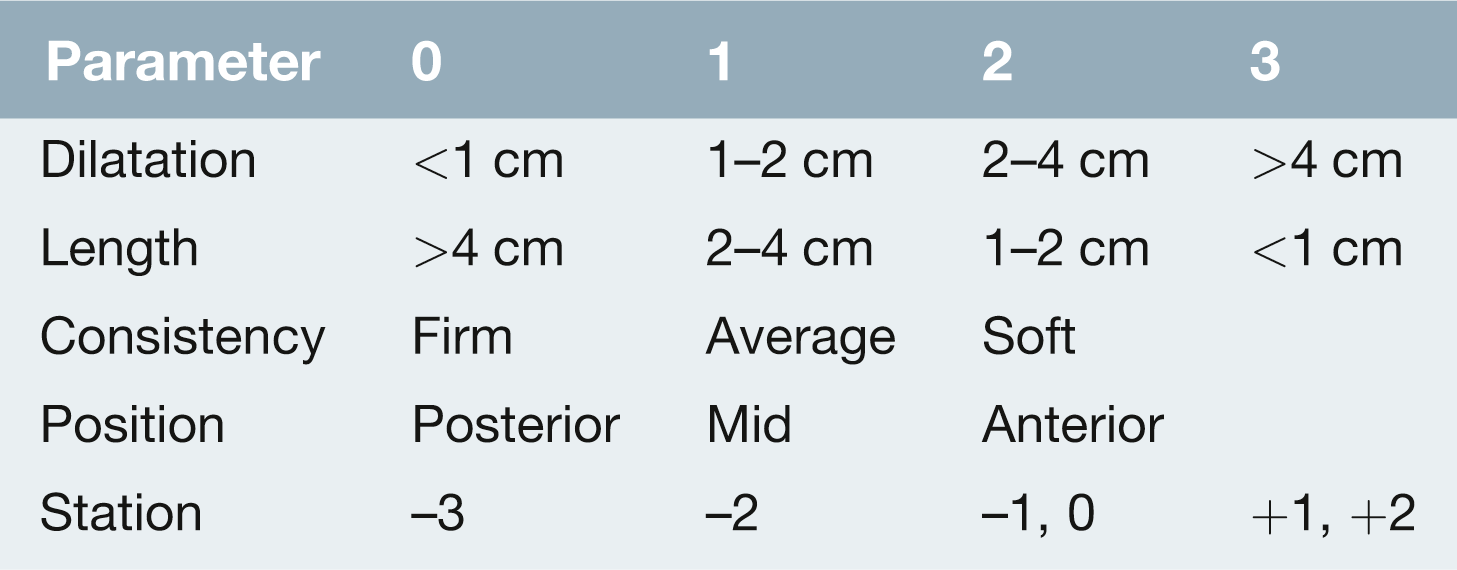
The cervix is composed of a network of collagen fibres embedded in proteoglycans and it needs to soften and efface before delivery can occur. Prostaglandins increase cervical ripening by inhibiting collagen synthesis and stimulating collagenase activity to break down the collagen. This collagenase activity comes in part from fibroblast cells but also from an influx of inflammatory cells, supporting the theory that labour is in part like an inflammatory process. Within the cervix, the result is an overall reduction in the firm collagen fibres, leaving it softer and ready to dilate. In clinical practice, cervical ripening is assessed using the Bishop’s score (Table 40.3). The parameters of this score include: cervical length, cervical dilatation, consistency, position and station of the presenting part.
Descent and delivery of fetus
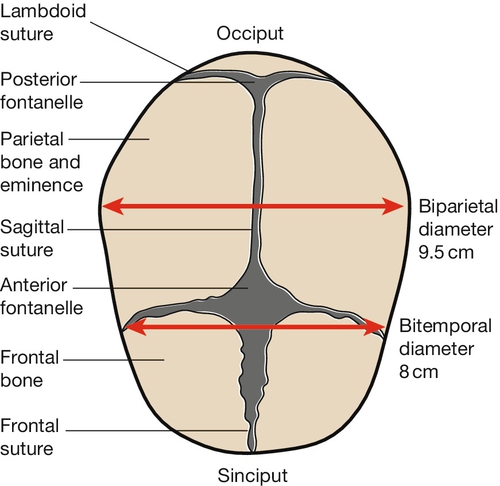
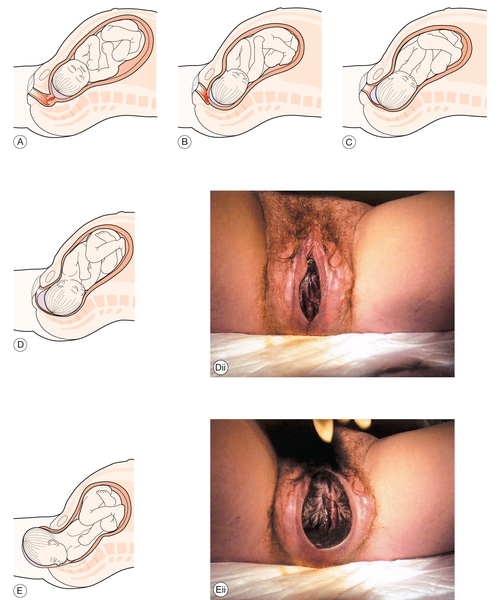
The fetus then needs to traverse the pelvis. The widest two points of the fetus are the head in the anteroposterior plane (Fig. 40.1) and the shoulders, laterally from one shoulder tip to the other (bis-acromial diameter). The head rotates from a lateral position at the pelvic brim to the anteroposterior position at the outlet (Figs 40.2–40.4). This rotation has the advantage that by the time the head is delivering through the outlet, the shoulders will be entering the inlet in the transverse position, maximizing the chance of successful delivery.
The position of the head as it traverses the canal is described according to the position of the occiput in relation to the mother’s pelvis. The head usually enters the pelvic brim in either the right or the left occipitotransverse position (Fig. 40.5A). The contracting uterus above causes the head to flex, so that the minimum head diameter is presented for delivery.
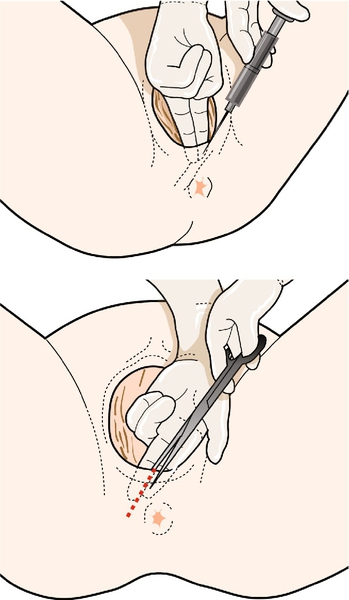
As the head descends it reaches the V-shaped pelvic floor at the level of the ischial spines (Fig. 40.5B–D). The V-shaped pelvic floor encourages the fundamentally important head rotation. Figure 40.6 illustrates the tendency for the longest part of the head to fit into the lowest part of the V-shaped gutter, achievable only by a 90° rotation to either the occipitoanterior or occipitoposterior position. In most cases, the head rotates anteriorly. The consequences of posterior rotation are discussed on page 363. The head, now occipitoanterior, descends beyond the ischial spines and extends, distending the vulva until it is eventually delivered (Fig. 40.5E,F).
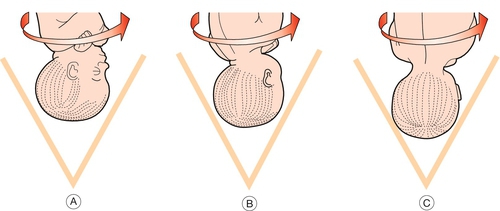
Fig. 40.6The head descends onto the pelvic floor.
This runs in a V shape, and it is this V shape, which encourages rotation of the fetal head.
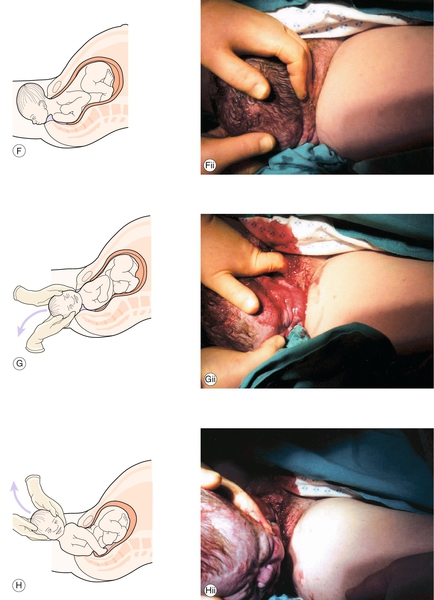
Meanwhile, at the pelvic inlet, the shoulders are now presenting in the transverse position. They too descend to the pelvic floor and rotate to the anteroposterior position in the V of the pelvic floor (Fig. 40.5G). By this time, the head has been completely delivered and it is free to rotate back to the transverse position along with the shoulders. The anterior shoulder can then be delivered by downward traction of the head, so that the lateral traction on the fetal trunk allows the shoulder to be freed from under the pubic arch (Fig. 40.5G). The posterior shoulder is delivered with upward lateral traction and the rest of the baby usually follows without difficulty (Fig. 40.5H).
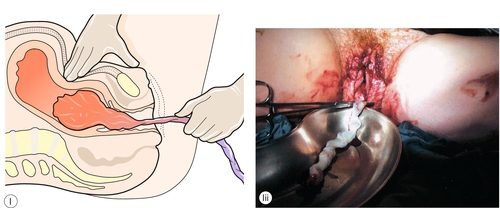
The third stage of labour is from delivery of the baby until delivery of the placenta. The uterus contracts, shearing the placenta from the uterine wall, and this separation is often indicated by a small rush of dark blood and a ‘lengthening’ of cord. The placenta can then be delivered by gentle cord traction (Fig. 40.5I) but caution is required to avoid uterine inversion.
Diagnosis of labour
The diagnosis of ‘labour’ is important but often surprisingly difficult. The diagnosis is easy in retrospect, but of course a prospective diagnosis is required. The presence of palpable contractions does not necessarily mean that a woman is in labour, as Braxton Hicks contractions are common antenatally. For labour diagnosis, there needs to be uterine contraction together with effacement and dilatation of the cervix.
Effacement has occurred when the entire length of the cervical canal has been taken up into the lower segment of the uterus, a process which begins at the internal os and proceeds downwards to the external os. This is analogous to pulling a polo-necked sweater over your head. It is of note that ‘dilatation’ refers only to the dilatation of the external os. Again, there is an important difference between primigravid and multigravid labours, as dilatation will not begin in a primigravida until effacement has occurred, whereas both may occur simultaneously in a parous woman (Fig. 40.7).
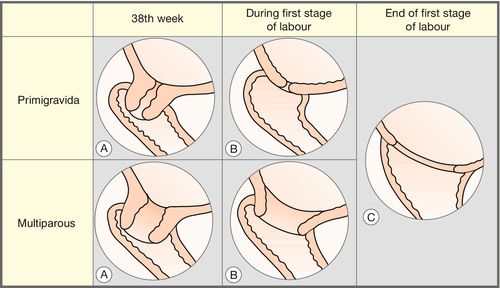
Fig. 40.7Cervical dilatation – primigravida versus multigravida.
Note that in a multigravida, the cervix may dilate before effacement is complete.
If there are regular contractions and a fully effaced cervix, the woman can be said to be in labour. If, however, there are contractions with an only partially effaced cervix, further objective evidence must be sought in the form of either a ‘show’ or spontaneous membrane rupture. A ‘show’, or blood-stained mucous discharge, has occurred in approximately two-thirds of women by the time of presentation and supports the diagnosis in those with regular contractions. Spontaneous membrane rupture in the presence of regular contractions also confirms the diagnosis.
Rupture of the membranes
Rupture of the fetal membranes is a vital part of normal labour. In 6–12% of labours, the membranes will rupture prior to the onset of uterine contractions or cervical dilatation, ‘pre-labour rupture of the membranes’. The mother will usually describe the feeling of ‘water’ leaking vaginally and, if a speculum examination is carried out, a pool of liquor is typically seen in the posterior vaginal fornix. A digital vaginal examination is not routinely indicated, as this increases the risk of introducing infection. If managed conservatively, 70% of mothers will establish in labour spontaneously by 24 h and 90% by 48 h. This conservative management, however, carries a small risk of ascending infection, which may lead to chorioamnionitis. Rarely, chorioamnionitis may progress to a rapid overwhelming fetal and maternal sepsis.
Nonetheless, in view of the high chance of spontaneous labour over the first 48 h a conservative approach may be appropriate. This is provided that the mother is apyrexial, the baby is in cephalic presentation, the liquor is clear and the fetal monitoring is normal. On the other hand, there is also evidence that induction of labour on admission may reduce the incidence of neonatal infection, with no increase in the rate of caesarean delivery. Women with pre-labour rupture of membranes should be counselled about their options and they and their partners should be involved in the decision-making process. In those managed conservatively, women should be made aware of signs and symptoms of infection and encouraged to record their temperature. If there is a clinical suspicion of chorioamnionitis with pyrexia or passage of meconium (see below), delivery must be expedited, usually by caesarean section, unless labour is well established. Pain and discharge are late features of intrauterine infection.
Clinical progress in labour
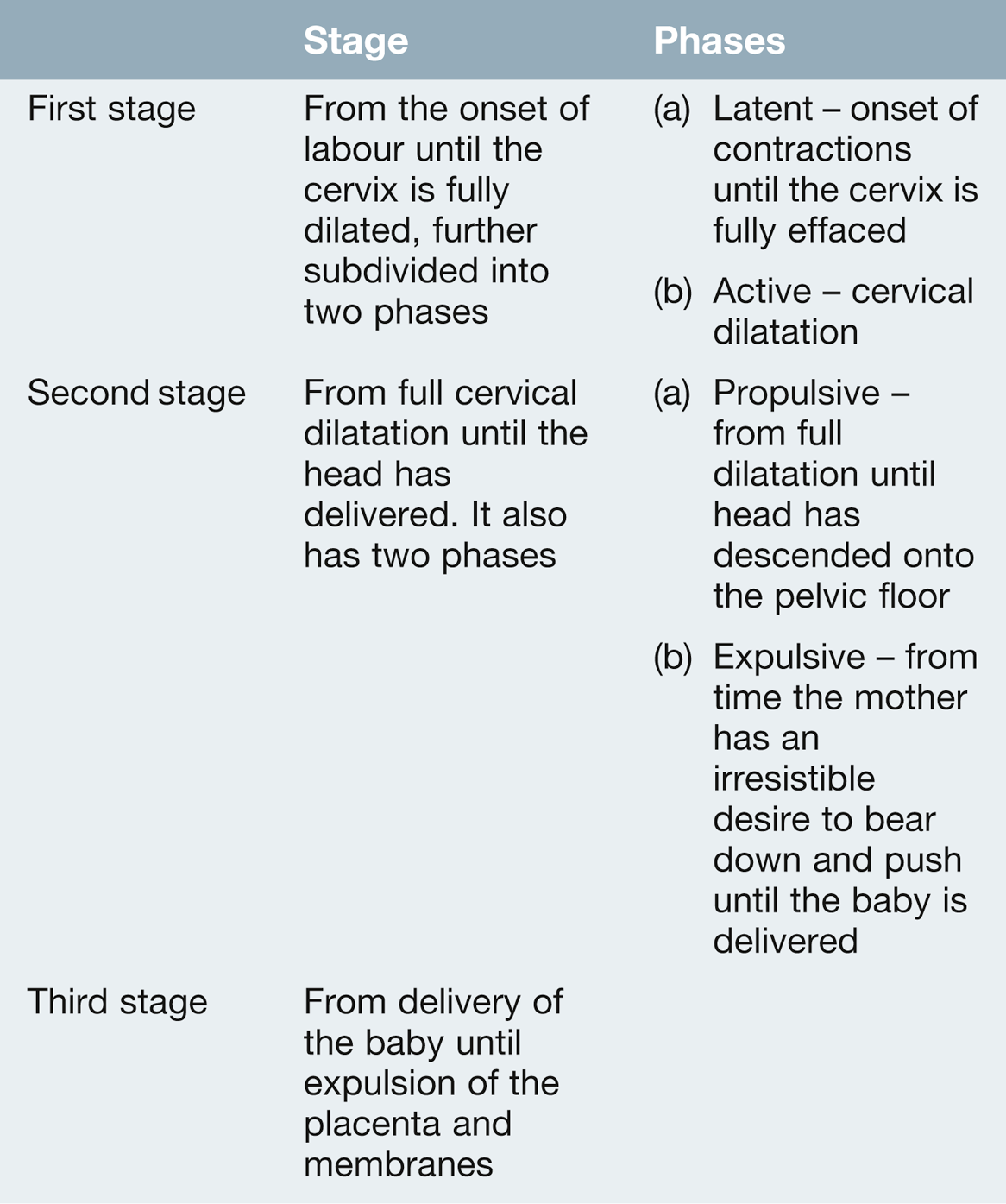
Labour is divided into three stages of unequal length (Table 40.4). There is no ‘normal’ time for the length of labour. However, the mean length of established labour (i.e. from 4 cm dilated, with regular painful contractions), is 8 h for primigravid women but can be up to 18 h. The mean length for second and subsequent labours is 5.5 h but can be up to 12 h. Even after a labour of 40 h, the chance of a vaginal delivery is still around 50%. Fetal distress (hypoxia) is only partly related to the length of labour. The highest incidence of caesarean section for distress is in the first hour of labour, probably related to babies already compromised antenatally with some pre-existing problem. Even after 24 h, however, the chance of fetal distress remains low. It is recognized that markedly prolonged labour is associated with subsequent maternal pelvic floor dysfunction and fistulae. There is therefore no ‘optimal’ length of labour and each mother should be assessed on an individual basis.
First stage
Progress in the first stage of labour is measured in terms of dilatation of the cervix and descent of the fetal head. Information about the labour is plotted on a partogram, which should be commenced when a woman is established in labour (Fig. 40.8). It forms a graphic record of clinical findings and any relevant events. The purpose is to help early recognition of abnormal labour, to ensure appropriate transfer of care and aid continuity of care.
While there is no research on the ideal frequency of vaginal examinations in labour, the World Health Organization recommends that 4-hourly vaginal examinations during normal labour are adequate. Vaginal examinations should ideally be performed by the same professional to minimise interobserver variation (Table 40.5). Vaginal examinations should not be regarded as routine; they are unpleasant, may be painful and are associated with a risk of infection even when performed in a ‘sterile’ manner. The average rate of cervical dilatation in primigravidae is around 1 cm/h, although it is accepted that ½ cm/h can be normal for some women.
Table 40.5
Vaginal examinations
| Findings on VE | Details |
| Presence or absence of meconium | Meconium staining might suggest fetal distress |
| Dilatation of the cervix | In centimetres from 0 to 10 cm |
| Station of the presenting part | In centimetres above or below the ischial spines |
| Position of the head | With reference to the occiput if cephalic, or sacrum if breech. A note should made of whether the head is flexed or deflexed |
| Presence of caput and/or moulding | If excessive, might suggest obstructed labour |
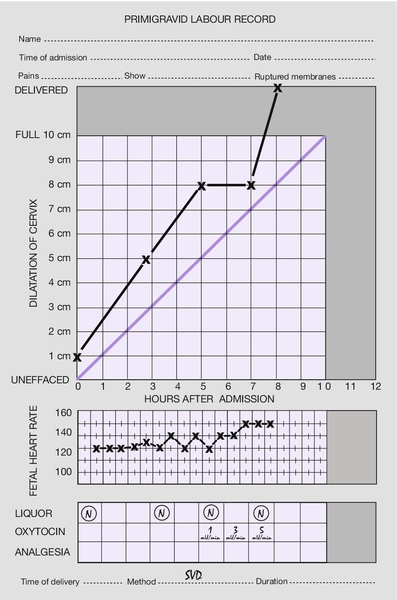
Descent of the fetal head is measured in labour by abdominal examination, when the amount of the fetal head palpable above the pelvic brim (in fifths) is documented on the partogram. If only two-fifths or less of the fetal head is palpable abdominally, then the head is determined to be ‘engaged’ (Fig. 40.9).
On vaginal examination, the ‘station’ of the fetal head with respect to the ischial spines is recorded. Care should be taken not to confuse increasing caput succedaneum (see below) with descent of the head itself. The ischial spines are designated station zero. When the head is above the spines, it is said to be at –1, –2, –3 or –4 cm. If the head is below the spines, the notation is + 1, + 2, + 3 or + 4 cm. If the head is at the level of the ischial spines, it must be engaged.
It is important to note that the ‘position’ of the head on vaginal examination is with reference to the occiput, for example occipitoanterior (OA), right occipitotransverse (ROT) or left occipitoposterior (LOT).
‘Caput’ (succedaneum) is oedema of the scalp owing to pressure of the head against the rim of the cervix and is classified somewhat arbitrarily as ‘+’, ‘++’ or ‘+++’. ‘Moulding’ describes the change in head shape, which occurs during labour, made possible by movement of the individual scalp bones. It is arbitrarily termed ‘+’ if the bones are opposed, ‘++’ if they overlap but can be reduced by digital pressure and ‘+++’ if they overlap but cannot be reduced.
Uterine activity is routinely monitored in labour by palpation, measuring length, strength and duration of contractions. Uterine activity over a 10-min period is plotted on the partogram. Women often report increasing, regular uterine activity at the onset of labour.
Second stage
This begins when the cervix is fully dilated. In a similar way to the first stage of labour, the duration of the second stage of labour is different for nulliparous and parous women. It is generally recommended that for nulliparous women, birth would be expected to take place within 3 h of the start of the active second stage of labour. For parous women, birth would be expected to take place within 2 h of the start of the active stage of labour in most women. Progress is measured in terms of descent and rotation of the fetal head on vaginal examination. There are two distinct phases:
1. The propulsive/passive phase. This is from full dilatation until the head reaches the pelvic floor. During this time, the head is relatively high in the pelvis, the position is typically occipitotransverse, the lower vagina is not stretched and the mother has no or little urge to push. In many respects it is a natural extension of the first stage of labour.
2. The expulsive/active phase. This begins when the fetal head reaches the pelvic floor and the mother usually has a strong involuntary desire to push.
With pushing, the head usually delivers. Normally it does so in the occipitoanterior position. After delivery it restitutes, returning to an occipitolateral position by rotating with the shoulders as they descend into the pelvis. The birth attendant then applies lateral traction to the head, moving it in the direction of the mother’s back to allow the birth of the anterior fetal shoulder (see above). At this point, an oxytocic is injected intramuscularly into the mother’s thigh to encourage a prolonged uterine contraction and minimize the chance of postpartum haemorrhage. The head is then lifted anteriorly to allow delivery of the posterior shoulder, after which the rest of the baby is delivered with lateral flexion of the fetal body. The umbilical cord is clamped and cut. If the baby does not require resuscitation, he or she may be placed on the mother’s abdomen and skin-to-skin contact encouraged. If this is not the woman’s preference, the baby should be wrapped in a warm towel and handed to the parents.
Third stage
Active management of the third stage of labour has been shown to decrease the risk of postpartum haemorrhage. This involves the use of an oxytocic (as above) and gentle controlled cord traction using the ‘Brandt–Andrews’ method (Fig. 40.5I). Placental separation is recognized by apparent lengthening of the cord and a gush of dark blood per vaginam. The operator exerts traction on the cord while the other hand maintains pressure upwards on the fundus. The main risk of cord traction is uterine inversion and the fundus is continually ‘guarded’ to prevent this (see p. 374). Once the placenta passes the vulva it may be gently twisted to allow the membranes to peel off completely and the uterine fundus is rubbed up to ensure that the uterus is well contracted. Some women may choose to have a physiological third stage of labour, and this involves no routine use of uterotonic drugs, no clamping of the cord until pulsation has ceased and delivery of placenta by maternal effort only.
The labia, vagina and perineum are inspected for tears and sutured if bleeding. Finally, the placenta is examined to ensure it is complete.
The normal blood loss at delivery is about 300 mL. The routine use of an oxytocic following delivery of the anterior shoulder reduces the risk of postpartum haemorrhage by about 60%.
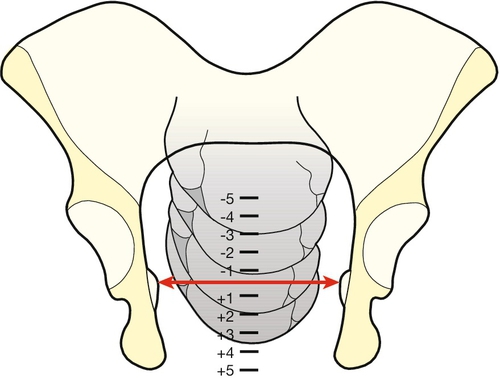
Episiotomies and perineal tears
It was previously considered that the use of episiotomy reduced the incidence of anal sphincter tears. There is, however, little evidence to support this, and there is no evidence to support routine episiotomy in all deliveries as a preventive measure against third- or fourth-degree tears. Midline episiotomy in particular, does not protect the perineum or sphincters during childbirth and may impair anal continence. If an episiotomy is to be performed, a right (or less commonly left) posterolateral episiotomy is preferred (Fig. 40.10).
Restricting the use of episiotomy to specific fetal and maternal indications leads to lower rates of posterior perineal trauma, less need for suturing and fewer long-term complications. A spontaneous tear may be less painful than an episiotomy and may also heal better.
Possible indications for an episiotomy are as follows:
![]() a rigid perineum which is preventing delivery
a rigid perineum which is preventing delivery
![]() if it is judged that a large tear is imminent
if it is judged that a large tear is imminent
![]() most instrumental deliveries (forceps or ventouse)
most instrumental deliveries (forceps or ventouse)
![]() shoulder dystocia (to permit access to the birth canal)
shoulder dystocia (to permit access to the birth canal)
![]() vaginal breech delivery.
vaginal breech delivery.
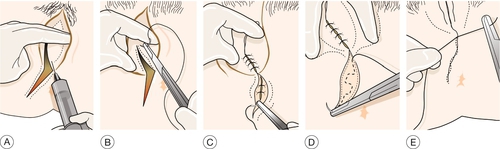
Prior to an episiotomy, local anaesthetic is injected into the subcutaneous tissues of the perineum and vagina (unless there is an effective regional block). A right mediolateral cut is made and pressure on the fetal head is maintained so that the delivery is slow and the head remains flexed, minimizing the possibility of the incision extending. Spontaneous tears are categorized into four degrees (Table 40.6). An episiotomy is an iatrogenic second-degree tear. Anterior perineal trauma is classified as any injury to the labia, anterior vagina, urethra or clitoris and is described as such.
Table 40.6
Classification of spontaneous perineal tears
| Tear involves | |
| First degree | Injury to the vaginal epithelium and vulval skin only |
| Second degree | Injury to the perineal muscles, but not the anal sphincter |
| Third degree | Injury to the perineum involving the anal sphincter complex |
| Fourth degree | Injury to the perineum involving the anal sphincter complex and anal/rectal mucosa |
Repair of episiotomies and perineal tears
Repair should be with a rapidly absorbable synthetic material (Dexon or Vicryl Rapide), using a continuous subcuticular (possibly non-locking) technique to minimize short- and long-term problems (Fig. 40.11). These newer materials result in less short-term pain and less analgesic requirements than do older materials, such as catgut and non-absorbable sutures. Good perineal hygiene after delivery is likely to aid healing, and the use of ice packs and analgesia may be useful to alleviate discomfort.
Repair of episiotomy and first- or second-degree tears
The perineum is infiltrated with local anaesthetic (Fig. 40.11A) (unless an epidural is in place or there has been a pudendal block or perineal infiltration prior to delivery). The apex of the vaginal incision or tear is identified and the first suture placed just above this level (Fig. 40.11B) (care is needed because the rectum is just posterior to the vaginal wall).
The use of a loose, continuous non-locking method for vaginal mucosa and perineal muscles and a continuous subcuticular technique for perineal skin is recommended (Fig. 40.11C–E).
Repair of third- or fourth-degree tears
This should be by an experienced clinician, in theatre, with good analgesia, good light, the appropriate instruments and an assistant. The anal mucosa (if involved) is repaired using interrupted dissolving sutures, with the knot of each suture placed in the anal canal. The internal anal sphincter is then identified and its ends approximated and sutured with a monofilament suture such as polydioxanone (PDS). Next, the ends of the external anal sphincter are identified and either approximated or overlapped, again with the monofilament suture. The rest is as described above for first- and second-degree tears. Antibiotics, laxatives and fibre are important to allow healing.